File - The Lima Project
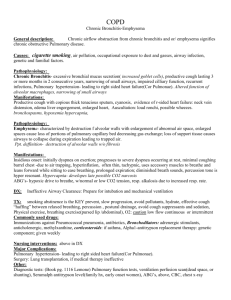
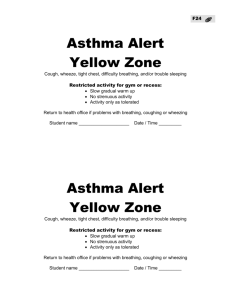
advertisement

Diagnosis Review: Pulmonary Dysfunction By: Jenny Lima and Becky Roberson Exercise can increase physical capabilities of clients with pulmonary disease, improve their quality of life, and reduce hospitalizations. Monitored exercise is incorporated into overall care of clients with chronic pulmonary disease. Treatment goals: Relieving symptoms and improving breathing through pt/caregiver education, airway clearance, breathing exercises, relaxations, and endurance and strength training will facilitate functional abilities. General Airway Clearance: Postural Drainage: Positioning a client so bronchus from a particular lung segment is perpendicular to the ground. See image. Percussion: Using cupped hands, apply rhythmic force to pt’s thorax. Shaking (not used much): Don’t Use Vibration: Both hands 1 on top of the other, directly over chest wall to provide pressure and manual vibration during exhalations. Airway Clearance: Cough (most common), Huff, Tracheal stim (in paralysis), Assisted cough, Splinting, Suctioning(last case) and aerobic Exercise. Aerobic Exercise: Adjunct to secretion removal techniques, to help clear secretions independently. Positioning: Gravity plays an important role in distribution of breath. Gravity dependcent portions of lung receive more blood flow. Therefore, gas exchange and ventilation distribution can be altered by a change in position. Diaphragmatic Breathing Exercises: Encouraging use of diaphragm, principle and most efficient muscle of inspiration, can decrease oxygen cost of breathing. Segmental or localized Breathing Exercises: expansion of a particular segment of lung using manual pressure to simulate expansion. Low Frequency breathing: Slow Deep Breathing, instruct client to breathe slowly, taking long and deep breaths, ensure the client does not hyperventilate. Breathing Devices: o Inspirometry: to encourage increased chest expansion; appropriate for all conditions where inspiration is to be encouraged. o Expirometer: Used to encourage complete emptying of lungs. Breathing through pursed lips or pursed lip breathing (PLB): Helps to improve ventilation by decreasing respiratory rate and increasing tidal volume. Blow Bottles, Candles, Weights on Abdomen: (use) General Conditioning Exercise: To prevent deconditioning caused by prolonged bed rest, thus maintaining functional abilities. Exercise: Choose correct mode/intensity, and frequency for each specific pt, exercise by heart rate, by rate of perceived exertion, or by metabolic equivalents. Warm up and cool down for 5-15 mins, with approximately 20 mins of aerobic exercise. (pt may have to take multiple breaks but end time should be 20 mins.) Focusing on controlled breathing throughout. Energy-saving Techniques: Using adaptive equipment may be helpful, and the organization and prioritizing of tasks can make a difference in functional abilities. Pacing: Used to make sure client does not become uncomfortably SOB during performance of an activity. Used during ADL’s, ambulating and stair climbing. Ex. Go up 1-2 steps at a time up the stairs, rest until breathing back to normal, then repeat. Education to Pt. HEP Patient education on exercise, conservation and Pacing. Pulmonary Pathologies Acute Respiratory Distress Syndrome (ARDS): Presents with- tachypnea, dyspnea, retractions, hypoxia, tachycardia, crackles. “My heart is racing and I can’t catch my breath”. Asthma- Obstructive condition: presents with wheezing, increased use of accessory muscles, dyspnea, non- productive cough. TX: bronchodilators, pt education, airway clearance, breathing exercises, relaxation, endurance and strength training. Bronchiectasis-Progressive obstructive condition: presents with consistent productive cough, hemoptysis, weight loss, anemia, crackles, wheezes, and loud breath sounds. Causes: Weak bronchial walls secondary to infection that will allow permanent dilation of bronchi and bronchioles. Restrictive Pulmonary Lung Disease (RLD)- Lungs’ failure to fully expand due to a weakened diaphragm, structural inability of chest wall to expand and decrease in elasticity of lung tissue. Symptoms: SOB, persistent non-productive cough, increased respiratory rate. May be caused by progressive fibrosis and decreased lung capacity, scoliosis, kyphosis, atelectasis, pneumonia, pneumothorax, and adult respiratory distress syndrome. Results in decrease in all lung volumes. Obesity can also be a cause. TX: treat the etiology. Tuberculosis (TB)- Bacterial infection transmitted in airborne fashion. Lungs are primarily involved, but can also involve kidneys, lymph nodes, and meninges. Lesion in lungs seen in x-ray. Symptoms: fatigue, weight loss, loss of appetite, low-grade fever, productive cough, chest discomfort, and dyspnea. TX: antituberculosis drug therapy. Tests and Measures Chronic Obstructive Pulmonary Disease (COPD): Increased resistance of air passage into and out of lungs due to narrowing of bronchial tree. Symptoms: dyspnea, chronic productive cough, excessive mucus production. Progressive disease that includes alveolar destruction and subsequent increase in air that remains in lungs. Pt will have increase in Total Lung Capacity and increase in Residual Volume. Types of COPD: Chronic Bronchitis, emphysema, asthma and bronchiectasis. Pt needs to make lifestyle modifications such as smoking cessation, flu shots, avoiding irritants, good nutrition and pulmonary rehab. Cor Pulmonale (Pulmonary Heart Disease)- Considered a medical emergency. Sudden dilation of rt ventricle of heart due to pulmonary embolism. Symptoms resemble CHF. Emphysema- Develops from long history of bronchitis. Alveoli are permanently inflated. Difficulty with expiration, usually in lower lobes. Known as “pink puffer”. Pt may present with barrel chest, orthopnea, chronic cough, dyspnea and increased respiratory rate. TX: same as COPD. Pneumonia- Inflammation of lungs. Viral or Bacterial. TX: pharmacology plus rest and drink plenty of fluids. Pulmonary Edema- Collection of fluid in alveoli within lungs making it difficult to breathe. Medical emergency. Symptoms: SOB, profuse sweating, bubbly, wheezing or gasping sound during breathing, frothy sputum cough, cyanotic skin color, rapid irregular pulse, drop in BP. 1. Breath Sounds 2. Voice Sounds 3. Pulmonary Function Test 4. Pulmonary Function Reference Value 5. Arterial Blood Gas Goals of Physical Therapy 1. Maximize Independence in secretion clearance 2. Maximize self-care skills 3. Maximize functional ability skills 4. Maximize aerobic capacity 5. Maximize independence with performing and monitoring HEP 6. Maximize pt/caregiver competence with energy conservation techniques, breathing techniques, and stress management techniques. Contraindications to Postural Drainage Positions 1. For the Trendelenberg position: Any neurological conditions such as recent neurosurgery, increased intracranial pressure, headaches, aneurysm precautions. Circulatory issues such as pulmonary edema, CHF, recent MI, unstable arrhythmias, hypertension, unstable BP. Abdominal reasons include obesity, large abdominal mass, distention, pregnancy, hiatal hernia. 2. For the side lying position: Fx with fixation of humerus, flail chest, axillo-femoral bypass graft.