Bowel Elimination Study Guide
advertisement
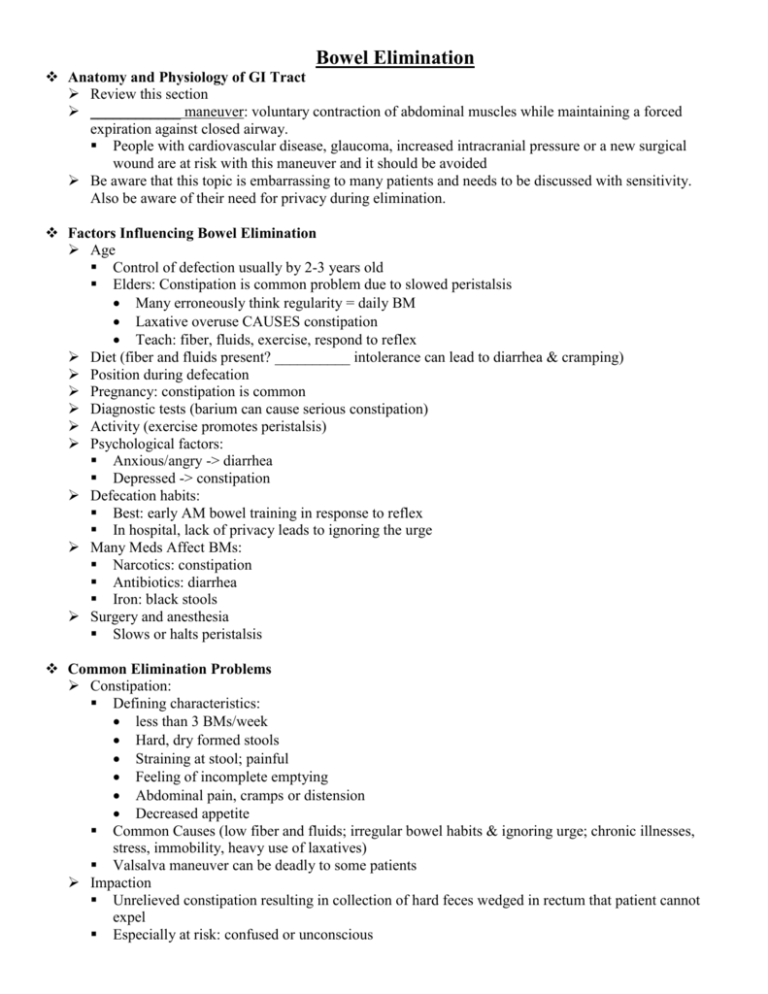
Bowel Elimination Anatomy and Physiology of GI Tract Review this section ____________ maneuver: voluntary contraction of abdominal muscles while maintaining a forced expiration against closed airway. People with cardiovascular disease, glaucoma, increased intracranial pressure or a new surgical wound are at risk with this maneuver and it should be avoided Be aware that this topic is embarrassing to many patients and needs to be discussed with sensitivity. Also be aware of their need for privacy during elimination. Factors Influencing Bowel Elimination Age Control of defection usually by 2-3 years old Elders: Constipation is common problem due to slowed peristalsis Many erroneously think regularity = daily BM Laxative overuse CAUSES constipation Teach: fiber, fluids, exercise, respond to reflex Diet (fiber and fluids present? __________ intolerance can lead to diarrhea & cramping) Position during defecation Pregnancy: constipation is common Diagnostic tests (barium can cause serious constipation) Activity (exercise promotes peristalsis) Psychological factors: Anxious/angry -> diarrhea Depressed -> constipation Defecation habits: Best: early AM bowel training in response to reflex In hospital, lack of privacy leads to ignoring the urge Many Meds Affect BMs: Narcotics: constipation Antibiotics: diarrhea Iron: black stools Surgery and anesthesia Slows or halts peristalsis Common Elimination Problems Constipation: Defining characteristics: less than 3 BMs/week Hard, dry formed stools Straining at stool; painful Feeling of incomplete emptying Abdominal pain, cramps or distension Decreased appetite Common Causes (low fiber and fluids; irregular bowel habits & ignoring urge; chronic illnesses, stress, immobility, heavy use of laxatives) Valsalva maneuver can be deadly to some patients Impaction Unrelieved constipation resulting in collection of hard feces wedged in rectum that patient cannot expel Especially at risk: confused or unconscious Signs: inability to pass stool for several days; continuous oozing of diarrhea stool; anorexia, abdominal distension, nausea, vomiting Diarrhea: increased frequency of loose stools Common causes: stress, infection, allergies, food intolerance, tube feedings, meds Rapid movement of contents so less water is absorbed; Can cause serious fluid and electrolyte imbalances, especially in elderly and children Acidity causes skin breakdown in anal region First aim of treatment is to maintain hydration Incontinence Inability to control passage of feces or flatus Treatment is based on cause Can lead to social isolation, change in body image Flatulence 3 sources: Action of bacteria on chyme in lg intestine Swallowed air Gas that diffuses b/t bloodstream and intestine Causes: foods, surgery, narcotics Can be severe causing abdominal distension and sharp pain Hemorrhoids Mass of dilated blood vessels beneath skin of anus Causes: Straining, pregnancy, chronic disease like CHF and liver disease Passage of hard stool causes bleeding, itching and burning Bowel diversions Ostomies Ileostomy (ileum) Frequent liquid stools Acidic Colostomy (colon) Stool at regular intervals Depends on location and condition 3 types Loop, end, double barrel Nursing Assessment History Usual pattern Usual characteristics of stool Specific routines to promote elimination Use of laxatives, enemas Presence of ostomies? Change in appetite Diet history Daily fluid intake History of illnesses, surgeries or meds Emotional state Exercise Any pain or discomfort? Any assistance required? Physical Exam Oral cavity & chewing Mobility: any need for assistance? Abdomen: observe, auscultate, palpate Stool characteristics Diagnostic Studies (see tutorials) Fecal Occult Blood Test (Hemoccult)– a screening tool Colonoscopy, Endoscopy, X-ray with contrast Barium Enema Stool specimens: Occult blood (Hemoccult); “positive” = blood present Stool Culture Ova and Parasites (O&P) Serum chemistry panel (“Chem 7”): If diarrhea, check electrolytes Nursing Diagnoses Bowel Incontinence Constipation Risk for Constipation Diarrhea Toileting Self Care Deficit Important to establish correct “related to” factor in order to select appropriate interventions Planning: Goals Maintain or restore normal bowel elimination pattern Maintain or regain normal stool consistency Prevent associated risks such as fluid/volume imbalance, skin breakdown, abdominal distension, pain Nursing Interventions Nutrition/Fluids If Constipation: increase fiber, fluids, prune juice If Diarrhea: fluids, small amts bland food, avoid spice, dairy products, fried foods If Flatulence: avoid gas producing foods (or increase slowly), carbonated fluids, straws, chewing gum Exercise Timing and Privacy Promote normal defecation with positioning and paying attention to defecation reflex If on bedpan raise HOB to __________________ Teach about side effects of meds Especially narcotics Monitor: Always ask “when was your last BM?” Bowel Training (for chronic constipation) Involves setting up a normal routine with measures to promote defection to gain control of reflexes For 2-3 weeks: Admin suppository 30 mins before designated time When feel urge, assist to toilet Provide privacy; allow 20-30 mins Teach: Lean forward, bear down, pressure on abdomen Medications R/T Bowel Elimination Bulk-forming: Ex: Psyllium (Metamucil) Combines with water in intestinal contents to promote peristalsis Safe to use daily; can be used for chronic constipation or watery diarrhea take with plenty of water, works in 1-3 days Stool softeners: (safe to use daily) Ex: Docusate sodium (Colace): PO prevents constipation by promoting incorporation of water into stool; works in 24-48 hrs Can also be used as rectal enema for impaction Enemas (Ex: water or Fleet’s Enema) Often used for impactions Phosphat/biphosphate (Fleet’s enema): onset 2-5 minutes Used to treat constipation or as bowel prep Laxatives: (only for short term therapy) Stimulant: Ex: Bisacodyl (Dulcolax) Treats constipation by stimulating peristalsis by altering fluid/electrolyte transport into colon PO: Onset 6-12 hours; Suppositories 15-60 minutes Osmotic: Ex: Milk of Magnesia (MOM) PO Magnesium salts osmotically draw water into intestine, distends bowel, stimulates peristalsis in 3-6 hours Polyethylene glycol (Miralax) PO powder to dissolve in 8 oz of water; works in 2-4 days; may be used up to 2 weeks Polyethylene glycol/electrolyte (GoLYTLELY) Used for bowel cleansing in prep for GI procedures; PO; onset 1 hr Pt should fast 3-4 hrs prior to administration and only have clear liquids after administration Anti-diarrheals Loperamide (Imodium): inhibits peristalsis and prolongs transit time by direct effect on nerves in intestinal wall Adults: 4mg PO initially then 2mg after each loose stool; can be used up to 10 days up to max daily dose Bismuth subsalicylate (Pepto-Bismol): promotes intestinal absorption of fluids, contains aspirin; may turn stools black; contraindicated in patients with impaction Psyllium (Metamucil): absorbs excess liquid Antiflatulent Simethicone: coalesces gas bubbles and facilitates passage Evaluation Evaluate success of interventions Did you meet patient’s expectations? Optimally patient should be able to eliminate soft formed stools regularly Patient should have information to establish normal pattern