File
advertisement

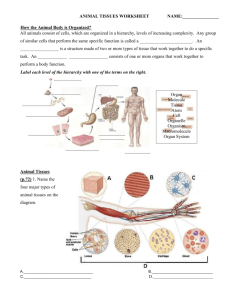
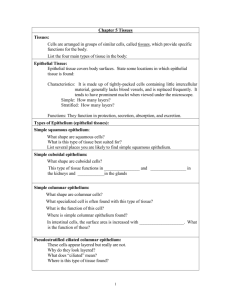
ANIMAL TISSUES Defn. TISSUE refers to a group of cells with similar structure and function plus the extracellular substances located between the cells. EPITHELIAL TISSUE Covers surfaces of the body (including skin outside the body and lining of cavities inside the body) or forms glands. Consists almost entirely of cells that have very little extracellular material between them. Have a free surface (part of which is not in contact with other cells), a basement membrane (which attaches the epithelial cells to underlying tissues), and, does not have blood vessels, (so gases and materials that reach the epithelium must diffuse across the basement membrane from the underlying tissue). The basement membrane is a mixture of carbohydrates and proteins secreted by epithelial cells and cells of the underlying tissue. A. Functions of the Epithelium 1. covering 3. absorption 2. protection 4. filtration 5. secretion B. Classification of the Epithelium I. According to the Number of Cell Layers 1. Simple epithelium – consists of a single layer of cells. 2. Stratified epithelium – consists of more than one layer of cells. 3. Pseudostratified epithelium – consists of one layer of cells but appears otherwise. 4. Transitional epithelium – special type of stratified epithelium that can be greatly stretched. II. According to the Shape of the Cells 1. Squamous epithelium 2. Cuboidal epithelium 3. Columnar epithelium Simple Squamous Epithelium Location: Lining of blood vessels, heart, lymph vessels, serous membranes, alveoli (air sacs) of lungs, and kidney tubules (Bowman’s capsule, thin segment of the loop of Henle). Structure: Single layer of thin, flat often hexagonal cells. Function: Diffusion, filtration, and protection against friction (secrete serous fluid). Simple Cuboidal Epithelium Location: Kidney tubules, glands and their ducts, choroids plexus of the brain, terminal bronchioles of lings, and surface of the ovaries and retina. Structure: Single layer of cube-shaped cells; some cells have microvilli (kidney tubules) or cilia (terminal bronchioles of lungs). The cells have a greater volume than simple squamous cells and contain more cell organelles. The organelles of cells produce carrier molecules and ATPs that control the movement of materials in and/or out of the cells by active transport and facilitated diffusion. Function: Secretion and absorption by cells of the kidney tubules; secretion by cells of glands and the choroids plexus; movement of mucus-containing particles out of the terminal bronchioles by ciliated cells. Simple Columnar Epithelium Location: Stomach, intestines, glands, some ducts, bronchioles of lungs, auditory tubes, uterus, and uterine tubes. Structure: Single layer of tall, narrow cells, some have microvilli (stomach, intestines, and glands) or cilia (bronchioles of lungs, auditory tubes, uterus, and uterine tubes) Function: Secretion of cells of the stomach, intestines, and glands; absorption by cells of the intestine; movement of mucus by ciliated cells clears the lungs and is partially responsible for the movement of the egg (ovum) through the uterine tubes. Page 1 of 8 Stratified Squamous Epithelium Location: Skin, mouth, throat, esophagus, anus, vagina, and cornea. Structure: Many layers of cells in which the basal layer is cuboidal and becomes flattened at the free surface. Function: Protection against abrasion and infection. Pseudostratified Epithelium Location: Nasal cavity, nasal sinuses, auditory tubes, pharynx, larynx, trachea, and bronchi of lungs. Structure: Single layer of cells. Some cells are tall and thin and reach the free surface, and others do not. The nuclei of these cells are at different levels and appear stratified. The cells are almost always ciliated and are associated with goblet cells which produce mucus. Function: Movement of mucus (or fluid) that contains foreign particles. Transitional Epithelium Location: Urinary bladder, ureters, and superior urethra. Structure: Stratified cells that appear cube-like when the organ or tube is relaxed and appear squamous when the organ or tube is distended by fluid. Function: Accommodation of fluid fluctuation in an organ or tube; protection against the caustic effects of urine. C. Functional Characteristics I. Cell Layers and Cell Shapes 1. Simple epithelium, with its single layer of cells, is found in organs where the principal functions are diffusion, filtration, secretion, or absorption. The movement of materials through a stratified epithelium would be hindered by its many layers. 2. Stratified epithelium is well adapted for a protective function. 3. Cells involved in diffusion are normally flat and thin. 4. Cells with the major function of secretion or absorption are usually cuboidal or columnar. Their greater size enables them to contain the organelles responsible for their function. II. Free Cell Surfaces The characteristics of the free surface reflect the functions performed by the free surface. 1. Smooth surfaces reduce friction. 2. Microvilli are found on the free surface of cells involved in absorption or secretion. 3. Cilia on free surfaces propel materials along the surface of cells. (Goblet cells are specialized mucusproducing cells.) III. Cell Connections 1.Tight junctions – bind adjacent cells together and form permeability barriers; are found in the lining of intestines. 2. Desmosomes – are mechanical links that function to bind cells together. Many are found in epithelia subjected to stress (e.g. skin). 3. Gap junctions – are small channels that allow materials to pass from one epithelial cell to an adjacent epithelial cell. Page 2 of 8 Glands – are single cell or multicellular structure that secretes substances onto a surface, into a cavity, or into the blood. Most glands are composed primarily of epithelium. Glands Endocrine Glands (Ductless Glands) Examples: Thyroid glands Adrenal glands Exocrine glands (Glands with ducts) Examples: Sweat glands Salivary glands Compound Simple Tubular Alveolar Tubular (Acinar) Alveolar (Acinar) CONNECTIVE TISSUES A. Functions of the Connective Tissue 1. Join together cells and other tissues 2. Provides a supporting framework for the body. 3. Transports substances (e.g. blood) B. Characteristics I. Characterized by a large amount of extracellular matrix that separates cells from each other. 3 Major Components of the Extracellular Matrix 1. Protein fibers 2. Ground substance consisting of non-fibrous protein and other molecules. 3. Fluid. II. Connective tissue cells are named according to their functions. 1. Blast cells produce the matrix. Example: fibroblast, osteoclast. 2. Cyte cells maintain it. Example: fibrocyte, osteocyte. 3. Clast cells break it down for remodeling. Example: fibroclast, osteoclast. III. Cells associated with the immune system are also found in the connective tissue. 1. Macrophages – are large cells capable of moving about and ingesting foreign substances, including microorganisms that are 2. found in the connective tissue. Mast cells – are non-motile cells that release chemicals promoting inflammation. Page 3 of 8 C. Classification The nature of the extracellular matrix determines the functional characteristics of the connective tissue and is used as a means of classifying the connective tissue. I. Matrix with protein fibers as the primary feature. 1. Dense connective tissue 2. Loose or areolar connective tissue – “loose packing” material of the body, which fills the spaces between organs and holds them in place. 3. Adipose tissue – has matrix with protein fibers; it is not a typical connective tissue. II. Matrix with both protein fibers and ground substance 1. Cartilage – is composed of cartilage cells or chrondrocytes, located in spaces called lacunae. Collagen in the matrix gives cartilage strength, and the ground substance of the matrix traps water, which enables the cartilage to spring back after being compressed. Cartilage heals slowly after an injury because blood vessels do not penetrate the cartilage. Types of Cartilage a. Hyaline cartilage – functions to cover the ends of bones where bones come together to form joints; provide a smooth, resilient surface that can withstand compression; and, forms the costal cartilages, which attach ribs to the sternum (breast bone). b. Fibrocartilage – functions, in addition to withstanding compression, to resist pulling or tearing force. Located or are found in the disks between vertebrae. c. Elastic cartilage 2. Bone – is a hard connective tissue that consists of living cells and a mineralized matrix. Bone cells are known as osteocytes. Types of Bones a. Compact bone – is mostly solid matrix and cells with few spaces. b. Cancellous bone – has many spaces within a lacy network of bone. 3. Fluid matrix Dense Connective Tissue Location: Tendons (attach muscle to bone), ligaments (attach bone to another bone), fasciae (hold muscle in a bundle), dermis of the skin, and organ capsule. Structure: Matrix consists almost entirely of collagen fibers produced by the fibroblasts. The fibers can all be oriented in the same direction (tendons, fasciae and ligaments), or in many different directions (dermis and capsules). Function: Able to withstand great pulling forces in the direction of the fiber orientation. Loose or Areolar Connective Tissue Location: Widely distributed throughout the body, it is the substance on which most epithelial tissue rests. It is the packing between glands, muscles, and nerves and attaches the skin (dermis) to underlying tissues. Structure: Cells (fibroblasts, macrophages, and mast) within a fine network of mostly collagen fibers; the cells and fibers are separated from each other by fluidfilled spaces. Function: Loose packing, support, and nourishment for the structures with which it is associated. Adipose Tissue Location: Under the skin, around organs such as the heart and kidneys, in the breasts, and in bones. Structure: Little extracellular material between adipose cells; the cells are so full of lipids that the cytoplasm is pushed to the periphery of the cell. Function: Energy storage, packing material that provides protection, and heat insulator. Cartilage Location: Hyaline cartilage is found in the costal cartilages of ribs, cartilage rings of the respiratory tract, nasal cartilages, covering the ends of bones, growth (epiphyseal) plates of bones, and the embryonic skeleton. Fibrocartilage is found in intervertebral disks, symphysis pubis, and articular disks (menisci of knees). Elastic cartilage is found in the external ear. Structure: Solid matrix with fibers dispersed throughout the ground substance. Chondrocytes are found within lacunae. Function: Hyaline cartilage forms a smooth surface in joints, a site of bone growth, and the embryonic skeleton. Fibrocartilage can withstand great pressure, and elastic cartilage returns to original shape when bent. Page 4 of 8 Bone Tissue Location: Bone or skeleton. Structure: Hard, mineralized matrix with osteocytes located within lacunae. Function: Provides great strength and support and protects internal organs such as the brain. Blood Location: Within the blood vessels and heart. Structure: Blood cells within a fluid matrix called plasma. Function: Transports oxygen, carbon dioxide, hormones, nutrients, waste products, and other substances; protects the body from infection and is involved in temperature regulation. NERVOUS TISSUES Forms the brain, spinal cord, and nerves. Functions: responsible for coordinating and controlling many of the body’s activities; awareness of ourselves and the external environment; emotions; reasoning skills; memory; etc. (Note: many of these functions depend upon the ability of the nervous tissues to communicate with each other by electrical signals called action potentials.) Nervous tissue consists of neurons, which are responsible for the action potential conduction, and support cells. 3 Parts of the Neuron (or Nerve Cell) 1. Cell body contains the nucleus and is the site of general cell functions. 2. Cell processes a. Dendrites – nerve cell processes which usually receive action potentials and conduct them toward the cell body. b. Axon – nerve cell processes (extensions) which usually conducts action potentials away from the cell body and there is only one axon per neuron. 3. Neuroglia – are the support cells of the nervous system, and they function to nourish, protect, and insulate the neurons. 3 Types of Neurons 1. Afferent or Sensory Neuron – the type of neuron that carries signals about the changing conditions into the integrating centers such as the central nervous system (CNS). 2. Efferent or Motor Neuron – the type of neuron that carries signals away from a body part or region, as from the brain or spinal cord (or CNS) to muscles or glands. 3. Associated Neuron – conducts impulses within the central nervous system. Cell Type NEURON Multipolar Bipolar Unipolar Description Several dendrites and one axon One dendrite and one axon A single process, which function as an axon and a dendrite. Function Most motor neurons Found in special sense organs such as the eyes and nose Most sensory neurons NEUROGLIA Astrocytes Star shaped Ependymal cells Epithelia-like Microglia Small mobile cells Oligodendrocytes Cell with several cell processes Single cells wrapped around axons Schwann cells Provide structural support; form a layer around blood vessels, contribute to bloodbrain barrier. Line ventricles of brain; form choroids plexuses , which produce cerebrospinal fluid. Protect the CNS from infection; become phagocytic in response to inflammation. Cell processes from myelin sheaths around Axons in the CNS. Form myelin sheaths around axons in the Peripheral nervous system (PNS) Page 5 of 8 MUSCLE TISSUE The main characteristic is its ability to contract or shorten, making movements possible. Muscle contraction is due to contractile proteins found inside muscle cells. The length of muscle cells is greater than their diameter. Muscle cells are called muscle fibers because they often resemble tiny threads. There are 3 type of muscle tissue: skeletal or striated or voluntary muscle tissue, cardiac muscle tissue, and visceral or smooth or involuntary muscle tissue. Skeletal Muscle Is what normally is thought of as “muscle”; it is the meat of animals and comprises about 40% of a person’s body weight. Attaches to the skeleton and causes body movements. Normally under voluntary (conscious) control. The skeletal muscle cells tend to be long, cylindrical cells with several nuclei per cell. Some cells extend the length of an entire muscle. The cells are striated or banded because of the arrangement of contractile proteins within the cells. Cardiac Muscle Is the muscle of the heart and is responsible for pumping blood. Is under involuntary (unconscious) control. Cardiac muscle cells are cylindrical in shape but are much shorter in length than skeletal muscle cells. They are also striated with one nucleus per cell and they often are branched and connected to each other by intercalated disks. The intercalated disks are important in coordinating the contractions of the cardiac muscle cells. Is dually innervated. Smooth Muscle Forms the walls of hollow organs (except the heart), and also is found in the skin and the eyes. Is responsible for a number of functions such as movement of food through the digestive tract and emptying of the urinary bladder. Is under involuntary control and is associated with the internal organs. Smooth muscle cells are tapered at each end and have a single nucleus and are not striated. MEMBRANES Definition: A thin sheet or layer of tissue that covers a structure or lines a cavity. Composition: Consist of epithelium and the connective tissue on which the epithelium rests. 2 Major Categories of Membranes 1. Mucous Membranes Consists of various kinds of epithelium resting on a thick layer of loose connective tissue. Line cavities that open to the outside of the body such as the digestive, respiratory, excretory, and reproductive tracts. Many, but not all, have mucous glands which secrete mucus. The functions vary depending on their location and include protection, absorption and secretion. 2. Serous Membranes Consist of simple squamous epithelium resting on a delicate layer of loose connective tissue. Line the trunk cavities and covers the organs located within the trunk cavities. Secrete serous fluid, which covers the surface of the membranes. The smooth surface of the epithelial cells of the serous membranes, and the lubricating qualities of the serous fluid, combine to prevent damage from abrasion when organs in the thoracic or abdominopelvic cavities rub against each other. Are named according to their location. a. Pleural membranes – associated with the lungs. b. Pericardial membranes – associated with the heart. c. Peritoneal membranes – are located in the abdominopelvic cavity. Other Membranes 1. Skin or cutaneous membrane – is stratified squamous epithelium and dense connective tissue. 2. Synovial membranes – line the inside of joint cavities (the space where bones come together within a movable joint) 3. Periosteum – surrounds the bone. (Note: The synovial membranes and the Periosteum are membranes made up of only connective tissue.) Page 6 of 8 INFLAMMATION The inflammatory response, or inflammation, occurs when tissues are damaged. It mobilizes the body’s defenses, isolates and destroys microorganisms, and removes foreign materials and damaged cells so that tissue repair can proceed. Inflammation produces five major symptoms: redness, heat, swelling, pain, and disturbance of function. Although unpleasant, the processes producing the symptoms are usually beneficial. Following an injury, chemical substances called mediators of inflammation are released and activated in the injured tissues and adjacent blood vessels. The mediators include histamine, kinins, prostaglandins, leukotrienes, and others. Some mediators cause vasodilation (expansion of blood vessels). This produces the symptoms of redness and heat, as occur when a person blushes. Vasodilation is beneficial because it increases the speed with which blood cells and other substances important for fighting infections and repairing the injury are brought to the injury site. Mediators of inflammation also increase the permeability of blood vessels, allowing materials and blood cells to move out of the vessels and into the tissue where they can deal directly with the injury. Edema, or swelling, of the tissues results when proteins and water from the blood move into the tissues. One of the proteins, fibrin, diffuses into the tissue and forms a fibrous network that “walls off” the site of injury from the rest of the body. This can help to prevent the spread of infectious agents. One type of blood cell that enters the tissues is neutrophils, phagocytic white blood cells that fight infections by ingesting bacteria. They also ingest tissue debris, clearing the area for tissue repair. Neutrophils are killed in this process and can accumulate as a mixture of dead cells and fluid, called pus. Pain associated with inflammation is produced in several ways. Nerve cell endings are stimulated by direct damage and by some mediators of inflammation to produce pain sensations. In addition, the increased pressure in the tissue caused by edema and accumulation of pus can cause pain. Pain, limitation of movement resulting from edema, and tissue destruction all contribute to the disturbance of function. This disturbance of function can be adaptive because it warns the person to protect the injured area from further damage. Sometimes the inflammatory response lasts longer or is more intense than is desirable, and drugs are used to suppress the symptoms by inhibiting the mediators of inflammation. For example, the effects of histamines released in hay fever are suppressed by antihistamines. Aspirin is an effective anti-inflammatory agent and relieves pain by preventing the synthesis of prostaglandins. TISSUE REPAIR Tissue repair is the substitution of viable cells for dead cells and it can occur by regeneration or replacement. In regeneration, the new cells are the same type as those that were destroyed, and normal function is usually restored. In replacement, a new type of tissue develops that eventually causes scar production and the loss of some tissue function. The tissues involved the nature of the wound determine the type of tissue repair that dominates. Cells can be classified into three groups based on their ability to divide and produce new cells. Labile cells (for example, the skin and mucous membranes) continue to divide throughout life. Damage to these cells can be repaired completely by regeneration. Stable cells (for example, connective tissue and glands, including the liver and pancreas) do not actively replicate after growth ceases. They also retain the ability to divide after an injury and are capable of regeneration. Permanent cells (for example, neurons and skeletal muscle cells) cannot undergo mitosis and divide. If they are killed, they usually are replaced by connective tissue. This does not mean permanent cells can’t recover from limited amount of damage. For example, if the axon of a neuron is damaged, it is possible for the neuron to grow a new axon. In addition to the type of cells involved, the severity of an injury can influence whether repair is by regeneration or replacement. Given that a tissue can repair by regeneration, if the injury is severe some of the tissue may be repaired by replacement. Generally, the more severe the injury, the greater the likelihood that repair involves replacement. If the edges of the wound are close together, the wound heals primarily by regeneration, and the process is called primary union. If the edges are not close together, or if there has been extensive tissue loss, the wound heals by regeneration and replacement, and the process is called secondary union Page 7 of 8 Repair of the skin can be used to illustrate tissue repair. In primary union, the wound fills with blood and a clot forms. The clot contains a threadlike protein, fibrin, which binds the edges of the wound together and stops any bleeding. The surface of the clot dries to form a scab, which seals the wound and helps to prevent infection. An inflammatory response is activated to fight infectious agents in the wound and to help the repair process. Vasodilation (increased blood vessel diameter) brings blood cells and other substances to the injury area, and increased blood vessel permeability allows them to enter the tissue. The area is “walled off” by the fibrin, and neutrophils enter the tissue from the blood. While the inflammatory response proceeds, the epithelium at the edge of the wound undergoes regeneration and migrates under the scab. After a few days, the epithelial cells from the edges meet, and eventually the epithelium is restored. After the epithelium is repaired, the scab is sloughed off (shed). Meanwhile, a second type of phagocytic cell, called a macrophage, removes the dead neutrophils, cellular debris, and the decomposing clot. Fibroblasts from the surrounding connective tissue migrate into the area, producing collagen and other extracellular matrix components. Capillaries grow from blood vessels at the edge of the wound and revascularize the area. The result is the replacement of the clot by a delicate connective tissue called granulation tissue, which consists of fibroblasts, collagen and capillaries. Eventually normal connective tissue replaces the granulation tissue. Sometimes a large amount of granulation tissue persists as a scar, which at first is bright red because of the vascularization of the tissue. The scar turns from red to white as collagen accumulates and the blood vessels are compressed. Repair by secondary union is similar to healing by primary union, but there are some differences. Because the wound edges are far apart, the clot may not completely close the gap, and the epithelial cells take much longer to regenerate and cover the wound. With increased tissue damage, the degree of the inflammatory response is greater, there is more cell debris for the phagocytes to remove, and the risk of infection is greater. Much more granulation tissue forms and wound contracture, a result of the contraction of fibroblasts in the granulation tissue, pulls the edges of the wound closer together. Although wound contracture reduces the size of the wound and speeds up healing, it can lead to disfiguring and debilitating scars. CANCER TISSUE Cancer refers to a malignant spreading tumor and the illness that results from such a tumor. A tumor is any swelling, but modern usage has limited the term to swellings that involve neoplastic tissue. Neoplasm means “new growth” and refers to abnormal tissue growth resulting from cellular division that continue after normal cell division of the tissue has stopped or slowed considerably. A neoplasm can be benign (kind), with little likelihood of spreading, or malignant (with malice or intent to cause harm), with the ability to spread. Although benign tumors are usually less dangerous than malignant tumors, they can cause problems. As the tumor enlarges it can compress surrounding tissues and impair their function. In some cases, for example brain tumor, the result can be death. Malignant tumors can spread by local growth or expansion or by metastasis (moving to another place), which occurs when tumor cells separate from the main mass and are carried by the lymphatic or circulatory system to a new site where a second neoplasm is formed. The illness associated with cancer usually occurs as the tumor invades and destroys the healthy surrounding tissue, eliminating its function. Malignant neoplasm lacks the normal growth control that most other adult tissues have. This breaking loose from normal control involves the genetic machinery and can be inducted by viruses, environmental toxins, radiation and other causes. Cancer therapy concentrates on trying to confine and then kill the malignant cells. This is accomplished by killing the tissue with radiation or lasers, by removing the tumor surgically, by treating the patient with drugs that selectively kill rapidly dividing cells (as in chemotheraphy), or stimulating the patient’s immune system to destroy the tumor. Oncology (tumor study) is the study of cancer and its associated problems. ***************** Page 8 of 8