Ch36 - Morgan Community College
advertisement

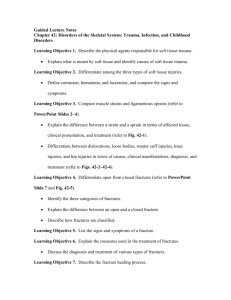
Guided Lecture Notes Chapter 36: Disorders of Brain Function Learning Objective 1. Differentiate cerebral hypoxia from cerebral ischemia and focal from global ischemia. Describe the relationship between cerebral ischemia and cerebral hypoxia (refer to PowerPoint Slides 2–6). Using examples, explain the difference between focal and global ischemia. Learning Objective 2. Characterize the role of excitatory amino acids as a common pathway for neurologic disorders. Explain how excessive activity of excitatory neurotransmitters may result in neurologic disorders (refer to PowerPoint Slide 21 and Fig. 36-1). Learning Objective 3. Compare cytotoxic, vasogenic, and interstitial cerebral edema. Define cerebral edema, and explain the difference between vasogenic and cytotoxic types in terms of causes and manifestations. Learning Objective 4. State the determinants of intracranial pressure and describe compensatory mechanisms used to prevent large changes in intracranial pressure when there are changes in brain, blood, and cerebrospinal fluid volumes. Define ICP, and identify factors that affect ICP (refer to PowerPoint Slide 7). Describe the effects of increased ICP on the brain, and explain the Monro-Kellie hypothesis of compensation. Identify the three signs (Cushing triad) that are indicators of increased ICP. Learning Objective 5. Explain the causes and consequences of tentorial herniation of the brain. Identify causes of brain herniation, and explain the difference between supratentorial and infratentorial herniation (refer to PowerPoint Slide 8). List the three major patterns of supratentorial herniation, and identify the structures involved and the clinical signs associated with each (refer to Fig. 36-2 and Table 36-1). Learning Objective 6. Compare the causes of communicating and noncommunicating hydrocephalus. Differentiate between communicating and noncommunicating hydrocephalus with regard to causes, pathologic changes, presentation, diagnosis, and treatment (refer to Fig. 36-3). Learning Objective 7. Differentiate between primary and secondary brain injuries due to head trauma. Using examples, explain the difference between primary and secondary brain injuries that occur as a result of head trauma in terms of cause, pathology, and prognosis (refer to PowerPoint Slide 9 and Figs. 36-5 and 36-6). Learning Objective 8. Describe the mechanism of brain damage in coup-contrecoup injuries. Using examples, explain the mechanism involved in coup-contrecoup brain injury (refer to Fig. 36-4). Learning Objective 9. List the constellation of symptoms involved in postconcussion syndrome. Define concussion, and list the symptoms that comprise postconcussion syndrome. Learning Objective 10. Differentiate among epidural, subdural, and intracerebral hematomas in terms of location, manifestations, and morbidity. Compare the location, pathology, and prognosis associated with epidural, subdural, and intracerebral hematomas (refer to PowerPoint Slide 12 and Figs. 36-7 and 36-8). Learning Objective 11. Define consciousness, and trace the rostral-to-caudal progression of consciousness in terms of pupillary changes, respiration, and motor function as the effects of brain dysfunction progress to involve structures in the diencephalon, midbrain, pons, and medulla. List areas of the nervous system that contribute to consciousness. Identify the signs of rostral-to-caudal progression of brain lesions (refer to Table 36-2). List the characteristics associated with various levels of consciousness, and explain how respiratory pattern, motor responses, pupillary reflexes, and eye movements are affected (refer to Table 36-3 and Fig. 36-10). Discuss the Glasgow Coma Scale as a means to assess level of consciousness (refer to Table 36-4). Learning Objective 12. State two criteria for the diagnosis of brain death. Define brain death, and identify criteria used to diagnose brain death (refer to Fig. 36-11). Learning Objective 13. List the major vessels in the cerebral circulation, and state the contribution of the internal carotid arteries, the vertebral arteries, and the circle of Willis to the cerebral circulation. Identify major cerebral blood vessels, and explain how they maintain collateral circulation in the brain (refer to PowerPoint Slides 13–17 and Figs. 36-12 and 36-13). Learning Objective 14. Describe the autoregulation of cerebral blood flow. Describe autoregulatory and local mechanisms that regulate cerebral blood flow. Learning Objective 15. Explain the substitution of “brain attack” for stroke in terms of making a case for early diagnosis and treatment. Explain the importance of early diagnosis and treatment for patients who have suffered a stroke (brain attack) in terms of recovery. Identify risk factors associated with stroke. Learning Objective 16. Differentiate the pathologies of ischemic stroke from hemorrhagic stroke. Differentiate between ischemic and hemorrhagic stroke in terms of incidence, pathology, manifestations, diagnosis, and treatment (refer to PowerPoint Slide 18). Describe how the signs and symptoms of a stroke are related to the brain area involved (refer to Table 36-5). List the five subtypes of ischemic stroke, and cite the incidence of each (refer to Fig. 36-14). Learning Objective 17. Explain the significance of transient ischemic attacks, the ischemic penumbra, and watershed zones of infarction and how these conditions relate to ischemic stroke. Describe ischemic penumbra and watershed zones of infarctions, and explain how they affect prognosis following an ischemic stroke. Characterize TIAs, and describe the risk factors for a stroke following a TIA. Learning Objective 18. Cite the most common cause of subarachnoid hemorrhage, and state the complications associated with subarachnoid hemorrhage. Describe types of aneurysms that may result in subarachnoid hemorrhage (refer to Figs. 36-16 and 36-17). Describe the causes, pathology, manifestations, diagnosis, and treatment of subarachnoid hemorrhage (refer to PowerPoint Slide 21 and Fig. 36-15). Learning Objective 19. Describe the alterations in vasculature that occur with arteriovenous malformations. Describe the causes, pathology, manifestations, diagnosis, and treatment of arteriovenous formations (refer to Fig. 36-18). Learning Objective 20. Describe the progression of motor deficits and problems with speech and language that occur as a result of stroke. Discuss stroke-related deficits that occur following the event, including motor, speech, and cognitive deficits. Learning Objective 21. List the sequence of events that occur with meningitis. Differentiate between bacterial and viral meningitis in terms of causes, pathology, manifestations, diagnosis, and treatment. Learning Objective 22. Describe the symptoms of encephalitis. Describe the causes, pathology, manifestations, diagnosis, and prognosis of encephalitis. Learning Objective 23. List the major categories of brain tumors, and interpret the meaning of benign and malignant as related to brain tumors. Discuss the incidence of brain tumors and describe various classifications, including benign (low-grade) and malignant (high-grade) (refer to PowerPoint Slide 22). Identify the three main types of brain tumors, and describe the location and pathology associated with glial tumors, ependyomas, meningiomas, and primary CNS lymphomas. Learning Objective 24. Describe the general manifestations of brain tumors. Describe the clinical manifestations of brain tumors and identify factors that determine the extent of these symptoms. Learning Objective 25. List the methods used in the diagnosis and treatment of brain tumors. Identify diagnostic procedures for brain tumors. List the three general categories for the treatment of brain tumors. Learning Objective 26. Explain the difference between a seizure and epilepsy. Define seizure and differentiate between partial and generalized seizures. Explain the classification system used to categorize epileptic seizures (refer to PowerPoint Slide 25). Learning Objective 27. State four or more causes of seizures other than epilepsy. List causes of seizures other than epilepsy (refer to Chart 36-1). Learning Objective 28. Differentiate between the origin of seizure activity in partial and generalized forms of seizures. Compare the origin of seizure activity in partial and generalized seizures (refer to PowerPoint Slide 24). Identify types of partial and generalized seizures (refer to PowerPoint Slide 24). Discuss pharmacologic and surgical treatment options for seizures. Learning Objective 29. Characterize status epilepticus. Define status epilepticus and discuss its incidence, prognosis, and treatment. Learning Objective 30. Compare the causes associated with Alzheimer disease, vascular dementia, Pick disease, Creutzfeldt-Jakob disease, Wernicke-Korsakoff syndrome, and Huntington disease. Compare various types of dementia with regard to their causes, pathology, manifestations, diagnosis, treatment, and prognosis (refer to PowerPoint Slides 28 and 32). Learning Objective 31. Describe the changes in brain tissue that occur with Alzheimer disease. Describe how brain tissue is affected in patients with Alzheimer disease (refer to PowerPoint Slides 29–31 and Fig. 36-19). Learning Objective 32. Use the three stages of Alzheimer disease to describe its progress. Categorize the progression of Alzheimer disease (refer to PowerPoint Slide 31). Learning Objective 33. Cite the difference between Wernicke disease and the Korsakoff component of Wernicke-Korsakoff syndrome. Describe both Wernicke syndrome and Korsakoff syndrome, and explain how they interact to result in Wernicke-Korsakoff syndrome (refer to PowerPoint Slide 32).