01995 (Word 97)
advertisement

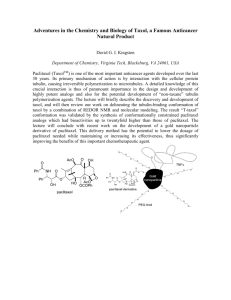
EUROPEAN LUNG CANCER WORKING PARTY PROTOCOL 01995 A PHASE III RANDOMISED TRIAL COMPARING SEQUENTIAL CHEMOTHERAPY VERSUS STANDARD CHEMOTHERAPY IN STAGE IV NON-SMALL CELL LUNG CANCER Writing Committee : J.P. SCULIER, T. BERGHMANS, J. KLASTERSKY Study Coordinator : J.P. SCULIER Data manager : P. MOMMEN Statistician : M. PAESMANS Second draft : December 1999 Activated : January 17, 2000 INDEX 1. Group 3 2. Introduction 5 3. Study objectives 9 4. 4.1 4.2 Study population Criteria of eligibility Criteria of ineligibility 9 9 9 5. Study design 10 6. 6.1 6.2 6.3 Investigations Initial investigations Evaluation during treatment Follow-up after chemotherapy 12 12 12 12 7. Treatment plan 12 8. Trial quality control 15 9. 9.1 9.2 9.3 9.4 9.5 Drug procurement, preparation and storage Cisplatin Ifosfamide Mesna Gemcitabine Paclitaxel 15 15 15 15 15 16 10. Side effects 16 11. Dose adaptation plan 17 12. Criteria of evaluation 17 13. Off treatment regimen and off study definitions and procedures 19 14. Entry and randomisation procedures 19 15. Data management and trial coordination 20 16. Ethical considerations 20 17. Statistical considerations 21 18. Publication and authorship 21 19. Bibliography 22 Appendix I Performance scale 25 Appendix II Staging classification 26 Appendix III WHO's criteria of toxicity 28 Appendix IV the World Medical Association Declaration of Helsinki 32 2 1. GROUP Participating centers and members : Belgium France Bruxelles Institut Jules Bordet J. Klastersky, J.P. Sculier, J.J. Body, M. Paesmans, P. Van Houtte, E. Markiewicz, P. Mommen, A. Awada, D. Cullus, D. Devriendt, T. Berghmans Hôpital Brugmann A. Drowart, T. Prigogine Hôpital Erasme P. Rocmans, S. Luce Hôpital St Pierre R. Sergijsels, T. Bosschaerts, V. Ninane Boussu Hôpital de Warquignies M. Richez, Charleroi Hôpital civil de Charleroi J. Thiriaux, J. Lecomte, Namur Clinique St Luc O. Van Cutsem, M. Mairesse Montignies le-Tilleul C.H.U. A. Vesale D. Brohée, I. Louviaux Ath Hôpital de la Madeleine P. Ravez Tournai IMC Mutualités Socialistes A. Tagnon, G. Nuttin Brainel'Alleud Hôpital de Braine l'Alleud C. Finet Mons C.H. de Mons P. Wackenier, P Recloux, C. Juquelier, M. Thirion Baudour Clinique Louis Caty V. Richard, D. Diana La Louvière C.H. de Tivoli J. Michel,J. Bruart, A. Renaud, A. Leleux Verviers C.H. Peltzer-La Tourelle J.L. Corhay Jumet Hôpital Civil de Jumet A. Wattiez Douai C.H. de Douai M.C. Florin, E. Maetz, A. Strecker Centre Pasteur M. Guiselin Hayange Hôpital d'Hayange M.C. Berchier Roubaix C.H. de Roubaix F. Kroll, F. Steenhouwer 3 Lille Clinique de la Louvière F. Fortin, J.M. Dernis, J.M. Grosbois Hôpital A. Calmette J.J. Lafitte Polyclinique de H-B R. Roboubi Centre Oscar Lambert B. Prévost Anzin Cabinet Médical Dampierre B. Stach, J.P. Roux Montfermeil C.H.I. de Montfermeil C. Zacharias Metz Centre Hospitalier Régional de Metz-Thionville E. Barthelmé Valenciennes Clinique Médico-Chirurgicale Teissier Hôpital de Valenciennes G. Demarcq Boulogne s/Mer Hôpital Duchenne J.L. Crépin Tourcoing Centre Hospitalier de Tourcoing X. Ficheroulle Cabinet de Pneumo-Allergologie J.L. Duriez Cabinet de Pneumologie Y. Watrigant Henin Beaumont Marcq en Baroeul Cabinet Médical des Flandres M.L. Line P. Coleaux E. Mensier Lens Centre Hospitalier du Dr Schaffner J. Amourette Arras Centre Hospitalier d’Arras J.F. Bervar, F. Herengt Y. Lierman Italy Padoue Registro Tumori del Vento L. Simonato Spain Valence Hospital de Sagunto V. Giner Marco A. Galan Brotons Greece Athènes Hellenic Cancer Institute A. Efremidis, G. Koumakis Evangelismos General C.G. Alexopoulos, M. Vaslamatzis Hospital Hungary Czech Republic Prague Brno Slovak Republic Kosice National Koranyi Institute J. Moldvay Charles University Medical Faculty L. Petruzelka Institut Masaryk d'Oncologie H. Coupkova Klinika radiotherapie a onkologie J. Baumöhl 4 2. INTRODUCTION Cisplatin is a main drug in the management of patients with advanced non-small cell lung cancer (NSCLC). Its introduction in chemotherapy regimens has allowed to obtain survival improvement in stage IV disease in comparison to best supportive care and in stage III disease by neoadjuvant applications in comparison to surgery and/or chest irradiation alone (1-4). High-doses cisplatin induces however significant toxicity, consisting particularly in increased emesis, polyneuropathy, hypoacousia and renal function impairment. This poor tolerance avoids giving prolonged administration of the drug in a lot of patients. An association between moderate doses of cisplatin and carboplatin can prevent this long-term limiting renal, auditive and neurological toxicity. Respectively 60 mg/m2 and 200 mg/m2 dosages are as effective in term of response rate and survival as 120 mg/m2 of cisplatin alone and reduces from 26 % to 6 % the occurrence of a grade II to IV of long-term toxicity during the overall therapy (5). In a recently analysed randomised trial of our Group, we compared in stage IV NSCLC, the combination of moderate dosages of cisplatin (60 mg/m²) and carboplatin (200 mg/m²) -CarboMIP regimen- to a regimen with low dose cisplatin (50 mg/m²) alone -MIP regimen- in association with mitomycin (6 mg/m²) and ifosfamide (3g/m²). A total of 305 patients with no prior chemotherapy were randomised, including 297 patients assessable for survival (147 in the MIP arm and 150 in the CarboMIP arm) and 168 patients assessable for response to chemotherapy. All but 8 (with malignant pleural effusion) had stage IV disease. There was a 27% (95% confidence interval [CI], 19-34) objective response (OR) rate to MIP (25% of eligible patients) and a 33% (95% CI, 24-41) OR rate to CarboMIP (29% of the eligible patients). This difference was not statistically significant (p=0.34). Duration of response was not significantly different between the arms. There was also no difference (p= 0.67) in survival: median survival times were 28 weeks (95% CI, 24-32) for MIP and 32 weeks (95% CI, 26-35) for CarboMIP with respectively 1-year survival rates of 24% and 23% and 2-year survival rates of 5 and 2%. Our trial fails to demonstrate a significant improvement in response or survival when patients with metastatic NSCLC are treated, in addition to ifosfamide and mitomycin, by combination of moderate dosages of cisplatin and carboplatin instead of moderate dosage cisplatin alone. The results support the use of a moderate dose (50 mg/m²) of cisplatin for the chemotherapy of this disease. Other active drugs against NSCLC, that are today commercially available, include vindesine, vinblastine, mitomycin C and ifosfamide (6) and, more recently, include gemcitabine, paclitaxel, vinorelbine, docetaxel (7). Although probable, it is so far not demonstrated that combination chemotherapy improves survival in advanced NSCLC by comparison to cisplatin alone. One ELCWP randomised trial conducted in stage IV NSCLC had as primary purpose to demonstrate this point by adding ifosfamide to the cisplatin-carboplatin combination. The regimen with ifosfamide resulted in a significantly much higher response rate (31 % vs 16 %) but without improvement of survival (8). Our current trial in this patients population has as purpose to determine if the combination of gemcitabine with ifosfamide or with the cisplatin-carboplatin association will improve the survival obtained by our standard regimen cisplatin-carboplatin-ifosfamide. Gemcitabine appears to be particularly promising because of its relatively better tolerance. It has a close resemblance to cytosine-arabinoside (AraC), acting as a pyrimidine antimetabolite (9). It was initially synthesised as an antiviral drug. When administered in a once weekly three times every 4 weeks schedule (10), dose-limiting toxicity appeared to be myelosuppression, with thrombocytopenia and anaemia quantitatively more important than granulocytopenia. Non haematological toxicity was minimal or rare: rash, vomiting, nausea, fever, "flu-like" syndrome, 5 peripheral oedema, and respiratory failure. Gemcitabine has been combined with various other cytostatic agents including cisplatin, carboplatin and ifosfamide. Experimental data support a synergistic interaction between cisplatin and gemcitabine in vitro (11), by incorporation of the drug into DNA and/or CDDP-DNA adduct formation. Regimens combining gemcitabine with cisplatin (12) or ifosfamide (13) have been shown active. The three drugs have combined, leading to the GIP regimen (14). Four phase I-II studies performed in advanced NSCLC have been reported in abstracts. Two of them (14) recommend as dosage for cisplatin 50 mg/m² (d1), for ifosfamide 3 g/m² (d1) and for gemcitabine 1 g/m² d1 + 8. The reported response rates averaged 50% and these studies established that the recommended doses could be delivered fully. A new concept, the sequential approach, has emerged and has been discussed at the First World Conference on Clinical Cooperative Research for Lung Cancer that the ELCWP organised in Brussels in March 1999. The idea is treat the patients by consecutive non-cross resistant chemotherapy regimens. Practically, a first combination would be cisplatin-based and a second one taxane-based. Paclitaxel (Taxol) has been shown active in NSCLC (15-22) when administered as single agent (table I) and has been the object of combination therapy studies with drugs like cisplatin or carboplatin. In monotherapy (15-22), in patients with mainly stage IV disease, an objective response rate between 20 and 30% has been observed, whatever the infusion duration (1, 3 or 24h) or the administered dosage (from 136 to 250 mg/m²). The median survival time has ranged between 6 and 9 months. Moreover, in one trial (18), paclitaxel was given as second-line chemotherapy after failure of a cisplatin containing regimen and 6/16 treated patients had an objective response. It should be noted that there is so far no identified confirmed effective second-chemotherapy regimen after failure of a cisplatin-based combination. 6 Table I: Activity of paclitaxel as single agent therapy. Reference Doses (mg/m²) N pts OR (%) MS St III (n pts) OR (%) Gatzemeier, 1995 15 225 (over 3h) 43 22 ? 13 St IV OR (n pts) (%) ? 30 ? Alberola, 1995 16 210 (over 3h) 50 36 ? 23 ? 27 ? Furuse, 1997 17 210 (over 3h) 60 32 30 w 22 27 38 34 Tester, 1997 18 200 (over 3h) 20 32 6m 0 - 20 32 Milward, 1996 19 175 (over 3h) 51 10 7m 18 6 33 10 Hainsworth, 1995 20 135 or 200 (over 1h) 59 25 8m 6 ? 53 ? Chang, 1993 21 250 (over 24h) 24 21 24 w 0 - 24 21 Murphy, 1993 22 200 (over 24h) 25 24 40 w 3 ? 22 ? The purpose of the present trial is to determine if a sequential approach with the successive administration of the GIP regimen followed by paclitaxel will improve the survival obtained by GIP alone as first-line chemotherapy, using paclitaxel as salvage treatment. 3. STUDY OBJECTIVES 31. Primary endpoint to determine if a sequential approach (GIP followed by paclitaxel) will improve survival in comparison to the combination gemcitabine-ifosfamide-cisplatin alone (GIP) in patients with stage IV NSCLC. 32. Secondary endpoints - to determine the impact of each approach on the best objective response rates - to compare the toxicity of the 2 approaches - to determine the activity of paclitaxel as salvage regimen after GIP - to determine the effectiveness of erythropoietin in the control of anaemia due to cisplatin 7 4. STUDY POPULATION 4.1 Criteria of eligibility include : - Histological or cytological diagnosis of non-small cell lung cancer - Inoperable stage IV disease or stage IIIB disease with malignant pleural effusion - Availability for participating in the detailed follow-up of the protocol - Presence of an evaluable or measurable lesion - Informed consent. 4.2 Criteria of ineligibility include : - Prior treatment with chemotherapy - Performance status < 60 on the Karnofsky scale - A history of prior malignant tumour, except non-melanoma skin cancer or in situ carcinoma of the cervix and cured malignant tumour (more than 5-year disease free interval) - Polynuclear cells < 2,000/mm³ - Platelet cells < 100,000/mm³ - Serum bilirubin >1.5 mg/100 ml - Serum creatinine > 1.5 mg/100 ml and/or creatinine clearance < 60 ml/min - Perception hypoacousia - Peripheral neuropathy - Recent myocardial infarction (less than 3 months prior to date of diagnosis) - Congestive cardiac failure requiring medical therapy or uncontrolled cardiac arrhythmia - Uncontrolled infectious disease - Serious medical or psychological factors which may prevent adherence to the treatment schedule. 5. STUDY DESIGN After registration, eligible patients will be treated by 3 courses of GIP : Cisplatin Ifosfamide Gemcitabine 50 mg/m² 3 g/m² 1 g/m² d1 d1 d1+8 Courses will be repeated every 3 weeks. A complete staging will be performed after 3 courses. Non progressing patients will be randomised between 3 further courses of GIP or 3 courses of paclitaxel (225 mg/m² over 3 hours every 3 weeks). Patients will be treated until best response. Assessment of response will be done every 3 courses. Patients with no change or no further improvement of response will be off treatment. Those with progressive disease will be treated by paclitaxel if in the GIP arm or further GIP if in the paclitaxel arm. 8 Table II : STUDY PLAN STAGE IV NSCLC REGISTRATION 3 courses of GIP Cisplatin 50 mg/m² d1 Ifosfamide 3 g/m² d1 Gemcitabine 1 g/m² d1+8 Evaluation of response NO PROGRESSION PROGRESSION RANDOMISATION Paclitaxel 225 mg/m² Paclitaxel 225 mg/m² GIP progression progression GIP PROGRESSION OFF TRIAL 9 6. INVESTIGATIONS 6.1 Initial investigations: a. Clinical examination completed by weight, height, surface area and record of performance status b. Biological tests including haemoglobin, white blood cell count, differential count, platelet count; serum urea; serum creatinine, serum bilirubin, alkaline phosphatase, SGOT; LDH, calcium, uric acid, Mg, electrolytes (Na, K, Cl, HCO3) c. Chest X-ray (P.A. and lateral) and CT scan (with contrast administration in case of a central lesion taken as response target) d. Bronchoscopy with biopsy e. Electrocardiogram and cardiac echography or isotopic ejection fraction f. Bone isotopic scan g. CT Scan or echography of the liver and adrenals h. Brain CT Scan or NMR. 6.2 Evaluation during treatment: Weekly: Hb, WBC, diff, platelets, creatininemia before each new course : clinical examination, PS, weight, biological tests(cf 6.1 b.), chest Xray After the 3rd course and every 3 subsequent courses of chemotherapy: same investigations as initially 6.3 Follow-up after chemotherapy: The patient should be seen after discontinuation of therapy at least every 2 months for the first six months and thereafter every 3 months. Following investigations have to be performed : clinical examination, PS, weight, biological tests (cf 6.1.b.), chest X-ray. 7. TREATMENT PLAN Treatment will be given at the following dosages and with the suggested following policy for emesis: 7.1 GIP Time (hours) Drug Route Dosage -5 min 0 min 30 min 30 min granisetron gemcitabine mesna ifosfamide mesna iv iv iv iv iv 3h30 min 3h30 min mesna cisplatin iv iv 3 mg in 50 ml NaCl 0.9% 1 g/m² in 250 ml NaCl 0.9% 0.75g/m² in 50 ml NaCl 0.9% 3 g/m² 1.5 g/m² in the same 1l NaCl 0.9% 3 g/m2 in 1 l NaCl 0.9 % 4h30 4h30 12h30 furosemide 1 l NaCl 0.9 % + 1.5 g KCl 1 l NaCl 0.9 % + 1.5 g KCl iv iv iv 2 50 mg/m in 250 ml NaCl 3% 20 mg - Duration of infusion 5 min 30 min 5 min 3h 18 h 1h bolus 8h 8h 10 21h30 stop treatment If urine output is < 800 ml/6h, 40 mg furosemide iv should be administered. 7.2. Gemcitabine d 8 - gemcitabine 1 g /m2 over 30 min in 250 ml NaCl 0.9 % - suggested antiemetics : metoclopropamide. 7.3. Paclitaxel - suggested antihypersensitivity premedication: dexamethasone 20 mg orally 12 ,6 h and iv 30 minutes before paclitaxel administration, promethazine 50 mg im or diphenhydramine 50 mg iv and cimetidine 300 mg iv or ranitidine 50 mg iv 30 min before paclitaxel - paclitaxel : to be given over 3 hours in 500 ml NaCl 0,9% - suggested antiemetics : metoclopropamide - vital signs have to be monitored or checked during chemotherapy administration. 8. TRIAL QUALITY CONTROL Each patient record will be evaluated for evaluation and response in regular meetings of the Group. Patient’s original record and radiological documents have to be available at this time. 9. DRUG PROCUREMENT, PREPARATION AND STORAGE Each drug may have different commercial names and pharmaceutical presentations according to the country. Investigators have to get local information. 9.1. Cisplatin: * How supplied: 10 mg - 25 mg - 50 mg vials as a lyophilisate powder (PlatinolR) * Storage: the product remains stable in a cool (+ 4°C) and dark place for 18 months * Reconstitution: with sterile water (1 mg/1 ml). * Stability after reconstitution: - 1 h at light and room temperature - 8 h at dark and room temperature - in refrigerator : risk of cristallisation. * Procurement: commercially available (PlatinolR). 9.2. Ifosfamide: * How supplied: 1 g vials as a lyophilisate powder * Storage: at room temperature and protected from light * Reconstitution: with sterile water * Stability after reconstitution: 6 hours protected from light * Procurement: commercially available. (HoloxanR). 9.3. Mesna: * How supplied: 400 mg ampoules (4 ml) * Storage: at room temperature * Stability: - after opening of ampoule : extemporaneous use 11 * - after dilution for infusion : in NaCl 0,9 % - 6 hours, at light, at 4°C or room temperature. Procurement: commercially available. (UromitexanR) 9.4 Gemcitabine: * How supplied: 200 and 1000 mg vials as lyophilisate powder * Storage: at room temperature (below 30°C) * Reconstitution: with NaCl 0.9 % (5 ml/200 mg) up to 40 mg/ml * Stability after reconstitution: stable at room temperature for 24 hours * Procurement: commercially available (GemzarR) 9.5 Paclitaxel: * How supplied: TaxolR, solution at 6 mg/ml in a 5-ml vial * Storage: at room temperature (15 - 25 °C), protected from light * Reconstitution: must be diluted with NaCl 0.9 % or 5% glucose to reach a final concentration of 0.3 – 1.2 mg/ml * Stability after reconstitution: stable at room temperature for 27 hours * Administration: should be administered using non-PVC containing equipment, through an in-line filter with a microporous membrane not greater than 0.22 µm. * Procurement: to be provided by Bristol Myers Squibb, as long as the drug is not taken in charge by the local social security system 10. SIDE EFFECTS 10.1 Cisplatin: - Hypersensitivity reactions (rare) - Nausea, vomiting - Nephrotoxicity: transient or permanent renal insufficiency, hypomagnesemia; avoidance of aminoglycoside antibiotic therapy is recommended - Myelosuppression (mild), haemolytic anaemia (uncommon) - Neurotoxicity: peripheral neuropathy, papilledema, retrobulbar neuritis, normal pressure hydrocephalus, seizures (rare) - Ototoxicity: tinnitus, high frequency hearing losses. 10.2. Ifosfamide : - Urotoxicity (toxic cystitis with haematuria): prevented by Mesna. Microscopic haematuria can be observed - leucopenia and less frequently thrombocytopenia - Fall in haemoglobin: of more than 4 g/dl in 10 % of the cases - CNS symptoms (20 %): somnolence, disorientation, confusion and lethargy, occurring within hours after ifosfamide and lasting for one or two days - Alopecia - Nausea and vomiting - Mild and transient liver test abnormalities. 10.3 Mesna: - Rarely nausea - Vomiting - Diarrhoea. 12 10.4 Gemcitabine: - Myelosuppression : thrombopenia and anaemia often more important than neutropenia - Nausea, vomiting, diarrhoea (moderate) - Fever, chills, asthenia, malaise, "flu-like" syndrome, (frequent) responding to low dose corticotherapy - Alopecia (moderate) - Peripheral oedema not due to cardiac failure - Skin rash responding to low dose corticotherapy - Moderate and reversible elevation in transaminases 10.5 Paclitaxel: - myelosuppresssion : neutropenia, thrombopenia - nausea, vomiting - mucositis - hypersensitivity : frequent and severe, requiring systemic premedication (dexamethasone, H1 and H2 antihistaminics) - peripheral neuropathies (frequent) - alopecia - bradycardia (common), other arrhythmia possible (particularly in patients with other risk factors) - tissue necrosis if extravasasion 11. DOSE ADAPTATION PLAN 11.1 Myelotoxicity: - - If neutrophil count is < 1,500/mm3 and/or platelets < 100,000/mm3 on day 22, treatment is postponed by one or two weeks If myelosuppression persists on day 36, the patient is off treatment Gemcitabine will be given on day 8, only if there is no grade IV neutropenia (neutrophils < 500/mm3) or grade III/IV thrombopenia (platelets < 50,000/mm3). Administration has not to be postponed on day 15. dose adaptation according to the haematological nadirs for GIP or paclitaxel: 75% of dosage of all the drugs for next course if during last course, nadir for neutrophil and/or platelet was respectively < 500/mm³ or 50,000/mm³ 11.2 Nephrotoxicity: - If serum creatinine peak is 1.5-3.0 mg/dl with return to normal value, the dose of CDDP is reduced by 50 % - If serum creatinine peak has exceeded 3.0 mg/dl, CDDP administration is stopped (even if return to normal value) - If serum creatinine is not in the normal range on day 36, the patient is off treatment. 11.3 Neurotoxicity: In case of WHO grade > II neurotoxicity, CDDP or paclitaxel administration is stopped (if peripheral polyneuropathy) or ifosfamide administration is stopped (if encephalopathy). 11.4 Otoxicity: If hearing loss becomes evident clinically, CDDP administration is stopped. 13 11.5 Occurrence of anaemia. If anaemia is observed with the GIP regimen, when the haemoglobin level is < 10 g/dl and if it is attributed to cisplatin treatment, patient may be proposed to be treated by erythropoietin (Eprex R), 10000 U subcutaneously three times per week until one month after the administration of the last dose of cisplatin. 11.6 Other toxicity: For any other significant toxicity, the investigator should contact the coordinator. 12. CRITERIA OF EVALUATION Patients are considered as evaluable if they complete 3 courses of treatment. Patients with early progression or death prior to evaluation due to malignant disease or to toxicity are considered as treatment failures and incorporated in the evaluable patients. The duration of overall response is the period between the first day of treatment and the date of first progression or first relapse. Survival will be dated from the day of registration. 12.1 Measurability of the disease * Are not considered measurable or evaluable, lesions in previously irradiated fields, ascitis and pleural effusion, lesions evaluated by bone scintigraphy. * Are considered measurable, lesions which are measurable in two perpendicular diameters as: - lung tumour surrounded by aerated lung - skin nodule - a superficial lymph node * Are considered evaluable, lesions that are deeply located and not measurable in two diameters: - a lung tumour not completely surrounded by aerated lung - a palpable deep lymph node - a bronchial lesion evaluable by endoscopy. 12.2 Response criteria Complete response Complete disappearance of all tumoral lesions, for duration of at least 4 weeks. Partial response Defined as a decrease of > 50% in the product of cross-sectional diameters of well-outlined lesions or > 50% decrease of poorly outlined lesions for at least 4 weeks in the absence of progressive disease elsewhere or occurrence of new lesions elsewhere. Patients who have had a complete clinical response but a positive repeat bronchoscopy with biopsy will be considered partial responders. Progressive disease > 25% increase in the product of cross-sectional diameters of one or more outlined lesions or the occurrence of new lesions irrespective of response elsewhere. 14 Stable disease This includes all patients who have reductions of < 50% or increases of < 25% of well-outlined lesions whether progressing or improving, for a period of at least 4 weeks. 12.3 Death Early death Death prior to time of response evaluation. Toxic death Death occurring as a result of drug toxicity. 12.4. Toxicity Will be evaluated according to standard WHO criteria (appendix II). All medication taken by the patient will be documented concerning type, amount, start and end of administration. 13. OFF TREATMENT REGIMEN AND OFF STUDY DEFINITIONS AND PROCEDURES 13.1. Treatment regimen A course of treatment and follow-up, modified for toxicity and supplemented by supportive therapy, as laid down in this protocol. 13.2. Off treatment regimen A patient is off treatment regimen when it is no longer possible to continue treatment in accordance with the protocol, including those cases of patient's refusal of treatment. Follow up continues. 13.3. Off trial Patients can only be withdrawn from the trial for one of the following reasons. An appropriate form has to be sent to the data centre. (1) Initial ineligibility discovered after registration: cite reason by letter; survival followup should be provided. (2) Death. Submit form 7. (3) Patient refuses follow-up: report by letter the stated and apparent reasons. 14. ENTRY AND RANDOMISATION PROCEDURES All patients eligible for this study must be registered and randomised by calling the data manager at 02/539.04.96 between 9 a.m. and 12 a.m. The following information will be required at registration: - Trial number - treatment centre - patient's name or code- birthday - performance status - neutrophil count - results of brain CT scan 15 - existence of prior chest irradiation - diagnosis of local pathologist - TNM Stratification of randomisation: In this study stratification will be done by: 1 - center 2 – initial P.S. 3 – initial neutrophil count 4 – response status 5 – sex 9 - age 15. DATA MANAGEMENT AND TRIAL COORDINATION Study coordinator and data manager The study coordinator is Dr. Jean-Paul Sculier (tel. : 02/539.04.96) and the data manager is Mrs Paule Mommen (Institut Jules Bordet, rue Héger-Bordet 1, 1000 Bruxelles, tél. : 02/539.04.96 or fax : 02/534.37.56). Forms to be submitted The following forms have to be submitted: Form A 2 3 B 5 7 10 Role Current tumour status Registration report Evaluation report Indication at the registration and at each evaluation at the time of initial allocation together with form A after 1st evaluation (3 courses of chemotherapy) together with form A Chemotherapy report after each course of chemotherapy Post-treatment follow-up every 3 months following the end of the chemotherapy or at or failure report progression of the disease Final report on death of the patient Serious adverse events at occurrence at any serious adverse event, to be submitted report as soon as possible to the data centre 16. ETHICAL CONSIDERATIONS 16.1 The protocol will investigator's hospital be approved by the ethical committees of 16.2 Patients will be asked to agree to participate to the study. The outline of the trial will be explained by the investigator and patient will have to give consent. Patient will be informed of the modalities, anticipated benefits and possible hazards and discomforts in taking part in the trial. The patient will be informed that the trial will comply with the principles present in the Declaration of Helsinki. If during the study, the patient wants to stop the treatment, this will be respected by the investigator. 16 the 16.3 Patient consent will be noted in the hospital file. 16.4 Information in case of occurrence of unexpected events like particular toxicity has to be communicated between the investigators as soon as detected. Those have to be reported as soon as known by the local investigator to the study coordinator. 16.5 The patient’s confidentiality has to be respected. 17. STATISTICAL CONSIDERATIONS The primary endpoint of the study will be to compare the survival duration of patients allocated to GIP alone (standard arm) versus those having received paclitaxel after GIP (experimental arm). Randomisation will occur in patients having non progressive disease after 3 courses of GIP; survival will therefore be measured since the day of randomisation. The sample size evaluation has been based on the following assumptions generated by the analysis of ELCWP study 01952: a) rate of randomisation is expected to be about 50-60% b) 1-year survival rate in the standard arm (since randomisation) is expected to be 20% c) an increase of this rate to 35% is judged as clinically worthwhile and should be detected with a 80% probability (power) using a two-sided logrank test with a significance level of 5%. With these assumptions, the total number of events to be observed is 178 and should be achieved with randomisation of 123 patients in each arm of the study (23). Taking into account the expected randomisation rate, the number of patients to be registered in the study is then estimated to be around 450. 18. PUBLICATION AND AUTHORSHIP Authors on publication include the study coordinators, the authors of the protocol, the statistician and a member of each institution entering at least 10% of evaluable patients for abstracts and 5% of evaluable patients for full papers. Authorship will also include the data manager for full papers. All information generated by the study is full property of the European Lung Cancer Working Party. No information may be used for publication or presentation without written approval of the study coordinator and the chairman of the group. 19. BIBLIOGRAPHY 1. Sculier J.P.: Chimiothérapie des formes inopérables non métastatiques : une indication formelle ? Les Dossiers des 3e Rencontres de Pneumologie. Ed. Margaux Orange, Paris, 1994, pp 244-246. 2. Souquet P.J., Chauvin F., Boissel J.P. et al: Polychemotherapy in advanced non-small cell lung cancer: a meta-analysis. Lancet 342:19-22; 1993. 3. Non-small Cell Lung Cancer Collaborative Group: Chemotherapy in non-small cell lung cancer: a meta-analysis using updated data on individual patients from 52 randomised clinical trials. BMJ 311:899-909; 1995. 4. Sculier J.P., Berghmans T., Castaigne C., Lalami Y., Luce S., Sotiriou C., Vermylen P., M. Paesmans : Best supportive care or chemotherapy for stage IV non small cell lung cancer. In Progress and perspectives in lung cancer. Ed. Van Houtte P., Klastersky J. and Rocmans P. Springer, Berlin, 1999, pp 199-207. 17 5. Sculier J.P., Klastersky J. Giner V. et al: Phase II randomized trial comparing high-dose cisplatin with moderate dose cisplatin and carboplatin in patients with advanced non-small cell lung cancer. J. Clin. Oncol. 12:353-359; 1994. 6. Donnadieu N., Paesmans M., Sculier J.P.: Chemotherapy of non-small cell lung cancer according to disease extent: a meta-analysis of the literature. Lung Cancer 7:243-252; 1991. 7. Sculier J.P.: Nouvelle vague d’agents chimiothérapeutiques: le point en cancérologie pulmonaire. Rev. Mal. Resp. 14:154-156; 1997 8. Sculier J.P., Paesmans M., Thiriaux J., Lecomte J., Bureau G., Giner V., Efremidis A., Lafitte J..J., Berchier M.C., Alexopoulos C.G., Zacharias C., Mommen P., Ninane V., Klastersky J. and the European Lung Cancer Working Party: A phase III randomized trial comparing cisplatin and carboplatin with or without ifosfamide in patients with advanced non-small cell lung cancer. J Clin. Oncol. 16:1388-1396; 1998 9. Lund B., Kristjansen P.E.G., Hansen H.H.: Clinical and preclinical activity of 2',2'difluorodeoxycytidine (gemcitabine). Cancer Treatment Reviews 19:45-55; 1993. 10. Abbruzzese J.L., Grunewald R., Weeks E.A., Gravel D., Adams T., Nowak B., Mineiski S., Tarassoff P., Satterlee W., Ruber Mn., Plunkett W.: A phase I clinical plasma and cellular pharmacology study of gemcitabine. J. Clin. Oncol. 9:491-498; 1991. 11. Bergman A.M., Ruiz Van Haperen V.W.T., Veerman G. et al.: Synergistic interaction between cisplatin and gemcitabine in vitro. Clin Cancer Res 2:521-530;1996. 12. Cardenal F, Paz Lopez-Cabrerizo M, Anton A, Alberola V, Massuti B, Carrato A, Barneto I, Lomas M, Garcia M, Lianes P, Montalar J, Vadell C, Gonzalez-Larriba JL, Nguyen B, Artal A, Rosell R. Randomized phase III study of gemcitabine-cisplatin versus etposide-cisplatin in the treatment of locally advanced or metastatic non-small-cell lung cancer. J Clin Oncol 17: 12-18; 1999. 13. Gatzemeier U., Manegold C., Eberhard W. et al.:A phase II trial of gemcitabine and ifosfamide in non-small cell lung cancer. Semin Oncol: 24 (suppl 8): 36- 38;1997. 14. Bunn P.A.Jr: Triplet chemotherapy with gemcitabine, a platnum, and a third agent in the treatment of advanced non-small cell lung cancer. Semin Oncol: 26 (suppl 4): 25-30; 1999. 15. Gatzemeier U, Heckmayr M, Neuhauss R, Schlüter I, Pawel JV, Wagner H, Dreps A. Phase II study with paclitaxel for the treatment of advanced inoperable non-small cell lung cancer. Lung Cancer 1995; 12: S101-S106. 16. Alberola V, Rosell R, González-Larriba JL, Molina F, Ayala F, Garciá-Conde J, Benito D, Pérez JM. Single agent taxol, 3-hour infusion, in untreated advanced non-small-cell lung cancer. Ann Oncol 1995; 6: S49-S52. 17. Furuse K, Naka N, Takada M, Kinuwaki E, Kudo S, Takada Y, Yamakido M, Yamamoto H, Fukuoka M. Phase II study of 3-hour infusion of paclitaxel in patients with previously untreated stage III and IV non-small cell lung cancer. Oncology 1997; 54: 298-303. 18 18. Tester WJ, Jin PY, Reardon DH, Cohn JB, Cohen MH. Phase II study of patients with metastatic nonsmall cell carcinoma of the lung treated with paclitaxel by 3-hour infusion. Cancer 1997; 79: 724-729. 19. Millward MJ, Bishop JF, Friedlander M, Levi JA, Goldstein D, Olver IN, Smith JG, Toner GC, Rischin D, Bell DR. Phase II trial of a 3-hour infusion of paclitaxel in previously untreated patients with advanced non-small-cell lung cancer. J Clin Oncol 1996; 14: 142148. 20. Hainsworth D, Thompson DS, Greco FA. Paclitaxel by 1-hour infusion: an active drug in metastatic non-small-cell lung cancer. J Clin Oncol 1995; 13: 1609-1614. 21. Chang AY, Kim K, Glick J, Anderson T, Karp D, Johnson D. Phase II study of taxol, merbarone, and piroxantrone in stage IV non-small-cell lung cancer: the Eastern Cooperative Oncology Group results. J Natl Cancer Inst 1993; 85: 388-394. 22. Murphy WK, Fossella FV, Winn RJ, Shin DM, Hynes HE, Gross HM, Davilla E, Leimert J, Dhingra H, Raber MN, Krakoff IH, Hong WK. Phase II study of taxol in patients with untreated advanced non-small-cell lung cancer. J Natl Cancer Inst 1993; 85: 384-388. 23. Machin D. and Campbell M.J.: Statistical tables for the design of clinical trials. Blackwell Scientific Publications, Oxford, 1987. 19 Appendix I Performance scale (Karnofsky) PERFORMANCE STATUS SCALE (KARNOFSKY INDEX) ___________________________________________________________________________ Able to carry on normal activity; 100 Normal; no complaints, no evidence no special care is needed of disease 90 Able to carry on normal activity; minor signs or symptoms of disease 80 Normal activity with effort; some signs or symptoms of disease _________________________________________________________________________ Unable to work, able to live at home, care for most personal needs; a varying amount of assistance is needed 70 Care for self, unable to carry on normal activity or do active work 60 Requires occasional assistance, but is able to care for most of his needs 50 Requires considerable assistance, and frequent medical care _________________________________________________________________________ Unable to care for self; requires equivalent of institutional or hospital care; disease may be progressing rapidely 40 Disabled; required special care and assistance 30 Severely disabled; hospitalization is indicated, although death not imminent 20 Very sick; hospitalization necessary, active supportive treatment necessary 10 Moribund; fatal process progressing rapidely 0 Dead ___________________________________________________________________________ (Cancer 1 : 634 (1948) ) 20 Appendix II : Staging classification A. TNM : T: primary tumors TX Tumor proven by the presence of malignant cells in bronchopulmonary secretions but not visualized by roentgenography or bronchoscopy, or any tumor that cannot be assessed as in a pretreatment staging. TO No evidence of primary tumor T1S Carcinoma in situ T1 A tumor that is 3.0 cm or less in greatest dimension, surrounded by lung or visceral pleura, and without evidence of invasion proximal to a lobar bronchus at bronchoscopy* T2 A tumor more than 3.0 cm in greatest dimension, or a tumor of any size that either invades the visceral pleura or has associated atelectasis or obstructive pneumonitis extending to the hilar region. At bronchoscopy, the proximal extent of demonstrable tumor must be within a lobar bronchus or at least 2.0 cm distal to the carina. Any associated atelectasis or obstructive pneumonitis must involve less than an entire lung. T3 A tumor of any size with direct extension into the chest wall (including superior sulcus tumors), diaphragm, or the mediastinal pleura or pericardium without involving the heart, great vessels, trachea, esophagus, or vertebral body, or a tumor in the main bronchus within 2.0 cm of the carina without involving the carina. T4 A tumor of any size with invasion of the mediastinum or involving heart, great vessels, trachea, esophagus, vertebral body, or carina or with presence of malignant pleural effusion.** NB : * The uncommon superficial tumor of any size whose invasive component is limited to the bronchial wall and that may extend proximal to the main bronchus is classified as T1. ** Most pleural effusions associated with lung cancer are due to tumor. There are, however, some few patients in whom cytopathologic examination of pleural fluid (on more than one specimen) is negative for tumor and the fluid is nonbloody and is not an esudate. When these elements and clinical judgment dictate that the effusion is not related to the tumor, the cases should be staged T1, T2 or T3, with effusion being excluded as a staging element. 21 N: M: regional lymph nodes N0 No demonstrable metastasis to regional lymph nodes N1 Metastasis to lymph nodes in the peribronchial or the ipsilateral hilar region, or both, including direct extension N2 Metastasis to ipsilateral mediastinal lymph nodes and subcarinal lymph nodes N3 Metastasis to contralateral mediastinal lymph nodes, contralateral hilar lymph nodes, or ipsilateral or contralateral scalene or supraclavicular lymph nodes. distant metastasis M0 M1 B. No (known) distant metastasis Distant metastasis present-specify site(s). AJCC/UICC 1987 Staging : Stage Occult carcinoma O I A II B II A II B III A IIIB IV T X IS 1 2 1 2 3 1 2 3 any 4 any N 0 0 0 0 1 1 0 2 2 1,2 3 any any M 0 0 0 0 0 0 0 0 0 0 0 0 1 22 Appendix III : WHO's Criteria of toxicity 23 24 25 26 Appendix IV THE WORLD MEDICAL ASSOCIATION DECLARATION OF HELSINKI Recommandations guiding physicians in biomedical research involving Human Subjects. Adopted by the 18th World Medical Assembly, Helsinki, Finland, June 1964, amended by the 29th World Medical Assembly, Tokyo, Japan, October 1975, the 35th World Medical Assembly, Venice, Italy, October 1983 and the 41st World Medical Assembly, Hong Kong, September 1989. INTRODUCTION It is the mission of the physician to safeguard the health of the people. His or her knowledge and conscience are dedicated to the fulfillment of this mission. The Declaration of Geneva of the World Medical Association binds the physician with the words, "The health of my patient will be my first consideration," and The International Code of Medical Ethics declares that, "A physician shall act only in the patient's interest when providing medical care which might have the effects of weakening the physical and mental condition of the patient". The purpose of biomedical research involving human subjects must be to improve diagnostic, therapeutic and prophylactic procedures and the understanding of the aetiology and pathogenesis of disease. In current medical practice most diagnostic, therapeutic or prophylactic procedures involve hazards. This applies especially to biomedical research. Medical progress is based on research which ultimately must rest in part on experimentation involving human sujects. In the field of biomedical research, a fundamental distinction must be recognized between medical research in which the aim is essentially diagnostic or therapeutic for a patient, and medical research, the essential object of which is purely scientific and without implying direct diagnostic or therapeutic value to the person subjected to the research. Special caution must be exercised in the conduct of research which may affect the environment, and the welfare of animals used for research must be respected. Because it is essential that the results of laboratory experiments be applied to human beings to further scientific knowledge and to help suffering humanity, the World Medical Association has prepared the following recommendationd as a guide to every physician in biomedical research involving human subjects. They should be kept under review in the future. It must be stressed that the standards as drafted are only a guide to physicians all over the world. Physicians are not relieved from criminal, civil and ethical responsibilities under the laws of their own countries. 27 I. BASIC PRINCIPLES 1. Biomedical research involving human subjects must conform to generally accepted scientific principles and should be based on adequately performed laboratory and animal experimentation and on a thorough knowledge of the science literature. 2. The design and performance of each experimental procedure involving human subjects should be clearly formulated in an experimental protocol which should be transmitted to consideration, comment and guidance to a specially appointed committee independent of the investigator and the sponsor, provided that this independent committee is in conformity with the laws and regulations of the country in which the research experiment is performed. 3. Biomedical research involving human subjects should be conducted only by scientifically qualified persons and under the supervision of a clinically competent medical person. The responsibility for the human subject must always rest with a medically qualified person and never rest on the subject of the research, even though the subject has given his or her consent. 4. Biomedical research involving human subjects cannot legitimately be carried out unless the importance of the objective is in proportion to the inherent risk to the subject. 5. Every biomedical research project involving human subjects should be preceded by careful assessment of predicatable risks in comparison with foreseeable benefits to the subject or to others. Concern for the interests of the subject must always prevail over the interests of science and society. 6. The right of the research subject to safeguard his or her integrity must always be respected. Every precaution should be taken to respect the privacy of the subject and to minimize the impact of the study on the subject's physical and mental integrity and on the personality of the subject. 7. Physicians should abstain from engaging in research projects involving human subjects unless they are satisdied that the hazards involved are believed to be predictable. Physicians should cease any investigation if the hazards are found to outweigh the potential benefits. 8. In publication of the results of his or her research, the physician is obliged to preserve the accuracy of the results. Reports of experimentation not in accordance with the principles laid down in this Declaration should not be accepted for publication. 9. In any research on human beings, each potential subject must be adequately informed of the aims, methods, anticipated benefits and potential hazards of the study and the discomfort it may entail. He or she should be informed that he or she is at liberty to obtain from participation in the study and that he or she is free to withdraw his or her consent to participation in any time. The physician should then obtain the subject's freely-given informed consent, preferably in writing. 10. When obtaining informed consent for the research project the physician should be particularly cautious if the subject is in a dependent relationship to him or her or may consent under duress. In that case, the informed consent should be obtained by a physician who is not engaged in the investigation and who is completely independent of this official relationship. 11. In case of legal incompetence, informed consent should be obtained from the legal guardian in accordance with national legislation. Where physical or mental incapacity makes it impossible to obtain informed consent, or when the subject is a minor, permission from the 28 responsible relative replaces that of the subject in accordance with national legislation. Whenever the minor child is in fact able to give a consent, the minor's consent must be obtained in addition to the consent of the minor's legal guardian. 12. The research protocol should always contain a statement of the ethical considerations involved and should indicate that the principles enunciated in the present Declaration are complied with. II. MEDICAL RESEARCH COMBINED WITH PROFESSIONAL CARE (Clinical Research) 1. In the treatment of the sick person, the physician must be free to use a new diagnostic and therapeutic measure, if in his or her judgment it offers hope of saving life, re-establishing health or alleviating suffering. 2. The potential benefits, hazards and discomfort of a new method should be weighted against he advantages of the best current diagnostic and therapeutic methods. 3. In any medical study, every patient including those of a control group, if any should be assured of the best proven diagnostic and therapeutic methods. 4. The refusal of the patient to participate in a study must never interfere with the physicianpatient relationship. 5. If the physician considers it essential not to obtain informed consent, the specific reasons for this proposal should be stated in the experimental protocol for transmission to the independent committee (1, 2). 6. The physician can combine medical research with professional care, the objective being the acquisition of new medical knowledge, only to the extent that medical research is justified by its potential diagnostic or therapeutic value from the patient. III. NON-THERAPEUTIC BIOMEDICAL RESEARCH INVOLVING HUMAN SUBJECTS (Non-clinical biomedical research) 1. In the purely scientific application of medical research carried out on a human being, it is the duty of the physician to remain the protector of the life and health of that person on whom biomedical research is being carried out. 2. The subjects should be voluntaires either healthy persons or patients for whom the experimental design is not related to the patient's illness. 3. The investigator or the investigating team should discontinue the research if in his/her or their judgment it may, if continued, be harmful to the individual. 4. In research on man, the interest of science and society should never take precedence over considerations related to the well-being of the subject. 29 ADDENDUM TO PROTOCOL 01981 Radiotherapy for patients with brain metastases 1. Background By analyzing, retrospectively, the survival data relative to the subgroup of 128 patients with non small cell lung cancer and brain metastases at diagnosis randomised in a previous trial of the European Lung Cancer Working Party (01901) testing the addition of ifosfamide to the combination of cisplatin-carboplatin, we obtained the following results. Brain irradiation was given at induction, in complement to chemotherapy, in 35% of the patients when the brain metastases were asymptomatic and in 62% of the patients in case of symptomatic metastases. Survival of the patients receiving this immediate brain irradiation was shown to be superior to that of the patients who received only chemotherapy using a logrank test (p=0.04) stratified for the type of brain metastases. Estimated 1 year survival rates were 29% for asymptomatic patients having been treated with irradiation at induction and 15% for those treated with chemotherapy alone. The corresponding figures for patients with symptomatic metastases were 5% and 24%. Furthermore, using a Cox regression model, administration of brain irradiation remained an explanatory factor of better survival after adjustment for performance status, number of metastatic sites and neutrophil count. However, due to the retrospective non randomised design of our analysis, these survival differences can simply be due to patients selection and non comparability of the two patients populations rather than due to irradiation itself. Therefore, the present study will be a randomised trial assessing the survival benefit obtained with immediate brain irradiation for selected non small cell lung cancer patients presenting, at diagnosis, with brain metastases. 2. Study design The objective of the present study is to assess if brain irradiation given as induction treatment, concomittantly to the first chemotherapy cycle will improve survival compared to irradiation postponed until the brain metastases have become symptomatic (or never administered according to the evolution of the disease, the choice of late irradiation being left to the investigator). Randomisation will then be performed between immediate or delayed (if necessary) brain irradiation (30 Gy given in 10 daily fractions). 3. Eligibility criteria Eligible patients for this study will be those eligible for the chemotherapy trial 01981 with brain metastases at diagnosis, either asymptomatic either symptomatic with a response, within one week, to corticotherapy. 4. Radiotherapy treatment Treatment will consist of 30 Gy delivered to the whole brain in 10 fractions and 2 weeks. The dose is specified according to ICRU recommendations (at midplane). Two opposing fields are treated daily and the treatment will be given with megavoltage equipment. Corticosteroids are advised during radiotherapy and taperred off as soon as possible 30 5. Sample size Considering that an improvement in the 1 year survival rate from 15% to 30% has to be dectected with a power of 80%, using a two-sided logrank test and a significance level of 5%, we need to follow until death 158 patients in the trial. To achieve this number of observed events, the required sample size for randomised patients is estimated to be 102 in each arm. 6. Randomisation procedure Treatment will be allocated at the same time the patient will be randomised in the trial 01981 by calling the data manager, Mrs P. Mommen, at 32.2.539.04.96. Randomisation will be stratified by center, brain metastases status (asymptomatic versus symptomatic) and chemotherapy arm (cisplatin-carboplatin-ifosfamide versus cisplatin-carboplatin-gemcitabine versus ifosfamidegemcitabine). 31