PE 102 Course Material
advertisement

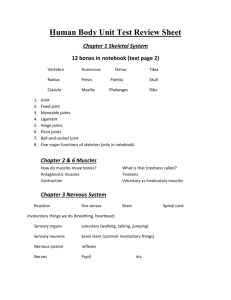
1 Table of Contents 1 2 3 4 5 6 Anatomy 4 Types of Bones 5 Posture 6 Postural Examination 7 Joints 10 Types of Joints 10 Muscular System 12 Types of Muscle Major Skeletal Muscles and their Location 12 13 Sports Injuries 14 Common Sports Injuries of Skin and their Treatment 17 References 20 2 Preface The PE 102 course is offered in the 2nd semester of the undergraduate programme. The content of this health education course describes the body structure, the names and location of the important bones and muscles, and their relation to the basic movements in sports activities. Posture, which is considered essential for maintaining a healthy body structure, is explained in detail with the emphasis on the use of correct posture in everyday activities. Injuries are common in the sports arena and a brief outline of the sports injuries, their symptoms, causes, precautions and treatment are listed for the benefit of the students. 3 ANATOMY Anatomy- It is the science of understanding body parts. Human Anatomy- It is the science of structure components and positions which make up the human body. The human body is made of: cells, tissues, organs and systems. SKELETAL OR BONY SYSTEM IT’S IMPORTANCE Rigid supporting framework of connective tissue. Prevents body from collapsing into heap of soft tissue. Provides mechanical levers for muscle. Protective shell or casing for vital viable organs like; Brain, lungs, heart and pelvic organs. Factories for formed elements of blood i.e. manufacture of RBCs (Red Blood Cells) and WBCs (White Blood Cells). Great reserves of calcium and phosphorus. Vital living tissue continuously undergoing changes of building up and tearing down. 4 TYPES OF BONES: 2. Short bones 1. Long bones 3. Irregular bones 4. Flat bones STRUCTURE OF BONE: - Hard connective tissue - As child grows hardening takes place - Yellow bone marrow – vital minerals and calcium stored in spongy area of bone. - Red marrow in the end of bone - manufactures RBC’s. - Ratio of inorganic and organic substances in bone varies during life time: child 1:1, adult 4:1, elderly 7:1. - Fragile in elderly DIVISION OF SKELETON: Head and Torso Upper and Lower Limbs 5 Two parts: Axial & Appendicular. Total Bones 206. Axial 80 – Appendicular 126. IMPORTANT BONES AND THEIR LOCATIONS: Application of the skeleton system to Physical Activity: 1. Condition of bone is improved by exercise. 2. More mineral salts are deposited and more fibers are produced. 3. Density and size of bone increased. 4. Due to fracture, the bone becomes decalcified when in plaster because of a lack of mechanical stress which can be improved with stationary movement of the part. Human Bones 5. In old age bones lose calcium, which causes osteoporosis, and due to lack of protein the bones become brittle. Physical activity will help to overcome the above conditions. 6. Regulation of calcium metabolism is maintained between blood and the bone. 7. The mineral metabolism can be maintained with longitudinal pressure on long bones by stress of gravity with physical activity. 8. Pressure due to activity stimulates bone growth and there is increased weight-bearing, Ability, increased thickness of bone and density of shaft. 9. Prolonged bed rest affects Ca (calcium)+ metabolism. Increased urinary Ca+ excretion in bed rest is not due to inactivity but due to absence of longitudinal pressure on long bones. There is no change in Urinary Ca+ excretion if heavy bicycle ergometer work is performed in a supine position for 1 to 4 hours daily or 8 hours of inaction sitting in a wheelchair. But 3 hours of standing per day with bed rest results in restoring the Ca+ excretion to normal values. POSTURE Ability to stand erect: To handle the body easily, gracefully & efficiently under all circumstances, muscular strength is involved in correct posture and emotional condition is frequently reflected in carriage. 6 CAUSES OF POOR POSTURE: Heredity Poor circulation Over-training Poor training methods or exercise regime Strain on joints and chronic stress Lack of flexibility Continued fatigue Muscle imbalances POSTURAL EXAMINATION Posture is tested by reference to the rating guides for 13 different segments identified in the posture rating chart. POSTURAL DEFORMITIES KYPHOSIS Exaggeration or increase in the amount of normal convexity of the thoracic region of the spine. Causes: Lack of strength or tonus of extensors of spine weight of body parts such as forward head or forward position of the arms may cause stretching of the posterior muscles. Excessive relaxations may allow gravitational forces to flex the spine too much. Ex. tall people – slumping. 7 CORRECTION: Extensors to be strengthened and tonus improved. Excess gravitational stress must be removed by realignment of head, arms and shoulder girdle by variety of occupational positions LORDOSIS • It is an exaggeration or increase in the amount of the norm of concavity of the lumbar region of the spine. • Relaxation and poor tonus of abdominals may allow the curve to collapse. Also if the hips are thrust forward the curve increases in order to throw the upper trunk back into balance. CORRECTION : • Normal spine Develop the abdominal strength Lordosis SCOLIOSIS • This is the lateral curvature of the spine when the bodies of the vertebrae are usually rotated to the convex side and the spinal processes rotated to the concave side and is known as right or left scoliosis. • The condition is sometimes congenital but most often acquired, due to lack of postural tone, or one - sided occupations. • Structural scoliosis is caused by rickets, infantile paralysis, unilateral lung diseases and one leg shorter being than the other. Correction: Exercises aimed at stretching the strong muscles on the concave side thereby contracting the weak, unstretched muscles on the convex side. 8 BOW LEGS KNOCK KNEE This is a deformity in which the legs are bowed outwards with the thighs in normal alignment but often the thigh is bowed outwards as well. This throws weight on the inner side of the knee. Deformity when the internal condyles of the femur have enlarged so that the knees knock together when the patient walks or are in a contact with the ankles separated when patient stands. The weight will be on the outer side of knee and inner side of foot. Causes: 1. As children start walking; rickets is a common cause; muscular weakness; Napkins tightly applied; bowing of femur. 2. in adults due to horse riding or injury. Slight degree in women due to greater width of hips. Causes: Rickets develops at the end of 1st year when bones fail to harden and remain so at the end of 4th year; bad posture. • Excessive walking, over weight. CORRECTION: 1. Stretching movements to adduct the knee. 2. Standing with cushion between the angles and drawing the knees together. NORMAL Correction: Passive stretching to over contracted muscles. BOW LEGS KNOCK KNEES FLAT FOOT This is a condition in which the inner longitudnal arch of the foot is depressed or fallen down from its normal position causing various degrees of pain, swelling and tiredness according to the disability CAUSES: 1. Acquired condition due to excessive standing/walking – overweight – muscular weakness – paralysis - fracture – sprains – rheumatism – rickets – badly fitting shoes - bad postures and illness. 2. Congenital – Usually not noticed until the infant begins to walk. 9 Normal foot • Flat foot Correction: 1. Passive movement of inversion, plantar and dorsiflexion. Walking on outer border, rolling leg and ankle, balancing in half crook position, walking feet turned in short wave diathermy – faradism. 2. Acute rest-petrissage, tappotment, efflurage with friction to toes. JOINTS When two or more bones of the skeleton meet one another. Functions of joint depend upon the type and allow efficient transfer of muscular force from muscle to bone. Types of Joints: THREE TYPES 1. Synarthtosis or immovable or fibrous. Eg. Skull bones. 2. Amphirathrosis or slightly movable or cartiliaginous e.g. Vertibral column. 3. Diarthrosis or freely movable or synovial e.g. hip. FIGURE SHOWING DIFFERENT JOINTS IN THE HUMAN BODY 10 TYPES OF SYNOVIAL JOINTS IN THE BODY Ball and Socket Ball and Socket: For example, at the femur-hip interface. This is where the head of the bone fits into a socket on the other bone, allowing a wide range of motion, in a number of axes. Hinge Joints Hinge joints: As their name indicates, these joints provide movement in one plane, like a door hinge. Found at the joint between humerous, ulna and knee joints. Pivot Joints Pivot joints: These allow rotation of one bone around another, such as where the radius and the ulna meet. Condyliod Joints Condyliod: Also known as ellipsoid joints, this is where curved facia meet, offering movement in a number of planes. Found in the fingers. Gliding and Saddle joints Gliding joints: Found between two flat parts of bone, and allow a little lateral movement only. Found between the carpels in the hands. Saddle joints: These joints allow a greater range of movement than condyloid joints, yet are similar in shape. The most well known example is at the base of the thumb. 11 MUSCULAR SYSTEM The bodily system that is composed of skeletal, smooth, and cardiac muscle tissue and functions in the movement of the body or of materials through the body, the maintenance of posture, and heat production. There are 700 muscles in the body which constitute 50% of body weight. PROPERTIES OF MUSCLES Contractility - Ability to shorten. Excitability – Respond to stimulus. Extensability – Lengthen beyond its normal resting length. Elasticity – Return to original length without damage. TYPES OF MUSCLES Voluntary – Skeletal – Striated. – form bulk of body’s muscles tissue – gives general shape to body- striped alternating bands of light and dark bandsconscious of work -phasic – responds quickly to stimulus. Caridac - Vaguely striated – involuntary control – pacemaker- special muscle tissue of the heart. Involuntary – Smooth – non striated - lines most of hollow organs – not under voluntary control – regulated by autonomic nervous system – lines blood vessels, hair follicles, digestive tract, urinary tract, etc. – tonic – responds gradually to stimulus. 12 TYPES OF SKELETAL MUSCLES Type I Fibers These fibers are also called slow twitch or slow oxidative fibers: they have more myoglobin and many mitochondria and blood capillaries. They are red, split ATP at a slow rate, have a slow contraction velocity, are very resistant to fatigue, have a high capacity to generate ATP by oxidative metabolic processes and are found in the postural muscles of the neck. Type II A Fibers These fibers are also called fast twitch or fast oxidative fibers and contain very large amounts of myoglobin, many mitochondria and blood capillaries. Type II A fibers are red, have a very high capacity for generating ATP by oxidative metabolic processes, split ATP at a very rapid rate, have a fast contraction velocity and are resistant to fatigue and are infrequently found in humans. Type II B Fibers These fibers are also called fast twitch or fast glycolytic fibers contain a low content of myoglobin, few mitochondria, few blood capillaries and large amounts glycogen. Type II B fibers are white, geared to generate ATP by anaerobic metabolic processes, are not able to supply skeletal muscle fibers continuously with sufficient ATP, fatigue easily, split ATP at a fast rate, have a fast contraction velocity and are found in large numbers in the muscles of the arms. MAJOR MUSCLES OF THE BODY Anterior View 13 Posterior View APPLICATION OF MUSCULAR SYSTEM TO PHYSICAL ACITIVITY More effective and efficient Tone increased Good posture Hypertrophy – Increase in size Efficient metabolism Increase in capillary penetration Increase in myoglobin Increase in glycogen storage Atrophy – shrinkage due to disuse SPORTS INJURIES Sports injuries are injuries that occur to athletes in sporting events. Most sports injuries are due to either trauma or overuse of muscles or joints when participating in a certain activity. The majority are caused by minor trauma involving muscles, ligaments, or tendons including: sprains, strains, contusions (bruises), fractures and dislocations. Sprain: Sprain refers to the damage or tearing of ligaments or a joint capsule When excessive force is applied to a joint, the ligaments that hold the bones together may be torn or damaged. This results in a sprain and its seriousness depends on how badly the ligaments are torn. Any joint can be sprained, but the most frequently injured joints are the ankle, knee, and finger. Prevention Signs and symptoms: The typical signs and symptoms associated with a sprain are the cardinal signs of a sprain. inflammation, localized pain, swelling, loss of function, loss of normal limb function, elasticity of ligament decreases. Treatment: The first modality for a sprain which can be used is R.I.C.E. i.e. 1. Rest 2. Ice 3. Compression 4. Elevation. Sprains can best be prevented by proper use of safety equipment (wrist, ankle guards; carts vs. lifting), warm-ups and cool-downs (including stretching), being aware of surroundings and maintaining strength and flexibility. Physical conditioning is the best way to avoid or lessen the degree of sprains. 14 Strain It is an injury to a muscle or tendon in which the muscle fibers tear as a result of overstretching. Strains are colloquially known as pulled muscles. Symptoms: Typical symptoms of a strain include: localized pain, stiffness, discoloration, and bruising around the strained muscle. . Causes: Strains are a result of muscular-fiber tears due to overstretching. They can happen while doing everyday tasks and are not restricted to athletes. Nevertheless, people who play sports are more at risk of developing a strain due to increased muscle use. Treatment: The first line of treatment for a muscular strain in the acute phase includes four steps commonly known as R.I.C.E Fractures Fractures are breaks in the bone that are often caused by a blow or a fall. A fracture can range from a simple hairline fracture to a compound fracture. Most fractures occur in the arms and legs. Bones form the skeleton of the body and allow the body to be supported against gravity and to move and function in the world. When outside forces are applied to the bone it has the potential to fail. Fractures occur when bone cannot withstand those outside forces. Fracture breaks or cracks all mean the same thing, that the integrity of the bone has been lost and the bone structure has failed. If the fracture line goes across the bone it is transverse, if it is at an angle it may be spiral. The fracture may be simple, commuted and multiple. Fractures should be treated by a medical expert but the first aid is to immobilize the joint. CONTUSION A contusion is an injury often produced by blunt force, such as a kick, fall or blow. The immediate result will be pain, swelling and discoloration. The severity of contusions ranges from simple skin contusions to muscle and bone contusions to internal organ contusions. Treatment: Use of R.I.C.E. as the first step of treatment. 15 Dislocation A dislocation occurs when extreme force is put on a ligament, allowing the ends of two connected bones to separate. Stress on the joint ligaments can lead to dislocation of the joint. The most commonly dislocated joint is the shoulder. Precautions 1. If you play sports, always wear appropriate protective equipment during practices and competitions, such as kneepads and shin guards. 2. When it comes to your workouts, always warm up and cool down, and do remember to work up to your training program slowly. 3. Suddenly increasing the intensity or duration of your workouts can lead to overuse injuries. 4. Try weightlifting to strengthen your muscles and stretching to improve your flexibility because strong, flexible muscles help support and protect joints. 5. Try conditioning and training year-round to maintain coordination and balance. That way you'll be less likely to injure yourself during your competitive season. 6. Regular stretching can help. After an injury or surgery has healed, it is also important to continue a regular stretching or conditioning program to prevent another injury. 7. The way you move can also help you prevent knee injuries. If your sport involves a lot of jumping, make sure to bend your knees when you land, which takes pressure off the ACL. Use your joints to crouch and bend at the knees and hips, reducing the possibility of a ligament injury. Common Sports Injuries of Skin and their Treatment Sports injuries result from acute trauma or repetitive stress associated with athletic activities. Sports injuries can affect bones or soft tissue (ligaments, muscles, tendons). Abrasions Abrasions are very common sports injuries that are usually caused by a fall on a hard surface. When an athlete falls or slides on the ground, friction causes layers of skin to rub off. The skin is composed of an outer layer (the epidermis) which provides protection and a deep inner layer the dermis, which provides the firmness and flexibility of the skin. Abrasions typically refer to an injury that removes these layers of skin. While there is often little or no blood loss from an abrasion, there can be a great deal of pain because of the many nerve endings that are exposed. 16 Treatment for Abrasions 1. 2. 3. 4. 5. Clean the wound with mild soap and water or mild antiseptic wash like hydrogen peroxide. Cover the area with an antibiotic ointment and a dry dressing which should be changed every few days. Take the tetanus booster if it has been 10 years since your tetanus shot. If there is a deep and large cut on the skin, it may require stitches which should be done by a physician. As healing begins, the area of the abrasion may look pink and raw, but in time the wound will form new skin that is pink and smooth which should not be scarred. Prevention: Prevention of abrasions is possible by wearing protective pads and covering any exposed skin with a layer of clothing. It is wise to have the necessary first aid supplies available in the event of an emergency. LACERATION A person with a laceration has a cut, or tear, in the skin, caused by an injury. Lacerations may also involve structures that lie beneath the skin. A laceration may be superficial or deep. Long, shallow lacerations may cause no great problems and require simple cleaning and closure. Symptoms: The symptoms of a laceration include pain, bleeding, swelling, and bruising to the skin. Worsening redness, swelling, and tenderness around a laceration are signs of a skin infection, called cellulitis. Treatment : Treatment for a laceration may include wound irrigation, wound cleansing, and laceration repair. Additional treatment for lacerations may include a tetanus vaccine, antibiotics, and pain medications. Lacerations caused by animal bites may also cause rabies. Always consult a doctor for wounds caused by animal bites. HEMATOMA An abnormal localized collection of blood in which the blood is usually clotted or partially clotted and is usually situated within an organ or a soft tissue space, such as within a muscle. A hematoma is caused by a break in the wall of a blood vessel. The break may be spontaneous, as in the case of an aneurysm, or caused by trauma. Treatment: It depends on its location and size. Treatment can involve draining the accumulated blood. A hematoma in or near the brain is particularly dangerous. 17 BURSITIS Bursitis is the inflammation of one or more bursae (small sacs) of synovial fluid in the body. The bursae rest at the points where internal functionaries, such as muscles and tendons, slide across bone. Healthy bursae create a smooth, almost frictionless functional gliding surface making normal movement painless. When bursitis occurs, however, movement relying upon the inflamed bursa becomes difficult and painful. Moreover, movement of tendons and muscles over the inflamed bursa aggravates its inflammation, perpetuating the problem. Causes: Bursitis usually results from a repetitive movement or due to prolonged and excessive pressure. Symptoms: Swelling or warm to the touch . Occasional skin redness in the area of the inflamed bursa. Pain and tenderness are common symptoms. Treatment : 1.Medications known as “Steroids“ to reduce inflammation. 2. Physical Therapy or exercise to strengthen the muscles in the area. BLISTER: A blister is a fluid- filled bump on the skin. Causes: Friction or constant pressure, such as from wearing a tight fitting shoe or gripping a tool, second degree burns , including sunburn, viral infections, such as chickenpox or shingles fungal infections such as athlete’s foot, contact dermatitis, such as poison, ivy or oak allergic reactions, drug reactions, certain cancers and inflammatory conditions, severe skin swellings especially of the legs. Treatment: A blister will often heal without treatment. Some general tips for treatment include: Protect Area: Be gentle with the injured area. To prevent further injury, put a bandage over the affected area. The blister should begin to shrink in about seven days. Do not pop or lance the blister. Opening the blister increases the chance of infection and delays healing. In the case of poison ivy or a viral infection, do not scratch the blister. If necessary call your doctor for medicine to relieve any itching or discomfort. Wash the Area: If the blister is closed, wash the area with soap and water and apply a bandage to help protect it. If the blister is open, wash the area, apply an antibiotic ointment, and then cover with a sterile dressing or bandage. See doctor if::The blister is unusually large; if the blister is in a critical area, such as on the face or the groin; if the blister is associated with a burn; or if there are signs of infection, such as increasing redness around the blister, red streaks, severe swelling, pus drainage, fever, or an increase in pain. 18 Prevention: To help prevent blisters: 1. Wear shoes that fit properly. 2. Always wear socks with your shoes. 3. Use gloves or protective padding when working with tools. 4. Wear a hat, protective clothing, and sunscreen when out in the sun. References Anatomy Bambi, Saulo. Anatomica Encyclopaedia. Koln: B. Taschen, 1999. Porter, Roy. Cambridge Illustrated History of Medicine. Cambridge: Cambridge University Press, 1996. The Greatest Benefit to Mankind: A Medical History of Humanity. New York: W.W. Norton and Company, 1997. Reiser, Stanley Joel. Medicine and the Reign of Technology. Cambridge: Cambridge University Press, 1978. Muscles Mooar, Pekka (2007). "Muscles". The Merck Manuals Online Medical Library. http://www.merck.com/mmhe/sec05/ch058/ch058c. 2008. Bárány, Michael (2002). "SMOOTH MUSCLE". http://www.uic.edu/classes/phyb/phyb516/index. 2008. "The Mechanism of Muscle Contraction". Principles of Meat Science (4th Edition). http://meat.tamu.edu/muscontract.. 2008. Costill, David L and Wilmore, Jack H. (2004). Physiology of Sport and Exercise. Champaign, Illinois: Human Kinetics. ISBN 0-7360-4489-2. Encyclopædia Britannica. 2008. Encyclopædia Britannica 2006 Ultimate Reference Suite DVD 2008 Huxley HE. The fine structure of striated muscle and its functional significance. Harvey Lectures, 1966. Skeletal System Kahn, Cynthia; Scott Line (2008).Musculoskeletal System Introduction: Introduction. NJ, USA: Merck & Co., Inc.. http://www.merckvetmanual.com/mvm/index.jsp?cfile=htm/bc/90100. Applegate, Edith; Kent Van De Graaff. "The Skeletal System".http://www.mnsu.edu/emuseum/biology/humananatomy/skeletal/skeletalsystem.. 2009. Engelbert, Phillis; Carol DeKane Nagel (2009). The Human Body / How Many Bones Are In The Human Body?". U·X·L Science Fact Finder. eNotes.com, Inc.. http://www.enotes.com/science-fact-finder/humanbody/how-many-bones-human-body. 2009. Gary, Farr (2002-06-25). "The Musculoskeletal System". http://www.becomehealthynow.com/category/bodymusculo/. 2008. joint at eMedicine Dictionary Ellis, Harold; Susan Standring; Gray, Henry David (2005). Gray's anatomy: the anatomical basis of clinical practice. St. Louis, Mo: Elsevier Churchill Livingstone. "Introductory Anatomy: Joints". http://www.leeds.ac.uk/chb/lectures/anatomy 2008 Sports Injuries Fridén, J., Kjorell, U., and L-E. Thornell. (1984). Delayed muscle soreness and cytoskeletal alterations. An immunocytological study in man. Int. J. Sports Med. 5. Fridén, J. and R.L. Lieber (1992). The structural and mechanical basis of exercise-induced muscle injury Med. Sci. Sport Exerc. 24. Russell B; Dix DJ; Haller DL; Jacobs-El J. Repair of injured skeletal muscle: a molecular approach. Medicine and Science in Sports and Exercise, 1992 Feb. Spinal Cord Medicine: Principles and Practice (2002) Lin VWH, Cardenas DD, Cutter NC, Frost FS, Hammond MC. Demos Medical Publishing Tursz A, Crost M. Sports-related injuries. A study of their characteristics, frequency, and severity, with comparison to other types of accidental injuries. Am J Sports Med. 1986 Jul–Aug;14(4) Chambers RB. Orthopaedic injuries in athletes (ages 6 to 17). Comparison of injuries occurring in six sports. Am J Sports Med. 1979 May–Jun;7(3) By: PE Department 2009 19