STEMI
advertisement
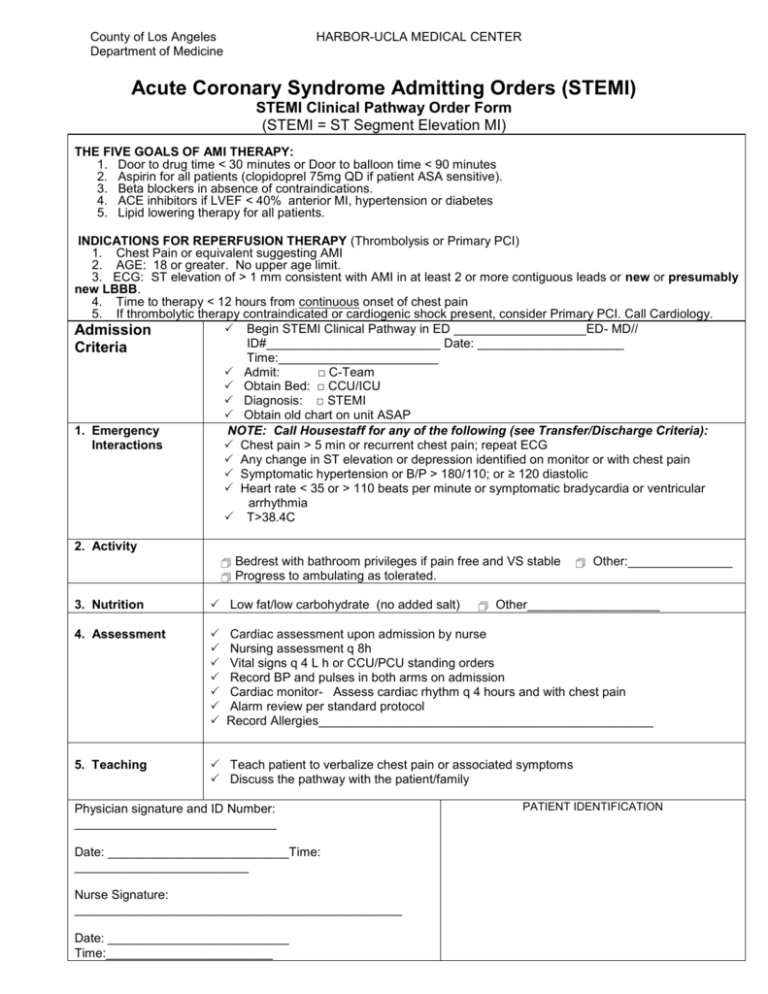
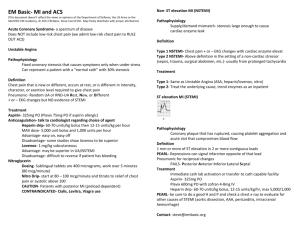
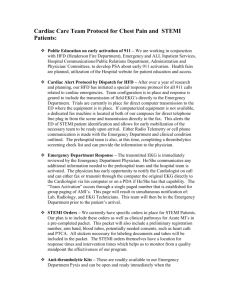
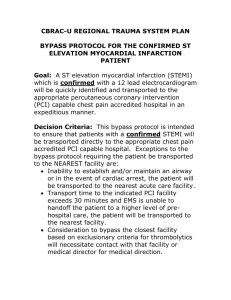
County of Los Angeles Department of Medicine HARBOR-UCLA MEDICAL CENTER Acute Coronary Syndrome Admitting Orders (STEMI) STEMI Clinical Pathway Order Form (STEMI = ST Segment Elevation MI) THE FIVE GOALS OF AMI THERAPY: 1. Door to drug time < 30 minutes or Door to balloon time < 90 minutes 2. Aspirin for all patients (clopidoprel 75mg QD if patient ASA sensitive). 3. Beta blockers in absence of contraindications. 4. ACE inhibitors if LVEF < 40% anterior MI, hypertension or diabetes 5. Lipid lowering therapy for all patients. INDICATIONS FOR REPERFUSION THERAPY (Thrombolysis or Primary PCI) 1. Chest Pain or equivalent suggesting AMI 2. AGE: 18 or greater. No upper age limit. 3. ECG: ST elevation of > 1 mm consistent with AMI in at least 2 or more contiguous leads or new or presumably new LBBB. 4. Time to therapy < 12 hours from continuous onset of chest pain 5. If thrombolytic therapy contraindicated or cardiogenic shock present, consider Primary PCI. Call Cardiology. Begin STEMI Clinical Pathway in ED ___________________ED- MD// Admission ID#_________________________ Date: _____________________ Criteria Time:_______________________ Admit: □ C-Team Obtain Bed: □ CCU/ICU Diagnosis: □ STEMI Obtain old chart on unit ASAP 1. Emergency NOTE: Call Housestaff for any of the following (see Transfer/Discharge Criteria): Interactions Chest pain > 5 min or recurrent chest pain; repeat ECG Any change in ST elevation or depression identified on monitor or with chest pain Symptomatic hypertension or B/P > 180/110; or ≥ 120 diastolic Heart rate < 35 or > 110 beats per minute or symptomatic bradycardia or ventricular arrhythmia T>38.4C 2. Activity Bedrest with bathroom privileges if pain free and VS stable Progress to ambulating as tolerated. 3. Nutrition Low fat/low carbohydrate (no added salt) 4. Assessment 5. Teaching Teach patient to verbalize chest pain or associated symptoms Discuss the pathway with the patient/family Other:_______________ Other___________________ Cardiac assessment upon admission by nurse Nursing assessment q 8h Vital signs q 4 L h or CCU/PCU standing orders Record BP and pulses in both arms on admission Cardiac monitor- Assess cardiac rhythm q 4 hours and with chest pain Alarm review per standard protocol Record Allergies________________________________________________ Physician signature and ID Number: _____________________________ Date: __________________________Time: _________________________ Nurse Signature: _______________________________________________ Date: __________________________ Time:________________________ PATIENT IDENTIFICATION County of Los Angeles HARBOR-UCLA MEDICAL CENTER Department of Medicine Acute Coronary Syndrome Admitting Orders (STEMI) STEMI Clinical Pathway Order Form 6. Medication Aspirin (enteric coated) 325 mg po and QD Metoprolol 5 mg IV over 2-5 min X3. If IV dose tolerated, start 50 mg PO orally. Goal: HR 60 bpm and no hypotension Nitroglycerin 1/150 tab Q 5min X3 if chest pain persists. (SL or spray) Morphine: PRN to control chest pain Statin: ______________________________________________ ACE Inhibitor for CHF or LV EF< 40%, hypertension or diabetes Enoxaparin 1 mg/kg SC Q12h - Avoid if creat >2.5 - Above 140kg, consider use of UFH Heparin Hospital protocol (Bolus 60/kg, max 4,000 units ; infusion 12 u/kg/hr, max 1000/hr) Contact Cath Lab Fellow for primary PCI or urgent Cath if pain and/or ischemia occurs on therapy TNK Protocol: lbs. kg. DOSE OF TNK (Reconstituted) <135 lbs <60 kg 6 ml (30 mg) ≥135 to <155 lbs. ≥60 to <70 kg 7 ml (35 mg) ≥155 to <175 lbs. ≥70 to <80 kg 8 ml (40 mg) ≥175 to < 200 lbs. ≥80 to < 90 kg 9 ml (45 mg) ≥200 lbs. ≥90 kg 10 ml (50mg) 7. Treatment Insert heplock O2 @ 2l/ min via nasal cannula X 24 hrs if O2 saturation < 90% 8. Labs/Test CBC, Chem. 7, fasting lipid panel, (INR/a PTT) Troponin at 0, 6 and 12 hours (If abnormal, repeat daily) CK-MB at 0, 6 and 12 hours (if abnormal, repeat daily) ECG at 0, 6 and 12 hours Chest x-ray (portable) Cardiac Cath Consult 9. Cardiac Rehab/ Discharge Planning 10. Other Orders: √ √ Coordinate outpatient follow-up Patient Education – Risk factors - Smoking cessation - Nutritional counseling - Activity levels - Low level Bruce, 4 mets, before discharge ______________________________________________________________________________ ______________________________________________________________________________ ______________________________________________________________________________ ______________________________________________________________________________ PATIENT IDENTIFICATION Physician Signature and ID Number: ___________________________________________ Date: _______________Time: ____________ Nurse Signature: ___________________________________ Date:_______________Time:_____________ STEMIAdmittform 12/31/2002 County of Los Angeles HARBOR-UCLA MEDICAL CENTER Department of Medicine ACUTE CORONARY SYNDROME DISCHARGE ORDERS (STEMI) I. Medications/Other Treatments Y N (ALL Highly Recommended) C (Check y = yes; n = not indicated; c = contraindicated) ASA _______________________________________________________ Beta Blocker_________________________________________________ Ace Inhibitor_________________________________________________ Statin ______________________________________________________ Smoking cessation counseling for current smokers Exercise 5-7 times 1 week; 30-45 minutes each time Dietary guidelines II. Outpatient follow-up Cardiology Clinic appointment in 1 week for Cardiac Rehab follow-up. Cardiology Fellow’s signature required. __________________________MD________________________ID#______________________ Other Clinic appointment__________________________________ All PCI patients referred to the Cath/Interventional Clinic EXT. 5146 If on Warfarin, enroll in Anticoagulation Clinic ext. 5146; Beeper #501-5559 III. Discharge Diagnosis/Codes AMI (NSTEMI and STEMI) Primary ACS Diagnosis Code Secondary or Other Co-Morbid Diagnoses STEMI - Anterolateral 410.0 Aortic Stenosis STEMI - Anterior STEMI - Inferolateral STEMI - Inferoposterior STEMI - Inferior STEMI - Lateral 410.1 410.2 410.3 410.4 410.5 STEMI -True posterior 410.6 Unstable angina 411.89 NSTEMI 410.07 Old MI 412 Chest pain –Non Cardiac Other 786.59 Cath - right heart 93501 Cath - left heart 93510 Angioplasty 92980 IABP 33967 Ventilator 94656 395.0 Diabetes: ● No insulin ● No insulin-PVD ● Insulin ● Insulin-PVD Heart failure Hyperlipidemia Hypertension Hypertension/CHF Obesity: ●< 100 kg ● > 100 kg Procedure Codes Code Pericarditis Pulmonary edema Pulmonary hypertension Renal failure – acute Renal failure –chronic Shortness of breath Smoking Warfarin 250.8 250.7 250.8 250.73 428.1 272.0 401.0 402.01 278.00 278.01 420.91 518 416 584.9 585 786.09 989.84 V58.6` Physician Signature and ID Number: _________________________________________ Date:_______________Time:__________________ Nurse Signature: _____________ _______________ Date:_______________Time:___________________ PATIENT IDENTIFICATION