Integumentary System
advertisement

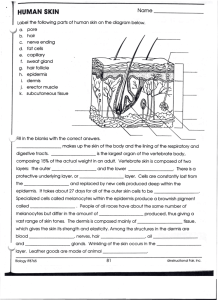
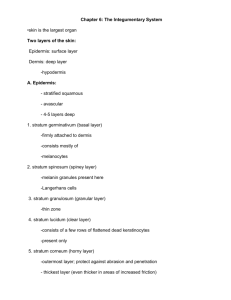
Integumentary System 1. List and describe the morphology and functions of the layers in the skin. Epidermis: Most superficial layer; composed of stratified squamous keratinized epithelial tissue, derived from ectoderm, avascular and consists of 5 well-defined layers. The epidermis is hard, can be sloughed off and readily replenished, can protect the underlying tissues from damage and invasion, etc. Dermis: Deepest layer of the skin; composed of connective tissues and fibers, blood supply is located here, glands and hair follicles extend down to this layer, etc. The dermis is derived from mesenchyme. Hypodermis: Not actually a part of skin, but often discussed with it. The hypodermis is actually the subcutaneous fascia and is made up of loose areolar connective tissue. There is often a great deal of fat stored in this layer – subcutaneous fat is called panniculus adiposus. 2. List and describe the morphology and arrangement of the layers and components in the epidermis, dermis and hypodermis. Epidermis (5 Layers): Pages 28-29. Dermis (2 Layers, Vascularized): Pages 38-40 (section B). Hypodermis: Described in previous objective. 3. List and describe the morphological and functional changes in epidermal cells as they move from the basal lamina to be sloughed off at the surface of the stratum corneum. Epidermal cells are called keratinocytes. They begin their journey to the surface from the stratum basale (germinativum), which is directly superficial to the basal lamina. The cells in the stratum basale are arranged in a single layer and are cuboidal to columnar in shape. It is this layer in which mitosis is primarily occurring. Small bundles of keratin, called tonofilaments or cytokeratin, first appear in this layer. These cells have desmosomes to attach to each other and hemidesmosomes to attach to the basal lamina. The primary function of this layer is proliferation. The cells in the stratum spinosum are arranged in several layers and are irregularly shaped. The cells are crossed by intercellular bridges (desmosomes) that are visible in preparation because the processing leads to shrinkage of these cells away from one another. The spaces that appear between the cells are crossed by these intercellular bridges, which look like spines. The large number of desmosomes in this layer helps hold the cells together in a unified sheet. This layer produces more keratin, which begins to fill the cytoplasm. The tonofilaments become organized into bundles called tonofibrils. Lamellar granules also appear in the cytoplasm – these are membrane-bound packets of light and dark bands that are extruded as the cells approach the next layer. The cells in the stratum granulosum are arranged in a narrow layer that is approximately 3-5 cells thick. The cells in this layer are more flattened and the nuclei have begun to disappear due to lack of nutrients. They stain darker due to the presence of numerous keratohyalin granules (not membrane-bound). The lamellar granules extruded from the cells as they enter this layer release a substance rich in glycolipids that surrounds the cells. This hydrophobic secretion forms a waterproof barrier between the cells – this also increases the intercellular space between cells. The tonofibrils are crosslinked by a protein called filaggrin in this layer. Involucrin, produced in the stratum spinosum, is crosslinked onto the cell membrane by the enzyme transglutaminase. This leads to the cell membrane becoming water impermeable, hastening cell death. The cells in the stratum lucidum are arranged in a thin layer that is 2-3 cells thick. Neither the individual cells nor the nuclei are visible, giving this layer a transparent (clear) appearance. This layer is actually the lower portion of the stratum corneum. The cells in this layer, which at this point are dead, are accumulating even more keratin in increasingly complex forms (such as eliden, a transformed keratohyalin granule). The cells in the stratum corneum are arranged in a very thick layer of dead cells that are completely filled with keratin. There are no visible nuclei in this layer, and these cells are sloughed off from the surface at reasonable regularity. The cells here are flattened and are called squames. They are arranged in tight proximity to one another to help facilitate the watertight barrier of the epidermis. The plasma membrane in this layer is also thickened with non-keratinous material, and no granules are visible in the squames. The stratum basale and spinosum are collectively known as the Stratum Malpighi. 4. List and describe the morphology and function of all cells in the epidermis. Keratinocytes are the principle cell type of the epidermis; they produce keratin and are derived from ectoderm. They change substantially as they process from the deepest layers up to the surface, and are responsible for maintaining the waterproof barrier of the epidermis. Melanocytes are the pigmented cells of the epidermis, and are found in the stratum basale with their processes projecting between neighboring cells. They are derived from the neural crest, and are involved in the conversion of tyrosine to melanin through a series of reactions using the enzyme tyrosinase. They are known as “clear cells” in light microscopy because they have no desmosomes and can form clear regions around themselves during preparation. There are approximately 800-1000 of these cells per mm2 in normal skin (1 in every 10 epidermal cells) and 2000 per mm2 in pigmented skin (about 1 in ever 4 epidermal cells). Pigmented skin is located on the face, forehead, areola and genitals. Langerhans cells are immune cells that are scattered throughout the stratum spinosum. They are stellate in shape and have many processes which project between neighboring cells (thus they are often called dendritic cells). They move freely within the stratum spinosum and are antigen presenting cells (they present antigens to T-helper cells) during hypersensitivity reactions such as contact dermatitis. Merkel cells are small, clear cells in the stratum basale. They contain dense core vesicles and are similar to the cells in the adrenal medulla (but do not contain catecholamines). They are individually innervated are function as slow-adapting cutaneous mechanoreceptors responsible for some of the sensation of light touch. 5. Describe the morphology of the epidermis / dermis junction and its functional significance. The epidermal-dermal junction is irregular (not flat) due to dermal papillae, which interdigitate with the epidermal pegs and / or ridges, preventing shearing forces from separating the two layers. In thick skin, the primary dermal ridges are divided into 2 secondary ridges by the Interpapillary pegs (rete pegs) of the epidermis. Dermal papillae extend up from the secondary ridges and cause even more interdigitation (see page 40). In thin skin, there are simple rounded bumps or mounds of connective tissue extending up into small recesses in the epidermis. The primary dermal ridges correspond to the epidermal ridges that you can see on your fingers and toes (friction ridges). These improve grip and can be studied in forensic medicine and criminology using the science of dermatoglyphics. 6. Define and describe the cleavage lines of Langer and their clinical significance. These are the predominant directions of the bundles of collagen fibers in the reticular layer of the dermis in a region of the body. They are clinically important because in surgery (especially plastic surgery), if the incision is made parallel to LL (Langer lines), the wound will not gap open. If the incision is made across these cleavage lines, the wound will gap open and leave a large scar. See page 41. 7. Describe the arrangement of the blood supply to the skin and relate it to temperature regulation. The blood supply of the skin is arranged in three longitudinal plexuses, which run parallel to the surface of the skin primarily. The subcutaneous plexus is the deepest and is located in the subcutaneous fascia (hypodermis). The cutaneous plexus is located at the dermal-subcutaneous junction. The subpapillary plexus is located in the papillary layer of the dermis and contains capillary loops which run up into the individual dermal papillae. In skin, you have A-V shunts (glomuses) that run parallel to the capillaries-- a coil of small vessels running from the arterioles to the venules that connect the two most superficial plexuses. When partially closed (as occurs normally), blood will run up near the surface in moderate amounts, maintaining current temperature conditions of the body. In high temperatures, partial dilation occurs so blood can reach the surface and release heat. Cold temperatures cause sympathetic innervation to fire, clamping down on AV shunts so the blood cannot reach the surface. Apical skin: Covers ears, nose, etc. Process above occurs. In Non-Apical skin, there are no A-V shunts: sympathetic nervous system causes release of norepinephrine, which prevents blood from reaching surface. In warm temperatures, acetylcholine release causes vasodilation. 8. List and describe the functions of the skin. The functions of the skin are listed on pages 27-28. 9. Integrate the morphology of the skin to its functions. Mechanical protection and maintenance of body fluids are provided by the junctions between cells, the numerous layers of cells and the secretions of hydrophobic materials into the intercellular spaces that help keep water out. This also helps prevent bacteria and other harmful agents from entering the body. Maintenance of body temperature is accomplished by sweat glands (water at the surface evaporates, cooling the body), blood vessels (AV shunts) and by adipose tissue (which provides insulation). The synthesis of vitamin D is accomplished by converting cholesterol in the superficial layers to precursors of the vitamin, which are transported to the liver and converted to another precursor, which is transported to the kidneys to finally produce vitamin D. Immunity is afforded by the Langerhans cells and by the ability of other wandering cells to enter the dermis and provide immunity. Sensory innervation and receptors provide us with feedback on stimuli of our environment and innervation along with vasculature change the appearance of the skin (embarrassment, cyanosis, jaundice, age and nerve damage). Repair is afforded by the ability of healing cells to come from the vasculature to the epidermis. 10. List and describe the arrangement and location of skin appendages (hair, glands, nails). Hair covers most of our body and is located in hair follicles which extend down into the dermis and hypodermis. Glands are located in many places in our body in the skin and either insert into hair follicles or develop as invaginations of the epidermis into the dermis. Nails are produced at the distal ends of each of our 20 digits and are modified epithelial structures. 11. List and describe the arrangement of the parts and layers of the hair and hair follicle. See section IV-A, pages 43-45. 12. Relate the layers of the epidermis to those of the hair follicle and nails. Hair follicle: The external root sheath is an extension of the strata basale and spinosum down around the hair follicle. The matrix of the follicle is the equivalent of the stratum basale. Nails: The nail bed is continuous with the stratum basale & granulosum of the epidermis, while the nail plate is a structure that replaces the stratum corneum in the nail (these keratinocytes are full of hard keratin, while normal stratum corneum is full of soft keratin). 13. Define and describe terminal, vellus and lanugo hair; give their distribution over the body. Terminal hairs are hard, large, coarse, long and dark – they cover the scalp and eyebrows, as well as the genital areas and are more common on males than females (95% of male body hair is this type). Vellus hairs are soft, fine, short and pale – they cover 65% of the female body and are located in the so called “hairless regions” of males. Lanugo hair is fine hair that is slightly thicker than vellus hair – it is present on the fetus and can also replace vellus hair in anorexics. 14. List the parts and describe the growth cycle of hair. Hair does not grow continuously and has 3 phases, making hair growth more complex than epidermal growth. It is cyclic in that hair is lost and replaced periodically. Growth Phase (Anagen): This involves the proliferation of the matrix; during this phase, the hair grows in length at a rate of about 0.4 – 0.5 mm per day. The growth phase is not the same length of time for all hair of the body – it is longest in the terminal scalp hair. Transitional Phase (Catagen): This short phase involves the stoppage of hair growth; the hair remains in the follicle for this stage. Resting Phase (Telogen): This short phase involves the hair shaft falling out of the follicle. Note that all individual hairs are in different phases of this cycle so that normally there is always some hair falling out. 15. List the parts and describe the process by which a hair shaft increases in length. The matrix of the follicle is where proliferation of the keratinocytes occurs, and cells are pushed superficially from this layer. As the cells make there way toward the surface, they pass through the keratogenous zone, where they become fully keratinized (with hard keratin). Melanocytes are also included in the medulla (center) of the hair, imparting pigment to the hair shaft. 16. Integrate the morphology of hair and its function. Hair is a hard, keratinous epithelial fiber. It is made up of a hair shaft, root and bulb which insert into the follicle of the skin. Hair is used to keep us warm and to keep things out of places where they shouldn’t go (such as keeping dust out of our eyes and nose). 17. List and describe the morphology, function and secretion of the 3 types of glands (sebaceous, sudoriferous (sweat), ceruminous). Sebaceous glands are attached to the follicles of hair. They can be simple or branched alveolar, and secrete using the holocrine method (the entire cell is filled with lipid substance, degenerates and becomes the secretion product). The sebum is them emptied into the upper hair follicle by a single duct. These glands can become infected by bacteria and lead to acne. There are two types of sudoriferous glands: Eccrine are the more numerous and secrete a serous secretion using the merocrine method. They are simple coiled tubular glands which are important for temperature excretion of ions, water, ammonia and urea. These glands can secrete up to 10 liters of sweat per day. Eccrine sweat glands contain clear cells (which secrete serous fluid), dark cells (which secrete mucous material) and myoepithelial cells (which have contractile ability and help expel the secretions from the gland). Apocrine sweat glands are less numerous and open into the hair follicles above sebaceous glands on some terminal hairs. They are also simple coiled tubular glands, but are larger than eccrine sweat glands. They also secrete a serous secretion using the merocrine method (MISNOMER – NOT APOCRINE METHOD!). They don’t start functioning until puberty and bacteria that act on these glands and there secretions can lead to the characteristic odors of the armpit and other regions where these glands are present. Ceruminous glands are modified apocrine sweat glands that secrete wax (cerumen) into the external auditory canal. 18. List the distribution of the different types of glands across the body. Sebaceous glands are located in areas where terminal hairs exist. Eccrine sweat glands are located all over the body (3-4 million in total). Apocrine sweat glands are located in the axilla, perineum (circumanal region) and pubic region. Ceruminous glands are located in the external auditory canal. 19. List and describe the morphology and function of the parts of nails. See pages 49-50. 20. List and describe the morphology, function and location of the sensory receptors of the skin (free epidermal nerve endings, Merkel endings, Pacinian corpuscles and Meissner’s corpuscles). See pages 51-52. 21. Define the describe the following terms: Stratum germinativum: Another term for stratum basale. Stratum granulosum: The middle layer of the epidermis, composed of granules, moderately keratinized. Keratinocytes: The primary cells of the epidermis, these cells are the ones that become the squames and are sloughed off and constantly replenished. Langerhans cells: These are immune cells of the epidermis which are usually in the stratum spinosum and are antigen-presenting cells. Keratinizing type: Keratin type a cell produces – skin is soft, nails and hair hard. Intercellular bridges: These are the “spines” in the stratum spinosum, and are actually just visible desmosomes processes between cells in this layer. Thick skin: Also called glabrous skin, this skin has thicker epidermis (more than 1 mm thick) and is thickest on palms and soles. This skin lacks hair and sebaceous glands. Squames: These are another name for the flattened squamous cells in the stratum corneum. Corneum: Literally means leather – in Latin it refers to the dermis. Epidermal ridges: These are raised lines on the skin that indicate the location of primary dermal ridges under the epidermis. Subpapillary plexus: This is the most superficial plexus of capillaries in the skin, with loops that project into the dermal papillae. Root of hair: This is the portion of the hair that reaches from the center of the follicle down to the bulb. Arrector pili muscle: Muscle that attaches from the dermal papillae nearby to the follicle; during contraction is stands the hair erect and causes goose bumps by pulling the dermal papillae down. Differentiation zone: The zone just above the matrix of the hair follicle. Cuticle of hair: This is the outermost layer of the hair shaft and is composed of hard keratin. Sebum: This is the oily secretion produced by sebaceous glands. Stratum Basale: This is the deepest layer of the epidermis and consists of a single layer of keratinocytes in constant mitotic division to produce more cells as the cells of the stratum corneum are sloughed off. Stratum Lucidum: This is the deeper portion of the stratum basale where the cells appear clear and indistinct with no nuclei under light microscopy. They are full of keratin, however. Melanocytes: These are cells of the epidermis that lie in the stratum basale and are responsible for converting tyrosine to melanin, which imparts color to the keratinocytes. Papillary layer: This is the superficial layer of the dermis and is the portion where undulations of the dermis called dermal papillae exist. The connective tissue of this layer is modified areolar (loose) connective tissue. Prickle cells: Name for a cell of the stratum spinosum, indicating its spiny appearance. Keratohyalin granules: Basophilic, non-membrane-bound, irregularly shaped inclusions in the stratum granulosum. Thin skin: Also called hairy or non-glabrous skin, this skin has hair and sebaceous glands, has a reduced stratum corneum, granulosum and spinosum and has no stratum lucidum. It is located everywhere in the body that does not have thick skin. Clear cells: These are the cells in eccrine sweat glands that secrete serous solution. These can also be the name of Melanocytes at the LM level, because they produce a clear area around themselves. Interpapillary pegs: These are the projections of epidermis that lie between the dermal ridges. Cutaneous plexus: This is the plexus of capillaries that exists at the dermal-subcutaneous junction. Hair follicle: Tubular invagination of the epidermis down through the dermis into the hypodermis, surrounded by connective tissue and containing the hair and the root sheaths. Dermal sheath: The connective tissue surrounding the follicle. Outer (external) root sheath: extension of the strata basale and spinosum down into the skin. Cortex of hair: The part of the hair that makes up the bulk of the shaft and consists of hard keratin. Sweat: Mixture of serous and mucous secretion from sudoriferous glands. Contusion: Another name for a bruise. Eczema: Common skin disorder that is characterized by edema, exudation and crusting, along with severe itching (pruritus). The dermis is also affected and immune cells can infiltrate this region more than normal. For this reason, this disease is thought to have an immunological origin. Nail bed: Portion of the epidermis over which the nail plate lies – composed of / continuous with the strata basale and granulosum. Eponychium: Cuticle of the nail at the root (flap of skin that grows over nail). Stratum Spinosum: Layer just superficial to stratum basale, consists of prickle cells that have intercellular bridges visible due to the numerous desmosomes. Stratum Corneum: Most superficial layer, consisting of highly keratinized squames which are sloughed off and replaced from the bottom up. Merkel cells: These are cells that exist in the stratum basale and are individually innervated to allow for the sensation of light touch. Reticular layer: This is the deeper of the two layers of the dermis and is made up of irregular dense connective tissue. Desmosomes: Intercellular junctions which bind the cells of the epidermis together and cause the cells to be tightly associated with one another. Keratin: Large MW fibrous protein that is present in many of the integumentary cells and structures and imparts hardening and waterproofing of structures. Lamellar granules: These are granules that are produced in the stratum spinosum that extrude their contents into the intercellular space to provide hydrophobic waterproofing. Melanosome: Vesicles full of melanin on their way into the keratinocytes through the processes of the melanocytes. Dermal papillae: Undulations of dermal tissue which stick up into the epidermis. Melanin: Brown pigment produced by the skin from the action of tyrosinase. Hair shaft: Portion of hair from the center of follicle up to the tip of the hair. Bulb: The enlargement at the deep end of the hair follicle, with the dermal papilla (connective tissue) pushing into its deepest margin. Inner root sheath: Area of the root that is derived from the outside region of the follicle matrix – it contains soft keratin and disappears half way up the follicle. Medulla of hair: The center of the hair shaft, consisting of soft keratin. Solar elastosis: Degeneration of the elastic tissue of the skin in sun-exposed patients, particularly older patients. UVA: 320 nm, causes increased wrinkling and sagging of skin, increases chance of skin cancer and does not burn the skin – thus, most tanning salons use this. UVB: 370 nm, causes inflammation of the BVs in the dermis and causes sun burning. Most sunscreens block this wavelength, but they should block both. Nail plate (body): The main body of the nail, composed of keratinocytes containing large amounts of hard keratin. It replaces the stratum corneum. Nail matrix: The portion of the nail root where keratinocytes proliferate. Nail root: The proximal portion of the nail. Decubitus ulcers: Also known as bedsores, these are ulcers of the skin that are caused by compromised circulation to an area of skin. Basal cell carcinoma: Most common type of all skin cancers, affecting only the keratinocytes in the basal layer of the epidermis. These carcinomas destroy local tissue but do not readily metastasize. Acne: Inflammation of sebaceous glands and associated hair follicles due to bacterial infection of them. Lunula: The whitened crescent of the nail at the proximal end, where proliferation is occurring. Hyponychium: Portion of epidermis growing under the distal end of the nail plate. Psoriasis: Chronic skin condition characterized by patches of red-brown area with whitish scales – the cause is complex. The direct cause is proliferation of keratinocytes – they reach the surface far too quickly. The integrity of the epidermis is compromised because lamellar granules are not secreted. Squamous cell carcinoma: Second most common skin cancer, this carcinoma affects the squamous keratinocytes and can be caused by a variety of factors such as exposure to UV radiation, X-rays, chemical agents and arsenic. It readily metastasizes. Malignant melanoma: Carcinoma of the melanocytes and extremely malignant. Sunburn: Burn of the skin caused by excessive exposure to UV radiation, leading to inflammation of the blood vessels in the dermis of the exposed skin. Nevus: Benign localized overgrowth of melanocytes arising during early life. Phemphigus: Potentially fatal skin disease caused by autoimmune disorder targeting desmosome proteins in epidermis – severe blistering and loss of fluids, as well as easy infection. Melanin-epidermal unit: Single melanocyte and its associated keratinocytes. Vitiligo: Depigmentation disorder which is genetically inherited defect in skin an hair – characterized by scattered patches of white skin and hair (from destruction of melanocytes). Can be treated cosmetically or using hydroquinone to reduce formation of melanin in normal skin. Albino: Person without tyrosinase but with normal number of melanocytes – has unpigmented skin, hair and eyes. Striae: Stretch marks, caused by tearing of the dermis with the epidermis remaining intact. This leads to the gap being repaired with scar tissue and the tear showing through the epidermis as a cosmetic defect. EPU: One stem cell in the basal layer and the 10-11 basal cells it produces that migrate to the periphery. Keratogenous zone: This is where the cells become fully keratinized in the hair follicle as they move upward.