1 ANTIVIRAL AGENTS Steps for Viral Replication 1) adsorption and
advertisement
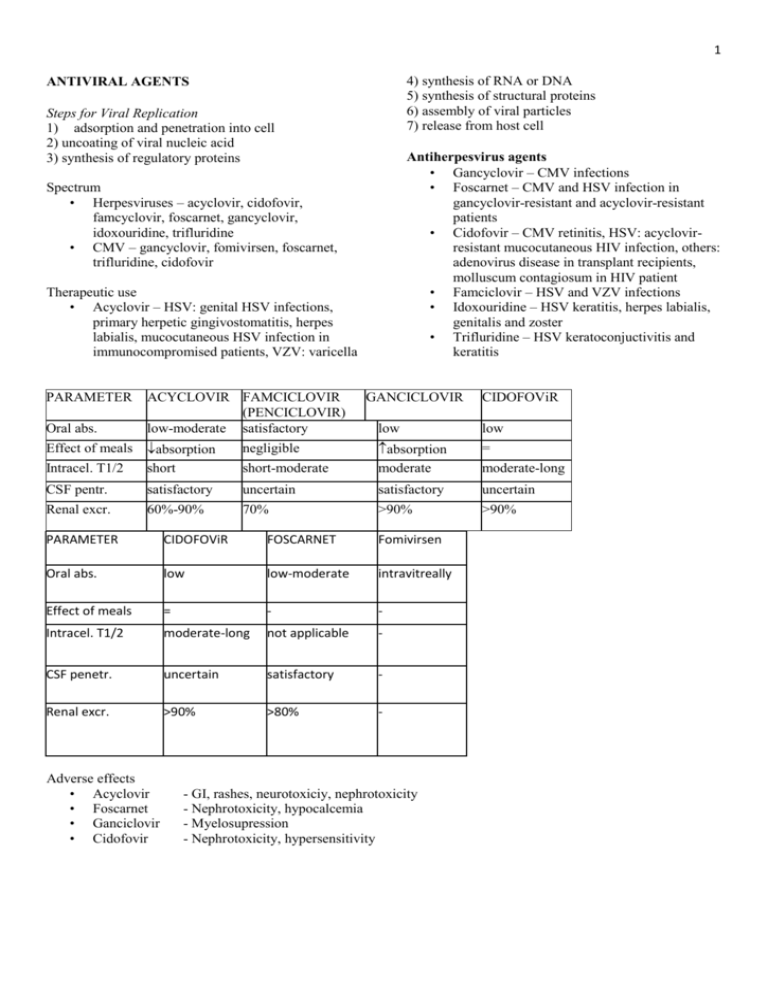
1 4) synthesis of RNA or DNA 5) synthesis of structural proteins 6) assembly of viral particles 7) release from host cell ANTIVIRAL AGENTS Steps for Viral Replication 1) adsorption and penetration into cell 2) uncoating of viral nucleic acid 3) synthesis of regulatory proteins Antiherpesvirus agents • Gancyclovir – CMV infections • Foscarnet – CMV and HSV infection in gancyclovir-resistant and acyclovir-resistant patients • Cidofovir – CMV retinitis, HSV: acyclovirresistant mucocutaneous HIV infection, others: adenovirus disease in transplant recipients, molluscum contagiosum in HIV patient • Famciclovir – HSV and VZV infections • Idoxouridine – HSV keratitis, herpes labialis, genitalis and zoster • Trifluridine – HSV keratoconjuctivitis and keratitis Spectrum • Herpesviruses – acyclovir, cidofovir, famcyclovir, foscarnet, gancyclovir, idoxouridine, trifluridine • CMV – gancyclovir, fomivirsen, foscarnet, trifluridine, cidofovir Therapeutic use • Acyclovir – HSV: genital HSV infections, primary herpetic gingivostomatitis, herpes labialis, mucocutaneous HSV infection in immunocompromised patients, VZV: varicella PARAMETER Oral abs. ACYCLOVIR FAMCICLOVIR (PENCICLOVIR) low-moderate satisfactory GANCICLOVIR CIDOFOViR low low = negligible Intracel. T1/2 absorption short short-moderate absorption moderate CSF pentr. satisfactory uncertain satisfactory uncertain Renal excr. 60%-90% 70% >90% >90% Effect of meals PARAMETER CIDOFOViR FOSCARNET Fomivirsen Oral abs. low low-moderate intravitreally Effect of meals = - - Intracel. T1/2 moderate-long not applicable - CSF penetr. uncertain satisfactory - Renal excr. >90% >80% - Adverse effects • Acyclovir • Foscarnet • Ganciclovir • Cidofovir - GI, rashes, neurotoxiciy, nephrotoxicity - Nephrotoxicity, hypocalcemia - Myelosupression - Nephrotoxicity, hypersensitivity moderate-long 2 Antiretroviral agents Nucleoside RT inhibitors Nonnucleoside RT inhibitors HIV protease inhibitors Entry inhibitors Fusion inhibitors Integrase inhibitors Nucleoside RT inhibitors – bind to the catalytic site of the enzyme ZIDOVUDINE LAMIVUDINE STAVUDINE DIDANOSINE Oral bioavailability satisfactory excellent excellent satisfactory Effect of meals (high fat) (acidity) Intracellular T1/2 3-4 12 3.5 8-24 Metabolism intensive moderate intensive moderate Renal excr. % 15 70 40 20-50 ABACAVIR ZALCITABINE TENOFOVIR EMTRICITABE Oral bioavailability good excellent acceptable excellent Effect of meals (fat) Intracell. T1/2 3 2-3 11-49 39 Metabolism intensive mild negliglible negliglible Renal excr. % <5 70 80 80 Adverse effects • Zidovudine - anemia, granulocytopenia, malaise, myalgia, nausea, insomnia, hyperpigmentation, lactic acidosis-steatosis syndrome • Didianosine, stavudine - neuropathy, pancreatitis, diarrhea • Zalcitabine - nephropathy • Lamivudine - well tolerated • Abacavir - hypersensistivity • Tenofovir - well tolerated, flatulence 3 Nonnucleoside RT inhibitors - bind to the site distant from the catalytic site of the enzyme PARAMETER NEVIRAPINE EFAVIRENZE DELAVIRDINE Oral bioavailability Plasma protein binding, % Metabolism Renal excretion (%) excellent 60 Extensive Negliglible satisfactory 99 Extensive Negliglible excellent 98 Extensive Negliglible Adverse effects Rashes, sedation, hepatotoxicity Attention: cytochrome P450 HIV protease inhibitors • Saquinavir, ritonavir, indinavir, nelfinavir, amprenavir, lopinavir, atazanavir • Active against HIV-1 and HIV-2 • Mechanism: inhibit protease which is responsible for cleaving precursor molecules necessary to produce final structural proteins of the virion core • Pharmacokinetics: bioavailability depends on preparation, high protein-bound, metabolized in the liver, CNS penetration (indinavir) • Adverse effects: altered body fat distribution, insulin resistance, dyslipidemia, liver function impairement, GI symptoms, nephrolithiasis (Indinavir), skin rashes Fusion inhibitors - enfuvirtide Blocks gp 41 subunit of the viral envelope glycoprotein – involved in fusion Active: against HV-1 Pharmacokinetics: given parenterally only Adverse effects: injection-site reactions Integrase inhibitors - Raltegravir Immune reconstitution syndrome - patients treated with combination antiretroviral therapy, which may include raltegravir-containing regimens. During the initial phase of treatment, a patient whose immune system improves may develop an inflammatory response to indolent or residual opportunistic infections (e.g., Mycobacterium avium, cytomegalovirus, Pneumocystis pneumonia, tuberculosis, varicella zoster virus), which may necessitate further evaluation and treatment Entry inhibitors - Maraviroc Inhibitor of CCRT coreceptor Caution: patients with liver dysfunction (CYP2A4) and at increased risk of cardiovascular events Antiinfluenza Agents AMANTADINE RIMANTADINE ZANAMIVIR OSELTAMTViR Type of influenza A Route Oral A Oral A,B Inhaled A,B Oral Oral abs. moderateexcellent excellent negliglible very good Metabolism < 10% ~75% Negligible Negligible Renal excr. % 50%-90% ~25% 100% 95% Neuraminidase inhibitors • Active against influenza virus A and B • Mechanism: inhibit neuraminidase which is an essential viral glycoprotein for replication and release • Adverse effects: well tolerated • Therapeutic use: uncomplicated influenza infection, given intranasally (z) or orally (o) 4 Anti-hepatitis agents Lamivudine -Nucleoside Reverse Transcriptase Inhibitor (NRTI) Adefovir -Nucleotide Inhibitor Interferon Alfa Pegylated Interferon Alfa Ribavirin Interferon Alfa Intracellular effects 1. Transcription inhibition (inhibits Mx protein and mRNA synthesis) 2. Translation inhibition: activated 2’-5’oligoadenylate [2-5(A)] synthetase – vRNA cleaved, protein kinase - intiation of mRNA inhibited, phosphodiesterase – tRNA function blocked 3. Proteins posttranslational modyfication glycosylation of proteins inhibited 4. Inhibition of virus maturation – glycoproteins maturation inhibited, changes in membrane – budding inhibited Spectrum - Most of viruses except few of DNA types Pharmacokinetics - parenerally only, given 3-times weekly, pegIFN (polyethylene glycol) once a week, steady-state levels 5-8 weeks after initiation of weekly dosing, eliminated by the liver and/or kidneys (endstage renal disease) Therapeutic uses - chronic hepatitis type C and B Adverse effects • Influenza-like symptoms • Bone marrow depression • Autoimmune effects: hypothyreosis • Neurotoxicity: somnolence confusion, behavioral disturbances, neurasthenia, depression • Hair loss • Nephritis • Cardio, - hepatotoxicity • Impaired fertility Ribavirin Mechanism of action: intracellulary phosphorylated • Inhibits inosine-5’-dehydrogenase – synthesis of GTP • Inhibits GTP-dependent 5’capping of viral mRNA • Inhibits influenza virus transcriptase • Enhances viral mutagenesis – lethal mutagenesis Spectrum: Influenza and parainfuenza viruses, RSV, HCV, adenoviruses, paramyxoviruses, arenaviruses, bunyaviruses, flaviviruses Pharmacokinetics: well absorbed, large volume of distribution, hepatic metabolism and renal elimination Therapeutic use: chronic HCV infection, RSV bronchiolitis and RSV pneumonia in children (aerosol), in immunocompromised patients, occasionaly – influenza, vaccinia, parainfuenza, measles, Lassa fever, SARS, Congo hemorrhagic fever Adverse effects: irritation, wheezing, anemia (hemolysis and bone marrow depression), nausea, insomnia, depression, embryotoxic, teratogenic and oncogenic (cat. X) Adefovir Spectrum – HBV • inhibits DNA polymerase and reverse transcriptases, serves as chain terminator Pharmacokinetics: well absorbed, small volume of distribution, eliminated by the kidneys Adverse effects: nephrotoxicity, diarrhea, hepatitis exacerbation, genotoxic, embryotoxic Therapeutic use: chronic HBV infections Imiquimod • Topical treatment of condylomata acuminata (genital and perisanal warts) • Induces cytokines with antivirial and immunomodulatory effects • Skin irritations