Drugs for Non HIV Viral Infecti
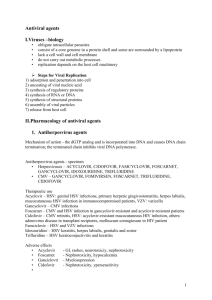
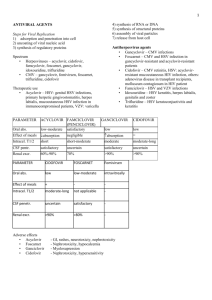
advertisement

Drugs for Non-HIV Viral Infections Paul Lewis, PharmD Infectious Diseases Pharmacy Resident Possible Sites of Action Viral attachment Cell entry Transcription Translation Viral assembly Drugs for HSV and VZV Oral Agents Topical Agents Acyclovir Acyclovir Valacyclovir Docosanol Famciclovir Penciclovir Ophthalmic Trifluridine Acyclovir Mechanism of Action Inhibition of viral synthesis of DNA Uptake by infected cell Virus-specific thymidine kinase phosphorylates to acyclovir monophosphate Cellular enzymes convert to acyclovir triphosphate Competes with deoxyguanosine triphosphate for viral DNA polymerases Lacks 3’-hydroxyl group Chain termination Inactivates the viral DNA polymerase Acyclovir (Zovirax®) Guanosine analog Topical, oral, and intravenous formulations Spectrum: Herpes simplex 1 and 2, varicella-zoster virus, possibly the EpsteinBarr Virus Treatment of choice for visceral, disseminated, or central nervous system involvement Acyclovir Adverse effects Phlebitis Reversible renal toxicity Crystalization in the renal tubules Neurological symptoms Encephalopathic changes such as somnolence, hallucinations, confusion coma GI symptoms Headache TTP/HUS Photosensitivity Anemia Valacyclovir (Valtrex®) L-valyl ester prodrug of acyclovir Rapidly and almost completely converted to acyclovir Available orally only Spectrum: similar to acyclovir Adverse effects: headache, nausea, weakness, dizziness, confusion Famciclovir (Famvir®) Cyclic guanine analog Converted to pencyclovir in the liver and intestines Available orally only Spectrum: HSV 1 and 2, VZV, to a lesser extent, EBV, in vitro activity to HBV Adverse effects: headache, GI, abnormal LFT’s Acyclovir Resistance Defined as MIC > 2-3 mcg/mL Mostly occurs in immunocompromised host 4-14% Three basic resistance mechanisms exist: Reduced or absent thymidine kinase (compared to 0.1-0.7% in immunocompetent) Most common Less neurovirulent and unable to reactivate Altered TK substrate specificity Alterations in DNA polymerase Cross resistance to famciclovir and valacyclovir Famciclovir Resistance Mutations in viral TK or DNA polymerase Cross resistance with acyclovir in TK negative strains May still have activity in TK altered strains Resistance to HBV is due to the point mutation L528M (viral DNA polymerase) Also associated with lamivudine resistance Dosing for HSV Acyclovir Valacyclovir Famciclovir Primary Genital Recurrent Genital Chronic Suppressive Encephalitis 400 mg PO TID X 10d 1 g PO BID X 10d 400 mg PO TID X 5d 500 mg PO BID 125 mg PO X 5d BID X 5d 200-400 mg PO BID-TID 500-1000 mg PO QD 10-15 mg/kg IV Q8hrs NA 250 mg PO TID X 5-10d 125-250 mg PO BID NA Dosing for VZV Drug Dosage Varicella Duration Acyclovir 20 mg/kg (max 800) PO QID 5 days Valacyclovir Herpes Zoster 1 g PO TID 7 days Famciclovir 500 mg PO TID 7 days Acyclovir 800 mg PO 5X/d 7-10 days Varicella or Zoster in Immunocompromised Acyclovir 10 mg/kg IV Q8h 7 days Other Topicals for HSV Orolabial herpes Penciclovir (Denavir® 1% cream) Topical guanine analog similar to acyclovir Apply every 2 hours while awake Docosanol (Abreva® OTC) Active against a broad range of lipid-envelop viruses MOA: interferes with viral fusion to host cell Apply 5X per day until healing (up to 10 days) Shortens healing time by 0.7 days HSV Keratoconjuctivitis Trifluridine (Viroptic® 1% ophthalmic) 1 drop q2h (max 9 drops/day) Active against acyclovir resistant strains Also active against vaccinia virus and smallpox Anti-CMV Agents Ganciclovir Valganciclovir Foscarnet Cidofovir Ganciclovir Mechanism of Action Competes with deoxyguanosine triphosphate similar to acyclovir However in CMV, viralencoded phosphotransferase converts to ganciclovir triphosphate Unlike acyclovir, ganciclovir contains a 3’-hydroxyl group, allowing for DNA to continue Ganciclovir (Cytovene®) Oral, intravenous, and intraocular Spectrum: CMV (10X potency of acyclovir) EBV (10X potency of acyclovir) HSV/VZV (equal to acyclovir) Human Herpesvirus 6 Ganciclovir Adverse effects: reversible pancytopenia (most common) Fever Rash Phlebitis, Confusion Renal dysfunction Psychiatric disturbances Seizures Vanganciclovir (Valcyte®) L-valyl prodrug of ganciclovir Available orally only Quickly hydrolysed after absorption Spectrum: similar to ganciclovir Adverse effects: similar to ganciclovir (Val)ganciclovir Resistance Mutations in the viral protein kinase (UL97) Responsible for monophosphorylation Confers resistance to ganciclovir alone Mutations in the viral polymerase gene (UL54) May show cross resistance to similar antivirals Foscarnet – Mechanism of Action Trisodium phosphonoformate hexahydrate Does not require thymidine kinase Works on HSV strains deficient of this enzyme Selective inhibition at the pyrophosphate binding site on virus-specific DNA polymerase Inorganic pyrophosphate analog Noncompetetive inhibitor Does not affect cellular DNA polymerase Resistance by alterations to viral DNA polymerase Not caused by thymidine kinase alterations Does not cause cross resistance to ganciclovir or cidofovir Foscarnet (Foscavir®) Intravenous only – controlled infusions Spectrum: CMV including ganciclovir resistant strains, acyclovir resistant HSV or VZV, EBV, Influenza A and B, HBV, and HIV Adverse effects: renal dysfunction (common, can require dialysis), NV, anemia, CNS disturbances, electrolyte abnormalities, seizures, arrhythmias, neutropenias Reduction of renal failure Saline loading (adequate hydration) Appropriate renal dosing adjustments Avoidance of concurrent nephrotoxic medications Cidofovir – Mechanism of Action Acyclic nucleoside phosphonate derivative Phosphorylation not dependant on viral kinases May actually enhance activity to TK deficient strains Selective inhibition of CMV DNA Active drug as cidofovir diphosphate DNA polymerase Incorporation into viral DNA chain results in reductions of the rate of viral DNA synthesis Cidofovir (Vistide®) Available intravenous only Spectrum: CMV including acyclovir and foscarnet resistant strains, HSV 1 and 2, VZV, EBV, HHV-6, HHV-8 Also has activity against DNA viruses: papilloma virus, polyomavirus, poxvirus, and adenovirus Must be avoided in preexisting renal impairment Adverse effects: nephrotoxicity (dose-limiting), neutropenia, metabolic acidosis Must be given with adequate hydration and PO probenecid---see labeled dosing directions Cidofovir Resistance Due to point mutations in viral DNA polymerase in CMV, pox, and adenovirus Confers resistance to ganciclovir in CMV Foscarnet activity not affected by cidofovir resistance Still active against UL97 mutation Not active against the UL54 mutation Dosing for CMV Load Maintenance Ganciclovir 5mg/kg IV q12 X 14-21 days 5 mg/kg IV daily 1 g PO TID Valganciclovir 900 mg PO BID X 21 days 900 mg PO daily Foscarnet 90 mg/kg IV q12 X 14-21 days 90-120 mg/kg IV daily Cidofovir 5 mg/kg IV qwk X 2 doses 5 mg/kg IV every 2 weeks Dosing for Resistant HSV/VZV Drug Dosage Duration Acyclovir-Resistant Herpes Simplex (severe infection, immunocompromised) Foscarnet 40 mg/kg IV q8hrs 14-21 days Acyclovir-Resistant Zoster (not FDA approved) Foscarnet 40 mg/kg IV q8hrs 10 days Hepatitis B Agents Interferon alfa-2b/-n3/-2a Peginterferon alfa-2a/-2b Entecavir Adefovir Telbivudine Lamivudine/ Emtricitabine Tenofovir Interferons Discovered in 1957 for their antiviral effects Glycoproteins Interferes with viral growth Responsible for complex antiviral, immunomodulating, and antiproliferative effects Three classes (α, β, and γ) Each distinct Different producer cells, inducers, and biologic effects INF-α and –β are produced by nearly all cells in repsonse to invasion Only INF-α has been approved for viral treatment INF- γ only produced by T cells and NK cells Interferons Mechanism of action Not directly virucidal or virustatic Induces changes in the infected or exposed cell to promote resistance to the virus Induces several enzyme activities that promote an antiviral state Proteins that inhibit synthesis of RNA Proteins that cleave viral DNA Proteins that inhibit mRNA Alterations of the cell membrane that inhibit the release of replicated virions Interferon Alfa HBV Parenteral or subcutaneous administration Pegylated similar or slightly better than conventional Combination therapy not superior to monotherapy HCV Subcutaneous administration preferred Given in combination with ribavirin Herpes Systemic not associated with lesion reduction Topical may have efficacy with trifluridine in drugresistant mucocutaneous HSV Interferon Alfa HIV Papillomavirus High doses have shown to induce responses Kaposi’s May have dose-related antiretroviral effects May benefit HIV-related thrombocytopenia and eosinophilic folliculitis Intralesional and systemic admin associated with regression of anogenital warts Respiratory Viruses Broad spectrum of activity in preventing respiratory viruses Except adenoviruses Has been used to treat SARS coronavirus Interferon Alfa Adverse Effects Flu-like syndrome Fevers/chills Headache Malaise Myalgia/arthralgia NVD Local reactions Bone marrow suppression Thyroid dysfunction Neuropsychiatric disturbances Depression Anxiety Somnolence Behavioral disturbances Fatigue/anorexia Seizures Cardiotoxicity Pulmonary toxicity Entecavir (Baraclude®) Deoxyguanosine analog Available orally only More potent than lamivudine Some activity against 3TC resistant HBV at higher doses Should not be used to treat HBV/HIV coinfection when HIV treatment deferred Adverse effects: Generally well tolerated Headache, fatigue, NVD, cough, myalgia Adefovir Dipivoxil (Hepsera®) Phosphonate nucleotide analog Converted to the diphosphate form Competes with deoxyadenosine triphosphate Inhibits viral DNA polymerase Inhibits reverse transcriptase Chain terminator of DNA synthase Available orally only Activity includes HBV resistant to lamivudine and entecavir, HIV, pox, HSV Adefovir Should not be used to treat HBV/HIV coinfection when HIV treatment deferred Adverse effects: Well tolerated Asthenia, headache, diarrhea, ab pain Nephrotoxicity at higher doses Resistance to HBV DNA polymerase by N236T or A181V Hepatitis C Agents Ribavirin Pegylated interferon Ribavirin Purine nucleoside analog Mechanism of action not fully understood Causes alterations to cellular nucleotide pools Inhibits viral RNA synthesis Lethal mutagenesis of certain RNA viral genomes Possibly acts as an analog of guanosine or xanthosine Possibly results in neutralizing antibody response (RSV) Resistance only documented in Sindbis virus and HCV Point mutation F415Y RNA polymerase identified Ribavirin Available orally and via inhalation Intravenous and intraventricular available through the CDC Spectrum: RNA and DNA viruses including influenza A and B, mumps, measles, parainfluenza, HSV, togavirus, bunyavirus, adenovirus, coxsackievirus, RSV, Hepatitis A, B and C Data also available for hemorrhagic fever, Lassa fever, and Hantaan virus Ribavirin Adverse Effects Hemolytic anemia Respiratory deterioration Depression Suicidal ideation Bacterial infections Psychiatric effects Anxiety Fatigue Dizziness Influenza Agents Oseltamivir Zanamivir Amantadine Rimantadine Oseltamivir (Tamiflu®) Oral neuraminidase inhibitor Cleaves terminal sialic acid residues on glycoconjugates and destroys receptors Newly formed virions adhere to cell surface and limit spread Spectrum: Infuenza A and B in both children and adults, avian influenza, H5N1 disease Adverse effects: NV, headache Zanamivir (Relenza®) Neuraminidase inhibitor Given via inhalation Spectrum: Uncomplicated influenza A and B, some strains of avian influenza, possibly effective for H5N1 Adverse effects: nasal and throat discomfort, bronchospasm Amantadine (Symmetrel®) Rimantadine (Flumadine®) MOA: Prevents the release of viral nucleic acid into host cell Spectrum: Influenza A, however resistance is frequent Adverse effects: Seizures, anticholinergic, CNS, edema, blurry vision Not currently recommended in the US Papillomavirus Options Imiquimod Podofilox Trichloroacetic Acid Podophyllin Cryotherapy Imiquimod (Aldara®) Imidazoquinoline compound Immunomodulator Activates immune cells (monocytes, macrophages, NK cells) Topical treatment Produces antiviral cytokines (IFN-α, TNF-α, and various interleukins Indirectly activates APC’s including Langerhan’s cells and T-helper cells 5% cream 3X per week (for 8 hours) for 16 weeks Can be used as adjunctive therapy with laser or surgical tx Spectrum: External and perianal genital warts by HPV Adverse effects: Site reactions (pain, erythema, scarring, and pruritis) No systemic reactions reported Podofilox (Condylox®) Also known as podophyllotoxin Exact mechanism not known Topical treatment Main ingredient in podophyllin 0.5% solution or gel every 12 hours for 3 days then withhold for 4 days, repeat up to 4 times Similar in efficacy to imiquimod but more adverse effects Adverse effects Localized pain, burning, inflammation, and erosion Reported in over 50% Systemic effects not reported Trichloroacetic Acid (Tri-Chlor®) Keratolytic agent Given topically 80% Liquid Powder for reconstitution