Circulatory System Study Guide: Blood & Circulation
advertisement

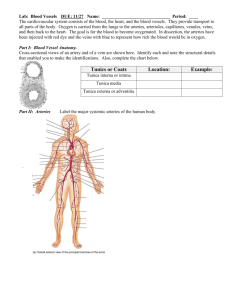
Unit J: Circulation & Blood BASIC FUNCTIONS OF THE CIRCULATORY SYSTEM 1. 2. 3. 4. Transports oxygen from lungs to tissue Transports carbon dioxide from tissue to lungs Absorbs and transports nutrients from small intestine to tissues Absorbs and transports water from stomach, small and large intestine to tissues and lungs 5. Carries waste products (urea, ammonia…) to kidneys for removal 6. Transports hormones from glands to target organs 7. Distributes body heat from internal source to peripheral skin for dissipation 8. Maintains pH in tissues (acts as a buffer with HHb) 9. Regulates fluid levels in tissues (along with the Lymphatic system) 10. Seals punctures in the skin or elsewhere by forming a blood clot; thus, preventing loss of blood and body fluids 11. Fights infection; involved in body defense A. The Five Types of Blood Vessels Basis of Comparison Arteries Arterioles Capillaries Venules Veins 1. 2. 3. 4. 5. Function Transport blood AWAY from the heart Control blood flow to capillaries Interconnect arterioles to venules Drain blood from capillaries and join to form a vein Transport blood TOWARDS the heart ARTERIES: (see page 226) ARTERIOLES: (see page 227) CAPILLARIES: (see page 241) VENULES: (see page 227) VEINS: (see page 226) Structure Location Thick, elastic walls Usually deep, along bones Thick, elastic walls, precapillary sphincters, thinner walls Very thin (1 cell thick) walls Leading towards all capillaries Thinner walls than veins Thin walls; contain valves Everywhere; within a few cells of each other Often on the surface Often on the surface surrounded by skeletal muscle Circulatory Pathways: Systemic Circulation: the system of blood vessels that delivers oxygenated blood to the body systems. Pulmonary Circulation: the system of blood vessels that delivers deoxygenated blood to the lungs to be replenished with oxygen. *What’s the big deal? The systemic arteries carry oxygenated blood. The pulmonary arteries carry deoxygenated blood. B. The MAJOR BLOOD VESSELS OF THE BODY Aortic Arch 1. AORTA: This major blood vessel carries oxygenated blood from the left ventricle to the body systems. When the aorta leaves the left ventricle, it loops over the top of the heart, creating the AORTIC ARCH, and descends along the inside of the backbone, creating the DORSAL AORTA. Other arteries branch off this main artery to ‘feed’ the body cells. Dorsal Aorta Superior Vena Cava 2. VENA CAVAS The superior and inferior vena cavas are the largest veins in the body. They are the location where all other veins converge to. All veins from above the heart drain into the superior vena cava while blood from below the heart is collects in the inferior vena cava Inferior Vena Cava 3. CORONARY ARTERIES/VEINS: The very first branches of the aorta are the coronary arteries (relatively small blood vessels that FEED the heart muscle). WHY CAN’T THE HEART JUST GET ITS OXYGEN AND NUTRIENTS FROM THE BLOOD THAT PASSES THROUGH IT? The muscle tissue is too dense and thick, and the blood travels though it too quickly for diffusion to occur. 4. CAROTID ARTERIES: These arteries branch off the aortic arch to take the blood to the head; including the brain. They are highly specialized with CHEMORECEPTORS that detect oxygen content and PRESSURE RECEPTORS that detect changes in blood pressure. The carotid arteries run reasonably close to the surface, so the pulse can be found along both side of the neck. 5. JUGULAR VEINS: These veins correspond to the carotid arteries and take blood out of the head region and to the anterior vena cava. These veins DO NOT contain any valves! Therefore, the blood flow through them is under the influence of gravity (try standing on your head for a while). 6. SUBCLAVIAN ARTERIES/VEINS: These arteries branch off of the aorta and travel under the clavicle (collar bone). They branch to feed the arms (via the BRACHIAL ARTERIES) and the chest wall region. It is interesting to note that the lymphatic ducts join the circulatory system right before the subclavian veins meet up with the anterior vena cava. 7. MESENTERIC ARTERIES: These arteries branch off from the dorsal aorta. They go to the intestines, where they branch into the capillaries that can be seen in the villi. They pick up the newly digested nutrients and carry them to the liver. 8. HEPATIC PORTAL VEIN: Mesentery Hepatic = Liver; Portal = capillary bed on either end. This vein transports blood rich in nutrients directly from the intestines to the liver. You have already studied all of the functions of the liver. Significant functions for the circulatory system are: regulation of blood glucose concentration, destruction of aged RBC’s, and detoxification of blood. 9. HEPATIC VEIN: Carries the blood from the hepatic portal vein to the inferior vena cava. RENAL ARTERIES/VEINS: The renal arteries branch off the dorsal aorta and bring blood to the kidneys. The renal veins take blood from the kidneys to the posterior vena cava. We will discuss this in depth in Unit O (Urinary System). 10 ILIAC ARTERIES/VEINS: When the dorsal aorta gets to the pelvic area, it branches into two iliac arteries. One goes down each leg. The femoral artery is a major branch of the iliac artery that serves the large quadricep muscle of the leg. The iliac veins bring the blood back to the posterior vena cava. 11 PULMONARY VEINS/ARTERIES: The deoxygenated blood has been collected from the rest of the body moves into the right atrium and then ventricle, and is pumped into the pulmonary artery and taken to the lungs to be replenished. The pulmonary vein takes the newly oxygenated blood back to the heart and into the left atrium and then ventricle (where it is pumped into the aorta and to the rest of the body). C. The BLOOD Blood is more than just a red liquid that leaks onto your best white shirt when you cut yourself. What is Blood? 55% Plasma (liquid) 91% Water 7% Proteins Salts, gases (oxygen, carbon dioxide), nutrients (fats, glucose,amino acids), urea, hormones, vitamins… 45% Solid (formed elements) Red Blood Cells White Blood Cells Platelets *An interesting note about RED BLOOD CELLS: the liver and kidneys are sensitive to the amount of oxygen that is being delivered to them. They both respond by releasing chemicals if the level of oxygen delivered to them drops. The kidneys release REF (RENAL ERTHROPIOETIC FACTOR) and the liver releases specialized GLOBULINS. The combination of these 2 substances stimulates the red bone marrow to increase the rate of production of erythrocytes (RBC’s). It takes several weeks to build up the rate of erythrocyte production and this is why it takes a while to become ACCLIMATIZED when you visit or move to a higher elevation. SOLID PORTION OF THE BLOOD (see page 236): FORMED ELEMENTS Red Blood Cells (Eyrthrocytes) Function & Description Transports oxygen and helps to transport CO2 4-6 million/mm3 blood White Blood Cells (Leukocytes) Bioconcave disks without nuclei that are bright red to dark purple in colour Pass through several developmental stages during which they lose a nucleus and gain a hemoglobin & carbonic anhydrase molecule and an antigen (the basis for blood type). Live for ~120 days (4 months) Fights Infection a. Granular leukocytes 1) Basophils (0.5 – 1%) Spherical cells with lobed nuclei. Release HISTAMINE when damaged. Leads to swelling as it increases the permeability of capillary walls; allowing water to leak into tissues. 2) Eosinophils (1 – 4%) Spherical cells with bilobed nuclei. Are PHAGOCYTIC & engulf and destroy foreign things in blood. 3) Neutrophils (55-75%) Spherical cells with multilobed nuclei. Are also PHAGOCYTIC and make up ~ ¾ of all blood cells! b. Agranular leukocytes Are further specialized into TCELLS and B-CELLS. T-cells mature in thymus and are the TRIGGERS of the immune Source Red bone marrow (p. 238 – the formation of RBC, WBC, & platelets) Red bone marrow 1) Lymphocytes (20-30%) 2) Monocytes ( 2 – 8 %) Platelets (Thrombocytes) 150,000 to 300,000 / mm3 blood system. One type of T-cell signals the production and release of ANTIBODIES from B-cells. Lymphocytes are the 2nd most abundant type of WBC. PHAGOCYTIC Enlarge greatly in size at the site of an infection. Aid in clotting the blood Disk-shaped cell fragments with no nuclei. We produce ~ 200,000,000,000 per day Red bone marrow There is a series of reactions that lead to the formation of a blood clot. PLASMA PORTION OF THE BLOOD (see page 236): PLASMA ELEMENTS Water (90-92% of plasma) Function Maintains blood volume; transports molecules Source Absorbed from large intestine Plasma Proteins (7-8% of plasma) Maintain blood osmotic pressure & pH, blood clotting, fight infection Osmotic balance (maintain blood volume & pressure), pH buffering Blood clotting Liver a) ALBUMIN b) FIBRINOGEN c) IMMUNOGLOBULINS Salts (>1% of plasma) Na+, K+, Cl-, NaCO3… etc Transport; fight infection with antibodies (lymphocytes) Maintains blood osmotic Pressure and pH; aid metabolism Absorbed from intestinal villi Gases a) OXYGEN Cellular Respiration Lungs b) CARBON DIOXIDE Nutrients a) FATS End product of Metabolism Tissues Protection, Insulation, Energy b) GLUCOSE Energy for Cellular Respiration Absorbed from intestinal villi c) AMINO ACIDS Used to make functional and structural proteins we need d) NUCLEOTIDES Used to make nucleic acids (DNA, RNA) Nitrogenous Waste Wastes: urea, ammonia Hormones, Vitamins, etc… (Thyroxin, adrenalin, Vit. K) Aid the process of metabolism Liver Varied THE FORMATION OF A BLOOD CLOT (positive feedback): 1. The first step is that the PLATELETS must become DAMAGED in some way. This could be as simple as impact, or platelets rubbing against the rough edge of a blood vessel that has been damaged. 2. Platelets respond by releasing a protein called THROMBOPLASTIN. 3. The thromboplastin initiated the CONVERSION of PROTHROMBIN (a blood protein produced by the liver) into THROMBIN. This reaction requires the presence of CALCIUM. 4. Thrombin then catalyzes a second reaction which results in the CONVERSION of FIBRINOGEN into FIBRIN. Fibrin (unlike all of the other proteins just mentioned) is INSOLUBLE and therefore forms a BLOOD CLOT in the area that has been damaged. PLATELETS are DAMAGED Thromboplastin Ca++ Prothrombin >>>Thrombin Fibrinogen >>>>FIBRIN BLOOD CLOT Capillary Fluid Exchange Arteriole: Blood Pressure > Osmotic Pressure The blood reaches a capillary bed through an arteriole. At this point blood pressure has decreased to about 35 mmHg. This pressure is significant enough to force the water out of the blood plasma, through the capillary walls, and into the tissue spaces. This water carries with it the HbO2 (oxygen) and nutrients (products of digestion). Because the [oxygen] in the tissues if greater than the [oxygen] in the cells, the oxygen will diffuse into the body cells. Nutrients will move into the tissue spaces and into the cells at the same time. The larger things stay in the blood as they are too big to get out (ie: fibrinogen, albumin, prothrombin, platelets, RBC, WB Now, the blood is really concentrated (has very little water) and on the venule side of the capillary, the water from the tissue fluids is drawn back into the capillaries due to osmotic pressure. When the fluid returns, it brings with it CO2 (a product of cellular respiration that is more concentrated in the tissue spaces than in the plasma) and other metabolic wastes like ammonia. Venule: Osmotic Pressure > Blood Pressure The blood pressure on the venule side of the capillary bed is now only ~15 mmHg. The end result of the change is that there is no change in the blood volume. (*unless there is histamine involved – we will discuss this later). Comparison of Velocity, Blood Pressure & Cross-sectional Area of Vessels BLOOD TRACINGS Start in the Left Ventricle and go through the digestive system and back to the left ventricle Fetal Circulation: A fetus does not use its pulmonary circuit. Therefore, the main difference between fetal circulation and adult circulation is the fact that the fetus receives its O2 blood from the placenta, and does not use its lungs. To do this, there are four features in the fetus not present in the adult. Oval opening or foramen ovale This is an opening between the Left and Right atria which is covered by a flap that acts as a valve. It allows the blood to bypass the lungs and reroutes most of the blood that enters the right atrium directly into the left atrium. Arterial duct or ductus arteriosus This is a small arterial connection, like a shunt, between the pulmonary artery and the aorta. It further allows blood to bypass the lungs. Umbilical Cord The Umbilical Cord has three blood vessels traveling through it. The largest one is the umbilical vein, which transports blood with oxygen and nutrients into the fetus. The other two are the umbilical arteries, which branch off of the iliac arteries in the fetus, and take “spent” (wastes and CO2) blood back into the mother via the placenta. Venous duct or ductos venosus This blood vessel is the extension of the umbilical vein to the vena cava. The umbilical vein carries oxygenated blood, which mixes with unoxygenated blood in the vena cava. Blood is delivered to the fetal liver for treatment through the hepatic portal vein, but this comes after the blood goes through the heart and is distributed to the body. This is why the fetus is so susceptible to toxins in blood, as the liver functions are initially bypassed. CHANGES AT BIRTH The First Breath: the lungs are filled with air instead of fluid and 1. this allows for vascular resistance to decrease. Higher oxygen levels in the blood and alveoli results in an increase in pulmonary blood flow. 2. Anatomical Changes: The placenta is removed from circulation. The foramen ovale, ductus venosus, and ductus arteriosus close. Why? Higher pressure in the left atrium due to increased pulmonary blood flow causes the foramen ovale to close. Higher concentrations of oxygen in the blood, decreased prostaglandin levels and decreased pulmonary vascular resistance closes the ductus arteriosus. When the umbilical cord is clamped, the umbilical vein closes, systemic vascular resistance is increased, and this causes the ductus venosus to close. E. ANTIGENS, ANTIBODIES, & BLOOD TYPING These are two different types of proteins that have very different, but related functions. An ANTIGEN: a protein identification on the surface of a RBC. Made up of a protein and glycoprotein on a RBC’s outer membrane. There are two kinds of antigens that can be on human RBC's, A & B. . .Therefore, there are 4 possibilities of blood types: Antigens for each blood type 1. Antigen A: 2. Antigen B: Type A Blood Type B Blood 3. Antigens A&B: Type AB Blood 4. No Antigens: Type O Blood An ANTIBODY: (made by the B cells in the body) a protein designed to combat a foreign protein. When they come in contact with foreign antigens on cells that are not supposed to be in the blood, they will bind to them. This causes the agglutination of the foreign cells. Other WBC will then destroy the agglutinated cells. Within the plasma (blood fluid), are the antibodies of the antigens that are not present in the blood. Antibodies for each blood type Type A has B antibodies Type B has A antibodies Type O has A and B antibodies Type AB has no antibodies Antigen + Antibody (foreign) (body) Inactive complex (agglutination) This explains why blood transfusions have to be carefully worked out before they are administered. Obviously, the introduction of foreign RBC with antigens different from the recipients RBC will cause agglutination. On a large scale, this leads to death. DONOR R E C I P I E N T BLOOD TYPE A B AB O A B YES X X YES X YES X YES AB YES YES YES YES O X X X YES X=AGGLUTINATION *all agglutinated RBC will be destroyed by phagocytosis F. ERYTHROBLASTOSIS & THE Rh SYSTEM The Rh factor is another antigen that may be present on the RBC. The presence of this antigen plays a role in childbirth. If you are Rh+ you have the antigen and don’t have the ‘D’ antibodies. (85% of Caucasions are Rh+) If you are Rh – you don’t have the antigen. You don’t normally have the ‘D’ antibodies, but can make them if you are exposed to Rh antigens. If Rh antigens are mixed with Rh antibodies, clumping occurs. This becomes important in pregnacies because a Rhmother can have and Rh+ baby. Normally, the mother / fetal blood does not mix or cross the placenta. At birth, there is usually some mixing, so the mother begins to produce Rh antibodies in response to the Rh antigens on the baby's RBC's introduced during birth. There is no danger for either the mother or the first baby. If the mother becomes pregnant with another Rh + baby, Rh (‘D’) antibodies now in the mother's plasma are small, and may cross the placenta and agglutinate the baby's blood. This causes the baby to die / be still born (Erythroblastosis). How can this be prevented? Doctors can destroy the 1st baby's Rh + blood cells in the mother's plasma just after the 1st baby's birth before the mother has time to make the Rh antibodies in her plasma. An injection of Rh immune globulin injection (RhoGAM) does this. D. The LYMPHATIC SYSTEM (Chapter 14) The lymphatic system is a system of thin-walled vessels with valves (like veins) that start in the tissue spaces throughout the body. FUNCTIONS? 1. Take up excessive tissue fluids 2. Transport fatty acids and glycerol (from intestines) 3. Fight infection (lymphocytes) 4. Trap and remove cellular debris form tissue fluid Lymphatic Structures: 1. Lymph Vessels: The lymph capillaries drain excess fluids and plasma proteins, and transport this fluid through a CLEANSING PROCESS controlled by the Lymph Nodes. The smooth muscle around the vessels and the skeletal muscle surrounding the vessels both contract to move the lymph towards the nodes and elsewhere. The cleansed ‘lymph’ travels through lymph ducts back to the circulatory system where they meet up with the subclavian veins just as they are dumping their contents into the anterior vena cava. 2. Lacteals: blind ends found in the villi of the small intestines which absorb and transport fats. 3. Lymph Nodes: small ovoid/round structures packed with phagocytic macrophages. These macrophages produce lymphocytes which produce T and B cells. These cells produce antibodies that combine with and deactivate foreign proteins found on bacteria, cancerous cells, and incompatible blood types, etc…. 4. Other lymphoid organs: Tonsils, Appendix, Spleen, and Thymus Gland. All fight infection and make WBC’s. How do antibodies do their job?