File
advertisement

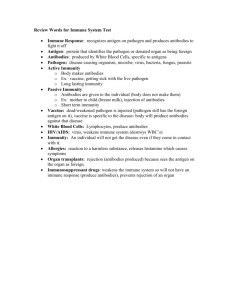
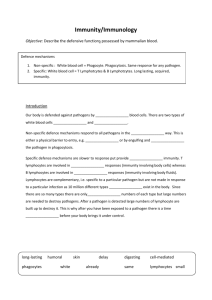
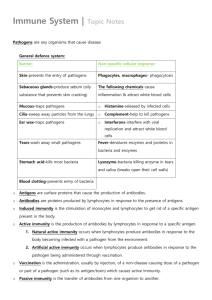
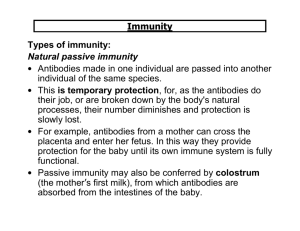
Notes Unit 14 The Immune System Overview of the Immune System A person’s immune system consists of two main types of resistance: non-specific and specific. Nonspecific resistance is the body’s defense against ANY pathogen, regardless of species; specific resistance is the body’s defense against a SPECIFIC pathogen. See chart below for a brief overview: Part I: Nonspecific Defenses of the Host There are 5 main nonspecific methods of defense against pathogens: 1. Skin and Mucous Membranes – the first line of defense. These are all of the mechanical and chemical factors that our body has already in place. Includes the following: Mechanical Factors – skin, mucous membranes, tears, mucus, cilia in the throat, epiglottis, urine, vaginal secretions. All of these factors form a mechanical (physical) barrier against microbes who try to enter the body. Chemical Factors – sebum (skin oil), perspiration (which contains lysozyme, an enzyme), gastric juice, acid in vaginal secretions, transferrins in blood. All of these factors are chemicals produced by our bodies that have microbe-killing ability. Normal Microbiota – because our skin and various body surfaces have normal microbiota (flora), these bacteria act as a barrier to other microbes trying to enter by competing for nutrients and producing substances that are toxic to other bacteria. We have normal flora in the following areas of our bodies: skin, mouth, lower GI tract (intestines), vagina, nose, and throat. 2. Phagocytosis – phagocytosis is defined as the ingestion of a microorganism or any particulate matter by a cell. This is part of the second line of defense against pathogens. The cells that perform this function are collectively called phagocytes, all of which are types of white blood cells. Before we go any further, lets stop and consider the different components of blood. Blood consists of two main things: plasma, which is the liquid part of blood; and cells, including red blood cells, white blood cells, and platelets. Another name for white blood cells is leukocytes. During many kinds of infections, the total number of white blood cells increases in the blood because phagocytes are needed to help kill the invading pathogen. Look at the chart below for the different types of cells and their approximate percentage in the blood: 1 Notice that in the above chart, neutrophils, eosinophils, and monocytes are the phagocytic cells of our blood. When infection occurs, the phagocytic cells invade the infected area, to form a familiar substance called pus (white blood cells) at the infection site. Phagocytosis occurs in 4 stages: 1. Chemotaxis – this is the chemical attraction of the phagocyte to the microorganism. 2. Adherence – the attachment of the phagocyte’s plasma membrane to the surface of the microorganism. 3. Ingestion – plasma membrane of the phagocyte extends projections called pseudopods that engulf the microorganism 4. Digestion – digestive enzymes in phagocyte digest bacteria. 2 Here’s how phagocytosis works: 3. Inflammation – damage to the body’s tissues triggers a defensive response called inflammation. It is characterized by four signs and symptoms: redness, pain, heat and swelling. The purpose of inflammation is to destroy the pathogen, and if destruction is not possible, to limit the effects on the body by confining or walling off the pathogen and its by-products, and to repair or replace tissue damaged by the pathogen or its by-products. There are three stages to the process of inflammation: Vasodilation - immediately following tissue damage, blood vessels dilate (widen) and become very permeable. The purpose of this is to increase blood flow to the damaged area, which is what causes the redness at a wound site. This allows cells such as neutrophils and macrophages to escape from the blood vessels and move to the site of the pathogen. Also, allows chemicals, such as histamine, to be released at the site. Phagocyte Migration and Phagocytosis – generally within 1 hour after injury, phagocytes appear on the scene. They begin to engulf the pathogen, then they die, forming pus. Tissue Repair – the final stage of inflammation is when the body replaces dead or damaged cells. 4. Fever – this is the body’s systemic (overall) response to injury and is characterized by abnormally high body temperature. High body temperature speeds up the body’s reactions, thus causing body tissues to repair themselves more quickly. Also intensifies the effect of certain anti-viral proteins. 5. Antimicrobial Substances – the body produces certain antimicrobial substances in addition to everything else. Two of the main ones are: Complement – this is a system of serum proteins that participate in the lysis (breakdown) of foreign cells, in inflammation and in phagocytosis. This system is very complicated, and consists of many proteins, but they aid the microbial destruction in three ways: 3 o Cytolysis – they damage the plasma membrane of a microbe, thus causing cell contents to leak out and the cell will die. o Inflammation – these proteins aid in the inflammatory process o Opsonization – these proteins help promote phagocytosis Interferons – these are antiviral proteins produced after viral stimulation, and they interfere with viral reproduction. Part II: Specific Defenses of the Host – The Immune Response Immunity is a specific defensive response to an invasion by foreign organisms or other substances. This is the third line of defense against a pathogen – that is, if a pathogen manages to get past all of the nonspecific defenses, then this one will take over. These mechanisms are VERY SPECIFIC for each particular pathogen, and will remember a specific pathogen if it ever returns to the body again. This type of immunity is also called acquired immunity, because your body only makes these proteins AFTER it encounters a pathogen. Let’s look at an overview chart before we begin: Types of Acquired Immunity Acquired immunity refers to the protection we develop against certain types of microbes. It is developed throughout our lifetimes. It can be acquired either actively or passively; either naturally or artificially. 4 1. Naturally-acquired active immunity – produced when a person is exposed to pathogens naturally. Once acquired, it is lifelong for some diseases, but may only last a couple of years for others. Example: you are exposed to the flu virus, and your body produces antibodies to the virus. 2. Naturally-acquired passive immunity – when a mother transfers antibodies to her fetus across the placenta. They are produced naturally, but are passively given to the fetus. 3. Artificially-acquired active immunity – antibodies are produced by your body as a result of vaccination. Your body is actively producing antibodies, but you were not exposed to a real pathogen – it was artificially introduced into your body. 4. Artificially-acquired passive immunity – when antibodies are produced in another organism, and then introduced artificially into your body. Example: suppose you are exposed to Hepatitis virus, then you can be given a dose of antibodies that are pre-produced from another organism that are ready to “kick in” right away and kill viruses! Antibodies and Antigens Antibodies are proteins that are made in response to a pathogen and can recognize and bind to that pathogen. They are what is produced when immunity is acquired, as above. They are highly specific in recognizing the pathogen that stimulated their original formation. For instance, if you produce antibodies in response to a flu virus, you will not get THAT exact virus again. However, if another strain of the flu virus comes along next month, it will not recognize that one because it is slightly different. In pictures, antibodies are represented by the letter “Y” because that is kind of what they look like: Antigens are any foreign substance that enters our body and causes it to produce antibodies. They are specific, and each antigen will cause the formation of a different type of antibody. In microbes, antigens are the proteins or polysaccharide formations found on the outer cell wall. Notice above that antigens can look different, and each antigen must fit the antibody that matches its “shape” – it’s like a lock and key mechanism. 5 The Duality of the Specific Immune System Our specific immune system (Part II) consists of two major mechanisms: humoral immunity and cell-mediated immunity. 1. Humoral (Antibody-mediated) Immunity – involves what we described above: the production of antibodies that act against foreign organisms. Cells in our bodies called B cells are responsible for the production of antibodies, and these B cells arise from stem cells (cells that have not specialized yet) in our bone marrow. The humoral response defends primarily against bacteria, bacterial toxins, and viruses that are free-floating in our bodies. 2. Cell-Mediated Immunity – involves specialized lymphocytes (white blood cells) called T cells that act against foreign organisms or tissues. T cells originate in the thymus gland. Most effective against intracellular pathogens (ones located in our cells). Although cell-mediated and humoral immunity are considered separate branches of the specific immune system, they are closely interrelated. They work together to accomplish the task. 6