Chapter 14 - Moorpark College
advertisement
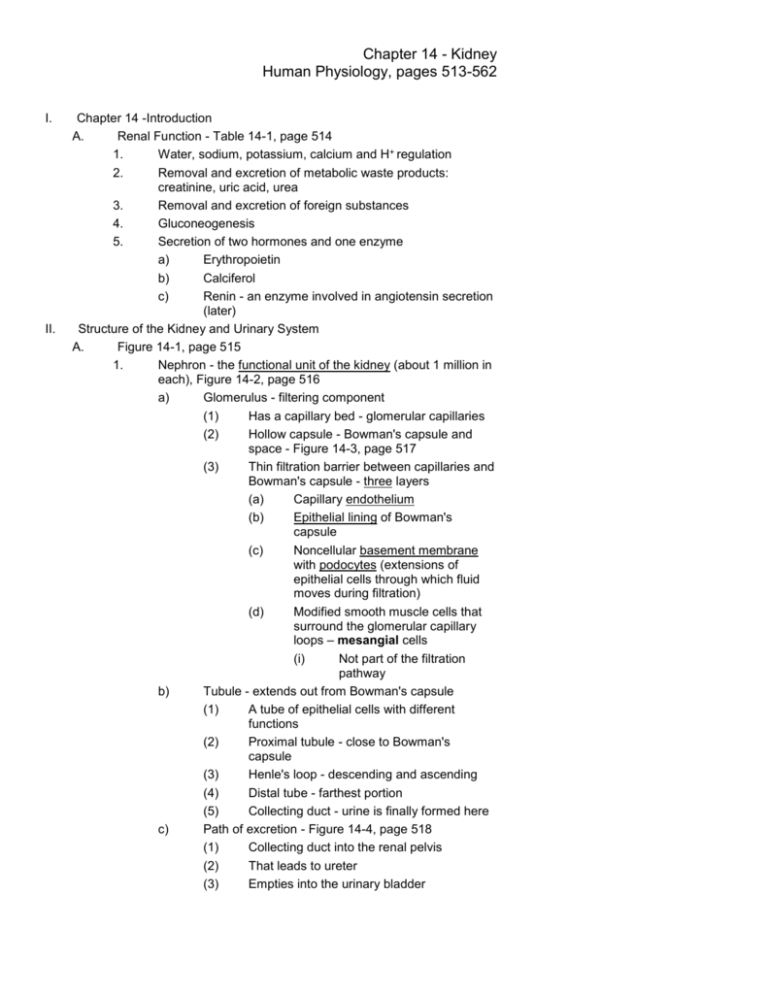
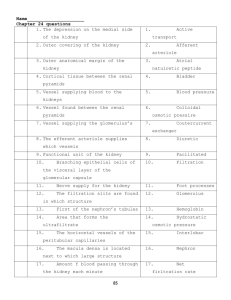
Chapter 14 - Kidney Human Physiology, pages 513-562 I. II. Chapter 14 -Introduction A. Renal Function - Table 14-1, page 514 1. Water, sodium, potassium, calcium and H+ regulation 2. Removal and excretion of metabolic waste products: creatinine, uric acid, urea 3. Removal and excretion of foreign substances 4. Gluconeogenesis 5. Secretion of two hormones and one enzyme a) Erythropoietin b) Calciferol c) Renin - an enzyme involved in angiotensin secretion (later) Structure of the Kidney and Urinary System A. Figure 14-1, page 515 1. Nephron - the functional unit of the kidney (about 1 million in each), Figure 14-2, page 516 a) Glomerulus - filtering component (1) Has a capillary bed - glomerular capillaries (2) Hollow capsule - Bowman's capsule and space - Figure 14-3, page 517 (3) Thin filtration barrier between capillaries and Bowman's capsule - three layers (a) Capillary endothelium (b) Epithelial lining of Bowman's capsule (c) Noncellular basement membrane with podocytes (extensions of epithelial cells through which fluid moves during filtration) (d) Modified smooth muscle cells that surround the glomerular capillary loops – mesangial cells (i) Not part of the filtration pathway b) Tubule - extends out from Bowman's capsule (1) A tube of epithelial cells with different functions (2) Proximal tubule - close to Bowman's capsule (3) Henle's loop - descending and ascending (4) Distal tube - farthest portion (5) Collecting duct - urine is finally formed here c) Path of excretion - Figure 14-4, page 518 (1) Collecting duct into the renal pelvis (2) That leads to ureter (3) Empties into the urinary bladder Chapter 14 - Kidney Human Physiology, pages 513-562 d) (4) Urine eliminated through the urethra Macula densa and granular cells (juxtaglomerular cells) of afferent arteriole meet and form juxtaglomerular apparatus (JGA) - an area of enzyme secretion and monitoring of plasma - Figure 14-5, page 518 B. III. Circulation 1. Afferent arteriole brings blood to glomerulus for filtration 2. Unfiltered blood then leaves glomerulus via the efferent arteriole where it breaks down into the peritubular capillaries 3. The peritubular capillaries surround the tubules allowing exchange - VERY IMPORTANT 4. Blood leaves via the renal vein 5. This is the Renal Portal System! Basic Renal Processes A. Three basic processes - glomerular filtration, tubular reabsorption and tubular secretion - Figure 14-6, page 519, Figure 14-7, page 519 Excretion - elimination of urine via kidneys Defecation - elimination of feces via G.I. tract Secretion - from cells to surfaces, lumens or into blood stream B. Questions about any given substance 1. Extent of filterability? 2. Is it reabsorbed? 3. Is it secreted? 4. What role does metabolism by the tubular cells play regarding the substance and its homeostasis? C. Glomerular filtration 1. Formation of ultrafiltrate a) Figure 14-8, page 520 Favoring filtration: Blood Pressure 60 mmHg Bowman's back pressure Osmotic gradient due to absence of protein in ultrafiltrate Net filtration pressure = -15 mmHg Opposing filtration: -29 mmHg 16 mmHg Chapter 14 - Kidney Human Physiology, pages 513-562 b) 2. 3. Ultrafiltrate is essentially protein free plasma containing all the constituents of plasma in the blood but lacking the protein (or most of it) - important to understand! c) In a healthy person any protein that gets filtered is reabsorbed by tubule cells Rate of glomerular filtration (mention inulin) a) A 70 kg person filters (from plasma into Bowman's capsule) 180 liters/day or 45 gallons weighing about 450 lbs b) The entire plasma volume is filtered 60 times a day, i.e. a continuing process c) Glomerular filtration rate [GFR] - the volume filtered per unit time d) GFR X plasma concentration of a substance will determine total amount filtered, filtered load glucose @ 1 g/l X 180 l/day= 180 g/day e) Comparing this figure with the amount appearing in the urine can indicate whether absorption or secretion is occurring normally Balance between renal efferent and afferent arterioles and PGC a) Back pressure effect, etc., Figure 14-9, page 522 Mesangial cells surround glomerular capillaries and when they constrict the total surface area for exchange is reduced and decreases GFR 4. Total renal plasma flow a) About 900 liters/day b) The GFR of 180 l/day is 20% of volume 5. Total renal blood flow a) Plasma is 55% of whole blood b) Total renal blood flow = 1640 l/day (1.1 l/min) 6. Kidneys receive 20 to 25% of total cardiac output of 5 l/min even though their weight is less than 1% of the body weight Tubular reabsorption, Table 14-2, page 522 1. Compare values (Per Day) b) D. Substance Water, l Sodium, g Glucose, g Urea, g amt filt 180 630 180 54 a) b) amt/exc % reabsorbed 1.8 99.0 3.2 99.5 0 100 30 44 Certain substances, under normal conditions, are reabsorbed completely, others partially Not all substances are regulated as such, i.e. glucose - even though it is reabsorbed it is dependent on the number of carriers Chapter 14 - Kidney Human Physiology, pages 513-562 c) E. F. G. H. Several substances can exceed the capacity of the tubule to reabsorb them - more below d) Tubular epithelium, Figure 14-10, page 523 2. Types of reabsorption a) Most tubular reabsorption is by mediated transport mechanisms and/or diffusion b) The transport of some is coupled to an active transport mechanism and is secondary active transport (1) Movement of glucose is usually by facilitated transported except in kidney tubules where it is active (2) Maximal tubular capacity - Tm, when the number of carriers are exceeded glucose can "spill" over into the urine; this holds for some other organic substances also c) Some substances are transformed by the kidney into polar compounds and these are poorly reabsorbed by the tubules so they go out in the urine Reabsorption by diffusion 1. As tubular-fluid moves through it becomes more concentrated and materials will diffuse out 2. Urea is an example Tubular secretion a) This is from peritubular capillaries TO tubular lumen b) Two most important substances that are secreted are potassium and hydrogen ion c) Some foreign substances are excreted by tubular secretion such as penicillin Metabolism by the tubules 1. The cells of the tubules are capable of metabolizing or synthesizing certain substances that can then be secreted into the tubule 2. The cells can synthesize ammonia and eliminate it in the urine Regulation of membrane channels and transporters 1. Tubular reabsorption and/or secretion is under control of regulation of transporter and channel proteins 2. Regulation is by hormones, neurotransmitters and paracrine/autocrine agents Channels also respond to local changes membrane potential, mechanical forces and intracellular ion concentrations I. Division of labor in the tubules 1. Each part of nephron plays a different role in renal function 2. From Bowman's capsule to the collecting tubules different regulating forces are responsible for the overall homeostasis IV. Concept of Renal Clearance 3. Chapter 14 - Kidney Human Physiology, pages 513-562 A. B. The volume of plasma from which that substance is completely cleared by the kidneys per unit time Clearance of substance S Us (mg/l) x V(l/hr) Cs (l/hr)= -------------------Ps (mg/l) V = urine volume/minute Us = urine concentration of substance S Ps = plasma concentration of substance C. Inulin is freely filterable but is neither reabsorbed nor secreted, Figure 14-11, page 525 300 (mg/l) x 0.1 (l/hr) CIn (l/hr)= -------------------4 (mg/l) D. V. = 7.5 l/hr The 7.5 l/hr clearance value for inulin is equal to the GFR since inulin is not reabsorbed or secreted E. 4.0 mg/l * 7.5 l/hr = 30 mg/h (total inulin secreted) Micturition (urination) - Figure 14-12, page 526 A. Smooth muscle contractions of the ureter-wall propel the urine to the bladder for storage and eventual elimination or micturition B. Walls of smooth muscle are collectively termed the detrusor muscle. 1. Contraction of the detrusor muscle squeezes on the urine in the lumen to produce urination. 2. The detrusor muscle at the base of the bladder is called the internal urethral sphincter. When the detrusor muscle is relaxed, the sphincter is closed. 3. When the detrusor muscle actively contracts, changes in the muscle's shape pull open the outlet. Beyond the internal urethral sphincter, skeletal muscle surrounds the urethra. 4. This is the external urethral sphincter, the contraction of which can prevent urination even when the detrusor muscle contracts strongly. C. Descending CNS pathways can influence the local spinal reflex action of micturition 1. Involuntary: infancy or in persons with spinal-cord damage a) Afferent stretch receptor fibers in the bladder wall stimulate the parasympathetic nerves that stimulate the detrusor muscle b) The filling of the bladder stimulates detrusor muscle to contract via the parasympathetic effector neurons c) The detrusor muscle (in response to filling) becomes strong enough to pull open the internal urethral sphincter. Simultaneously, the afferent input from the stretch receptors inhibits, within the spinal cord, the somatic motor neurons that were stimulating the external urethral sphincter to contract. Chapter 14 - Kidney Human Physiology, pages 513-562 d) 2. 3. Both sphincters open and the contraction of the detrusor muscle is able to produce urination. Voluntary prevention of micturition, learned response a) As the bladder fills, the input from the bladder stretch receptors causes, via ascending pathways to the brain, a sensation of bladder fullness and the urge to urinate. b) In response to this, urination can be voluntarily prevented via descending pathways that stimulate the motor nerves to the external urethral sphincter and simultaneously inhibit the parasympathetic nerves to the detrusor muscle. c) The prevention of urination can be overcome once the bladder exceeds its capacity. In contrast, urination can be voluntarily initiated, regardless of the degree of bladder fullness, via the descending pathways. SECTION B - REGULATION OF SODIUM, CHLORIDE AND WATER BALANCE VI. Total body balance of sodium and water A. Table 14-3, page 529 - water balance Intake: Drunk Food Metabolically 1200 ml 1000 ml 350 ml TOTAL 2550 ml Output Insensible loss Sweat Feces Urine Total output B. 900 ml 50 ml 100 ml 1500 ml 2550 ml Table 14-4, page 529 (sodium chloride per day) Intake: Food Output Sweat Feces Urine Total output 10.5 g 0.25 g 0.25 g 10.0 g 10.5 g + The kidney can regulate wide differences - this deals with Na , Cl and water balance (kidney can produce from 400 ml to 25 liters a day of urine!) VII. Basic Renal Processes for Sodium and Water A. Ninety-nine (99%) of sodium, chloride and water are reabsorbed 1. Sodium is reabsorbed by primary active transport - Na, KATPase pump, Figure 14-13, page 530 2. Chloride follows sodium passively and in some cases actively C. Chapter 14 - Kidney Human Physiology, pages 513-562 3. B. C. D. E. VIII. A. Water is reabsorbed by diffusion (osmosis) and is dependent on the transport of Na+ and Cla) When Na+ is actively transported across the membrane that creates an osmotic gradient which water can move down if the membrane is permeable to water b) The tubular cells can have their permeability to water altered, either increased or decreased Coupling water reabsorption to sodium reabsorption 1. Changes osmolarity 2. Aquaporins regulated water channels 3. Figure 14-14, page 530 Antidiuretic hormone - (ADH), also known as vasopressin 1. Diuretic - anything that increases the output of water, an antidiuretic prevents water loss 2. ADH prevent water loss by increasing the tubular permeability (last nephron section) to water 3. ADH has little effect on Na+ reabsorption Crucial aspects 1. Response to ADH is not all-or-none but can be graded (fine control over water balance) 2. There is an obligatory water loss associated with sodium excretion (or any substance) and this can be large if a large amount of Na+ must be excreted and greatly effect extracellular volume 3. Large volumes of water can be excreted with virtually no Na+ present - important in control of extracellular osmolarity Urine concentration: The countercurrent multiplier system 1. Review of osmosis may be required to understand the following material - Chapter 6 2. Problem: How does the kidney produce a hyperosmotic urine? from 300 mOsmol to 1,400 mOsmol a) Daily output of waste is about 600 mOsmol b) 600 mOsmol/day / 1,400 mOsmol/l = 0.444 l/day c) 444 ml is the obligatory water loss per day 3. Figure 14-15, page 532 4. The key is the increasing hypertonicity of the interstitial fluid that "draws" out of the collecting ducts and concentrates the urine 5. Figure 14-16, page 533 Renal Sodium Regulation Sodium balance equation, page 534 Na+ excreted = Na+ filtered - Na+ reabsorbed 1. Major reflex pathways that alter Na+ balance are a) Cardiovascular baroreceptors effects on hormone secretions, next section Chapter 14 - Kidney Human Physiology, pages 513-562 B. C. b) Efferent and hormonal pathways to the kidneys c) Renal effector sites - arterioles and tubules 2. Three cases of balance challenge a) Drink two liters of distilled water b) Drink two liters of Gatorade (balanced salt solution, i.e. isotonic) c) Take six salt tablets, little water Control of GFR 1. Constriction of renal arterioles decreases GFR 2. Dilation of renal arterioles increases GFR 3. Figure 14-17, page 535 - summary of response to severe water and salt loss due to diarrhea Control of sodium reabsorption 1. While altering the GFR can quickly change the amount of Na+ excreted for long term control the hormonal control of reabsorption is more important 2. Aldosterone and the renin-angiotensin system a) Aldosterone - secreted by adrenal cortex, stimulates Na+ reabsorption b) In absence of aldosterone a person can lose 35 g of salt a day tell story about boy who ate salt c) Renin - specialized cells in the afferent arterioles synthesize and secrete this enzyme into the blood (don't confuse with rennin), Figure 14-18, page 536 (1) Renin secretion can be elicited by sympathetic input and pressure changes in the renal arterioles - JGA intrarenal baroreceptors (2) A complex regulatory mechanism d) Angiotensinogen - from liver, is converted into angiotensin I by the enzyme renin which is then further converted to angiotensin II by a "converting enzyme" in lung capillaries e) Angiotensin II stimulates cells of the adrenal cortex to secrete aldosterone f) Figure 14-19, page 530 - Effect of plasma volume on Na+ excretion 3. Factors other than aldosterone a) Renal nerves and angiotensin II also act directly on the tubules to stimulate sodium ion reabsorption b) Atrial natriuretic peptide (ANP), Figure 14-20, page 538 (1) From atria of heart and inhibits the reabsorption of Na+ (2) Increases GFR by acting on renal blood vessels Chapter 14 - Kidney Human Physiology, pages 513-562 (3) (4) c) Also inhibits secretion of renin and aldosterone Stimulated by excess sodium and increased blood pressure or atrial distension Pressure natriuresis increase in arterial pressure inhibits sodium reabsorption and increases sodium excretion D. Conclusion 1. Na+ balance doesn't vary more than 2% 2. A balance between osmolarity and volume IX. Renal Water Regulation A. Person drinking 2 liters of water - no change in total body salt (it gets diluted) 1. Must excrete water and keep salt 2. ADH is inhibited and Na+ is reabsorbed normally - a large volume of dilute (hypoosmotic) urine is excreted B. Baroreceptor control of vasopressin secretion, Figure 14-21, page 539 Decreased extracellular volume the renin-angiotensin system causes an increased aldosterone secretion. a) Decreased extracellular volume also triggers increased vasopressin secretion. b) Increased vasopressin secretion increases the water permeability of the collecting ducts, more water is reabsorbed and less is excreted, and water is retained. 2. This reflex is initiated by several baroreceptors in the cardiovascular system. a) The baroreceptors; decrease their rate of firing when cardiovascular pressures decrease b) When blood volume decreases few impulses are transmitted from the baroreceptors via afferent neurons and ascending pathways to the hypothalamus, and the result is increased vasopressin secretion. c) Conversely, increased cardiovascular pressures cause more firing by the baroreceptors, resulting in a decrease in vasopressin secretion. 3. If the plasma vasopressin concentration becomes very high it, like angiotensin II, causes widespread arteriolar constriction. 4. The baroreceptor reflex for vasopressin has a relatively high threshold - there must be a sizable reduction in cardiovascular pressures to trigger it. Therefore, this reflex, compared to the osmoreceptor reflex described next, generally plays a lesser role under most physiological circumstances ADH Secretion and Extracellular Volume 1. C. Chapter 14 - Kidney Human Physiology, pages 513-562 1. Figure 14-22 page 540 - ADH secretion is decreased when plasma volume is increased 2. Osmoreceptors control of ADH secretion 3. What controls ADH secretion in pure water gains or deficits? osmoreceptors 4. Osmoreceptors are located in hypothalamus - an decrease in osmolarity inhibits ADH X. A Summary Example: The Response to Sweating A. Figure 14-23, page 541 B. Understand XI. Thirst and Salt Appetite A. Thirst is stimulated by both low volume and high plasma osmolarity intake will compensate 1. Angiotensin can effect thirst directly, (on brain) 2. Extracellular volume is down and angiotensin causes thirst which can eventually increase volume if intake is increased 3. Summary Figure 14-24, page 542 Salt appetite - questionable in humans XII. Potassium Regulation A. Closely regulated - effects nerve and muscle, too high is dangerous, too low is dangerous 1. Most K+ is found intracellular 2. Main control is renal B. Renal regulation of potassium 1. Freely filterable at glomerulus 2. Regulation is primarily by secretion, Figure 14-25, page 543 3. Aldosterone - increases tubular potassium secretion a) Simpler mechanism than for Na+ b) Adrenal cortex cells respond to the fluid bathing them, i.e. increased K+ stimulates the cells to secrete aldosterone which then causes secretion of excess of K+, Figure 14-26, page 543 4. Summary - Figure 14-27, page 544 B. SECTION C - CALCIUM REGULATION XIII. Calcium regulation A. Important for neuromuscular function 1. Hypocalcemia - increased excitability of nerve and muscle and hypocalcemic tetany 2. Hypercalcemia - cardiac arrhythmias and depressed muscular ability B. Functions of Bone, Table 14-5, page 547 1. Supports the body and “opposes” gravity 2. Rigidity for locomotion 3. Protection of internal organs 4. Reservoir of calcium Chapter 14 - Kidney Human Physiology, pages 513-562 5. C. D. E. F. G. Produces blood cells in marrow Cross section of bone Figure 14-28, page 547 Summary of major hormones regulating bone mass, Table 14-6, page 547 Effector sites for calcium homeostasis - Not regulated like Na+ and K+ but has three sites listed below 1. Bone - 99% of the body Ca2+ is in the extracellular matrix and can be drawn from and deposited to a) Hydroxyapatite b) Osteoblasts c) Osteocytes d) Osteoclasts 2. Gastrointestinal tract - little Ca2+ is absorbed by gut but it can be increased and decreased as part of regulation 3. Kidney - Ca2+ filtration and reabsorption occurs to regulate, phosphorus (PO3-) is intimately involved in Ca2+ regulation Parathyroid hormone → Figure 14-29, page 548 1. All three sites above are directly or indirectly subject to control by this hormone 2. The regulation of secretion is direct, that is, the secretory cells of the parathyroid are effected by the Ca 2+ concentration in the extracellular fluid a) Low Ca2+ stimulates PTH secretion b) Increased Ca2+ inhibits PTH secretion 3. Four distinct effects in Ca2+ homeostasis a) Increases bone demineralization (Ca2+ and PO3-) b) Stimulates vitamin D which acts alone to increase gut Ca2+ absorption c) Increases renal tubular Ca2+ reabsorption d) Reduces renal tubular PO3- reabsorption, thus increases PO3- excretion e) Summary Figure 14-30, page 549 4. Importance of phosphorus a) Due to equilibrium constant the product of [Ca2+] x [PO3-] = constant b) If PO3- increases that "forces" a deposition of Ca2+ into bone to maintain the product of [Ca2+] x [PO3-] constant c) Since PTH cause both Ca2+ and PO3- to be lost from bone then the increased PO3- would retard the process but PTH causes excretion of PO3- which allows further bone demineralization and increased plasma [Ca2+] Vitamin D - calciferol, (a hormone) 1. This is actually a steroid hormone of which there are about 25 active derivatives Chapter 14 - Kidney Human Physiology, pages 513-562 2. H. The main role of vitamin D (calciferol) is to stimulate the absorption of Ca2+ from the gut thus increasing the plasma Ca2+ level 3. Pathway of vitamin D activation a) Sunlight strikes skin & activates or from dietary source b) Next stop is liver for further transformation c) The kidney is the last step which regulates the amount of circulating hormone, 1,25-(OH)2D3 d) The level of PTH can act on the kidney, if the Ca2+ level drops PTH causes vitamin D to be increased which increases absorption and raises plasma Ca2+ concentration e) When plasma Ca2+ is "normalized" the extra Ca2+ can be deposited in bone f) Lack of vitamin D (no sunlight and from diet) leads to rickets in children and osteomalacia in adults g) Discuss osteoporosis and calcium 4. Summary - 1,25-(OH)2D3 and PTH action to increase plasma Ca2+ level, Figure 14-31, page 550 Calcitonin (a hormone) 1. In thyroid gland, separate from cells that secrete thyroxine and are directly effected by plasma Ca2+ concentration 2. Lowers plasma Ca2+ concentration by inhibiting release from bone 3. Opposes PTH but plays a minor role in regulation SECTION C - HYDROGEN-ION REGULATION XIV. Hydrogen Ion Regulation A. Table 14-7, page 553 - Sources of hydrogen gain or loss B. Acids and Buffers 1. Strong acid ionizes almost completely 2. HCl H+ + ClWeak acid does not ionize completely 3. H2CO3 HCO3- + H+ General buffer equation: pKa is equilibrium constant of acid pH = pKa + log10 C. [salt] [acid] Generation of hydrogen ions by metabolism in the body - 1. H2PO41- H+ + HPO42- 2. H2SO4 2H+ + SO42- Chapter 14 - Kidney Human Physiology, pages 513-562 CO2 + H2O H2CO3 HCO3- + H+Organic acids such as lactic, glutamic etc. 4. Proteins can ionize Buffering of hydrogen ions in the body 1. The concentration of plasma [H+] is 0.00004 mmol/l which is a pH of 7.4 a) An increase or decrease of H+ can change the pH if it were not buffered b) Buffers maintain the pH by "picking up" or "releasing" hydrogen ions 2. Bicarbonate-carbon dioxide - Figure 14-32, page 555 - pH and CO2 3. Reabsorption of carbonate, Figure 14-33, page 556 3. D. Figure 14-34, page 556 renal contribution of new bicarbonate from glutamine (mainly in proximal tubule) E. Renal regulation of extracellular hydrogen ion concentration 1. Buffers do not remove extra H+ but just "bind" them 2. Hydrogen ion excreted in the urine is almost totally by tubular secretion a) Rather complex b) Depends on the ability of tubular cells to synthesize ammonia NH3 + H+ NH4+ F. Renal response to acidosis & alkalosis, Table 14-8, page 557 G. Classification of disordered hydrogen-ion concentration, Table 14-9, page 557 1. Respiratory acidosis or alkalosis a) Failure of lungs to eliminate CO2 (acidosis) or eliminate too much (alkalosis) b) Explainable in terms of mass action 2. Metabolic acidosis or alkalosis a) Body producing excess H+- (acidosis) (1) Hypoxia or exercise producing lactic acid (2) Fasting or diabetes producing ketone bodies b) Excessive hydroxyl ions - (alkalosis) (1) Bicarbonate loss due to diarrhea (2) Loss of HCl in severe vomiting XV. Diuretics and Kidney Disease A. Read on own 4.