RENAL DISEASE PACKET
advertisement

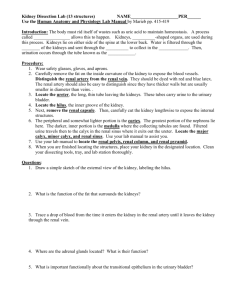
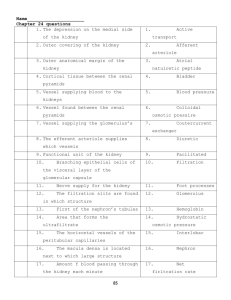
Renal_2012 Due August 17, 2012 RENAL DISEASE PACKET Name: Jaclyn Lee PLEASE ANSWER ALL QUESTIONS IN YOUR OWN WORDS. THE END OF EACH SECTION. LIST THE APPLICABLE REFERENCES AT A.) MEDICAL TERMINOLOGY 1. Fill in the blanks in the following table: BODY PART Kidney nephr, ren PRIMARY FUNTION OF BODY PART Collects urine produced by the kidney Organ that processes urine Urine -uria, urin Removes waste from blood stream Example: Renal Pelvis RELATED ROOT WORD pyel Ureters ureter Tubes that propell urine from the kidneys to the bladder Bladder cyst, vesic Retains the body’s urine until it is ready to be released Urethra ureth Tube that connects the bladder to the genitals 2. Break the following words up into their prefix, root and suffix and then provide the meaning of the word. Not all words will have all three parts. Medical Term Prefix & Meaning Root & Meaning Suffix & Meaning Ex: Nephrotic - nephro - kidney Uremia Ure-nitrogen Nephrologist Nephro - kidney Anuria Nephrosis An- No tic – pertaining to Pertaining to the Kidney emia- blood High levels of nitrogenous waste in the blood ologist- one who studies Uria-urine Nephro - kidney -1- Meaning of Medical Term A kidney/renal physician A nonpassage of urine osis- condition Kidney disease Renal_2012 Glomerulonephritis Nephrolithiasis Due August 17, 2012 Glomeruloglomerulus Nephro- kidney lithia-stone Cystorrhagia Hemodialysis Neph - kidney Hemo-blood Cystectomy Polyuria itis- inflammation Inflammation of the glomerulus of the kidney asis-condition or state of Kidney stones Cyst- bladder hagia-blood Blood in the bladder dia-throughout lysis-destruction Removal of certain elements in the blood Cyst- bladder ectomu-removal Removal of all or part of the bladder uria-urine Excessive amounts of urine Poly-many B.) NORMAL RENAL ANATOMY AND FUNCTION d. e. 1. Label the parts of the kidney. c. b. f. a. g. List your answers here a. Renal pyramid e. Convoluted tubule b. Ureter f. Collecting duct -2- Renal_2012 Due August 17, 2012 c. Renal artery g. Loop of Henle d. Renal Corpuscle -3- Renal_2012 2. Due August 17, 2012 In your own words, discuss the mechanism of action for the following functions of the kidneys: a. Blood filtration, excretion and regulation of body wastes. The kidneys filter small molecules and water in the blood. The red blood cells are too big to be filtered thats why, under normal conditions, no blood appears in the urine. The rate of filteration is approximately 125ml/min or 180 liters each day. Most adult humans have 7-8 liters of blood, meaning the blood gets completly filtered 20-25 times a day. The kidney is also responsible for removing excess fluid and waste from the blood it filters. While filtering 180 L of blood, the kidneys produce 1-2 L of urine to excrete. The urine contains urea, a byproduct of protein metabolism, excess vitamins, minreals, and metabolites from drugs. b. Regulation of blood volume, blood pressure and electrolyte balance. High blod pressure can damage the small blood vessels in the kidnets. When the vessels are damaged they cannot filter the blood as they should. c. Acid-base regulation of body fluids When fluid voluem is low the antidiuretic hormone called vasopressin is released from the anterior pituitary gland increasing absorption of water in the colecting duct. When extracellular volume decreases, the renin-angiotensin-aldosterone system is activated and it excretes less sodium chloride. These systems work together to keep a homeostatic acid-base balance of body fluids. d. Gluconeogenesis (occurs under specific condition) When the body is in a time of insufficent carbohydrate consumption, it breaks down amino acids in the liver or kidneys into glucose the body can used for immediate energy. e. Note: Hormone production is another important function but is discussed in later sections. Reference for this section: http://www.urologyhealth.org/urology/index.cfm?article=24 4 Renal_2012 Due August 17, 2012 Byham-Gray, Wiesen, eds. A Clinical Guide to Nutrition Care in Kidney Disease. ADA, 2004 http://medical-dictionary.thefreedictionary.com/gluconeogenesis C.) RENAL DISEASES AND CONDITIONS 1. Define the following as they relate to renal function or disease. a. Azotemia- Elevated blood urea nitrogen (BUN) and serum creatine circulating in the blood. b. Oliguria- A very low output of urine, somewhere between 300-500ml/day. This may be a sign of dehydration or renal failure. c. Hyperparathyroid- The excessive production of parathyroid hormone (PTH) by the parathyroid glands. c. Glomerular filtration rate (GFR), what does it measure and how is it used? The GRF measures how much blood passes through the glomerulli in the kidneys each minute. This test measures how effectivly the kidneys are filtering the blood. Reference: http://www.nlm.nih.gov/medlineplus/ency/article/007305.htm mayoclinic.com Powerpoints on Kidney Disease from Janet Rouslin RD, JWU. For each of the following kidney diseases and conditions: a. I am giving you the definition of the disease or condition b. I am giving you the causes (etiologies) c. You describe the physical changes specific to the disease process and progression (pathogenesis). d. You explain how the disease impacts the patient’s nutritional status (in some cases there will be no impact.) e. You tell me - is a modified diet recommended for this condition? If so what is the diet prescription? 2. Glomerulonephritis a. Definition: Condition resulting from inflammation of the capillaries of the glomeruli. 5 Renal_2012 Due August 17, 2012 b. Etiology: Acute GN is most commonly triggered by an infectious process, often streptococcal, but may also result from drug/toxin exposure, immunological abnormalities, vascular or other systemic disease. Starts as an acute syndrome but if underlying cause isn’t treated, may persist in the form of rapidly progressing glomerulonephritis (RPGN). Chronic GN is often an autoimmune disease. c. Pathogenesis: Physical changes include blood in the urine, vomit, or stools, fever, loss of apetite, edema and abdominal pain. d. Nutritional Status: Nutritional status is based on fluids status and electrolyte balance. e. MNT: PRotein 0.8-1 g/kg IBW 80%, monitor potassium, sodium, and other minerals, fluids are unrestricted. Reference: Powerpoint from JWU, Janet Rouslin RD 3. Acute Renal Failure a. Definition: An abrupt decline in renal function with elevation of BUN and plasma creatinine levels. Oliguria or anuria is common in the first phase, although urine output may be normal or increased. b. Etiology: Chronic risk factors include diabetes, heart failure, HTN, other renal disease or damage, chronic liver disease, advancing age. Causes may be: prerenal (associated with alterations in the blood supply to the kidneys – hypovolemia, decreased cardiac output, obstruction of renal blood flow); intrarenal or intrinsic (damage to the kidney nephrons – inflammatory, lack of blood flow within the renal tubules, toxic effect of medications or other substances); or postrenal (obstruction to the urinary tract beyond the kidney – stones, UTI, strictures, tumor. c. Pathogenesis: There is rapid, often reversible deteroriation of the kidney function, GFR declines over days, most often occurs during hospitalization. d. Nutritional Status: Urine output is usually low, dehydration, electrolyte imbalances, watch BUN and creatinine. 6 Renal_2012 Due August 17, 2012 e. MNT: Energy BEE x1.2-1.3. Protein 0.8-1.2 g/kg. Fluid 24hr urine output plus 500ml. Sodium 2g, potassium 2g, phosporus 8-15 mg/kg Reference: Source: Byham-Gray, Wiesen, eds. A Clinical Guide to Nutrition Care in Kidney Disease. ADA, 2004 4. Chronic Renal Failure a. Definition: Progressive and irreversible loss of renal function. May take months to years to develop. b. Etiology: Diabetes is the leading cause, uncontrolled HTN is another common cause. CRF often results from other renal conditions, or from unresolved ARF. c. Pathogenesis of AFR and glomerulonephritis should be described above. Either can progress to CRF if not effectively treated. Continue with the pathogenesis from other causes here: Majority of the incidence comes from DM, or long term uncontrolled hypertension. GFR rate will continue to decline through the stages of chronic renal failure. d. Nutritional Status: Very compromised. Electrolyte imbalances due to edema and dehydration. caloric intake is ususally low to do lack of appetite. e. MNT: Protein based on energy expenditure,0.6-0.75 g/kg. No restriction on potassium. Monitor phosphorus and increase calcium. Reference: Fedje and Karalis. Nutrition mgt in early stages of CKD. Clin Guide Nutr Care Kidney Dis, ADA, 2004 5. End-stage Renal Disease (will discuss diet prescriptions in Nutrition Prescription section, can leave it out here.) a. Definition: Final stage of chronic, irreversible kidney failure. Less than 10% of renal function remains. Treatment with dialysis or transplantation is required. b. Etiology: May be last stage of chronic disease or resulting from infection or acute disease. Previous sections should discuss etiology. c. Pathogenesis: Regain glycemic control if DM is present. Control blood pressure. These will slow the progression. 7 Renal_2012 Due August 17, 2012 d. Nutritional Status:Prevent deficiencies, control edema and electrolytes, prevent renal osteodystrophy. Reference: Powerpoint by JWU, Janet Rouslin RD 6. Polycystic Kidney Disease a. Definition: Loss of kidney function due to the formation of multiple fluid-filled cysts in the kidneys. b. Etiology: This is most commonly a genetic disease. Autosomal recessive PCK (rare) occurs in fetuses and infants, half of whom die within a few days of birth, 25% live to their 10th year. Autosomal dominant PCK (90% of cases) is also genetic but generally doesn’t manifest until adulthood; symptoms usually start between ages 30 and 50. A third type is acquired cystic kidney disease (ACKD) most typically occurs in patients with kidney failure from other causes who have been on long term dialysis. c. Pathogenesis: Overtime can lead to kidney failure because these cycts cause strain and damage to the kidneys. d. Nutritional Status: No impact. e. MNT: Monitor electrolytes, BUN, creatinine, I&O. Prevent deficiencies. Reference: http://kidney.niddk.nih.gov/kudiseases/pubs/polycystic/ 7. Renal tubular acidosis a. Definition: Metabolic acidosis develops because kidneys don’t excrete excess acid into the urine and/or are unable to retain adequate bicarbonate to buffer the blood. b. Etiology: May be caused by drug or heavy metal toxicity, by autoimmune disorders, diabetes, or obstruction. Types 1 and 2 may also be hereditary. c. Pathogenesis: A secondary disease, so there is more than likely another disease or conditionn associated with RTA. These other diseases and/or conditions needs to be treated along with treatment for RTA. 8 Renal_2012 Due August 17, 2012 d. Nutritional Status: Patients with RTA have very acidic blood, some alternative practices say that eating foods with alkalinizing properties will help treat RTA. Foods with alkalinizing properties most often contain high levels of potassium which can be extremely harmful for patients with already high potassium levels due to other kidney problems. e. MNT: Recommend electrolytes per lab results. Monitor BUN, creatinine, albumin, prealbumin. Reference: http://www.livestrong.com/article/485719-diet-for-renal-tubular-acidosis/ D.) NUTRITION RELATED TOPICS 1. Describe the process of hemodialysis and how it works. How does CAPD differ from hemodialysis? Hemodialysis is a process that removes concentrated molecules and excess fluid from a patients blood through diffusion and filtration. The patients kidneys (that usually do this work) are not working efficently enough to properly filer the blood. Threfore the patient needs to be hooked up to a machine for hours a day so the bood to be filtered. CAPecontinuous ambulatory peritoneal dialysis, is another form of dialysis. In this patients do 45 exchanges of blood per day. A specific volume of dialysate is infused into the patients peritoneal cavity via a catheter. This dwells in the blod for about 4 hours as excess fluid and toxins diffuse through the membrane. The dialysate and wates are drained from the body and this process is repeated. 2. What is “dry” weight? Dry weight is the weight of a patient without any excess fluid build up. 3. Why would a dialysis patient be prescribed a daily water-soluble vitamin supplement instead of a regular multivitamin? Fat soluble vitamins like A, D, K, and E are not filtered when on dialysis. Therefore they can build up to toxic amount and can lead to complications such as anemia and hypertriglyceridemia. 9 Renal_2012 4. Due August 17, 2012 Discuss the causes of anemia in chronic renal failure. Are iron supplements an effective treatment? Why or why not? In patients with CRF, the failing kidneys lack the ability to secrete the hormone erythropoitein. Erythropoitein is a hormone that stimulates the bone marrow to produce red blood cells, these red blood cells are what carry oxygen throughout the blood. The iron in the blood is lost through dialysis, so is folate, an important part in red blood cell production. 5. How would a low serum albumin impact your interpretation of calcium labs and why? Calcium binds to the protein albumin, in the blood. Therefore if serum albumin is low calcium is also low in the blood. 6. Describe the influence of dietary oxalates on urinary oxalates. Give examples of foods with high bioavailability of oxalate that may increase urinary oxalate excretion. Oxalate is available in many kinds of fruits and vegetables. These foods contain berries, kiwi, grapes, figs, dark leafy greens, leeks, quinoa, celery, green beans, almonds, cashews, peanuts, soybeans, chocolate, and balck tea. Reference for this section: http://msl1.mit.edu/ESD10/kidneys/HndbkHTML/ch19.htm http://www.ncbi.nlm.nih.gov/pubmed/11135080 http://www.ncbi.nlm.nih.gov/pubmed/11135080 E.) NUTRITION PRESCRIPTIONS 1. For each of the following treatments, list the nutrient recommendations in the chart. Then answer the related questions below in your own words. Calories Impaired renal 30-35 function kcal/kg (non-dialyzed) Hemo-dialysis 30-35 kcal/kg Protein 0.6-1.0 g/kg 1.1-1.4 g/kg Fluid Sodium <2g 5002-3g/day 700+urine output Potas-sium <2g Phosphorous Calcium 800-1000 <2000mg/d mg/day ay ~40mg/kg individual individual IBW 10 Renal_2012 (CAPD) Transplant 2. Due August 17, 2012 30-35 kcal/kg 30-35 kcal/kg 1.2-1.5 individual 2-4g/day g/kg 1.3-2g/kg individual 80-100 mEq individual individual individual individual individual individual Give the rational for the protein restriction in impaired renal function. What are the hazards vs. benefits of this practice? What would you monitor to determine the adequacy of protein intake in these patients? Overworking impaired kidneys can result in a faster progression of kidney disease or increased damage. Keeping the protein restricted and frequently monitoring lab values can track the progress of the kidneys and see if eventually protein can slow be increased. 3. Why is it recommended for these patients to have at least 50% of their protein from sources that have high biological value (HBV)? Protein that comes from sources of high biological value are more beneficial. Patients on dialysis actually are having some of their protein removed from their bodies and to replenish that the more efficient way is from a diet rich in high biological value proteins. 4. Why are CAPD patients allowed more sodium, potassium and fluid than HD patients? Patients on hemodialysis need to restrict sodium, potassium and fluid more than CAPD patients because potassium builds between dailysis treatments and can cause complications such as weakness, muscle cramps, and irregular heartbeats. 5. When might CAPD patients need more protein than HD patients? Explain why. Patients on CAPD need more protein because there is a much greater risk for protein malabsorption than in patients on HD> 6. Why is fluid restricted in most hemodialysis patients? Make 4 suggestions to help patients control their fluid intake. 11 Renal_2012 Due August 17, 2012 Fluid restriction will help keep down the swelling, edema and fluid retention in a patient on hemodialysis. These can be dangerous to the patient by causing shortness of breath, irregular heart beats and possibly a heart attack. Suggestions 1. Fill a water bottle with the amout of water allowed in a day and only drink from there. 2. Try drinking out of small cups. 3. If you drink soda, buy the small 8oz cans and after one can, stop drinking soda. 4. If you feel thirsty, sip your water to get your mouth wet without drinking too much per sip. 7. Why is potassium a critical restriction in kidney failure? Damaged kidneys are unable to remove potassium from the blood. High levels of potassium in the blood can be toxic and cause things like abnormal heart rhythms. 8. List 6 commonly consumed foods or beverages that are high in potassium and suggest alternatives that would be acceptable and economical substitutions in menu planning. HIGH POTASSIUM FOOD Kiwi 9. LOWER POTASSIUM ALTERNATIVE Blueberries Grapefruit juice cranberry juice orange juice grape juice asparagus green beans spinach watercress tomatoes peppers List 3 potential problems resulting from an excessive sodium intake in a patient with kidney failure. Make 4 suggestions to help patients control their sodium and salt intake. 12 Renal_2012 Due August 17, 2012 3 Problems: 1. High blood pressure 2. Fluid retention 3. Hypernatremia 4 Suggestions: 1. Cook more at home- the salt you add to season your food with will NEVER add up to the sodium in processed foods. 2. Season food with natural flavors such as citrus zest/juice, spices, herbs, fresh aromatics. 3. Start a garden-eating food as fresh as can be and in season has the best flavor and often doesnt need any manipulation. 4.Frozen veggies over canned- in the winter months when fresh produce isnt always cost effective and readily available, frozen vegetables and fruits are much better than sodium soaked canned versions. 10. The balance between serum levels of calcium and phosphorus is difficult to maintain in patients with kidney failure, sometimes resulting in a condition called renal osteodystrophy. Discuss the following related to this balance: a. Give at least 3 reasons that serum calcium levels drop with progressive kidney disease. Calcium levels drop because there is a lack of serum protein (albumin) in the blood. The calcium binds to the protein, and the protein is not effectively filtered through the kidneys. b. How does kidney failure impact the regulation of calcium-phosphate product (also known as calcium-phosphate ratio)? How might these changes lead to osteomalcia? How might they lead to tissue calcification and why is this a critical issue? Osteomalcia occurs when there is not enough vitamin D in the diet, or there is a malabsorption of vitamin D by the intestines. c. List 5 foods that have the highest levels of phosphorus. Why are phosphate binders used? What are their nutrition related side effects? Bran, pumpkin seeds, sunflower seeds, toasted wheat germ, cheese. d. What are the diet modifications suggested for renal osteodystrophy? e. Would you suggest increasing milk intake to treat low serum calcium levels in a renal patient? Why or why not? 13 Renal_2012 Due August 17, 2012 Milk is a great source of calcium, however when it comes to a patient with renal conditions it is not the best option. Milk is very high in potassium which can be very harmful for renal patients. f. What is calcitriol and why is it often supplemented in kidney failure. Why must the response to calcitriol be carefully monitored? Calcitriol is a form of vitamin D that is used to treat and prevent calcium in the blood of patients whose kidneys or parathyroid glands are not working efficiently. Calcitriol will only work if the right amount of calcium is consumed by dietary sources. If too much calcium is consumed serious side effects may occur. If the patient is consuming too little calcium then the Calcitriol will not work to treat their condition. 11. Your patient is starting hemodialysis and has a nutrition prescription of: 35 kcal/kg, 1.2 g protein/kg, 2 g K, 1 g phosphorus, 2 g Na, 1,000 mL fluid + urine output per day; decrease saturated fat and cholesterol intake. She has approximately 200 ml urine output per day. Use a weight of 75 kg for the calculations. Consider her typical intake, plan a sample menu to meet her nutrition prescription. Do a nutrition analysis to show that your menu meets the recommendations. 14 Renal_2012 Due August 17, 2012 Typical Intake Sample Menu Recommendation Breakfast: Cold cereal (¾ c unsweetened), 2% milk (½c) Bread (2 slices) or fried potatoes (1 med potato) 1 fried egg (occasionally) Lunch: Bologna sandwich (2 slices white bread, 2 slices bologna, mustard) Potato chips (1 oz) 1 can Coke Dinner: Chopped meat (3 oz beef) Fried potatoes (1½ medium) HS Snack: Crackers (6 saltines) and peanut butter (2 tbsp) Nutrient Analysis: Calories: 2400 , Protein: 89g , Potassium: 1954mg, Sodium: 1600mg, Phosphorus: 1000mg , Fluid: 56oz/1600ml References for this section: www.andrew.cmu.edu/~sorensen/ Menu Breakfast Rice flakes 2 cup Whole milk 1 cup Cranberry juice 16oz Coffee 8 oz Bread 2 slices Jam 2T Lunch 15 Renal_2012 Due August 17, 2012 2 slices white bread 2 slices turkey Lettuce Mustard Peppers Soda water with lemon 16 oz Apple sauce with fresh blueberries 1 cup Dinner Chicken 6 oz Brown rice .75 cup Green beans 1 cup Water 8 oz Salad Spinach Iceberg Peppers Oil Vinegar Snack Popcorn 3 cup Iced tea 8 oz Nutrient Analysis: Calories: 2400 , Protein: 89g , Potassium: 1954mg, Sodium: 1600mg, Phosphorus: 1000mg , Fluid: 56oz/1600ml 16