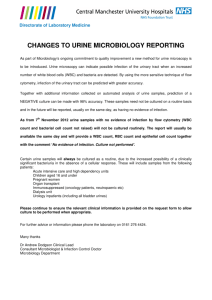
Document
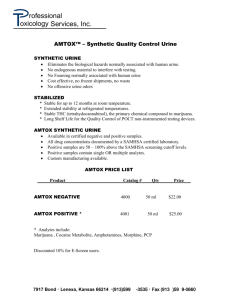
advertisement

PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni PATHOLOGICAL ANALYSIS - Histopathology analysis General analysis Bacteriology analysis Serology analysis Semen analysis Biochemistrys and Hematology analysis First \\ Histopathology analysis Disease Is in abnormal condition of a living thing, pathology is that branch of biology that involves the study of living things in their abnormal forms and conditions is the development and the structural and functional changes produces by them. The pathologist acts a consultant to physicians in diagnosis of disease during life and after death by the laboratory chemistry microbiology hematology examination of surgical removed specimens and autopsy or postmortem examination Individual + disease = Illness Etiology Refer to the cause of disease and contributing factors. (Ecological, Immunological, Physiological) Pathogenesis Refer to the mechanism of development of disease and it is the ability of M.O to cause disease by ability to initiation of the infection process and the mechanism that lead to the development of signs and symptoms of disease. 1 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni Lesion The characteristic change in an organism produced by disease is a tissue cellular or molecular alternation that develops as a result of disease-producing or pathogenic agent ex. Sickle-cell which is due to abnormal hemoglobin molecules with abnormal pattern of amino acid in the protein lobar pneumonia tumor of the lung, hemorrhoid, boil, hemolytic disease of the new born (coated RBC). Cellular adaptation The changes that are intermediate between the normal cell and injured cell. The most important changes of cellular adaptation are: 1. Induction of endoplasmic reticulum development of more endoplasmic reticulum EPR due to drug administration over a period of time. Ex: increase amount of (EPR) in liver can detoxify many drugs. 2. Atrophy : is shrinkage of cell by loss of cell substrate or decrease in the size of organ due to decrease in the size of cell and a trophy is the partial or complete washing a way of a part of the body. Causes of a trophy include: Poor nourishment Poor circulation Loss of hormonal support Loss of nerve supply to the target organ Atrophy is a general physiological process of reabsorption and breakdown of tissue involving apoptosis on a cellular level. When it occurs as a result of disease or loss of trophic support due to other disease or loss of trophic support due to other disease. It is termed pathological atrophy. 3. Hypertrophy An increase in size of the cell lead to increase in size of organ new cell are not formed there is enlargement of cell. Ex: muscles of body bilders. 2 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni 4. Hyperplasia An increase in number of cell in an organ or tissue due to mitotic activity that lead to increase in size or volume. Ex: breast during pregnancy (physiological) and lactation thyroid hyperplasia (pathological) 5. Hypoplasia, Failure of an organ To reach full adult size (lung kidney) Aplasia, Agenesis. total failure of an organ to develop 6. Metaplasia Is a reversible change in which one adult type is replaced by another adult cell type as a result of chronic irritation. Ex: pseudo stratified ciliated columnar epithelium in tracheobronchial tree to stratified squamous epith. In the habitual cigarette smoker. Cell injury and response The cell is the basic functional unit of the organism all abnormalities in the normal processes of the body that result from injury or disease must originate in the cell. The causes of injury: 1. Physical: trauma heat cold radiation electrical energy Ex: burning freezing cell or effect on the molecular structure. 2. Chemical agents: acids, alkalies, poisons may destroy the membranes, alter cell functions or may cause death. 3. Living agents, bacteria viruses, Rickettsiae and parasites. 4. Nutrition disturbance deprivation in proteins or vitamins. 5. Genetic defects-hereditary disease or mutation during development. 6. Disturbance in arterial circulation-loss of blood supply. 7. Derangement in the immune mechanism-Ag stimuli. 8. Regressive changes in brain muscle and gonads (testes and ovaries) 3 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni Reversible cell injury and degeneration: Degeneration : changes that occur in the cell following injury. The most common reaction to cell injury are swelling with or without appearance of abnormal substance in the cytoplasm. They may still be reversible if the nucleus remain unimpaired and the injurious agent is removed or destroy before nuclear damge (changes are found in the cytoplasm may be reversible. Types and reversible degeneration: a) Cellular swelling : in acute infection or poisoning is the most common type of acute degeneration, M\S: the cell appear swollen their outlines may not be clear there is damage to the plasma membrane and disruption of mitochondria. Best seen in parenchymal cell of heart kidneys and liver. b) Hydropic degeneration : great cellular swelling due to highly absorption of water by the cell. M\S: fine or coarse vacules in the cytoplasm. Best seen in epithelial cells of tubules of kidneys. c) Fatty change : accumulation of fatt in the cytoplasm M\S: a small membrane - bound inclusion closely to the endoplasmic reticulum, small vacuoles in the cytoplasm accumulate to form large clear space. The vacuoles displace the nucleus to the periphery. Often seen in liver, kidney and heart. d) Hyaline degeneration : structurless, smooth, homogenous, glassy appearance, stains pink with hematoxylin. Ex: old scar tissue - yellow fever in liver, or cirrhosis of the liver. e) Amyloidosis : proteinaceous material that accumulate extra cellular in tissue and organs. f) Mucinous degeneration : carbohydrate and protein, appear blue. Ex: catarrhal inflammation - epithelial tumor cell. g) Mucoid degeneration : change that occur in connective tissue defer from mucinous deg. By higher sulfer content. 4 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni Irreversible cell injury (Necrosis) It is the cell or tissue death in the living body & resulting from the temporary or permanent loss of the blood supply to the tissue. Cytoplasmic degeneration followed by loss of cell structure fragmentation of organelles & liquefaction of the cytoplasm and nuclear change necrosis is less orderly than apoptosis, which is part of programmed cell death. In contrast with apoptosis, clean up of cell debris by phagocytes of the I.S is generally more difficulty as the disorderly-Death generally dose not send cell signals which tell nearby phagocytes to engulf the dying cells this lack of signaling makes it harder for the immune system to locate and recycle dead cells which have died through necrosis than if the cell had undergone apoptosis. The release of intracellular content after cellular membrane damage is the cause of inflammation in necrosis. Causes include: physical, chemical, bacterial or viral, Prolonged exposure to injury, infection, comcer, poisons & inflamma. Types a. Coagulation necrosis loss of cellular details Ex: heart infarction. b. Liquefaction nec. – softening & Liquefaction of the dead tissue Ex: infarcts of the brain. c. Caseous necrosis – soft cheesy appearance. Ex: Tuberculoses necrosis. d. Gummatous nec. – not soft, but rubbery and firm. Ex: Tertiary lesion of syphilis. e. Fat necrosis – associated with pancreatic injuries or disease while spots in the tissues, foci surrounded by RBCs + PMN later become seat of Ca++ deposition. f. Gangrene – caused by cuts off the circulation suddenly in diabetics from atherosclerosis, by trauma, pressure, freezing or infection by Cl. Perfringens. g. Zonal necrosis : the injurious agent effect a certain zone. Ex: phosphorous & ca tetrachloride cause zonal necrosis of the lobule of lymph node. h. Focal necrosis : minute foci of dead tissue – Ex: lesion found in liver in typhoid fever. 5 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni Inflammation Is the local reaction of the living body to any injury. It is a well – coordinate series of vascular and cellular reactions occurs at site of injury The object of these reaction is: a. b. c. d. e. To destroy or remove the injurious agent. To limit its spread. To neutralize toxins. To remove the remnants of destroyed tissue. To prepare the area to the final repair of the damage. Etiology (causes): Physical → heat, radiate Chemical → Alcohol, acids Mechanical → cut Mo. → Bact Exudates Inflammatory edema fluid, highly protein content, high cell counts, low glucose content, some times clots due to fibrinogen content, its function is to dilute toxins, brings various types of Abs, and limitation of some infection. Classification of inflammation: 1. According to duration: Acute, Sub acute, chronic. 2. According to type of exudates: a. Serous : Watery inflame – edema fluid. b. Fibrinous containing large amount of fibrinogen which ppt. c. Catarrhal : Mucus. d. Purulent or supportive : pus in large amount. e. Hemorrhagic : RBCs + exudates. f. Fibrinopurulant – Fibrinogen + PUS g. Mucopurulent : mucin + PUC. 6 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni Inflammatory Cells: Are derived from leukocytes of blood and certain tissue cells. The normal proportion of WBCs in blood are: Neutrophils Basophiles 54% - 73% Monocytes 24% - 8% 0% - 1% Eosinophils 2% - 4% Lymphocytes 21% - 35% Bloods cells: 1) Granulocytes : polymorphnucleur leukocytes a. Neutrophils :- are the first cells to accumulate in acute inflammatory response, directed by chemotactic agents, they are actively phagocytic, they are the chief cells in pus. b. Eosinophils :- phagocytic cells, respond chemotactically to split C3 & C5 – seen in allergic responses and in healing phase of infl. c. Basophiles :- they have met achromatic granules that contain heparin and histamine. 2) Monocytes and Macrophages : both are phagocytic, taking up large & small particles, dead cells, cellular debris and erythrocytes – kill the organism they ingest – Monocyte leave the blood stream to become tissue macrophages. 3) Lymphocytes : small round cells, less motile related to immune system. Tissue cells: 1) Mast cells : similar to basophiles, they contain heparin & histamine. 2) Histiocyte or tissue macrophages : highly phagocytic especially when particulate matter is to be removed, like carbon particles, part of necrotic cell and M 0. 3) Giant cells : multinucleated cells may contain 50 or more nuclei found in tissue formed by fusion of histiocytes. 4) Plasma cells : not normally found in blood, not phagcytic, produce large quantities of Igs. 7 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni Acute inflammation signs: Swelling, heat, redress, pain and disturbance of function. Sequence of events in acute inflammation - Increase in permeability of venules and capillaries. - Exudation of fluid rich in proteins – albumin and globulins, followed by fibrinogen – between the junction of endothelial cell of venules. - Concentration and packing of erythrocytes. - Slowing of blood stream, stasis. - Emigration of neutraphils first, monocytes seconds, then others aided by chemo taxis. - Accumulation of WBCs and fluid in area of irritant. - Phagocytosis of irritants by neutrophils & monotypes of M.O - Reversal of vascular changes. - Fluid reabsorbed by venules and by lymphatic drainage. - Repair by ingrowths of capillaries and fibroblasts. Repair Is the process by which the tissue returns to normal or approximately normal state. Cells that have been destroyed are either replaced by healthy cells of the same type growing in from adjacent living tissue (Regeneration) or by the replacement of dead cells by fibrous tissue and new blood vessels that also come from uninjured neighboring tissues (granulation tissue or scar tissue). Is one of the end stage of inflame. Microscopic features of a cute inflammation :The acute inflame – lesion shoes varying proportion of : 1. Serous exudates. 2. Fibrin. 3. PMN leukocytes. 4. large mononuclear cells. 8 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni According to the character of the exudates, acute in flam : are classified as follows: 1. Acute serous or serofibrinous inflame : Occurs on serous membranes such as pericardium, pleura or the peritoneum. It may be absorbed completely or organized by the ingrowths of connective tissue. 2. Purulent : predominance of pus cells PMN, it may localized to form an : a. Abscess, which heals by walling off fibrous tissue and scar formation. b. Diffused to the surrounding tissue and invade blood stream (Pyemia) – often caused by streptococci, pneumococci. 3. Hemorrhagic : exudates contains large numbers of erythrocytes due to capillary injury and rupture, (e.g. hemorrhagic cystitis). 4. Catarrhal :- relatively mild, seromucinous exudates on the mucus membrane, later becomes mucopurulent. Ex: in flam of the upper respiratory or alimentary tract. 5. Pseudo membranous or diphtheritic in flam : Is formed by fibrinous exudates over a necrotic layer of mucosa. Ex: in diphtheria, in alimentary tract of person receiving large quantities of some antibiotics, and in infection with resistant staph. Chronic inflammation Is a process in which exudative changes are prolonged and proliferation of connective tissue is the dominate feature of the raction. The cellular of reaction consist primarly of lymphocyte, plasma cell and macrophages together with newly formed collagenous fiber. This chrortic process often follows an scute inflammatory one. When pus associated with chronic lesion, it is termed chronic supportive inflammation (chronic supportive osteomyelities). The proliferative activity lead to the formation of abundant scar tissue, which may in itself harm full. Ex: chromic nephritis where progressive glomerular scaring result due to functional failure of the kidney. Other cells may involved in chromic inflame : histiocytes, fibroblast, zosinophils + Basophiles and Giant cells. 9 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni Inflammation and cancer Some types of cancer arise from tissue irritation. And inflammation in fact, in the body, inflammatory cells such as neutrophils can play the role of turncoat by helping tumor cells multiply and spread. Some tumors have been likened to "Wounds that wont heal". Melanoma, which is caused by too much exposure to ultraviolet light from the sun, is thought to be caused in part by uncontrolled inflammation of the skin. In recent years, scientists have unveiled another link between inflammation and cancer. Medicine that block inflammation, such as aspirin, Tylenol and other so – called non-steroidal anti-inflammatory drugs (NSAIDs), have been shown to prevent certain kinds of colon, lung, mouth and stomach cancers. 10 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni Second \\ General analysis includes: General Urine Examination (G.U.E): Urine is a complex aqueous mixture consisting of %96 water +4% dissolved substances, most of which either are derived from the food eaten or are waste products of metabolism. The dissolved substances consist primarily of urea (the principle end products of protein metabolism, Nacl, sulfate and phosphates). This dissolved substances in Normal urine may be divided into: 1. The normal organic substances includes: Urea, Uric acid and Creatinine. 2. The normal inorganic substances include: (Cation: Na+, K+, NH 4 ) (Anion: Cl , PO 43 , Sulfate SO 4 2 ) 3. Normal urine Specimen also contains certain formed elements in low concentration, like Red blood cells, Pus cells and epithelial cells. Cellular Constituents I) Red Blood Cell RBCs are abnormal urinary constituents and the presence of more than two per high power field (H.P.F) is always of pathological significance. The condition in which RBCs are found in the urine is termed as hematuria. The distinguish between hematuria and hemoglobin uria that the last one mean presence of free hemoglobin in the urine. The degree of hematuria may vary from a frankly bloody specimen on gross examination to a specimen that show no change in color. II) Leukocytes (white blood cells, pus cells) The presence of a few leukocytes in urine is normal. More than an occasional cell (1-5/H.P.H) is considered abnormal.The presence of large number leukocytes in the sediment indicates inflammation at some point a long the urogenital tract. The inflammation may result from a bacterial infection or other causes. 11 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni III) Epithelial Cells (E.C) The structures that make up the urinary system consist of several layers of E-C, except for the single-layered tubules of the nephron. The E.C of organs such as the urethra and bladder (besides the contaminating cells of the male and female genital tracts) are continually sloughed off into the urine and replaced by cells originating from deeper layers. Therefore, urine always contains some E-C. IV) Casts Casts are long cylindrical structures that result from the solidification of material within the lumen of the kidney tabules. They are important because anything that is contained within the tubules is flashed out in the casts. Casts may be formed at any point of the nephron, either by precipitation of protein or by grouping together of material within the tubular lumen. Since cast represent a biopsy of the kidney, they are extremely important clinically. They are often contain RBCs., E-C, fat globules, bacteria and leukocytes. The types of the casts: 1) Hyaline cast 2) Granular casts 3) Blood or RBC casts 4) Leukocytes casts 5) Tubular epithelial casts 6) Waxy casts 12 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni When give normal result to (G.U.E): 1. The color of urine varies from pale to deep amber. 2. The specific gravity range between 1.008-1.030. 3. The appearance of the urine is clear. On standing Ammonia maybe formed by bacterial decomposition of urea, the resulting decreases of acidity which may cause cloudiness due to precipitation of calcium phosphate. 4. Contains minute traces of protein and sugar that not detect by routine methods. 5. Contains a few sequamous epithelial cells. 6. Urea found in rate about 2 mg/l When give abnormal results to (G.U.E): 1. Contain red blood cells (hematuria). 2. Contain white blood cells. The presence of large numbers of leukocytes in the sediment indicates inflammation which may results from bacterial infection or other causes. 3. Contain epithelial cells which results from continually sloughed of E.C into the urine and replaced by cells originating from deeper layers. 4. Contain Casts. How can make G.U.E? 1. Take urine specimen Ideal specimen for microscopic analysis of the urinary sediment is a fresh & first morning specimen, because it is most concentrated and is particularly important for reliable results. Several changes that may occur as the urine stands which are include: Red blood cells become distorted because the lack of an isotonic solution. White blood cells disintegrate in hypotonic solution Cast disintegrates, especially as the urine becomes alkaline because they must have sufficient acidity & solute concentration to exist. 13 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni 2. Gross examination of urine Physical properties of urine Urinalysis usually involves an assessment of physical properties, such as volume, colour, transparency and specific gravity. 1st) Volume The volume of the urine is not measured as a part of a routin urinalysis. However, in certain conditions the volume of urine excreted in 24 hours is a valuable aid to clinical diagnosis. In normal adults with normal fluid intake, the average 24 hours urine volume is 600-1600 ml. under normal conditions, there is a direct relation between urine volume and water intake. Polyuria : The consistent elimination of an abnormally large volume of urine, over 2 L in 24 hours. Oigouria : The excretion of an abnormally small amount of urine less than 500 ml in 24 hours. 2nd) Colour The normal colour of the urine varies from pale yellow to deep yellow, the normal colour of urine seem to result from the presence of three pigments: urochrome, uroerythrin and uribilin. Urochrome is a yellow pigment and is present in larger concentrations than other two. Uroerythrin is a red pigment and urobilin is an orange-yellow pigment. Colour of urine and disorder: 1) Pale urine may be associated diabetes mellitus or diabetes insipid us. The first one with sugar and high specific gravity. Also pale urine seen with a large quantity of protein in the nephritic syndrome. 2) Dark yellow or brown-red indicate of very concentrated constituents and low volume. It is ofyen seen in fever. 3) yellow-brown indicates the presence of bilirubin. 4) Drange-red or orange-brown indicate urobilin or urobilinogen . 5) Clear red is characteristically contains hemoglobin . 6) Cloudy red is characteristically the presence of RBC. 14 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni 3rd) Appearance When voided, urine is normally clear and most urines however, will become cloudy when allowed to stand. The causes of cloudiness may be solid materials that will be visible under the microscope. There are numerous words have been used to descried the degree of transparency of a urine specimen like, clear, cloudy, very cloudy and turbid. The causes of the cloudiness are: 1) On standing cloudiness may result from the presence of mucin, or mucous threads in the urine. 2) Inflammatory state of the lower urinary or genital tract. 3) Amorphous phosphates and occasionally carbonates. 4) Bacteria are another common cause of cloudiness in urine specimens that have been allowed to stand. In this case bacteria are not clinically significant. 5) Spermatozoa or prostatic fluid may also cause cloudy. 6) Amorphous urate in acidic urine. 7) WBC or pus will be seen as white cloudiness. 8) RBC and vaginal contamination. 15 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni 4th) Specific gravity The kidney is a regulator of the volume, acidity, composition and osmotic pressure of the extracellular fluid. A measurement of the specific gravity of urine is one means of assessing the ability of the kidney to regulate the composition and osmotic pressure of the extracellular fluid. Specific gravity of urine is a measure of the amount of dissolved substances present. More technically specific gravity describe the weight of a solution compared to the weight of an equal volume of water. It is the ratio of the density of the solution to the density of pure water density is the mass or weight of a substance per unite volume. Clinically, the S.G of urine may be used to obtain information about two general function the state of the renal epithelium, and the state of hydration of the patient. The normal value of S.G is 1.008-1,030. However, if the renal epithelium is not functioning adequately, it will gradually lose the ability to concentrate and dilute urine. 16 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni General Stool Examination (G.S.E) : Brown soft mass is normal stool specimen. The normal color influenced by diet & the formation of this color requires bacterial oxidation to take place in the Colon. The brown color of stool is caused by stercobillin (pigment derived from bilirobin after conversion to arobilin). When give normal result to (G.S.E) A soft but formed stool specimen is normally seen with brown color. When give abnormal or pathological results to (G.S.E) 1. Seen yellow to yellow green color: This indicates found diarrhea or the normal bacterial flora are not present in the bowel as in antibiotic therapy. 2. Appear clay color: occur when stercobilin is absent & there is some increase in fat. 3. The specimens are bulky, torthy, foul- smelling and found abnormally in large amounts of fat in the faeces, this case associated with cystic fibrosis and is called steatorrhea. 4. Dark specimens may be seen after the ingestion of iron and formed when bleeding from the upper gastrointestinal tract& the bloody specimen usually associated with disease of the lower rectum & anus. 5. Mucous & pus seen in faeces associated with inflammatory conditions such as colitis or a bowel tumor but pus only seen in disease such as ulcerative colitis & bacillary dysentery. 6. In faeces may be seen adult round worms or segments of tape worms macroscopically. The most important intestinal parasitic infection of human are: Class: Amoebae, Entamoeba histolytica Class: Flagellates, Giardia lamblia Class: Ciliates, Balantidium coli 17 PATHOLOGICAL ANALYSIS Class: Sporozoa, Dr. Wafaa S. Al wazni Isospora haminis Third \\ Bacteriology analysis : A. Infection of wounds &other tissues B. Infection of Blood C. Infection of CSF D. Infection of upper respiratory tract infection E. Infection of lower respiratory tract infection F. Infection of Gastrointestinal tracts G. Infection of Urinary tract A. Infection of wounds & other tissues There are many types of these infections are: Nosocomial wound infection Ex: Staph aureus Pseudo aeranginosa Coliform bacilli Soft tissue infection: Ex: many of aerobic & anaerobic bacteria Burns: Ex: S. aureus , P. aeroginosa Bone infections ( osteomyelitis) - S. aureus & coliform bacilli in infants - Group A Streptococci & H. influenzae in children - Various G -ve cocci & bacilli in adults. 18 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni In order to make the laboratory test for these infections should be follow these steps: Specimens Pus, exudates or fragments of tissue& pieces of abscess wall, if the patient is febrile or in shock a sample of blood should be taken for culture. Lab Examination include 1. Naked eye examination: The appearance of pus or exudates depended on colour, consistency& odor. The pus is creamy & Ex: Staphylococcus lesions. thick in consistency with pus cells. The pus is watery & straw colored. Ex: Str. pyogenes. The pus with fishy smell. Ex: Proteus infection. The pus with a sweat – musty odor & often blue pigmentation. Ex: Pseudomonas infection. The pus has an offensive putrid smell. Ex: Anaerobic organisms’ infections. 2. Microscopy examination: Gram stain show bacteria which belong to one of these types: - G+ve Cocci in clusters (Staph) or in chains (Strep) or Diplococci (Pneumococci) - G +ve filaments (Actinomyces) - G +ve rods large straight (Cl. perifringes: gas gangrene), (B. anthracis: anthrax) - G -ve rods (E. Coli, Klebsiella, Proteus, Serratia, Pseudomonas) Ziehl - Neelson stain Mycobacterium Nocardia 19 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni Immuno fluorescent staining with specific antisera for some pathogenic Clostridia. 3. Culture After taking specimen from a patient, should be cultured on one type of these media: CULTURE MEDIA Blood agar Cook meat broth Thioglycocte broth Macconkey agar Sabouraud dextrose agar Lowenstein jensen media Aerobically (in 5-10% CO2) Blood agar G –ve rods Yeast Acid fast rods -Coaqulase -Mannitol salt agar Anaerobically In N or H 5-10% CO2 Biochemical tests Staph Clostridium 20 Mycobacterium PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni B. Infection of Blood (Bacteraemia) The blood is sterile fluid, does not contain any M.O or toxic substances. The transient reach of fungi or bacteria to the blood and the blood serves as site of presence of bacteria, but the bacteria usually cleared from the vascular system with no harmful effect this called bacteriamia or fungimia, but the condition in which blood serves as a site of bacterial multiplication as well as a mean of transfers of infections a gents fromone site to another, this called septisemia. The most common causes of these infections are: G +ve Cocci .Ex: S. aureus, S. epidermiles G -ve Cocci. Ex: N. meningitidis G +ve bacilli. Ex: L. monocytogenes Clostridium G -ve bacilli. Ex: Enterobacterasea family Fungi. Ex: Candida albicans, Cryptococcus neoformans Specimens : 10 ml of blood for adults, 2-5ml for children and 1-2 ml for infants is transported to the lab in a tube containing anticoagulant solution or added to the blood culture bottles. Note: One to 3 blood cultures should be taken separated by 1hour intervals or less if treatment cannot be delayed, so that the chance of missing a transient bacteraemia is reduced and the pathogenic role of S. epidermidis is confirmed. Lab Examination (Blood culture) 1. The blood should be mixed with 10 times its volume of broth (5 ml blood in 50 ml broth which is tryptic soy broth (TSB) to dilute any antibiotic present and to reduce the bactericidal effect of serum. 2. Incubated the bottle at 37°C for 7 days. A sterile culture shows a layer of sedimented R.B.Cs covered by a pale yellow transparent broth, but microbial growth is evidenced by a floccular deposit on top of the blood layer. Turbidity, haemolysis, coagulation, gas production and white grains on the surface or deep in the blood layer. 21 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni Blood culture bottles after Incubation for 24h at 37°C Gram stain and Subculture G –ve rods MacConkey agar Biochemical test for detection of bacterial genesis G+ve Cocci Staph Strept Mannitol salt agar Blood agar with optochin, tellurite& bacitracin discs CAMP test (Bile esculine agar) 22 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni C. Infection of CSF (Meningitis) CSF is sterile, clear and color less, contains 0-5 leukocyte/mm3 & no RBC. There are 2 types of meningitis which are: 1. Purulent meningitis (CSF is turbid & contain 100-3000 PMNs/ mm3 ) Ex: H. influenzae N. meningitidis In all age groups But in infants (to 2 months) Ex: E. coli Salmonella spp L. monocytogenes 2. A septic meningitis (CSF is clear or slightly turbid, contains 10-500 leucocytes/mm3, mostly lymphocytes). Ex: Candida albicans Leptospira Specimens 1. 3-5ml of CSF is collected in two sterile tubes, one for chemical examination (glucose& protein), the other for microbiological examination & leukocytes count. 2. Blood culture should be collected because meningitis is often associated with bacteraemia. 3. The appearance of CSF should be noted: Clear, turbid, purulent, yellow (previous hemorrhage), contamination with blood. Lab Examination Microscopic examination which represented by: a) Direct examination for leukocytes, RBCs, Bacteria, yeast. b) Gram stain: very important because the culture depend on its result. c) Acid fast stain for tuberculosis meningitis. CSF culture As shown in this diagram: 23 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni 24 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni CSF G+ve Cocci CAMP test & optochin sensitivity for Strep. Blood agar Chocolate agar G –ve rod G –ve rod N. meningitidis Catalase test +ve, motility +ve, bile esculin agar (growth& black discoloration) for Listeria monocytogenes Macconkey agar& biochemical tests for enterobaceriaceas Oxidase test Slide aggl 25 Blood agar with S. aureus Lowen stain Jensen media H. Influenzae (Satellite colonies) Tuberculosis Slide aggl PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni D. Upper respiratory tract infection : The Upper respiratory tract extends from the larynx to the nostrils and communicating cavities the sinuses & the middle ear. There are many types of infection: Pharyngitis(sore throat) Nasopharyngitis Otitis media Sinusitis Epiglottitis Diphtheria (laryngitis & tracheitis) Diphtheria One of the important diseases caused by C. diphtheria which spread by droplets or by contact. The bacteria multiply locally without invading deeper tissue or spreads through the body. The toxin destroys epithelial cells & PMN & an ulcer from which is covered with necrotic exudates forming a false membrane (pseudo membrane) over the tonsil pharynx & within the membrane produce toxin which is absorbed into the lymphatic & blood, it cause fever pallor, exhaustion, mycocarditis & polyneuritis with paralysis of eye muscle. Specimen Should be collected after the tongue is kept down with a tongue depressor & a sterile cotton-wool swab is rubbed vigorously over each tonsil over the back wall of the pharynx & over any other inflammation area. Direct Microscopy Gram stained smear& the direct smear has specificity for the detection of the diphtheria bacillus which appear rod club shape with irregular swell at one end; but when stained with methylene blue, cell in stained smear tend to be parallel or at acute angles to one another. 26 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni Culture The swab should be rubbed over blood agar plate and Loffler coagulate smear (selective media for C. diphtheria), then incubation for 24h at 37°C. After growth appears complete other test to detect the type or genus of bacteria. Elek test Detection of toxin (Gel diffusion precipitin reaction) by producing serum in horses. 27 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni E. Lower respiratory tract infection : All infection occurring below the level of the larynx which involved trachea & lung tissue; such as: Epiglottilis Laryngotracheobronchiotitis Whooping cough Acute bronchitis Acute Pneumonias ( Labor pneumonia ) Chronic chest disease ( Tuberculosis ) Whooping cough The bronchial & pulmonary secretions of exudates are often studied by examination sputum; the most misleading aspect of sputum examination is the almost inevitable contamination with saliva & mouth flora. Thus finding Candida, S-aureus, even Streptococcus pneumonia in the sputum of patient with pneumonitis has no etiologic significance unless supported by the clinical picture. In whooping cough the personal swab in a special transport media is required, because this disease is highly contagious infection occur by respiratory droplet contain Bordetella pertussis which causative agent for this infection & not invade tissue or enter the blood but produce an endotoxin able to destroy the cilia cells, which in turn allows mucus to accumulate or the M.O attach to & multiply in the ciliated respiratory mucosa but don’t invade deeper & the surface component play important role in specific attachment to respiratory epithelium. 28 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni Tuberculosis Is a chronic disease caused by mycobacterium tuberculosis it most common in being but may occur in other organ, mode of infection by inhalation of droplets, (coughing, sneezing). M/S: appearance of large mononuclear cells, histiocytes, which become the characteristic large epithlioid cell with vesicular nuclei and abundant cytoplasm. Organization may occur & result in fibrous scarring in some cases, or aggressive disease may produce abscess. Resolution of the exudates usually restores normal lung stricture but this impaired sometime by organization, scarring & abcess formation. Lobar pneumonia This pattern of acute bact. Inflation involves a large portion of or an entire lobe of the lung. Most lobar pneumonias are caused by pneumococci, which enter the lung via airways. Occasionally they are caused by other organisms (Klebsiella, pneumonia, stash., strep, H. influenza). The following sequence of stage is ((classic)) but infrequently seen because of antibiotic therapy. However, the various stages portray the natural history of uncomplicated lobar pneumonia. Congestion Predominates in the 1st 24 hours. Red hepatization (consolidation): describes lung tissue with confluent acute exudation containing neutrophils & red cells, giving a red, firm, liver – like gross appearance. Gray hepatization: as red cells disintegrate & the remaining fibrinosuppurative exudates persist, giving a gray brown gross appearance. Resolution is the favorable final stage in which consolidated exudates undergoes enzymatic & cellular degradation & clearance. After these stages, normal structure is restored. 29 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni Collection of sputum specimen: The sputum should be collected in a sterile container with a secro, & send to the lab without delay. If the sputum is allowed to stand after collection over growth of contamination of bacteria may take place before the examination is carried out. Lab examination: Include: Microscopic Examination : A portion of purulent or mucopurulent sputum should be used for the preparation of Gram stain smear which give first impression for some M.O responsible for infection such as S. aureus , H. influenza ( coccoid bacilli, some times occurring in pairs or short chains ), & Bordetella pertussis in swab (cocco bacilli with Toludine blue stain, bipolar metachromatic granules can be demonstrated ). Culture: Select the purulent material in sputum or swab & incubate on the various culture plates which include: - Blood agar - Chocolate agar - Macconkey agar These agars incubated for 24h at 35-37°C & reincubation for an extra 24 hours when growth is less than expected; but swab taken from Nasopharyngeal of patient with whooping cough can culture on Bordet - Genqou medium (potato-blood-glycerol media) in a moist environment (in sealed plastic bag) or cough droplets expelled on to a cough plates, held in front of mouth during a paroxysm. 30 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni F. Gastrointestinal tract infection Acute diarrhea with or without vomiting is a common complaint. Microbial causes, either by multiplication in the intestine or from the effects of preformed toxin, are the most important reasons for acute gastro-intestinal upset in or otherwise healthy individual. The common microbial causes of infections intestine disease are : Viruses: Rotavirus, Astrovirus, Calicivirus. Bacteria: Salmonella Spp., Campylobacter Spp., Shigella Spp., E. coli, Vibrio cholera, V. parahaemolyticus, Yersinia enterocolotica. Protozoa: Cryptosporidium parvum, Entamoeba histolytica, Giardia lamblia. The GID can be divided into many types: a) GID associated with toxin producing M.O: Enterotoxin: caused by Clostridium botulinum, botulinal toxin after absorption into the blood stream, the toxin binds to the presynaptic nerve ending of the peripheral nervous system & cranial nerves, where it inhibits acetylcholine release. Cytotoxin: disrupt the structure of intestinal epithelium, Ex: Shigella dysenteriae. But in V. cholera produce entrotoxin diarrheal disease. The bacteria remain within the intestinal tract attach to microvillis of the brush border of epithelial cells. There the bacteria multiply & liberate Cholera toxin, that cause rice water stool contain mucus epithelial cell& large numbers of vibrios without PMN or blood. b) GID associated with invasive mucous: Certain parasites, Ex: Entamoeba histolytica invade the colonic mucosa, producing characteristic ulcerative lesions& a profuse bloody diarrhea (dysentery). The stool specimen examined by direct microscopy & the E. histolytica maybe recognized by its active movement, pushing out fingerlike pseudopodia & sometimes progressing across the microscopic field. 31 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni c) GID associated with adherent microorganisms: Ex: Giardia lamblia, which attached to the mucosal surface of the upper small intestine & cause malabsorption of fat & chronic diarrhea. Under microscope the G. lamblia is kite-shaped with two nucleated sucking pads& four pairs of flagella. Specimens Faecal specimens should be collected in the early stages of disease, in a sterile container & these specimens should be processed as soon as possible & not stand longer than 2 hours after collection, if it is not possible the specimen collected on swab & then incubated in a suitable transport medium & then make smear & stain. Laboratory examination Naked eyes examination: The stool specimen should be directly examined to determine: - The consistency (solid or liquid (diarrhea)) - Color (white, yellow, brown, bloody) - Typical components (mucus, blood (dark to black)) Microscopically examination: Saline & iodine preparation should be made & examined with low & high power; various ova may be seen in feces. Ex: - Hook warm - Ascaris (Round warm) - Taenia - Trichuris trichiura 32 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni Culture includes these steps: Preparation of fecal suspension & inoculation on agar plates: The stool should be suspended in saline to obtain a turbid suspension but liquid stool do not require the addition of saline. Inoculation of specimen There are differences for adult & child. For adults: the specimen should be inoculated on tetra thionat broth for the harvestation of Salmonella & Shigella from stool because these bacteria found in small number in stool. Then cultured on MacConkey if appear pink colonies the result is Negative & these colonies neglected but when other colonies should be transfer to the S.S Agar for detection of Salmonella & Shigella bacteria, appearance of black colonies indicates Salmonella but white colonies indicate Shigella. After that serological identification should be performed. Transfer stool specimen to peptone water (PH 8.6) after 6-8 hr incubation on TCBS (Thiosulfate- Citratebile-Sucrose) after incubation at 37 °C for 24 hr. Yellow colonies that appear identified by set of sugar & agglutination test (Vibrio). In children: growth of any bacteria on the appropriate media is considered as pathogenic in children. A sample is inoculated on tetrathionate broth, MacConkey agar, Mannitol salt agar, EMB as shown in this diagram: 33 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni Specimen from child incubated to Tetra thionate broth Macconkey agar Mannitol salt agar EMB agar S.S agar Pink colonies Yellow colonies S. aureus Green metallic sheen (E. coli) Coagulase Sensitivity to perform the identification Sensitivity test + biochemical test E. coli Salmonella & Shigella Serology & sensitivity test 34 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni G. Urinary tract infections : The urinary tract consists of the kidney, bladder& the urethra. The bacterial infection is usually acquired by the ascending route from the Urethra to the bladder& may proceed to the kidney. The diagnosis of urinary tract infection cannot be made without bacteriological examination of the urine because many patients with the frequency dysuria syndrome have sterile urine & conversely asymptomatic bacteriuria is common condition. A scending infections of the urinary tract are most commonly caused by G –ve rod such as E. coli & other members of the Enterobacteriaceae. Klebsiella, Enterobacter, Serration & P. aeruginosa are more frequently found in hospital acquired UTI, because their resistance to antibiotics & is the most frequent source of bacteriamia. All areas of the UT above the Urethra in a healthy human are sterile, but the epithelium of the Urethra usually colonized by some normal flora M.O such as coagulase, negative staphylococcus, not hemolytic streptococcus, lactobacillus and Diphtheroid; In addition some non pathogenic bacteria such as Neisseria, anaerobic bacteria& G –ve bacilli. Most urinary tract pathogen originate in the faecal flora, which have ability to colonize the periurethral areas because have particular type of pili, enable them to adhere to Urethral & bladder epithelium and some of them have capsular which associated with ability to cause pylonephritis. UTI is primarily of three types: Cystitis infection of the bladder Pyelorephritis Uritis infection of renal parenchyma infection of women more than men. 35 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni Laboratory work Specimens Mid stream urine specimen collection must be performed carefully for optimal results especially in females. In some time use urinary catheterization which allow collection of bladder urine with less Urethral contamination. The contamination of urine sample by normal perineal & anterior urethral flora is the most important consideration for collection of clinical samples, contamination with vaginal discharge may account with vaginal discharge may account for presence of albumin & pus. Container used for collection of urine samples, should be sterile & clean. Microscopic examination 1. A drop of fresh uncentrifuged urine placed on a slide, covered with a cover glass, and examined with light microscope can reveal leukocytes, epithelial cells & bacteria if can more than 105 ml are present. 2. Brief centrifugation of urine readily sediments pus cells, which many carry along bacteria & thus many help in microscopic diagnosis of infection. Culture The collected urine is cultured in measured amounts on solid media, such as blood agar plates& other solid media. Then identification of the M.O grows on these media. 36 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni H. Genital & Sexually transmitted pathogens (STDs) The number of M.O known to be STD & the laboratory approach to the diagnosis of genital infection is related to the sex of the patient, although some infections are common to both sexes. Ex: Gonorrhoea, Syphilis & Chlamydial infection but there are usually differences in the presenting symptoms & the sites & methods of specimens collection in these infections. General infection in women: Acute Vaginitis: Candida albicans Cervisitis with or without Urethritis: Clamydia trachomatis Uterine Sepsis: S. aureus Genital ulceration: T. palladium Tuberculosis of uterus: M. tuberculosis Laboratory works Specimens: Vaginal & urethral discharge is collected by swabs made of cotton that has been treated with charcoal to adsorb toxic material to gonococci, Mycoplasma & Chlamydia. For diagnosis of vaginitis or uterine sepsis the specimen is high vaginal swab (upper part of vagina). For gonorrhoea the vaginal discharge swab is unsuitable because gonococci tend to die in the acid vaginal secretion and if remaining viable are likely to be over grown by vaginal commensal bacteria so that endocervical swab must be collected. Urethral & pharyngeal swabs should be taken. Swabs for culture should be placed in tubes of Amines transport medium or modified Stuart’s media & transport to the lab. (Held at room temperature until inoculation). For examination of Trichomonas special specimens should be collected from the vagina, urethra, cervix, including a swab placed in clear Trichomonas transport medium or saline for microscopy &culture. 37 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni Since Chlamydia is intercellular pathogens, it is important to remove epithelial cells with swabs from the urethral mucosa. Microscopical examination: Both a wet film & gram stained film should be examined; the wet film is examined for the presence of motile Trichomonas vaginalis (rounded or pearshaped): 1. Examine under dark field microscope for T. pallidum 2. The gram stained film should be examined for Candidosis & bacterial vaginitis. 3. Candida = G +ve yeast forms & G +ve hyphae (Pseudomycelium) 4. Bacterial vaginitis = G –ve bacilli of diphtheroid morphology The diagnosis of bacterial vaginitis does not depend on the isolation of the organisms (G. vaginalis or M. hominis) but by: 1. The presence of homogenous vaginal discharge which adheres to the vaginal wall in a thin film that can vary from white to grey in color. 2. A fishy smell that can be detected by the addition of %10 KOH (NaOH) to fresh vaginal discharge (amine like odor). 3. Absence of G +ve bacilli (lactobacilli) & replacement with a mixed flora consisting G. vaginalis anaerobes such as Bacteroides. 4. The presence of clue cells, squamous epithelial cells covered with bacteria. 5. An increased vaginal PH ≥ 5 Culture: The specimen should be inoculated on two plates of a rich blood agar, one incubated 35-37°C in %5 CO2 with moisture & the other in anaerobic atmosphere with CO2. 1. Candida albicans can be recognized on the aerobic blood agar & grow well on Colombia agar base + %5 sheep blood + Naldixic acid (CAN) & Sabourauds agar. 2. N. gonorrhoeae grow well on rich blood agar & Thayer – Martin medium which contains the antibiotics. 38 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni 3. For Trichomonas vaginalis the Cysteine Peptone – Liver infusion Maltose (CPLM) medium is used under anaerobic condition. General infection in men: The infection in men are mostly caused by same organisms as in women, include: 1. Urethritis: Is classified as gonococcal or non gonococcal (NGU) depending on whether or not gonococci are found in gram film culture of discharge. 2. Prostatitis: Is usually caused by gonococci or Chlamydia. 3. Ulceration: Caused by T. pallidum. Collection of specimens & laboratory examination: Urethral discharge may be expressed directly on to the slide for gram stain & be inoculated immediately onto chocolate agar & selective medium for the culture of gonococci. If specimens have to be transported to the laboratory the exudates from ulcers should be collected on a swab & put into a tube of Amine’s transport medium. 39 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni Fourth\\ Serology analysis : Serology: is a science that attempts to detect signs of infection in patient’s serum such as antibodies (Abs) specific for a microbe. The basis of serological tests is that Abs specifically binds to Ag in vitro. The unknown Abs can detect when known Ag is added to serum & the reverse is true. The serological tests used the principle of : A. Precipitation: It involves the interaction of solute Ag (precipitinogen) with Ab (precipitin) in correct proportions resulting invisible precipitate. The Ags are solutions of molecules which are protein or carbohydrate in nature. T he reaction is carried out in semisolid media like agar gels through which soluble molecules can diffuse & give precipitation line, this reaction is called Immunodiffusion test. B. Agglutination: It involves the interaction of suspended particulate Ag (agglutinogen) with their specific Ab so agglutination or clumping of the particles is seen. There are many types of agglutination: 1. Active Agglutination or bacterial agglutination Is used to diagnosis some bacterial diseases like Widal test & Weil Felix test. 2. Hemagglutination The Ags are parts of cell membrane surface of RBCs & when mixed with their Abs caused clumping of the RBCs, like ABO system of blood types. 3. Hemagglutination inhibition The virus reacts naturally with the RBCs & agglutinates them but when the Abs for the virus are present they attach to the virus & the RBCs remain free 40 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni so there is no agglutination (+ve result). This test is used for diagnosis of several viral diseases (measles, rubella …etc). 4. Passive agglutination The Ags adsorbed on the surface of a particle like RBCs latex & bentonite. In latex agglutination test the polystyrene latex particles coated with the Ags which are agglutinated with specific Abs like kits used for identifying yeasts (Candida) & bacteria (Staph, Strept & gonococci). 5. Passive Hemagglutination The Ags adherence readily on RBCs, (like polysaccharide) or require tannic acid treatment before adsorption of Ag (protein) on RBCs which used as carrier. C. Immunoelectrophoresis: The Ag are separated by electrophoresis on a gel & to identify the Ags bands, specific Abs placed in a trough & allowed to diffused toward the bands Ags & arcs is formed, this test is useful for the differentiation of Ags with in a mixture & used widely to detect disorders in the production of Abs(serum protein, albumin, globulin). 41 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni D. The complement fixation test: The complement fixation test detects Ab. 1. A test antiserum is titred in doubling dilutions & a fixed amount of Ag is added to each tube or will; if Ab is present in the test serum, immune complexes will form. 2. Complement is then added to the mixture. If complexes are present, they will fix complement& consumed it. 3. Indicator cells (red cells) together with a sub agglutination amount of antibody (erythrocytes cells) are added to the mixture. If there is any complement remaining, RBC cells will be lysed. If it was consumed by immune complexes in stage, there will be insufficient to lyse the red cells. Antigen Complement Test intisera No imm. Comp. Free Comp. Immune Comp. Indicator No cell lysis Indicator cell lysis 42 Fixed Complement. PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni Serological tests for autoimmune disease : A. Rheumatoid arthritis: Is a chronic inflammatory disease affecting primarily the joints & periarticular tissues. Patients with rheumatoid arthritis have abnormal proteins produced in the synovium of involved joints & circulate in their blood. These proteins known as rheumatoid factor (RF) which is: 1) A macroglobulin (Ab) with γ globulin activity, their properties are very similar to those of normal IgM class. 2) RF directed against the Fc protein of IgG. 3) The origin of RF is related to formation of damaged IgG in in infectious joint disease. 4) RF is anti-antibodies. Test for RF: Test is designed to detect RF in patient’s serum that reacts with normal human IgG bound to particulate carriers. Ex: - SRBCs = passive hem agglutination (Rose-Waaler test) - Latex = latex agglutination (most popular) - Bentonite particle = flocculation test. 43 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni B. C - reactive proteins: A serum globulin reactive against the carbohydrate cell wall of pneumococci commonly occurs in the serum of patients with rheumatic fever & rheumatoid arthritis. This protein usually appears after 14-26 hours of disease beginning & may increase in concentration by as much as 1000 times its normal amount; thus it is a useful clinical indicator of disease state. CRP is an globulin, it has an (a.a) composition similar to that of Ig but differs from Ig in antigencity. The elevation of CRP in patient about 0.5 mg/100 ml indicates tissue damage, inflammation or both. Test: a) Precipitation test on slide or tube (serum + anti-CRP). b) Latex fixation test. 44 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni C. Systemic Lupus erythematous (SLE): Is an inflammatory disease of connective tissue occurring primarily in women & characterized by diverse clinical manifestation involving variant organs of body. The nucleus of PMNs or lymphocyte lyses first & then swells to as much as 3 or 4 times its normal size & then it is ingested by normal PMNs, the latter cell wit the lysed nucleus as an inclusion body is an LE cell. Abs against LE cell called LE factor which is an antinuclear antibody that some times react like an Ab. LE factor (antinuclear factor) found in % 95 of SLE patient & directed against a large number of tissue components (LE cell). Test for SLE: a) Immunofluoresence test: An antigen (human leukocytes) can be used for determination of antinuclear factor. On microscope slide the test serum& fluorescent Ab (anti LE factor) are added to the Ag; this test called Fluorescent antinuclear antibody test (FANA) FANA: is the most sensitive screening test for the detection of Abs in the patients serum directed against various nuclear constituents. b) Other tests: Include latex nucleoprotein test & CF test. 45 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni Serological tests for infection disease : A. Febrile antibody tests Several diseases cause fever so these diseases known as the febrile diseases like Salmonellosis brucellosis, rickettsie & tularemia. Febrile Ags are endotoxin, enzymes or other toxic products, test used for diagnosis of these Ags known as febrile antibody testes such as: I) Widal test: Classic serologic test of Salmonella infection. O Ag & H Ag prepare from bacteria species used in this test to detect Abs in patients serum, this test is agglutination test (tube or slide) used widely for detection of Abs in Typhoid fever, titers greater than 1/160 (O Ag) or 1/80 (H Ag) indicate +ve result. Widal test becomes less useful because of the cross reacting Abs or previous immunization against typhoid that may give +ve result with Brucella Ags. II) Wright agglutination test or Rose Bengal test: This test is used for diagnosis Brucella, a titer greater than 1/100 (+ve result), the test is helpful for diagnosis in about the 1 st week of the disease, whereas it usually takes from 4-6 weeks for the organisms to grow in culture. III) Tularemia: The agglutination test is widely used for diagnosis of tularemia which is caused by Francisella (pasteurella) tulareusis, the organisms is highly infected & difficult to isolate. IV) Weil – Felix test: Agglutination test for Rickettsial disease (typhus fever) which is based on the fact that certain strains of Proteus vulgaris OX-2, OX-19, and OX-K (non motile strains) share Ags with Rickettsia spp. So that the Abs against Rickettsia present in patient serum cause aggl with Ags for Rickettsia spp. 46 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni B. Cold agglutination test: Are Abs react with human RBCs at (1-10)°C& the agglutination disappear or dissolve at 25°C or higher; these Abs agglutinate all human RBCs regardless of blood group& these Abs are found in the serum of patients with primary atypical Pneumonia after (8-10) days of the disease. Patient with diseases caused by Adeno virus & mycoplasma Pneumonia have cold agglutinin; Mycoplasma develop agglutinins for human RBCs type O. C. Streptococcus MG agglutination test Patients with primary atypical Pneumonia develop in addition to cold agglutinins, agglutinins that react with non hemolytic strains of Streptococcus known as Streptococcus MG. These Abs are specific reacting with capsular polysaccharide of the organisms, a titer of 1/40 is considered to be infection. D. Antistreptolysin test (ASOT) Streptolysin o (SLo) is exoenzyme produce by St. pyogenes which is in reduced state cause lyses of RBCs & WBCs. It is an antigenic; eliciting the formation of Abs that effecting neutralizes its hemolytic action, these Abs appear in serum of patients with Streptococcal infection, therefore the measurement of serum antistreptolysin O (ASO) is an indicator of Streptococcal infection (rheumatic fever& glomerulonephritis). ASOT is based on the fact that ASO can be specifically fixed to streptolysin o in vitro, where it will neutralize its hemolytic activity. This test is reported in Todd units, which is the reciprocal of serum dilution that completely inhibit hemolysis of organism number of RBCs. 250 Todd units (IU) normal value for adult 330 (IU) for child 400 (IU) streptococcal infections Todd unit: denotes the reciprocal of the highest of test serum at which there continues to be neutralization of a standard preparation of the streptococcal enzyme streptolysin o. Lysis (-ve no Ab) 47 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni ASO (serum Ab) + SLo (Ag) Ag –Ab + RBCs No lysis (+ve Ab) Miscellaneous Serology : 1) Pertussis agglutination test : The detection of whooping cough can be made with suspensions of bacteria serotype 1,3 added to equal volumes of serum dilution after incubation for 18 hr in 37°C, test are read with magnifying glass. The titer is expressed as a highest dilution yielding complete agglutination. Complement fixation test is more sensitive for pertussis antibody testing. 2) Leptospiral agglutination test : Leptospirosis is a group of disease produced by a large number of antigenically distinct members of genus Leptospira. At least 80 serotypes & sub serotype have been identified, the disease agent can be detected by agglutination test & hem agglutination test (soluble Ag coupled to SRBCs + serum agglutination) 3) Lance field grouping : Thermo precipitation test for detection & differentiation the groups of hemolytic streptococci by precipitin reaction between solution of carbohydrate extracted from streptococcal cells & antisera prepared by immunizing rabbits with heat killed suspensions of streptococcal. Bacterial extract + serum Incubation precipitation ring At 37°C for 10 min 4) Pregnancy testing : A number of serological tests have been used in pregnancy testing, to detect human chorionic gonadotropin (HCG) when it appears in the urine during the first few weeks of pregnancy. Serological tests are done frequently in the laboratory to detect pregnancy in the early stages. Laboratory, tests for pregnancy are based on the fact that during 48 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni pregnancy, the placenta produces a hormone called chorionic gonadotropin this hormone rapidly disappears after delivery. Human chorionic gonadotropin (HCG) is also produced in other condition as in choriocarcinoma and in malignant teratomas of the ovaries and tests. In pregnancy, HCG is produced by the langhans cells of the developing placenta. It is a glycoprotein with a molecular weight of about 30000. Immunologic pregnancy tests depends on several factor: 1) The manufacturer's direction must be followed carefully. 2) Collected and delivered of specimen in the laboratory for testing. 3) Stored of antigens. 4) Stage of antigens. 5) Whether the pregnancy normal or abnormal. 6) Presence of interfering substances in the urine (including drugs, proteins, and red cells). 7) The sensitivity and specificity of the assay procedure and the use of quality control programs. Since detergents may interfere with results, the specimen should be collected in a disposable urine container if possible. If these are not available, the patients must be instructed to use a clean rinsed container that dose not contain traces of detergent or other substrates that might interfere with the test. For all HCG test an early morning urine sample is best. HCG is lost during storage, so the test should be does as soon as possible. The urine should be fresh and clear with specific gravity 1.010. The presence of hematuria or proteinuria may cause falsely positive results. Phenothiazine anal promethazine drugs may also cause falsely positive results. 49 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni The methods most commonly used now are based on the : I) Latex particle agglutination inhibition test This test consists of incubation of the patients urine with anti HCG, followed by the addition of latex particles coated with HCG, if HCG is present it neutralizes the Ab so that no agglutination is seen & if no HCG is present in the urine agglutination occurs between the anti HCG & HCG coated latex particles. The test gives reliable results about 42 days after the first missed period. II) Direct latex agglutination test The reaction between Ag (HCG in urine) & anti HCG adsorbed on latex particles, agglutination indicates presence of HCG (+ve). Syphilis serology Causative agent : Treponema palladium After syphilitic infection two types of Abs appears in the serum: a) Non treponemal Abs called reagin which reacts with lipid Ags. b) Treponemal Abs which react with T. palladium & closely related strains : 1. Ab reacts with protein component of a non pathogenic strain of T. palladium (Reiter’s strain). 2. Ab reacts directly pathogenic strain of T. palladium (Nichol’s strain). So that the serological tests for syphilis are of two types, those which detect reagin Abs against cardiolipin such as VDRL, & those which detect treponemal Abs include the FTA-Abs & TPI. Reagin tests for syphilis: 50 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni Infections with T. palladium cause tissue damage of the host, splitting of the lipoidal fraction which acting as hapten, combines with the protein fraction of the spirochaete & stimulates reagin production. Syphilitic regain has two components: a) Has large M.W bivalent termed reagin which takes part in flocculation test. b) Is relatively small M.W bivalent termed as coreagin & reacts in complement fixation test. Reactions which demonstrate the presence of these reagin & coreagin are known as standard test of syphilis (S.T.S) which includes these two types: 1. VDRL (Venereal Disease Research Laboratory) VDRL test can be used quantitatively & qualitatively for detecting reagin in serum & CSF. This test is replaced by rapid plasma reagin (RPR) test which include modified VDRL antigen (cardiolipin lecithin coated cholesterol with choline chloride & also contain charcoal particles) to allow for the testing of plasma without heating. Cardiolipin, lecithin coated cholesterol particles + reagin flocculation VDRL test can be used qantitively & qualitatively for detecting reagin in serum & CSF, this test is replaced by rapid plasma reagin (RPR) test which include modified VDRL antigen (cardiolipin lecithin coated cholesterol with choline chloride and also contain charcoal particles) to allow for the testing of plasma without heating. These Abs also produced by : Patients with other infections such as: leprosy, tuberculosis, measles, chicken pox, hepatitis & infectious mononucleosis. Non infectious conditions such as drug addictions & non disease such as advanced age, pregnancy, recent immunization & in autoimmune disease. When positive serological test for syphilis occurs in a patient without syphilis, it is called biological false positive (BFP) test. 51 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni 2. Wasser man test Is complement fixation test used in diagnosis of syphilis, it is required: a) Ag: cholestrolized alcoholic extract of ox-heart muscle which has slightly anti complementary activity but with high degree of sensitivity of sera. b) Human sera: some patients have inhibitors of complement therefore serum should be heated at 56°C for 30 min. c) Complements from guinea pig. d) Indicator system (Anti sheep hemolysin & sensitized SRBCs). For quantitative test serial dilution of serum are tested. The test consists of : Patient serum + Saline + Ag +Complement The control consists of : Serum control + Saline + Ag + Complement Then the indicator system is added & examine for hemolysis. Treponemal tests for syphilis : A. T. pallidium immobilization (TPI) test: The test is based on the fact that when the organisms incubated with syphilitic serum & guinea pig complement the organisms lose their motility (immobilized), examine under dark field microscope. B. The treponemal hemagglutination (TPHA) test: The Ag used is a suspension of formalized tanned SRBCs coated with Ag from Nichol’s strain of T. pallidium & the patient 's serum is absorbed with sorbent (an extract of a culture of Reiter treponemes) to remove the non specific Abs 52 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni (cross reactive Abs), then the sensitized SRBCs is added, the positive result is the agglutination of the sensitized SRBCs. MHA-TP micro hemagglutination test for Abs of T. pallidium (TPHA in micro titer plates) ELISA in infection disease (Enzyme linged immunosorbent assay) 1. Bacterial diseases - In the assay of antibodies against infection agents. - To measure the response to Salmonella ‘O’ antigen. - Application in Cholera serology differentiated ISA, ISG & ISm. - Serology of Brucella abortus serology of yersinia enterocolitica - Antibodies to Chlamydiae - Assay for Klebsiella - Assay for Legiounairea disease 2. Funcal diseases - Aspergillus antibody - Candida albicans antigens - Aplatoxin B 3. Viral disease - hepatitis - cyto megalo virus (CMV) (with newborn & in immuno suppressed patients) 4. Parasitic diseases - Plasmodium falciparum antigen - Trypanosomia - Helminthus 53 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni Materials needed: 1. Coating buffer (carbonate-bicarbonate, PH 9.6). 2. PBS Tween 3. Conjugates : a) Alkaline phosphatase labeled sheep anti human immunoglobulin b) Horse radish peroxidase labeled rabbit anti human IgG. 4. Substrates : For alkaline phosphatase conjugates:- Substrate solution is: - P-nitrophenyl phosphate (1mg/ml). - Tablets (5mg) are stored at -20°C in the dark until used. Immediately before use, one (5mg) tablet is dissolved in each 5ml of %10 diethanol amine buffer at room temperature. It must be used the same day. Reaction stopping solution -3M NaOH. Read in a spectrophotometer at 405 nm. For peroxidase conjugates: substrate solution arthophenylene diamine to be made up freshly immediately before use. Of phosphate citrate buffer PH 5 & add 40ml of %30 H2O2. This substrate is light sensitive & must be used at once. Reaction stopping solution 25M H2SO4. Read in spectrophotometer at 492nm. 54 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni Example The competition method of ELISA for assaying antigen: (1) Adsorb antibody to surface (2.a) (2.b) Add enzyme labelled antigen Add labelled antigen ''un know Ag'' (3.a) Add enzyme sub strate (3.b) The reference wells containing only enzyme labeled antigen show coloration. The inhibition of that color change in the wells with test samples is preparation to the amount of antigen is the test samples. 55 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni Modification of the indirect ELISA for assay of antigen: Ag 1) Plate coated with antigen Ab 2) Test sample thought to contain antigen mixed together with reference antigen No antigen in test sample Antigen in test sample 3) Enzymes antiglobulin conjugate added Anti Ab Conjugate becomes fixed to immobilized antibody 4) Enzyme substrate add Substrate degradation indicate sample 2 contain no antigen No substrate degradation indicate test sample 2 contain no antigen 56 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni The difference in color change between a reference sample containing no antigen & the test solution in step 2 indicates the amount of antigen in the test samples. This is competitive assay light antigen concentration results in less color at the end of the test. Solid phase Anti Ab IgM ELISA serology capture : 1) Anti IgM adsorbed to plate Anti Ab Ab IgM 2) Test serum sample added Method A Method B Reference enzyme labelled viral antigen solution added 3) Reference viral antigen solution 4) Reference enzyme labelled virus specific antiserum added 5) Enzyme substrate added Amount hydrolysed 57 anti IgM antibody in sample PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni The color change is proportional to the amount of virus specific. IgM is the serum tested in step 2. Fifth\\ Semen Analysis : Semen analysis is an integral part of the workup of couples consulting for infertility. The availability of semen renders possible direct examination of male germ cells, giving precious data that are not accessible for female germ cells. Semen analysis includes the examination of: - Spermatozoa - Other cell present in semen. - Seminal fluid All together, these data indications on the testicular function & of the integrity of the male genital tract. Type of assay: 1. Descriptive assay Spermogram 2. Functiinal assay :a. Penetration of cervical mucous (postcoital test, in vitro penetration assay). b. Binding of sperm to the zona pellucida. c. Fusion of sperm with zona free hamster oocyte. d. Hypoasmotic swelling of the flagella. Macroscopic analysis : 1. PH: The normal PH of semen is alkaline & measured with PH paper. 2. Volume: The volume is related to the number of days since previous ejaculation & after 3 days of abstinence the range of volume 2-6 ml. 3. Appearance: include smell, color & viscosity. Microscopic analysis : 1. Sperm concentration. 2. sperm viability (vital staining) 58 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni 3. spermatozoa motility affect by many factors such as: a- age of specimen b- Temperature 4. Morphology analysis 5. Bacteriological analysis Sixth \\ Biochemical analysis : Sugar Determination of Glucose in patient blood may be performed on specimens taken from patients in a fasting state or on specimen taken 2 hours after the patient has eaten 100 gm of carbohydrate. The increased blood glucose concentration, result from an imbalance between hepatic output of glucose & peripheral outlay of the sugar. Consequently a hyper glycine is may result from : 1. A normal hepatic output of glucose with a low subversion rate of peripheral removal. 2. An increase in hepatic production & release of glucose with normal removal rate by the peripheral tissues. 3. A combine of these factors. 4. Abnormal functioning of hormone may influence glucose levels. After a period of fasting, the usual amount of glucose in the blood is between 60 & 100 mg/100 ml of blood. The blood glucose level usually increases rapidly after carbohydrates are ingested but returns to normal in 1.5-2 hours. The normal value are different in fast & normal cause which are : 1. Fast 60-110 mg/dl. 2. Random 60-140 mg/dl. (1 dl = 0.1 L is a common metric unit of volume equal to 0.1 liter or 100 cubic centimeters). There are many causes associated with presence of sugar in blood : 1. After large amount of sugar of blood containing sugar are eaten. 2. In cases of acute emotional stress where glucose liberated by liver for energy 59 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni 3. It may also be associated with pregnancy, certain type of meningitis, certain tumors of adrenal medulla & some brain injuries. The method used for glucose determination can be divided into 3 categories: 1. Oxidation methods which depend on the reducing ability of glucose. 2. Aromatic amine methods, which involve a reaction between the aldehyde group of glucose & the amine group of an aromatic amine. 3. Enzymatic methods which are based on the enzymes glucose, oxidase & hexokinase. But the occurrence of sugar in the urine indicates that diabetes mellitus should be suspected, and test for urinary sugar are commonly used for the diagnosis and management of this disease. The type of sugar that is present in the urine in cases of diabetes mellitus is glucose which is also called dextrose, any condition in which glucose is found in the urine is termed glycosuria or glucosuria. Also the glycosuria may caused from another reasons than diabetes mellitus which are :1. After large amount of sugar or food containing sugar are caten. 2. In cases of acute emotional stress where glucose is liberated by the liver for energy. 3. It may also be associated with pregnancy, certain type of meningitis, hypothyroidism, certain tumors of adrenal medulla and some brain injuries. Virtually all tests for urinary sugar may be classified as one of two types:1. Nonspecific test for sugars in general, which are based on the ability of glucose to act as a reducing substance. 2. Specific tests for glucose, which are based on the use of the enzyme glucose oxidase. 60 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni The tests that are based on the reducing ability of glucose are not specific for glucose. In these tests, the glucose is merely acting as a reducing agent, and any compound with a free aldehyde or ketone group will give the same reaction. All these substances and glucose have the ability to reduce a heavy metal from a higher to lower oxidation state. Usually copper II ions are reduced to copper I ions. Metabolism of Carbohydrates The polysaccharide (starch) degradation in mouth into maltose by the action of salivary amylase, a pancreatic amylase in the duodenum continues the hydrolysis or breakdown of starch and glycogen into maltose (disaccharide). Monosaccharide which obtained by degradation of disaccharide absorbed through the wall of small intestine into the blood, the major portion going into the portal circulation and to the liver. Insulin is responsible for maintaining a healthy level of glucose in the blood. Glucose can also be provided to the blood by the process called gluconeogenesis, the production of glucose from fat and protein, this takes place in the liver, where glucose is derived from certain amino acids (protein) and glycerol (from fat) by glucocorticoid hormones produced by the adrenal cortex decreased blood glucose and decreased glycogen storage in cell stimulate this process. After a period of fasting, the usual amount of glucose in the blood is between 60 and 100 mg/100 ml of blood, depending on the method of analysis, the blood glucose level usually increases rapidly after carbohydrates are ingested, but returns to normal in 1-2 hours. The blood glucose concentration above which glucose is excreted in the urine is called renal threshold. For most individual the renal threshold for glucose is 160-170 mg/100 ml. Several hormones have the affect of raising the blood glucose concentration. The actions of growth hormone and adrenocorticotropic hormone (ACTH), which are secreted by the anterior pituitary, are opposite (antagonistic) to that of insulin and tend to raise the blood glucose level. Hydrocortisone and other steroid produced by the adrenal cortex stimulate gluconeogenesis, the production of glucose from 61 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni fat and protein epinephrine, which is secreted by the adrenal medulla, stimulates glycogenolysis, the conversion of glycogen to glucose. Thyroxin which is secreted by the thyroid, also stimulates glycogenolysis and contributes to an increased blood glucose level, besides increasing the rate of absorption of glucose from the intestine. Liver Function: Normal liver function The liver responsible for many metabolic, storage, excretory and detoxifying function. More specifically, the liver is a major factor in the metabolism of carbohydrates, lipids and proteins, in both intermediary metabolism and the synthesis of many essential compounds. Many necessary enzymes and coenzymes for carbohydrate, lipid and protein metabolism are present only n cells of the liver. Glycogen is formed, stored and converted back to glucose in the liver. Energy derived from food is made available to the cells of the body through the process of glycolysis of the high – energy bonds in adenosine triphosphate (ATP), which are formed by oxidative phosphorglation in the cells of the liver. The liver is essential sin the formation and secretion of bile, bile pigments and bie salts, which are necessary for digestion. These substances are derived from bilirubin, a major by – product of the destruction of red blood cells. In addition, the liver is the site of formation and synthesis of many of the factors involved in the clotting of blood. These important functions of the liver may be altered when the liver is diseased or damaged. Numerous laboratory teats are available to determine both the existence of the liver disease and the extent, location and type of damage so that appropriate treatment can be initiated. There is not one test will give a complete clinical view of liver function. One test of liver function I for the presence and concentration of bilirubin in the blood and the urine. 1) Bilirubin metabolism Bilirubinis a normal product resulting from the breakdown of red blood cells. As part red blood cell degradation, the heme portion of hemoglobin molecule is converted to the bile pigment Bilirubin by the Reticulo Endothelial (Re) system, 62 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni primarily by RE cells in the liver, soleen and bone marrow. A total of approximately 6 gm of Hb is released each day as overage RBCs are eliminated from the body. The cells of the RE system first phagocylizes the RBCs, then convert the released Hb through a complex series of reactions in which the heme portion of the molecule is finally converted to a vivid yellow pigment (Bilirubin). An increase in the concentration of bilirubin in RE cells, bilirubin is not soluble in water. Therefore it is transport from the RE cells through the blood to the liver cells as a bilirubin – albumin complex. This water – insoluble form of bilirubin is often refferd to as free bilirubin or unconjugated bilirubin. When free bilirubin reaches the liver, it is converted to a water – soluble product by the kupffer cells of the liver. It is made soluble by conjugation with glucuronic acid and some other hydrophilic substances to form bilirubin glucuronide. Water – soluble Bilirubin, often referred to as conjugated bilirubin, can be eliminated from the body by way of the kidney or the intestine. Normally, conjugated bilirubin is excreted by the liver into the bile, transported to the common bile duct and then to gallbladder. Where it is concentrated and emptied into the small intestine. In which most of the bilirubin is convert to urobilinogen by the action of certain bacteria. Urobilinogen in the intestine is either eliminated from the body unchanged or oxidized to the coloured compound urobilin . Abnormal bilirubin metabolism (Jaundice) Jaundice is a condition that occurs when the serum bilirubin concentration becomes grater than normal and there is an abnormal accumulation of bilirubin in the body tissues. Since bilirubin is a vivid yellow pigment an accumulation in the tissues results in a yellow pigmentation of the skin, the sclera and the mucous membranes. The classification of the jaundices causes are: a) Prehphtic jaundice (hemolytic jaundice) It occurs in conditions in which there is increased destruction of RBCs this type of jaundice is found in infants with: 1) Blood group incompatibilities. 63 PATHOLOGICAL ANALYSIS 2) In neonatal physiological jaundice 3) Increased production of free bilirubin. Dr. Wafaa S. Al wazni There is an increased formation of conjugated bilirubin and a subsequent increased formation of uvobilinogen. So that the increased of uvoblinogen in stool and the excess goes to circulation and then excrete with urine. b) Hepatic Jundice Results from condition that involve, the liver cells directly and prevent normal excretion such a condition might be specific damage such as conjugation failure in neonatal physiological jaundice, where there is an enzyme deficiency. Disease of conjugation failure result in an increased concentration of unconjugated bilirubin in the blood. Diffuse or overall hepatic cell involvement occurs in such condition as viral hepatitis, toxic hepatitis caused by heavy metal or dray poisoning and cirrhosis. In these cases the ability of the lives cells to remove and conjugate free bilirubin is decreased resulting in increased amounts of free bilirubin in the blood. c) Post hepatic jaundice Is also referred to as obstructive jaundice. It occurs when the common bile duct is obstructed by stones, tamers, spasms or a stricture. As a result the bilirubin that has been conjugated by the liver is returned back into the liver sinusoids and the blood. Clinical significance of bilirubin An increased serum bilirubin concentration may indicate either:1. Increased destruction (hemolysis ) of RBCs. 2. Impaired excretory function of liver cells. 3. Obstruction of the bile flow. In obstruction jaundice there is an increased in total bilirubin, and in direct bilirubin, while in hemolytic jaundice there is an increase In total bilirubin and direct fraction because the increasing occur in free bilirubin with liver damage such as viral hepatitis, both the free and conjugated bilirubin increase and total direct and indirect fraction are elevated. 64 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni Elevations in serum bilirubin occur in many infant in the first few days of live. This is especially true of premature infants such neonatal physiological jaundice may involve either a deficiency of the enzyme that transfers glucuronate group onto bilirubin or liver immaturity. Bilirubin can not be conjugated and the concentration of free or indirect bilirubin is increased in blood. 2) Protein Although plasma protein alternations are not usually specific for a particular disease condition but any observation revealing an abnormality in the plasma protein indicate that some pathologic or physiologic condition & a particular significance in respect to the internal metabolism of the protein is the functional state of liver & kidney. The hypoproteinemia is most associated with a lack of proper diet or poor absorption of dietary constituent from the intestinal tract or loss of the protein result from burns, draining wounds & disease or liver disease & in some cause the decrease in total protein may be associated with pregnancy & lactation. The hyperproteinemia occurs with less frequency & is most associated with shock, dehydration & lympho sarcoma or plasma cytoma. The total serum or plasma proteins can be determined by 2 methods: 1. Refractometric methods 2. Biuret methods The normal value for protein is range from 6.2-8.2 G/dl. 3) Blood uric acid The determination of blood uric acid as a liver function test. The blood uric acid levels were elevated signification in hepatocellular Jaundice but were normal in obstructive & hemolytic Jaundice, because the site of conversion of uric acid to allantion by Uricase in the liver. Normal blood values for uric acid in the human are between 3-7 mg/dl & the increase above 7 mg/dl may be an indication of liver disease & may have liver damage. Then 65 to PATHOLOGICAL ANALYSIS Purins uric acid Dr. Wafaa S. Al wazni allantion: in liver 4) Serum Enzymes activity Alteration in serum enzyme activity due to malfunctioning of the liver occurs as a result of three processes: 1. Elevation of enzymes due to disruption of hepatic cells as a result of necrosis or altered membrane permeability. 2. A decrease in concentration in the serum resulting from impaired synthesis by the liver. 3. Elevation in enzymes levels due to the lack of biliary excretion. The Gpt (Glutamic pyrunic transaminase) is present in large quantities in the liver & it is increased in serum when cellular degeneration or destruction occur in these organs; but the Got (Glutamic oxulacetic transaminase) it appears in extremely high concentration in muscles both skeletal & cardiac & the serum Got level may be increased with liver disease, therefore can not be considered to be specific test for liver damage but Gpt considered specific test for liver damage & diseases. The 2 enzymes present in small quantities in serum : a) The Got= 40 unit/ml b) The Gpt = 45 unit/ml As a consequence, normal tissue destruction & subsequent enzyme release which lose their principal function within the cell. The increases observed in serum reflection of cellular destruction or disease. 66 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni Kidney function: The kidneys are the chief organs of regulation of the internal environment of the body. This occurs by this works: 1. Limination of water introduced into the body in excess of the amount required for normal metabolic processes. 2. Elimination of inorganic element according to the needs of the body. 3. Elimination of non volatile end products of metabolic activity. 4. Elimination of certain foreign toxic substances. 5. Formation & excretion of substances such as hydrogen & ammonia. Analysis of urine (end product of kidney function) often reveals alteration typical of disease of that organ but in addition may provide information concerning alteration in other physiological processes in the body. Gross examination to urine: 1. Urine volume 2. Color 3. Specific gravity 4. Transparency Chemical examination: Although the urine contains a large number of organic substances, only a few of these are of clinical significance in urine analysis. 67 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni Analysis for chemical composition of urine routinely includes the following tests: 1. Reaction (PH): The normal hydrogen ion concentration of urine is dependent upon the type of diet. Man with vegetable diet has a tendency to produce alkaline urine; where as acid urine is normal in man with diet that has high protein content. The hydrogen ion concentration of urine can be readily determined by the use of litmus paper. 2. Protein: The detection of protein in the urine is always considered pathologic & any persistent protein urea should be investigated, because the normal urine does not contain detection protein & most of the protein that passes the glomerular filter is reabsorbed in the tubules, but when the glomerular capsule is damaged, protein molecules can pass through & end up in the urine. There is a correlation between the presence of casts in the urinary sediment & protein urea since casts are made of precipitated protein. The presence of casts with protein urea distinguished as an upper urinary tract (kidney) disorder. The presence of WBC & bacteria & protein in the urinary sedimentation, this distinguish the lower urinary tract without renal involve. A wide variety of methods for the detection of protein in the urine are available to the laboratory most of which dependent on available kit. One of the methods use strong acid such as that incorporated in Robert’s reagent which is consistent of: 1 part of concentrated uric acid 68 PATHOLOGICAL ANALYSIS Dr. Wafaa S. Al wazni Saturated solution of magnesium sulfate prepared by : - 770 gm magnesium sulfate - 1000 ml D.W The result represent while ring of the Junction after 2-3 minute. 3. Glucose: The occurrence of sugar in the urine indicate that diabetes mellitus (D.M) & the condition in which glucose is found in the urine is termed glucose urea, this occur as a result of fear, excitement & restraint. This appearance of glucose in urine is thought to be the result of hyper glycemia that occurs to an increased search of epinephrine which leads to a rapid mobilization of glucose & glucosuria occurs after heavy meal of carbohydrate. The normal value for protein in urine range from 1-2 G/d. A large number of methods are available for both qualitative & quantitative measure of glucose in the urine & all of them depending on available kit. 4. Blood urea: The levels of urea in the blood are affected not only by alterations in renal function, but maybe altered by certain physiological factors or diseases nor primarily of renal origin. Physiologically blood urea nitrogen level is increased with dietary increase in protein. Any factor that decreases glomerular filtration rate will increase blood urea nitrogen. The normal value of blood urea range from 20-45 mg /dl. 69