FEMALE FERTILITY AND NUTRITION AND OBESITY
advertisement

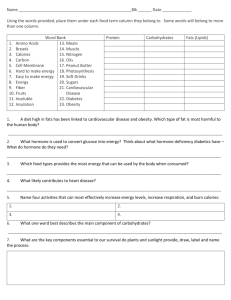
FEMALE FERTILITY, NUTRITION AND OBESITY Natalie Moska 10327381 Fertility rates are at their lowest level for the last hundred years and are continuing to fall, whilst at the same time obesity represents a rapidly growing threat to the population’s health. Many researchers have spent time investigating the links between the two and have found strong correlations between being overweight, and having a reduced ability to ovulate-and thus conceive and bear a child. What they are now trying to study is whether the lower overall fertility is actually caused by an overweight population. There is some speculation that fertility rates are declining due to other social reasons such as women pursing a tertiary education, studying longer and delaying the age of marriage and first birth, as well as breakdown of the nuclear family unit accompanied by increasing divorce rates and declining marriage rates. Biological factors such as a natural decline in women’s fecundity with advancing age, and as age at first birth increases, a woman’s chances of falling pregnant also decrease. Due to this delay in starting a family women often do not have enough reproductive years left to have as many children, so family numbers are remaining small. An aspect that is often overlooked are the lifestyle changes of the past 20 years or so. More women are working and have busy social and family lives and with such a hectic lifestyle, have less time to cook, so many people are eating high fat take away mealsespecially singles and couples without children. It is also interesting to note that this is having a detrimental affect on families themselves as more and more people are eating on the go and it was noted that only one in three families still use their kitchen or dining tables everyday for a sit down family meal! In the US alone “34% of women and 27.7% of men are classified as being obese” (ASSO 2005) and this is reflected by the enormous amount of fast food they consume. Australia is not far behind, being listed as the third fattest nation and this growing trend of obesity is causing a number of health problems with fertility being one of them is often a result of being overweight and having a diet of poor nutritional value. So does this increase in body weight and subsequent obesity experienced by one third of the population actually cause infertility, or is it the other associated problems which are having an impact on it? Why are falling fertility rates in Western countries important if the world population continues to grow and we always hear of the dangers of overpopulation and reaching the Earth’s carrying capacity? Governments are especially concerned as we are not replacing those that are dying and in the future this will cause an inverse population pyramid with the group greatest in number being those that are no longer working and are elderly. In Australia the current fertility rate of 1.75 children per one woman (ABS 2003) means that our population will go backwards and we may need to resort to higher immigration rates to boost our population levels. Even the treasurer Peter Costello said that we should “have 3 children, one for the mother, one for the father and one for the country”. This is because in order to keep the population level steady the birth rate needs to be slightly above 2.0, as not all children will make it to maturity to have their own offspring. This ensures that there are enough taxpayers to pay for the healthcare and pensions of the generation before. It has been established that fertility is important for maintaining a healthy population at a steady rate of growth. Seeing as the times at present are good and as a society in general we are prosperous with more money than we really need, we are we not having more children? One answer is that with money comes greed and materialism. Parents are looking at quality rather than quantity when it comes to planning their families. They would rather have 1 or 2 “quality” children which they can afford to send to private schools and pay for specialist lessons etc, rather than have 4 or 5 children and not have as much money to spend on “cultivating” them. This cultivation also includes feeding them high fat junk foods at an increasing rate, and when given in high doses can lead to pubertal problems, especially in girls. Also due to our materialistic society and the want for having a double income, women are educating themselves and instead of being married at 22 they are still usually at university. So not only are they delaying the age of first pregnancy, but also the number of subsequent children, in order to have the desired lifestyle. The female reproductive system is greatly influenced by environmental and nutritional factors, as well as emotional wellbeing. It has been statistically shown that in order for a human female to be able to reproduce efficiently she must not be too thin or too fat, ideally with a body mass index between 20 and 25 (Wang et al). This ensures that there is enough body fat (women require 17-21% of their body weight as fat) in order to menstruate but not so much as to cause fertility problems. “Significant associations are seen in reproductive endocrinology between excess body fat (particularly abdominal obesity) and irregular menstrual cycles, reduced spontaneous and induced fertility, increased risk of miscarriage and hormone sensitive carcinomas” (Kirschner et al 1982). This appears to be due to changes in the circulating sex hormones which are influenced by the amount of leptin produced which is a direct consequence of the amount of body fat a woman has. “Leptin is a main product of body fat and at the same time regulates the gonadotrophin surge which initiates the development of pubertal stages, which has shown that onset of menarche is earlier in obese women (Pasquali et al 2003). It was shown that obesity in childhood and in the early twenties increased the risk of menstrual and infertility problems, such as the most prevalent of all- Polycystic Ovary Syndrome (PCOS), where “the ovaries contain many small follicles that contain an egg but have not yet reached a mature size. Development of multiple cysts in ovaries is due to arrested follicle growth and is caused by an imbalance in the amount of LH and FSH released during the ovulatory cycle” (Serono, 2004) as well as affecting markers of insulin action. This hyperandrogenic disorder in caused by alterations involving “both androgens and estrogens and their carrier protein, sex hormone-binding globulin (SHBG)” (Pasquali et al 2003). Changes in SHBG concentration lead to an alteration of hormone delivery to target tissues such as the ovaries. Studies have shown that females with abdominal obesity have lower SHBG concentrations and this seems to be dependent on higher circulating insulin levels. “The role of adipose tissue is crucial in controlling the balance of sex hormone availability in the target non-fat tissues; adipose tissue is able to store various lipid soluble steroids, including androgens” (Pasquali et al 2003). Why is this important? Women with central obesity have increased rates of testosterone production, which as the main androgen, women should only have in small amounts or the feedback systems which work to regulate hormone production and distribution will go haywire. Therefore a condition of “relative functional hyperandrogenism” seems to be associated with the central obesity phenotype in women and “this excess in local ovarian androgen production induced by excess circulating insulin may also cause premature follicular atresia and anovulation” (Pasquali et al 2003). Obesity also causes an increase in estrogen production, however blood estrogen level usually remain normal as fat has the ability to store excess formed estrogen to keep it out of the circulation. It is thought that there is overproduction of estrogen to counterbalance tissue-specific androgenism. “PCOS is an endocrine and metabolic condition occurring in women of reproductive age…with over 50% of women with this condition being overweight” (Norman 2001). This suggests that being overweight has a causative effect on suffering from infertility, however more direct studies need to be undertaken to better establish this link. “During reproductive years, PCOS is associated with important reproductive morbidity, including infertility, abnormal bleeding, increased pregnancy loss and complications of pregnancy” (Lobo 2000). Some of the states of health associated with PCOS include: insulin resistance (with increased risk of developing type 2 diabetes later in life), hyperlipidemia, severe cardiovascular risk factors, hypertension, menstrual problems and lower incidences of spontaneous and stimulated ovulations and pregnancy rates (Lobo et al 1982, Norman 2001). Not only is insulin resistance dangerous to the liver function but “a large number of studies have shown that in the ovaries of PCOS women, excess insulin is capable of stimulating steroidogenesis and excess androgen production from the theca cell system. In addition by inhibiting SHBG synthesis by the liver proportionally to its blood levels, excess insulin may further increase the delivery of free androgens to target tissues (Poretsky et al 1999). Another factor influencing PCOS pathogenesis is leptin as it “is considered to be one of the main peripheral signals that affects food intake and energy balance, and obesity is a classic condition of excess circulating leptin” (Considine et al 1996) and obesity is thought to represent leptin resistance. “Recent in-vivo data indicate that leptin may exert a direct inhibitory effect on ovarian function, by inhibiting both granulosa and theca cell steroidogenesis (Spicer et al 1997). “There are now considerable data to show that lifestyle modification is the most important first step in the management of women who are overweight, anovulatory and have PCOS” (Norman 2001). This includes eating a healthier diet, losing weight through exercise and reducing intake of substances such as coffee and alcohol and quitting smoking which is also a contributing factor to infertility. “Lifestyle modification works by altering insulin sensitivity, body fat distribution, luteinizing hormone levels and reduction in circulating androgens” (Norman 2001) which causes a return to normal cyclic activity in most cases. If all these measures are taken but menses or normal hormone level do not return there are treatments available and the “use of insulinsensitizing agents such as metformin, troglitazone, pioglitazone and chiro-inositol may improve clinical outcomes in women with PCOS by lowering circulating insulin levels (Nestler et al 2000). However as “infertility is linked to obesity, we are going to see more of it” (McGovern 2004) and if nothing is done the current rate of 10% of PCOS affected women in the US could increase significantly, and perhaps even mirror the 30% obesity rate. Assisted Reproductive Technologies may also be used as a last resort if everything has failed, as ovulation can be induced and there are more options to becoming pregnant. Another question that needs to be asked is, what are the consequences of obesity induced infertility or subfertility? What are the costs to society? Firstly is the cost of having a reduced population and increased burden on society for the future, but obesity is a much greater burden on society. There are many serious diseases associated with it such as heart disease, greater risk of stroke, organ failure and death. Hospitalisation, operations, even disability pensions in extreme cases, as well as the cost of publicly funded ART are a burden on taxpayers and the government. It is in the interest of society to have healthy, fertile women who are able to bear children without draining the healthcare system. This is especially relevant when considering the high cost associated with ART and the low success rate. “IVF and ICSI represent the treatment of choice in the case of failure of pharmacologically induced ovulation (Dale et al 1991). “Obesity, particularlily the abdominal phenotype, appears adversely to affect the outcome of IVF or ICSI, impairing and reducing the pregnancy rate” (Crosignani 1994; Wass et al 1997). Granted it has been shown that body weight is heritable, so having parents that are obese could be a genetic factor. But given that children eat what their parents eat, is it really genetics, or just the dinner menu? Whatever the cause obesity is on the rise and is linked to the food that we eat. As Dr. Sinaikin says, heredity carves about 30 percent of our body shape. And it’s heredity that probably sticks us with a set point--the weight that we tend to maintain, through thick and thin and diet and exercise. “Compared with men, women bear an extra burden of body fat. On average we have about 8 percent more body fat than most men, which makes sense since we’re designed to carry reserves for childbearing, however there’s a relationship between fat and hormones. A woman needs to tote at least 16 percent body fat to produce estrogen, the hormone that’s essential for conception” (mothernature.com) There is a fine line between “carrying reserves” and carrying enough reserves for a small town! Being underweight also causes infertility as not enough fat will result in a drop in estrogen levels which will cause anovulation. “Smoking, alcohol consumption and a range of other lifestyle factors can all reduce a couple’s ability to conceive, usually affecting women more severely than men”(Butler 2004). As already stated this is because female’s hormone levels are strongly linked to body weight, whereas men’s sperm production is less affected by excess weight. The reason behind all of this is choice. It is a woman’s choice to delay pregnancy, it her hers and her partner’s choice how many children they have, if any at all, it is her choice to eat high fat, low nutritional value foods and it is a woman’s choice to indulge in an unhealthy lifestyle. There are many choices available to women today that were not possible 20 or 30 years ago- modern contraceptives, easy microwave dinners, better work arrangements, easier access to education and the ability to support themselves through working. A consequence of this is having less time for family and eating on the run which can lead to obesity which has been classified as an epidemic. Obesity then can result in infertility or subfertility which ultimately reduces the number of choices a woman can make. Female infertility and obesity as a result of poor nutrition needs to be addressed and resolved before it costs society even more. REFERENCES Australasian Society for the Study of Obesity 2005 Available at www.asso.org.au Butler, D. 2004. The Fertility Riddle Available at news@nature.com Insight into Infertility-Serono Symposia International 2004 Reproductive Health Booklet available from Concept Fertility Lobo, R.A. 2000. Importance of Diagnosing PCOS. Norman, R.J. 2001. Obesity, PCOS and anovulation-how are they interrelated? Obstetrics and Gynecology 2001, 13:323-327 Pasquali, R. et al 2003. Obesity and Reproductive Disorders in women Human Reproduction Update Vol 9, 4:359-372 Wang, J. X. 2002. Obesity increases the risk of spontaneous abortion during infertility treatment. Obstetrics and Gynaecology, University of Adelaide