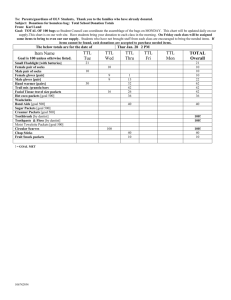
Report of the Mid-program evaluation of 'take the lead'
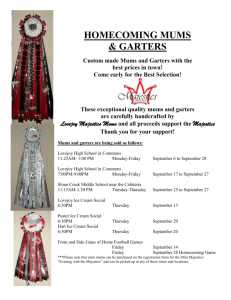
advertisement
Report of the Mid-program evaluation of ‘take the lead’ Centre for Clinical Governance Research Australian Institute of Health Innovation Report of the mid program evaluation of ‘take the lead’ Produced in 2011 by the Centre for Clinical Governance Research in Health, Australian Institute of Health Innovation, Faculty of Medicine, University of New South Wales, Sydney, NSW 2052. © Travaglia J, Debono D, Erez-Rein N, Milne J, Plumb J, Wiley J, Callaway A, Dunn A, Johnson J, Braithwaite J. 2011 This report is copyright. Apart from fair dealing for the purpose of private study, research, criticism or review, as permitted under the Copyright Act, 1968, no part of this publication may be reproduced by any process without the written permission of the copyright owners and the publisher. National Library of Australia Cataloguing-in-Publication data: Title: Report of the mid program evaluation of ‘take the lead’ 1. Report of the mid program evaluation of ‘take the lead’ 2. University of New South Wales, Centre for Clinical Governance Research in Health – Australian Institute of Health Innovation Centre for Clinical Governance Research Australian Institute of Health Innovation University of New South Wales, Sydney Australia http://www.med.unsw.edu.au/medweb.nsf/page/ClinGov_About i Report of the mid program evaluation of ‘take the lead’ TABLE OF CONTENTS Abbreviations and definitions ..................................................................................... 3 Executive summary ..................................................................................................... 5 Recommendations ...................................................................................................... 8 1. INTRODUCTION .................................................................................................. 10 2. Method .............................................................................................................. 15 2.1 Introduction ....................................................................................................... 15 2.2 Evaluation tools.................................................................................................. 16 2.3 Literature review ................................................................................................ 16 2.4 N/MUM interviews ............................................................................................ 16 2.5 N/MUM manager interviews ............................................................................. 17 2.6 Staff survey......................................................................................................... 17 2.7 Case studies........................................................................................................ 18 2.8 CSO survey ......................................................................................................... 18 2.9 Data analysis ...................................................................................................... 19 2.10 Approval ........................................................................................................... 19 3. Literature review ................................................................................................ 20 3.1 Introduction ....................................................................................................... 20 3.2 Special Commission of Inquiry into Acute Care Services in NSW Public Hospitals (‘The Garling Report’) ................................................................................................. 20 3.3 Caring Together: The health action plan for NSW ............................................. 21 3.4 Context for ‘ttl’ ................................................................................................... 23 3.5 The role of the Nursing/Midwifery Unit Manager within NSW Health ............. 24 3.6 The role of the CSO ............................................................................................ 24 3.7 Take the lead (‘ttl’) ............................................................................................. 25 3.8 Factors supporting and inhibiting workplace change ........................................ 26 4. Results ............................................................................................................... 27 4.1 Demographic and background data................................................................... 27 4.2 Implementation of changes post ‘ttl’................................................................. 29 1 Report of the mid program evaluation of ‘take the lead’ 4.3 Implementation of demonstrable changes in the capabilities and skills of N/MUMs post ‘ttl’ ...................................................................................................... 36 4.4 Key factors affecting changes implemented as a result of ‘ttl’ ......................... 46 4.5 Quantitative improvements at the unit level .................................................... 50 4.6 Barriers to the program’s implementation ........................................................ 57 4.7 Strategies required to ensure the sustainability of changes ............................. 58 4.8 Essentials of Care and Caring Together: The health action plan for NSW ......... 61 4.9 Conceptual Framework for the Nursing/Midwifery Unit Manager Role ........... 64 4.10 Strengthening of role as N/MUM .................................................................... 65 4.11 Introduction of the Clinical Service Officer’s position ..................................... 67 4.12 Impact of the CSO role on the clinical team .................................................... 71 4.13 Unexpected impacts/outcomes of the CSO role.............................................. 74 4.14 Case studies ...................................................................................................... 77 4.15 Reflections on ‘ttl’ ............................................................................................ 80 5. Discussion .......................................................................................................... 83 5.1 Overall findings .................................................................................................. 83 5.2 Positive benefits ................................................................................................. 84 5.3 Key factors .......................................................................................................... 85 6. Conclusion ......................................................................................................... 87 7. References ......................................................................................................... 88 8. Appendices ........................................................................................................ 95 8.1 Evaluation tools.................................................................................................. 95 8.2 Literature review .............................................................................................. 122 8.3 Demographic characteristics of participants ................................................... 132 8.4 Changes to N/MUMs’ capabilities and skills since ‘ttl’ .................................... 133 8.5 Improvements at the unit level since ‘ttl’ ........................................................ 142 8.6 CSO Survey ....................................................................................................... 153 8.7 Details of case study ........................................................................................ 167 2 Report of the mid program evaluation of ‘take the lead’ ABBREVIATIONS AND DEFINITIONS Abbreviations ACRONYM FULL TERM AHS Area Health Service AIHI Australian Institute of Health Innovation at University of NSW CCGR Centre for Clinical Governance Research at University of NSW CGU Clinical Governance Unit CI Clinical Indicator CEC Clinical Excellence Commission CPI Clinical Practice Improvement CSO Clinical Support Officer PHO Public Health Organisation SDM Service Delivery Model NMO Nursing and Midwifery Office (NSW Health) NUM Nursing Unit Manager MUM Midwifery Unit Manager N/MUM Nursing/Midwifery Unit Manager ‘ttl’ take the lead 3 Report of the mid program evaluation of ‘take the lead’ Definitions TERM DEFINITION Clinical Practice Improvement A combination of tools, techniques, skills and attributes designed to enhance care inputs, structures, cultures, processes, outputs or outcomes. Culture The configuration of attitudes, values, beliefs, meanings, behaviours and practices which together can be seen to be definitive of ‘what people are’ or ‘where people come from’. Culture can be seen as a ‘state’ or something people possess; it can be seen as performance; and also as a process. Ethnography A research technique used for describing and analysing what human beings do in selected settings, usually comprising ‘participantobservation’, fieldnotes, narrative accounts, temporal-spatial mapping, interviews, and other qualitative research methods. Evaluation The systematic examination of a policy, program or project aimed at assessing its merit, value, worth, relevance or contribution. Formative evaluation Evaluation conducted during the course of a policy’s, program’s or project’s life. Health services research The systematic examination of health care settings, institutions or organisations including quality, safety, structures, politics, cultures, financing, resource allocation and delivery systems . Innovation The rate, propensity, capacity and effectiveness in adopting new ideas, practices or behaviours. Organisational change Macro (organisational-wide), meso (divisional or departmental) or micro (small-scale) adaptations and adjustments to institutionalised processes, procedures, structures and strategies. Organisational culture The collective set of relationships in organisations that differentiate one group from another in terms of dress, attitudes, values, behaviours, beliefs, language and shared meaning. Summative evaluation Evaluation conducted at the end of a policy’s, program’s or project’s life. Triangulation A multi-method research or evaluation design which adduces converging or diverging evidence drawn from pluralist sources to illuminate an object of inquiry. 4 Report of the mid program evaluation of ‘take the lead’ EXECUTIVE SUMMARY This report presents the results of a mid-term evaluation of the ‘take the lead’ (‘ttl’) Nursing/Midwifery Unit Manager (N/MUM) program, conducted by the Centre for Clinical Governance Research (CCGR) in the Australian Institute of Health Innovation (AIHI), Faculty of Medicine, University of New South Wales (UNSW). The evaluation was commissioned by NSW Health, to assess the progress and achievements of the ‘ttl’ program. ‘ttl’ involved a series of strategies designed to develop, support and facilitate the role of N/MUMs The ultimate is that N/MUMs are able to provide highly co-ordinated care at the unit level, resulting in a well-managed unit and the improvement of the patients’ journey and their patients’ care experiences. The evaluation was conducted in the second half of 2010. A multi-method, triangulated research methodology was undertaken, involving seven inter-related studies and a literature review. Data were collected from participants across eight Area Health Services (AHS) and two state-wide services in New South Wales (NSW). Methods included: interviews with N/MUMs; interviews with managers of N/MUMs; two case studies; an online survey of staff; an online survey of Clinical Support Officers (CSOs); and document analysis. All of the participants in this evaluation recognised that the role of N/MUMs has changed significantly over the last three decades, and that this change has involved increased managerial and administrative responsibilities. Most N/MUMs and their managers commented on the lack of preparation for N/MUMs to pursue their managerial and leadership roles. The changes suggested or supported by the Garling Inquiry, including the formalisation of the role of N/MUMs, programs for their professional development, and the facilitation of their increased presence in their units and ‘away from their desks’ was seen to form a new phase in this development. We found that there was general agreement amongst all participating groups that ‘ttl’ had contributed to some degree to the skills development of N/MUMs. This was considered, by those who felt that ‘ttl’ had had an impact, to have enabled and empowered N/MUMs to implement changes in the workplace. It is important to note this distinction however: not all N/MUMs, N/MUM managers or staff considered that ‘ttl’ had had an impact on N/MUMs. Some participants were unable to identify whether it was ‘ttl’ specifically that had contributed to the N/MUM’s development or not. A range of confounding factors, including professional maturity, other development and change programs in the workplace, and the N/MUM’s own educational background and experience made it difficult to attribute the impact. 5 Report of the mid program evaluation of ‘take the lead’ Even though individual cases differ (both in response to the program and in assessing its subsequent impact), the results overall show that for those N/MUMs who were able to implement changes in the workplace, ‘ttl’ was an important contributing factor. This is particularly, but not only, in cases where N/MUMs had little prior training and or experience. N/MUMs have put in place a wide range of changes as a result of their participation in ‘ttl’. The most common changes involved implementation of some aspect of lean thinking: this may be because, in the view of one participant, that model allows for small incremental changes which are highly visible and ‘quick wins’. However, many N/MUMs have implemented other changes ranging from the modification of their individual communication styles, to new approaches to the rostering of staff, to the creation of multi-method team based approaches to the improved co-ordination of care. Differences in the sophistication and range of changes meant that their impact was difficult to measure; however individual participants indicated cost and time savings as a major impact. Changes in N/MUMs’ capabilities and skills varied. However, across all participants groups, there were indications of improved communication, particularly in critical contexts. Several N/MUM managers noted that one of the positive impacts on their own work of their N/MUMs participation in ‘ttl’ was a reduction in the number of performance reviews which ‘progress up’ the ladder for their attention. The success of, and barriers to, N/MUMs’ attempts at change were attributed to a range of structural, cultural, organisational and relational factors. These factors complemented the findings from the literature review. The three key elements to the successful transfer of learning into action were a combination of: the clinicians’ own personal commitments and characteristics; the way in which the training did or did not prepare them for the transfer of that learning; and workplace climate and organisational support. Participants gave consistent examples of the importance of these factors. The last of these factors, workplace climate and organisational support, was also said to be critical for the sustainability of the changes implemented. Although individual circumstances differ, overall, the role of the CSOs was said to have made a significant contribution to reducing the administrative workload of most N/MUMs. From the CSOs’ perspective, undertaking a new and at times not clearly defined role has posed some challenges, particularly for CSOs who are geographically or organisationally isolated, or whose work extends over more than one location. 6 Report of the mid program evaluation of ‘take the lead’ This evaluation shows that the introduction of ‘ttl’, along with other improvement mechanisms, such as the Essentials of Care program and the introduction of CSOs, has enabled some N/MUMs to develop, implement and sustain changes to their workplace. In cases where N/MUMs have been able to transfer their learning from ‘ttl’ effectively, these changes have resulted in improvements in finances, staff satisfaction and morale, and patient care. 7 Report of the mid program evaluation of ‘take the lead’ RECOMMENDATIONS Recommendation 1: ‘ttl’ should continue to be implemented On the whole, ‘ttl’ is perceived to have strengthened the role of the N/MUM, particularly new N/MUMs, and to have had positive impacts in many workplaces. However, it has been identified that there are some ways in which ‘ttl’ could be strengthened. As discussed networking and sharing of ideas was identified as very helpful. Therefore, implementation of ‘ttl’ should continue, particularly for new N/MUMs. Recommendations 1.1 – 1.8 are proposed to enhance ‘ttl’ and so maximise its potential impact. Recommendation 1.1 Future implementation of ‘ttl’ programs should cater for divergent levels of experience, geographical location, existing localised and state-wide systems requirements, and role demands of N/MUMs. Recommendation 1.2 Future implementation of ‘ttl’ should recognise and acknowledge prior learning. Alternative modules designed to build on prior knowledge should be included as an alternative for those N/MUMs with prior postgraduate management qualifications. Recommendation 1.3 A module on Change Management should be included to equip N/MUMs to lead and manage change in their units. Recommendation 1.4 Following ‘ttl’ an advanced program should be introduced to encourage further development of N/MUMs in their leadership role. Recommendation 1.5 A ‘ttl’ ‘refresher’ module would be helpful to consolidate what has been learnt during ‘ttl’ especially for less experienced N/MUMs. This would also provide an opportunity to share experiences of overcoming barriers to change. Recommendation 1.6 Methods should be established by which networking and sharing of experiences and ideas can be encouraged among N/MUMs. This may include regular debriefing sessions, email links, and group discussion boards. Recommendation 1.7 A mentorship program for N/MUMs who have undertaken ‘ttl’ should be introduced. Recommendation 1.8 An equivalent program to ‘ttl’ should be introduced for other managers. 8 Report of the mid program evaluation of ‘take the lead’ Recommendation 2 The CSO role should be developed and more CSOs employed The CSO role is perceived to have impacted positively on the work of N/MUMs largely through freeing them up from administrative duties to concentrate on their leadership role. However, shortcomings in the introduction of the CSO role have been identified. Recommendations 2.1 – 2.7 are proposed to address some of these issues. Recommendation 2.1 A clearer job description for the CSO should be developed. Input from N/MUMs and their managers should inform the development of the job description for CSOs. The CSO job description should be clearly defined while allowing room for local adaptation. Recommendation 2.2 A generic training and orientation program for CSOs should be introduced. CSOs should be required to undertake this program prior to commencing their role. Recommendation 2.3 N/MUMs should be involved in the recruitment process for the CSO role. Recommendation 2.4 A development session on the role of CSOs should be held so that N/MUMs are better informed about how to utilise the CSO role effectively. Recommendation 2.5 Methods should be established by which networking and sharing of experiences and ideas can be encouraged among CSOs. This may include regular debriefing sessions, email links, and group discussion boards. Recommendation 2.6 Ongoing evaluation of the introduction of the CSO role should be conducted. Input from CSOs, N/MUMs, managers, and other staff should inform further development of the role description, reporting lines and outcomes of the introduction of the CSO role. Recommendation 2.7 Further exploration of the role of CSOs in non acute services is warranted. 9 Report of the mid program evaluation of ‘take the lead’ 1. INTRODUCTION This report presents the results of a mid-term evaluation of the ‘take the lead’ (‘ttl’) – The Nursing/Midwifery Unit Manager (N/MUM) program, conducted by the Centre for Clinical Governance Research (CCGR), Australian Institute of Health Innovation (AIHI), Faculty of Medicine, University of New South Wales (UNSW). The evaluation was commissioned by NSW Health, to assess the progress and achievements of the ‘ttl’ program. ‘ttl’ involves a series of strategies designed to develop, support and facilitate the role of N/MUMs, so that they are able to provide highly co-ordinated care at the unit level, resulting in a well-managed unit and the improvement of the patients’ journey and patients’ care experiences. The project examined and reports on the outcomes of ‘ttl’ across ten Area or statewide Health Services including Sydney Children’s Hospital, Westmead and Justice Health. The Ambulance Service was excluded from the evaluation because no staff had participated in ‘ttl’. The evaluation used a comprehensive and sophisticated multi-method, triangulated research methodology. The evaluation investigated the identified outcomes of ‘ttl’ and in so doing answered the central questions: has the role of the Nursing/Midwifery Unit Manager been strengthened and are there identifiable improvements in patient care and flow? The framework for the evaluation took the form of eight inter-related studies (Figure 1). This report presents our findings. It begins with a brief history of ‘ttl’ within a wider context of health system reform in NSW subsequent to the Garling Inquiry (Garling, 2008). This is followed by a review of the literature on the role and development of nurse managers, reflecting in particular on the transfer of learning about, and for, change within health systems. The findings section presents the results of interviews and surveys gathered from N/MUMs, their managers, and clinical and administrative staff, relating to the impact of ‘ttl’ on the management of units and outcomes for patients across NSW. These results deal with various factors, including individual capacity development and structural support, which have contributed to, or hindered, the success and sustainability of changes N/MUMs wish to implement as a result of ‘ttl’. The report then considers how the introduction of the role of Clinical Services Officers (CSOs) has affected work of the N/MUMs and other staff of health services. 10 Report of the mid program evaluation of ‘take the lead’ Figure 1: Evaluation studies 1. Literature review 2. Changes put in place by N/MUMs as a result of participation in ’ttl’ 3. Demonstrable changes in the capabilities and skills of Nursing and Midwifery Unit Managers from the perspective of individual Nursing and Midwifery Unit Managers, the staff they manage, the staff to whom they report 8. Examine the impact of the introduction of the Clinical Services Officers’ position What is the progress made by, and achievements of, the ‘take the lead’ program? 4. Identify the key factor described by N/MUMs in any change they have been able to achieve 6. Identify barriers to the program’s implementation 5. Identify and measure quantitative improvements at the unit level to demonstrate change as a result of ‘take the lead’ 7. Identify strategies required to ensure sustainability of any changes achieved 11 Report of the mid program evaluation of ‘take the lead’ Each study had a core question and set of tasks. These are presented in Table 1. Table 1: Key research tasks, studies conducted and core questions asked relevant ‘ttl’ STUDY RESEARCH TASKS CONDUCTED 1. Review of the 1.1 Identification literature 2. Identify changes put in place by N/MUMs as a result of participation in ’ttl’ 3. Identify demonstrable changes in the capabilities and skills of N/MUMs 4. Identify the key factors described by N/MUMs in any change they have been able to achieve 5. Identify and measure quantitative improvements at the unit level to demonstrate change as a result of ‘ttl’ CORE QUESTIONS ASKED and the nurse What is known about the development of the role of nurse managers, and their ability to implement change? 2.1 Interview of N/MUMs 2.2 Interviews with managers of N/MUMS 2.3 Case studies of N/MUMs 2.4 Questionnaire survey of staff. What changes have N/MUMS been able to put in place as result of their participation in ‘ttl’ 3.1 Interviews with N/MUMs 3.2 Interviews with managers of N/MUMs 3.3 Case studies of N/MUMs 3.4 Questionnaire survey of staff. What changes have occurred in the capabilities and skills of N/MUMS from the perspective of individual N/MUMs the staff they manage, the staff to whom they report 4.1 Interviews with N/MUMs 4.2 Interviews with managers of N/MUMs 4.3 Case studies of N/MUMs 4.4 Questionnaire survey of staff. What key factors contribute to N/MUMs’ ability to implement successful changes supported by ‘ttl’? 5.1 Interviews with N/MUMs 5.2 Interviews with managers of What types of improvements in care have N/MUMs been able to achieve as a result of ‘ttl’. Including: decreased adverse event; improved staff satisfaction; implementation of lean methodologies; improved communication and management of difficult situations; improved patient satisfaction; reduced proportion of time spent on classification of literature on managers 1.2 Content analysis of the literature 1.3 Review of the key themes in the research literature. N/MUMs 5.3 Questionnaire survey staff 5.4 Case studies of N/MUMs. 12 of Report of the mid program evaluation of ‘take the lead’ STUDY RESEARCH TASKS CONDUCTED CORE QUESTIONS ASKED transactional administrative tasks; improvements in financial management; any other improvements in line with relevant recommendations in Caring Together 6. Identify barriers to the program’s implementation 7. Identify strategies required to ensure sustainability of any changes achieved 8. Examine the impact of the introduction of the CSOs position 6.1 Interviews with N/MUMs 6.2 Interviews with managers of N/MUMs 6.3 Case studies of N/MUMs 6.4 Questionnaire survey of staff. What factors acted as barriers to N/MUMs ability to implement successful changes in line with ‘ttl’? 7.1 Interviews with N/MUMs 7.2 Interviews with managers of What factors have and will contribute to N/MUMs ability to implement sustainable changes in line with ‘ttl’? N/MUMs 7.3 Case studies of N/MUMs 7.4 Questionnaire survey of staff. 8.1 Interviews with N/MUMs 8.2 Interviews with managers of N/MUMs 8.3 Case studies of N/MUMs 8.4 Questionnaire survey of staff 8.5 Questionnaire survey of CSOs 8.6 Document review of CSOs job descriptions. What differences are discernable in the way the CSOs position has been introduced across AHSs? What is their location within AHSs and units? What are their roles and lines of responsibility? What impact has the introduction of the CSOs had on the work of N/MUMs, other staff and on patients? In order to answer the evaluation questions, the findings from the studies have been structured in eight sections. Most of the data used in the studies comes from four larger studies. These were: a) interview survey of N/MUMs across eight AHSs, the Children’s Hospital Westmead and Justice Health; b) interview survey of managers of N/MUMs across eight AHSs, the Children’s Hospital Westmead and Justice Health; c) questionnaire survey of staff of the eight AHSs, the Children’s Hospital Westmead and Justice Health; and d) questionnaire survey of CSOs in the eight AHSs, the 13 Report of the mid program evaluation of ‘take the lead’ Children’s Hospital Westmead and Justice Health. In addition to the collection of these data, we conducted a literature review and analysis and a document review of CSOs’ job descriptions. The original proposal had not included the study of CSOs, but had included a content analysis and focus group analysis of patient complaints and incidents pre and post ‘ttl’. The study of CSOs was added in response to a request from the NMO. In discussion with NMO it was decided that that given the length of time it had taken some participants to undertake all five modules of ‘ttl’ (up to two years) that these latter tasks would not contribute any useful additional data. In the next section we describe our methodology in greater detail, followed by the literature review. Sections four to six outline the findings, a discussion of their implications, and then our conclusions. 14 Report of the mid program evaluation of ‘take the lead’ 2. METHOD 2.1 Introduction As outlined in the introduction, the mid-term evaluation of ‘ttl’ utilises a multimethod approach. This type of approach allows for triangulation of results, and therefore increased assurance of their validity. Triangulation is essentially a “… method of cross-checking data from multiple sources to search for regularities in the research data" (O'Donoghue et al., 2003: 78). Various types of triangulation are possible, including data triangulation (ie gathering different data sets), investigator triangulation (deploying more than one researcher), and methodology triangulation (across-method, that is qualitative and quantitative, or within-method, that is different forms of qualitative such as questionnaires and interviews) (Denzin, 1989). This evaluation uses all three types of triangulation. Data triangulation is achieved across location (AHSs, rural compared to metropolitan) and persons (individuals from various backgrounds and roles were interviewed). This allowed for data sets of different types to be analysed. Investigator triangulation was achieved through the use of a team approach to the research. The team included researchers with nursing, organisational psychology, medicine, social work, and health services management backgrounds. They came from academic disciplines including health services research, health policy research, organisational psychology, anthropology and sociology. Both across- and within-method triangulation was employed. Across-method triangulation was achieved through the quantitative analysis of Likert scale data on improvements achieved through ‘ttl’. Within-method triangulation was achieved through: thematic analysis of interview and survey results; thematic analysis of case studies; and document analysis of CSOs job descriptions. The evaluation also had some specific stipulations. In order to ensure that what was evaluated was the overall impact of ‘ttl’ and not the performance of individual N/MUMs certain parameters were set in regards to the selection of participants. These included: the random selection of N/MUMs for interviews; and ensuring that if an N/MUM was interviewed, then neither their direct managers nor their direct staff were interviewed or surveyed. Two limitations affected the second stipulation. First, in some instances (small hospitals, or hospitals with an N/MUM manager responsible for all N/MUMs) it was difficult to identify an N/MUMs’ manager who did not cover most or all of the N/MUMs who had participated in ‘ttl’. In the case of staff reporting 15 Report of the mid program evaluation of ‘take the lead’ directly to N/MUMs we surveyed all CSOs whose contact details were supplied by AHSs, so there is a possibility that some CSOs of N/MUMSs who were interviewed replied. However, as not all CSOs’ details were supplied, and as the focus of that research was primarily the CSOs themselves, it was felt that there would be minimal impact, and certainly no adverse consequences, from the design of the study. 2.2 Evaluation tools An inter-related set of tools was developed specifically for the ‘ttl’ evaluation (Appendix 8.1). The tools include: An interview schedule for N/MUMs An interview schedule for managers of N/MUMs A case study interview schedule A survey questionnaire for staff A survey questionnaire for CSOs. The tools were developed based on: the NSW Health Nursing and Midwifery Unit (NMU) briefing; meetings with the Director and staff of the NMU; the literature review; and the expertise of the researchers. Each tool was piloted, reviewed and modified as required. 2.3 Literature review The literature review was conducted using two methods. The first drew on existing literature relating to: the ‘ttl’ program; workplace and health service reform in Australia and New South Wales; changes in the role of N/MUMS in NSW; the impact of the introduction of new roles in the workplace; health systems’ capacity to absorb and respond to change; and transferability of training into the workplace. In addition to the review of this literature, a second targeted analysis was conducted of the international literature on the development of nurse-manager roles and strategies for developing this role. This literature was identified through a search of key databases including: Medline, EMBASE (general medicine) and CINAHL (nursing and allied health). 2.4 N/MUM interviews NSW Health provided a list of all participants of ‘ttl’ (n = 1610). It was decided that in order to assess the full impact of ‘ttl’ only participants who had attended all five 16 Report of the mid program evaluation of ‘take the lead’ modules; ‘Facilitating Critical Communication” (two days), “Lean Thing and Leadership” (two days), “Financial Management” (two days), “Rostering for Patient Care” (one day) and “Leadership – Making it Happen” (two days), would be included in the evaluation (n = 186). These individuals were then divided by their AHS and numbered. There were no participants from the Ambulance Service. Each N/MUM was randomly assigned using a random number generator (http://www.random.org/). They were then contacted in the order of their random assignment. Attempts were made to contact forty-nine N/MUMs. Eleven were on leave (long service, annual and maternity), four had changed jobs, four were un-contactable, and one was unable to participate due to workload. Subsequently, thirty telephone interviews were conducted with three N/MUMs from each Area Health Service. Phone interviews were held with each of the participating N/MUMs. Each interview lasted from three quarters to one and a half hours. Researchers took notes of the interviews, and these notes were later transcribed. Open ended responses were coded for key themes and concepts by two teams of independent researchers. Any disputes in interpretation were resolved by discussion. Likert-scale responses are reported using descriptive statistics. 2.5 N/MUM manager interviews Upon completion of the NUM selection, the random ranking of N/MUMs was further used to identify the managers of N/MUMs who had undertaken ‘ttl’ and had not participated in the N/MUM interview. These were contacted individually. As with the N/MUM interview, open ended responses were coded for key themes and concepts by two teams of independent researchers. Any disputes were resolved by discussion. Likert-scale responses are reported using descriptive statistics. A total of 30 interviews were conducted with N/MUM managers. 2.6 Staff survey Staff were contacted through the agreement of the managers of those N/MUMs who had completed ‘ttl’ but who had not been interviewed as part of this study. Attempts were made to contact ten staff from each AHS. A number of survey contact emails (n = 16) were returned as undeliverable. The remaining participants were then emailed and asked to complete an online survey. A follow-up reminder email was sent after three days. Of the contactable participants, a total of 23 participants (36%) completed the staff survey. Only one respondent indicated that they were sure that 17 Report of the mid program evaluation of ‘take the lead’ the changes made by their N/MUM were universally not attributable to ‘ttl’. A number indicated throughout their responses that they were not sure of the impact for one or more elements of the survey. These uncertainties are indicated in the text. 2.7 Case studies In addition to the N/MUM interviews two case studies were undertaken. Participants in the cases were interviewed in depth. In two cases the interviews were recorded and transcribed. The transcripts were coded for key themes and concepts by two independent researchers and differences resolved by discussion. The participants were contacted by researchers from the evaluation project and were informed that they had been chosen to participate in an in-depth interview of their experiences in regards to ‘ttl’. The participants were advised that the interviews would take between 1-1.5 hours. The main focus of the interviews was participants’ perceptions of the changes that occurred both in their own professional development and the unit practices, processes and culture as a result of ‘ttl’ and the introduction of the CSOs’ role. The interview questions were similar to the questions asked in the N/MUMs' interviews. In the questions directly regarding ‘ttl’ the researchers attempted to identify contextual details regarding the NUM and the unit pre and post ‘ttl’. NUMs were asked to relate how their perceptions of the program before attending and how or if their perceptions changed while attending or after attending the modules. Similar to the regular N/MUM interviews, the NUMs were asked to identify changes they had made and whether those changes were attributed to ‘ttl’ or other interventions. The NUMs were asked to identify barriers to successful implementation of changes as well as what enabled them to make sustainable changes. 2.8 CSO survey CSOs were contacted via email and invited to complete an online survey. A central contact list for all CSOs was not available. Access to CSO email addresses was requested by the Nursing and Midwifery Unit. A total of 207 contact names (of a possible estimated 500 CSOs) were supplied by the AHSs. Of these, 15 messages were returned undeliverable, two were away during the survey period, and one was not a CSO, making a final total of 189 CSOs contacted. Potential participants received one email asking them to participate, and follow up emails. A total of 92 responded, giving a 48% response rate. 18 Report of the mid program evaluation of ‘take the lead’ 2.9 Data analysis Descriptive statistics were used to examine the demographic items in interviews and surveys. Interview and case study responses and free text survey results were interrogated using content analysis, with two independent researchers reviewing the results for key themes independently, and then resolving differences through discussion. Comparisons of thematic results were made across groups (N/MUMs, managers of N/MUMs, staff and CSOs) in the same manner. Responses to several items were formulated using five (1 increased significantly to 5 decreased significantly or 1 improved significantly to worsened significantly) or six (1 increased significantly to 5 decreased significantly or 1 improved significantly to worsened significantly 6 don’t know) point Likert scales. In answering some different questions, including Likert scale responses, a number of respondents reported that while positive and negative changes had occurred, these, in their opinion were not directly attributable to their participation in ‘ttl’. Where an interviewee said that they did not or could not attribute their response to ‘ttl’, or where they were unsure whether it was attributable, or if they stated that the effect was attributable to another factor, this was marked as a zero response on the Likert scale. Only the remaining responses were included in the data set. Each set of Likert scale responses were validated by an additional question at the end of each set. Participants were asked if the changes were attributable to ‘ttl’. Where the response was no, the set of responses was removed. 2.10 Approval Ethics approval for the project was applied for, and granted by, the Human Ethics Research Committee of the University of New South Wales. The approval number was: HREC 10289 (PI)/Panel ref: 9-10-029. 19 Report of the mid program evaluation of ‘take the lead’ 3. LITERATURE REVIEW 3.1 Introduction This literature review provides a context for ‘ttl’ and the evaluation. We review the origins of Nursing and Midwifery Unit project, including the impact of the Garling Inquiry and the NSW Health Action Plan and the development of ‘ttl’ and related programs. We then consider how the role of N/MUMs has changed in NSW and why the role required clarification and formalisation. We conclude the review with a consideration of the factors affecting the implementation and success of changes, such as those intended by ‘ttl’, in health systems. 3.2 Special Commission of Inquiry into Acute Care Services in NSW Public Hospitals (‘The Garling Report’) In January 2008, a Special Commission of Inquiry into Acute Care Services NSW Public Hospitals was commenced by Commissioner Peter Garling SC. The Inquiry followed a coronial investigation into the death of a young patient in a public hospital in New South Wales and reported growing public concern about the safety and quality of care provided in public hospitals in New South Wales. The Inquiry was the most comprehensive review ever undertaken of the acute care services in New South Wales (Garling, 2008: 39). In the Commission’s final report (the Garling Report), publicly released on 27 November 2008, Garling recognised a paradoxical finding. Although application of the usual international criteria suggested the NSW public health care system was of a high standard, regular and alarming media reports of incidents in NSW public hospitals continued. The NSW public health system, he suggested, had entered a period of crisis and but for the goodwill and dedication of the public hospital system workforce, the reduction in quality of care would not only have been much greater but would have occurred sooner. Garling urged that patients be kept at the centre of care and noted that clinical staff were taken away from caring for their patients by an increasing burden of administrative tasks. The report’s 139 recommendations were directed at clinical leadership; interdisciplinary health care teams; medical workforce planning and management; clinical education; supervision, training and communication; information technology; use of evidence based protocols or models of care; quality and safety; use of collected health information; and equipment and infrastructure (Garling, 2008). 20 Report of the mid program evaluation of ‘take the lead’ Findings of the Special Commission of Inquiry recognised the pivotal role of the N/MUM in the provision of highly co-ordinated and safe care at a unit level. Specifically related to the role of the N/MUM, Garling made the following recommendations: “Recommendation 23 NSW Health should, as a matter of priority, review and redesign the role of the nurse unit manager (“NUM”) so as to enable the NUM to undertake clinical leadership in the supervision of patients and the enforcement of appropriate standards of safety and quality in treatment and care of patients in the unit or ward for which they are responsible. This redesign needs to encompass either the transfer of a range of duties from the NUM to other existing staff members or alternatively the creation of a role of clinical assistant to the NUM to undertake those tasks. The aim of the redesign is to ensure that at least 70% of the NUM’s time is applied to clinical duties and no more than 30% of the time is applied to administration, management and transactional duties.” (Garling, 2008: 39) “Recommendation 24 “All hospitals employing nurse unit managers report within 6 months to the Chief Nurse of NSW Health how they will re-allocate the duties currently being undertaken by the NUM in line with my earlier recommendation and all hospitals employing NUMs should complete the implementation of the redesigned role within 2 years.” (Garling, 2008: 39) 3.3 Caring Together: The health action plan for NSW Caring Together: The health action plan for NSW (the Action Plan) documented the New South Wales Government’s response to the recommendations in the Garling Report. Informed by the results of an extensive consultation process that canvassed input from over 12,000 health workers and community members, the New South Wales Government indicated its acceptance of 134 of the 139 recommendations made by Commissioner Garling. Two of the recommendations were not accepted and decisions on the remaining three recommendations were held over, requiring further consultation. The recommendations that were accepted were to be implemented in three stages with some measures introduced immediately, aimed to 21 Report of the mid program evaluation of ‘take the lead’ improve not only clinical care, but the environment and way with which it is delivered (NSW Department of Health, 2009). The first of the three stage approach is the Action Plan, an immediate response that focuses on the patient and includes their carers, the clinicians, managers and support staff. This stage aims to demonstrate the New South Wales Government’s commitment to building a better health care system. At stage two (six months), a sustainability plan will require a progress report from the New South Wales Government and specified changes to build a stronger health care system. During the third stage (at 18 months), an intergenerational health care system, the New South Wales Government will report on further progress and describe their plan for changing thinking and culture to create a future sustainable health care system. Six major strategies though which the Stage One response will be delivered are outlined in the Action Plan. These strategies include: “1. Creating better experiences for patients 2. Safety 3. Education for future generations 4. New ways of caring 5. Strengthening local decision making 6. Monitoring our progress.” (NSW Department of Health, 2009: 6) In implementing these strategies, the action plan emphasised the clinical leadership role of the N/MUMs. Furthermore it recognised that critical role of the N/MUM in the provision of safe care and in the successful implementation of responses to a wide range of the recommendations of the Garling Report. The following are the New South Wales’ Government’s responses to Recommendations 23 and 24 of the Garling Report (those that pertain to the role of the N/MUM). “Recommendation 23 New South Wales Government Response: (Stage One Supported) NSW Health will review and redesign the role of the Nursing/Midwifery Unit Manager as part of the move to the new Nurse/Midwife in Charge. Patients and 22 Report of the mid program evaluation of ‘take the lead’ families will better recognise the Nurse/Midwife in Charge through a prominently displayed ward photo. Already NSW Health has surveyed over 750 nurses and midwives to identify their views about the key capabilities required for the role and started the Take the Lead program for these positions. A Conceptual Framework has already been developed to outline the purpose of the role, the personal capabilities that should be able to be demonstrated and the broad core functions that are the responsibility and accountability of the role. The Nurse/ Midwife in Charge will provide leadership to ensure safer patient care, the right skill mix of staff on the ward, improved hand hygiene and coordination of ward rounds.” (NSW Department of Health, 2009: 19) “Recommendation 24 a & b (a) New South Wales Government Response: (Stage One Supported) The Chief Nursing and Midwifery Officer will annually report progress on the reallocation of administrative duties currently undertaken by Nursing/Midwifery Unit Managers so that they can provide a stronger focus on clinical care.” (NSW Department of Health, 2009: 19) The New South Wales Government’s decisions to strengthen the clinical leadership role of the N/MUMs and to reduce their administrative load by employing clinical support officers was strongly supported by the New South Wales Nurses’ Association (NSW Nurses' Association, 2009). The ‘ttl’ was identified as a key strategy in supporting this initiative. 3.4 Context for ‘ttl’ By way of providing context to ‘ttl’ we summarise here a range of initiatives and background that we deal with more fully in Appendix 8.2. There are currently multiple improvement strategies and programs underway across NSW Health. These provide positively reinforcing loops for ‘ttl’ initiatives. They include the: Essentials of Care (EOC) program (NSW Health Nursing and Midwifery Office, 2008); Between the Flags program (Clinical Excellence Commission et al., 2010); and the key principles for clinical handover initiative (NSW Health, 2009). 23 Report of the mid program evaluation of ‘take the lead’ 3.5 The role of the Nursing/Midwifery Unit Manager within NSW Health N/MUMs must straddle technical, managerial and clinical demands in a complex and continuously changing environment. While aiming to provide compassionate care and clinical leadership they are simultaneously required to manage finances, administrative demands, performance manage and staff their unit often within the context of staff shortages, and increasingly complex patient needs. The role of the N/MUM within NSW Health is essentially one of leadership and management. This role has changed over time and is now defined in the NSW Public Health System Nurses’ and Midwives’ (State) Award as a ‘registered nurse in charge of a ward or unit or group of wards or units in a public hospital or health service or public health organisation’ (NSW Health, 2010b: 4). A brief summary of the evolutionary course of the N/MUM role in NSW is provided below as it provides a context for the implementation of ‘ttl’. Appendix 8.2 provides a summary of the literature on the role and professional development of the N/MUM. The Charge Sister role was based on clinical experience and expertise until 1986 when in NSW the N/MUM role was created to replace this role. The Clinical Nurse Specialist role was simultaneously introduced to take over the clinical leadership role that was surrendered by the N/MUM for a focus on managerial responsibilities (Duffield et al., 2001). A recognised difficulty for N/MUMs was the lack of formalised training in management skills and an absence of role models, particularly given the dominance of role model based learning in nursing (Duffield et al., 2001). Decentralisation and the introduction of primary nursing affected the role of nurse unit manager requiring new types of managerial skills (Duffield, 1991). Uncertainty over role definition and a perceived gap in management skills has been identified as problematic not only in Australia (Duffield et al., 1994) but internationally (e.g. New Zealand (McCallin et al., 2010), South Africa (Pillay, 2009) and the United Kingdom (Gould et al., 2001). 3.6 The role of the CSO Linked to changes to the N/MUM’s roles, and also emerging from the Garling Inquiry, was the introduction across NSW of the CSOs. Their role was envisaged to support clinical and managerial staff in acute hospital settings, N/MUMs, nurses, midwives, medical staff and allied health personnel. Although most often located at ward or unit level, CSOs are able to work across multiple wards and units, or a whole service. CSOs were not intended to replace existing administrative staff such as ward clerks and communication officers, but rather to complement them. As part 24 Report of the mid program evaluation of ‘take the lead’ of the Action Plan, funds for 500 full time equivalent (FTE) CSOs were allocated, most of whom have now been employed. The CSOs usually work under the direction of a N/MUM at unit or ward level. Their role is intended to provide a range of administrative and or transactional services, with the possibility of a degree of independent initiatives and actions. The introduction of CSOs and the implementation of ‘ttl’ had the joint policy objective of freeing up time for N/MUMs to become more involved in clinical co-ordination and spend less time on purely administrative tasks. 3.7 Take the lead (‘ttl’) ‘ttl’ is a series of strategies to enhance the capabilities and skills of N/MUMs across NSW. Its ultimate goal is that of improving patient care and flow. ‘ttl’ develops the skills required by N/MUMs to provide co-ordinated care at the unit level by identifying ‘… strategies to support N/MUMs in achieving this role, recognising the pivotal part the N/MUM has in coordinating patient care’ (Hawe, 2009: 4). Although the Garling Inquiry and the NSW Actin plan contributed to the impetus for ‘ttl’, the origins of the program pre-date both reports. The project began as a collaborative between the Nursing and Midwifery Office (NMO) and the Health Service Improvement Branch at NSW Health, and is funded by the NSW Government. It was initiated in 2007, ‘… in response to patient and carer feedback and anecdotal information about the N/MUMs’ experiences’ (Hawe, 2009: 4). Early stages of the project were presented to Commissioner Garling. As a result of the recommendations (specifically 23 and 24) made by Garling, ‘ttl’ moved from being a voluntary, to a required program, for N/MUMs. Between August 2007 and February 2008, the NMO used a multi-method strategy to examine the experiences and expectations of N/MUMs. Data were collected on the activities, barriers and enablers, required skills and attributes that were perceived by N/MUMS to constitute both the ideal N/MUM role, and observed behaviours of a successful N/MUM. As a result of that study, the NMO created three streams of work. These were to: clarify and define the purpose and core function of the N/MUM role in NSW; identify strategies to support and strengthen the N/MUM role through education and professional development; and propose strategies to reduce the number of administrative tasks undertaken by the N/MUM that are not aligned with the purpose and core function of the role (Hawe, 2009: 4). Other related activities 25 Report of the mid program evaluation of ‘take the lead’ included workshops for N/MUMs and Directors of Nursing to increase understanding of the work being conducted in relation to ‘ttl’ and other projects. The aims of ‘ttl’ are that: There is clarity and standardisation around the purpose and core functions of the N/MUM role N/MUMs have the appropriate capacity and capability in order to fulfil their role N/MUMs are enabled and facilitate highly co-ordinated patient care reflective of their role and patient and carer expectations (NSW Health, 2008). A Conceptual Framework for the N/MUM role has been developed as part of the ‘ttl’ project. This framework identifies the purpose and broad functions of a N/MUM as defined by the State Award as well as the personal capabilities and core broad functions of the N/MUM role (NSW Health, 2010a). 3.8 Factors supporting and inhibiting workplace change Fundamental to the evaluation of ‘ttl’ is an identification of changes to practice and outcomes resulting from ‘ttl’, as well as the enablers and barriers to such changes. It is therefore useful to understand how the spread of innovation in healthcare organisations is reported within the literature. A brief overview of the literature on the spread of innovation in healthcare organisations is provided in Appendix 8.2 with key points summarised below. A key managerial role in healthcare is a constant striving for change and improvement (Braithwaite et al., forthcoming). Change may occur at a system-wide, organisational, group/team, or individual level and is influenced by formal and informal hierarchies within the organisation. The distribution of innovation within health service organisations is complex and affected by the interaction of multiple components including: the innovation itself; the adopter; the readiness of the system; the process chosen for implementation; the external context; the type of communication and influence used to transfer the innovation; and the linkages (Greenhalgh et al., 2004). The existence or lack of a certain characteristic does not guarantee the adoption or rejection of an innovation. It is imperative that change agents remember that “the attributes are neither stable features of the innovation nor sure determinants of their adoption or assimilation. Rather, it is the interaction among the innovation, the intended adopter(s), and a particular context that determines the adoption rate.” (Greenhalgh et al., 2004: 598). 26 Report of the mid program evaluation of ‘take the lead’ 4. RESULTS 4.1 Demographic and background data 4.1.1 Demographic data Input from a wide variety of clinicians and staff members were sought. Appendix 8.3 provides demographic details. These include the gender of participants; their age; their work and employment patterns; their professions and occupations; their organisational roles; and the number of years they occupied their current position. The demographic questions were included on the basis of their relevance to the aim of the evaluation. 4.1.2 Background to N/MUMs’ participation in ‘ttl’ In order to establish the context for their participation in ‘ttl’ N/MUMs were asked a series of questions relating to their attendance in ‘ttl’. These included their reasons for participating, Table 2 below, and the perceived benefits of their involvement. Table 2: reasons for participating in ‘ttl’ REASONS FOR PARTICIPATING IN ‘ttl’ NUMBER OF RESPONSES Mandatory 16 Mandatory, but participated willingly 4 Own initiative 4 Strongly encouraged 3 Result of work appraisal or needs identified 2 Mandatory and did not want to go 1 N/MUMs were asked about their experience of participating in ‘ttl’. Of the 30 respondents, 18 (60%) indicated that their experiences were positive in some way, ten (33%) indicated that their experiences were variable (experiences varied with the module or the interactions), and two (7%) that their experiences were negative. Apart from content, N/MUMs specifically mentioned networking (n = 11), new ideas or reflecting on their existing knowledge in new ways (n = 4), discussions, problem solving or gaining advice from peers (n = 4) and reflection on their own roles (n = 2) as adding value to their participation. Two N/MUMs stated that participation in ‘ttl’ had empowered them, or given them the skills to empower their staff. An additional 27 Report of the mid program evaluation of ‘take the lead’ five N/MUMs mentioned support provided by the organisation as a positive factor in their experience of ‘ttl’. Both rural and metropolitan staff identified the opportunity to compare experiences across locations as being beneficial. “I really enjoyed meeting NUMs from other areas and hearing their experiences and gaining “tips” and advice on how to deal with certain issues.” [N/MUM, metropolitan hospital] Respondents who felt their experiences were variable noted that a number of the modules were more suited to less experienced N/MUMs. This was also the case with N/MUMs who indicated their experience of the program was negative one and who described the content as “childish”. A total of 12 N/MUMs nominated one or more specific modules as not meeting their needs. There appeared to be no difference in positive or variable attitudes for N/MUMs based on their: participation in Essentials of Care; years since graduation; years as a N/MUM; or number of staff reporting to them. N/MUMs who had positive attitudes towards ‘ttl’ were more likely to be positive about the experience, rather than negative or variable. N/MUM’s positive attitudes about their experience in ‘ttl’ did not appear to be affected by whether they worked in a rural/regional hospital, or a metropolitan institution. Negative factors included; content already known (n = 3); content ‘useless’ or inappropriate (eg rostering centralised so not under control of N/MUM) (n = 2); ‘one size fits all approach’ (n = 1); and difficulty of implementing what was learnt (n = 1). There were three common suggestions made in relation to N/MUMs’ experience of ‘ttl’. These were that some modification was required based on N/MUMs’ level of experience (n = 6); consideration was needed of the difference between rural and metropolitan N/MUMs’ resources and experience (n = 2); and the possibility of arranging the modules in different ways, for example as a one week session (n = 2). 28 Report of the mid program evaluation of ‘take the lead’ 4.2 Implementation of changes post ‘ttl’ 4.2.1 Changes made as a result of participation in ‘ttl’ N/MUMs were asked several times through the survey whether they had made changes due to their participation in ‘ttl’. Of the 30 N/MUMs interviewed, three people (10%) said they had not. One of these respondents went on to note although they had not made changes, they had used the skills they had gained in staff management and communication, including being able to successfully negotiate and introduce change, and get staff to take ownership of changes made. Table 3 outlines the types of changes participants said they had made. Table 3: changes implemented as a result of ‘ttl’ (from perspective of N/MUMs)* CHANGES Implemented principles of lean thinking RESPONSES EXAMPLES OF CHANGES Changes to shift handovers and data collection 20 Patient transportation streamlined Equipment packs streamlined Re-organisation equipment of resources and Better utilisation of storerooms Clean up of storerooms and general environment Removal of out dated forms Modification of office layout Only keep stock which is needed now Set up a new unit using ‘lean thinking’ principles Introduced auditing and survey Communication/critical thinking Development of business plan 7 Communication book with ideas for discussion Checklists for nursing staff in waiting area New and quicker methods of capturing patient information Niggle board established Changed communication style with staff and managers Emailing of educational material to 29 Report of the mid program evaluation of ‘take the lead’ CHANGES RESPONSES EXAMPLES OF CHANGES staff Rostering Method of distribution of roster 4 Computerised rostering Six months of rostering available in advance Set up a roster which took into account patterns of sick leave Leadership or management Developed a business plan 3 Encourage staff to take leadership roles Helped implement CSO role Budgeting 1 Staff made more aware of, and increased ownership in, budgeting processes No changes 3 ‘ttl’ aimed at a lower level No changes, but brought more of what I knew to the ward No specific changes but gained skills in staff management Communication module helped with introduction of change DON runs staff through budgets *More than one response possible per participant Although asked about specific changes they had made as a result of their participation in ‘ttl’ a number of participants spoke about outcomes of their attendance and outcomes of changes they had instigated, rather than the changes per se. Incidental or flow-on outcomes are listed in Table 4 below. Table 4: outcomes as a result of ‘ttl’ from perspective of N/MUMs* AREA TYPES OF OUTCOMES Workload easier Save time Efficiency More patient information captured Rostering improved Avoided what could have become an industrial issue through effective communication and negotiation Reduced manual and double handling 30 Report of the mid program evaluation of ‘take the lead’ AREA TYPES OF OUTCOMES Patient care improved Patient outcomes Improved patient flow Better outcomes for patients Patient care is the focus Able to successfully introduce and implement changes to unit Change management Gained ownership from staff of changes Able to implement change by getting stakeholders on board Better at negotiation with staff and managers Team approach to problem solving Passed onto staff knowledge and skills learnt Staff outcomes Staff take ownership of rostering Staff take a leadership role Staff take greater accountability for approaching N/MUM over issues of concern Staff aware that change is possible Better at giving and receiving feedback More aware of emotions, moods and body language Capabilities skills and Better at seeing bigger picture More politically aware Improvements in general communication style and skills Calmer in responses Increased understanding of, and confidence in, role as manager *More than one response possible per participant N/MUMs were asked if they had evaluated any of the changes they had made. Two participants said that they had not yet evaluated the changes, but were hoping to do so. One N/MUM indicated that her unit was measuring patient flow at the moment. The rest of the respondents described informal methods of evaluation: Environmental changes (ie visible elimination of clutter, more equipment) (n = 2) Increased staff involvement (ie staff more involved in projects leading to a decrease in budget, staff more aware of budget constraints) (n = 2) 31 Report of the mid program evaluation of ‘take the lead’ Staff feedback demonstrating increased satisfaction (n = 2) Staff proactive in requesting equipment or advising N/MUM of issues Decrease in the number of incidents between staff Decrease in amount of time taken to resolve issues New ward set up with lean thinking, and running efficiently from day one Consultation increased with both staff and patients and relatives. N/MUMs’ managers were also asked about the types of changes made by the N/MUMs under their supervision. The majority of N/MUM managers (90%) reported changes as a result of N/MUMs’ participation in ‘ttl’. As with the N/MUMs themselves, a range of changes were reported, some minor, others reflecting large scale changes to the organisation of the ward. Table 5 lists the changes made by N/MUMs as identified by their managers, and some examples of outcomes. Table 5: changes implemented as a result of ‘ttl’ (N/MUMs’ managers)* CHANGES Implemented principles of lean thinking RESPONSES 24 EXAMPLES CHANGES 18 EXAMPLES OF OUTCOMES Store room audits and redesign Application of principle to other context Reviewed and updated use of folders Introducing new organising system, ‘ttl’ helped prepare for changes More user friendly and easier to do the stores and easier for new staff to find things, plus it has saved the unit some money Streamlining of processes in ward Easier and safer access to equipment N/MUM had intended to make changes to unit, ‘ttl’ enabled her to do so Range of communication tools (e.g. whiteboard) Communication/critical thinking Improved exchange of information Group huddles instigated Improved solving Problem solving has Communication and critical thinking OF 32 problem Report of the mid program evaluation of ‘take the lead’ CHANGES RESPONSES EXAMPLES CHANGES OF EXAMPLES OF OUTCOMES become more solution based rather than problem based Rostering Finances budgeting Combination 5 and 7 5 N/MUMS collaborate in rostering process Staff involved self-rostering Improved planning for skill mix Improved budgeting Improved awareness Change was due to a combination of factors, but ‘ttl’ provided the tools to make it possible Falls reduction program resulted in fewer adverse events Introduced staggered meal breaks so that staff are on the floor at meal times 33 NMUM talks to staff and focuses them to think of patient needs and not personal rostering preferences: changing a shift need to swap with someone at own level NUM more proactive, thinking outside the square, and thinking what will be needed and rostering for it More financially aware Scrutinise FTEs and Financial Reports and offer comments Staff morale has improved and there are better patient outcomes. Staff are smiling and they’re happy Patient outcomes have improved – tracked (no. of falls; medication errors) There are complaints More positive attitude of N/MUMS N/MUM felt empowered to make changes ‘ttl’ cements changes that are already underway Skills development in less Report of the mid program evaluation of ‘take the lead’ CHANGES Values clarification RESPONSES 3 EXAMPLES CHANGES OF Were able to clarify unit values EXAMPLES OF OUTCOMES Used as focusing provision tool for service *More than one response possible per participant Although the majority of responses identified positive changes as a result of ‘ttl’, three N/MUM managers reported that there had been no changes implemented as a result of N/MUMs’ participation in ‘ttl’. However, while they could not identify specific changes, two of these managers identified that ‘ttl’ had ‘reinforced aspects of good management and leadership’ and participating N/MUMs had returned from ‘ttl’ with ‘renewed enthusiasm and motivation’. One N/MUM manager reported that ‘ttl’ had not catalysed changes because there was mentoring and professional skills development in place at their hospital pre ‘ttl’. Other N/MUM managers (n=4) noted that the impact of participation in ‘ttl’ varied, with some N/MUMs demonstrating changes while others did not. It was suggested that this may be explained in part by ‘individual attributes’ or that the effect may be delayed (‘it takes time *for some of the concepts+ to sink in’). Other N/MUM managers proposed that ‘ttl’ was particularly beneficial for “newer N/MUMs”: “For the newer NUM it has given her skills to fulfill the role, development and growth. The more experienced NUMs had the knowledge.” [N/MUM Manager, rural hospital] One N/MUM manager raised possible unintended consequences of attendance at the program. Their description highlights the contextual factors which affect N/MUMs’ ability to meet expectations, even with training: “On the other hand, one of my NUMs went to ‘ttl’ and will probably leave nursing because he has realised that it is very hard. At ‘ttl’ he met likeminded people and found that his situation is like other N/MUMs so asked himself why he is staying in nursing? As a result of ‘ttl’ he dissected the role. He realised that it won’t get any better and everyone is in the same boat – he is disillusioned. ... the nurse in charge – they need to be everything – it is the schizophrenic nature of the role – they need to be everything, asking them to manage (e.g. staffing, budget) but also to be out there with the patients and their families. The expectations are that they are a clinical coordinator, they do rounds for each of the specialists, they manage staff, beds, finances etc. 34 Report of the mid program evaluation of ‘take the lead’ We have big wards … They run with 76% occupancy. We have over [a dozen] VMOs who all want the NUM to do rounds with them between 7-9am.” [N/MUM, metropolitan hospital] Of the 22 staff who responded to the online survey, 11 participants (41%) identified changes their N/MUMs had made as result of their participation in ‘ttl’. These included: establishing or facilitating a weekly multidisciplinary round (n = 2); decluttering and reorganising the unit (n = 2); inviting input and comments on issues involving patient care and service delivery; a patient handover initiative; implementing self rostering; a teamwork and organisation initiative; developing a holistic approach to leadership and management; increasing staff morale and team leadership; and developing a more proactive approach to the management of staff issues. One staff member said that as a result of ‘ttl’ their N/MUM was “more innovative and confident [and] reviewed the use and ordering of ward stock, saving a significant amount of money”. 35 Report of the mid program evaluation of ‘take the lead’ 4.3 Implementation of demonstrable changes in the capabilities and skills of N/MUMs post ‘ttl’ The evaluation sought to measure N/MUMs’, their managers and staff’s perceptions about changes in their capabilities and skills. Two types of indicators were chosen: the first was a Likert scale measure and the second qualitative comments and reflections by participants. A full set of figures representing these responses is presented in Appendix 8.4. In this, and in subsequent sections, we need to remember that responses reported are only from participants who indicated that they could be attributed to ‘ttl’. All other responses were removed. To clarify, respondents may have felt that there was an impact from ‘ttl’ overall on their or their N/MUMs work, but may have felt that this impact differed according to the variable. 4.3.1 Changes in capabilities and skills as assessed by N/MUMs and N/MUM managers Participants were asked to rate the changes to N/MUMs’ job performance and capabilities post ‘ttl’ on several indicators. These were: overall job performance; communication; ability to handle complex situations; and management skills. Job performance Most N/MUMs felt that their job performance improved significantly, or somewhat (67%). A third of respondents (33%) felt that it had stayed the same, and no N/MUM felt that their performance had deteriorated. One N/MUM said ‘ttl’ had no impact on their job performance overall. There were 67% of N/MUMs’ managers who thought that ‘ttl’ had had a positive impact, and felt that there had been some improvement to N/MUMs’ job performance. There were 13% who believed that an improvement in N/MUMs’ job performance was due to ‘ttl’ in combination with other initiatives. The remaining 20% felt that the ‘ttl’ had no impact or that N/MUMs’ performance had remained the same. Managers were also asked to provide free text responses to changes in the N/MUMs’ job performance as a result of ‘ttl’. Respondents felt that as a result of ‘ttl’ several positive effects had occurred. This included N/MUMs’: confidence had improved; they were better able to make decisions; they were better able to provide effective 36 Report of the mid program evaluation of ‘take the lead’ feedback to staff; they could operate more effectively and efficiently; they had created a virtuous circle of ongoing learning and self-confidence; and they were less anxious about staff management. One manager described the change between N/MUMs who had attended a ‘ttl’ module (leadership) and those who had not: “Those who have done the leadership module have started to piece all the bits of ‘ttl’ together. Also it improved their morale and motivation and means they are now looking for opportunities for change…” [N/MUM manager, metropolitan community health service] Communication Participants rated changes to three aspects of their communication. This included their ability to communicate with their own staff; their ability to communicate with other staff; and their ability to communicate with patients and their families. None of the N/MUMs felt that their ability to communicate with their own staff or patients had reduced, although 4% felt that their ability to communicate with other staff had decreased somewhat. The majority (81%) of N/MUMs felt that their ability to communicate with their own staff, with other staff (63%) and patients and family (59%) had improved. The remainder felt that their ability to communicate with their own staff (19%), other staff (33%) and patients (41%) had stayed the same. For managers of N/MUMs, no participant felt that N/MUMs’ communication skills had worsened in any way. The greatest increase was in N/MUMs’ ability to communicate with staff: 80% of their managers felt there had been an improvement of some kind; 88% of those who identified an improvement reported that the improvements were due to ‘ttl’; 12% indicated that improvements were due to ‘ttl’ in combination with other co-occurring programs. With respect to N/MUMs’ ability to communicate with other staff, 43% identified an improvement due to ‘ttl’. Among these managers, 25% reported that improvement as significant and 75% indicating that it had improved somewhat. Of those who did not report a change, the majority attributed this to extraneous variables such as: ‘Growing problems with staff being managed off site. It creates new difficulties. Not ‘ttl’. [N/MUM Manager, metropolitan hospital] Fewer N/MUMs’ managers identified a change in N/MUMs’ ability to communicate with patients and their families (40%). All managers who reported a change in N/MUMs’ communication skills with patients and their relatives indicated that the 37 Report of the mid program evaluation of ‘take the lead’ change was positive with 82% of these respondents attributing these positive changes to ‘ttl’. One manager of an N/MUM said that their N/MUMs were now: “more out on the floor, participating with staff and patient outcomes.” [N/MUM manager, regional hospital] Of those who reported no change, 90% identified that this was not attributable to ‘ttl’. Seven of these managers suggested that a lack of change was because ‘this is core business anyway’; we ‘do this every day anyway - daily contact with families’; ‘already good at it’. Ability to handle complex situations Three characteristics were measured in relation to N/MUM’s ability to manage complex situations. These included: management of difficult situations; negotiation; and problem solving. No N/MUMs felt that their abilities in any of these areas had deteriorated. Of the participants interviewed, four felt that their participation in ‘ttl’ had had no impact on their ability to manage difficult situations. No-one felt that it had had no effect on their negotiation or problem solving skills. Of the majority of participants who felt that ‘ttl’ had had an impact, 80% felt their ability to manage difficult situations and negotiation skills (71%) had improved. In relation to problem solving skills slightly more (58%) felt their problem solving skills had improved and 42% felt that these had remained the same. Of the N/MUM managers 65% felt that their N/MUM’s ability to manage difficult situations had improved since ‘ttl’, with 55% attributing the improvement solely to ‘ttl’, 10% reporting that the improvement was due to a combination of ‘ttl’ and other factors and 3.5% attributing a change to factors other than ‘ttl’. There were 31.5% of managers who reported no change; 28% identified that the lack of change in the N/MUMs’ ability to manage difficult situations was due to external factors not ‘ttl’. There were 62% of N/MUM managers who felt that their N/MUMs’ negotiation skills had improved since ‘ttl’: 55% attributed this improvement to ‘ttl’; 3% to ‘ttl’ and other factors; and 3% to factors other than ‘ttl’. An improvement in N/MUMs’ problem solving skills since ‘ttl’ was reported by 63% of N/MUM managers; 52% attributed the improvement solely to ‘ttl’; 7% partly to ‘ttl’; and 4% due to factors other than ’ttl’. In the case of the last two categories 38% and 36% of managers reported that their N/MUM’s ability had stayed the same. A lack of change in ability to problem solve (28%) and negotiate (31%) was predominantly attributed to factors other than ‘ttl’. 38 Report of the mid program evaluation of ‘take the lead’ Almost equal numbers of staff felt that their manager’s ability deal with difficult situations had improved (45%) or stayed the same (46%). The remainder were unsure. Management Participants were asked to gauge changes to several aspects of their management skills. These included their ability to manage staff, their ability to lead, and their ability to manage resources (including staff, through rostering, as well as finances and resources, and their ability to apply lean thinking). Most N/MUMs indicated that there had been changes in their ability to manage staff. A total of 82% of participants felt that their ability to manage staff had improved. The remaining participants felt that their ability had remained the same. No participant felt that their ability had been impaired. A slightly lower number of managers (75.5%) thought that their N/MUM’s ability to manage staff had improved; 65% due to ‘ttl’; 7% due in part to ‘ttl’; and 3.5% not due to ‘ttl’. The remainder, 24.5%, believed that their ability had remained the same. A similar pattern was demonstrated when N/MUMs were asked to rate changes in their leadership abilities. A total of 77% indicated that they felt that their leadership abilities had increased to some degree. The rest (23%) indicated that they felt these abilities had remained the same. The majority of N/MUMs’ managers skills (80%) also indicated that their N/MUMs’ leadership had improved; 74% due to ‘ttl’; 3% due to a combination of ‘ttl’ and other initiatives; and 3% due to factors other than ‘ttl’. The rest felt that their skills had remained the same. Of the three remaining indicators of N/MUM’s management skills, their ability to apply lean thinking showed the greatest increase, with 86% of participants indicating that their ability in this aspect had improved either somewhat or significantly, and 14% saying it had stayed in the same. In relation to their ability to manage finances and resources, had 50% of respondents said that their abilities had increased, and 38% felt their rostering ability had improved. In these last two indicators 50% and 62% felt that their ability had stayed the same. No-one felt their abilities had become poorer. Rostering and finances were the modules which were most commonly criticised by N/MUMs. In the case of rostering this was because it either did not meet N/MUMs needs, or because they had a centralised rostering system and therefore it was not applicable. Similar criticisms were made of the finance module. 39 Report of the mid program evaluation of ‘take the lead’ As with the N/MUMs themselves, most managers of N/MUMs attributed the greatest impact of ‘ttl’ to lean thinking (83%). For N/MUM managers, this was followed by financial management (54%). Improvement in N/MUMs’ ability to roster staff was noted by (50%) of participating N/MUM managers. There were 32% of managers who identified that a lack of change in abilities to manage finances or rostering was due to factors other than ‘ttl’ such as central rostering and financial constraints beyond their control. None of the participants felt that the N/MUMs’ abilities had decreased in any way due to participation in ‘ttl’. Of the staff who responded to this question, 48% felt their manager’s ability to manage finances had remained the same, 14% felt it had improved somewhat, and the rest were unsure. 4.3.2 Descriptions of changes in capabilities and skills Examples of improvements to capabilities and skills As well as rating the changes to their skills and abilities, N/MUMs were asked to describe any specific skills they had developed. Of the 30 respondents, six said that they could not identify any specific or additional skills and capabilities which they had developed and four indicated that they had either refreshed previous capabilities or enhanced others. Overall, the skills and capabilities identified by N/MUMs fell into two distinct groups: communication and the role of the N/MUM. Table 6 highlights these improvements and provides indicative examples. Table 6: examples of improvements in capabilities and skills of N/MUMS* CAPABILITY OR SKILL Communication (n = 27) EXAMPLE Communication Negotiation Communication with medical teams/doctors More measured/tolerant responses Widened range of communication techniques/tools Effect of communication on others Feedback Handling difficult conversations with staff Improved conversations with families and patients 40 Report of the mid program evaluation of ‘take the lead’ CAPABILITY OR SKILL Role of N/MUM (n = 14) EXAMPLE Renewed sense of enthusiasm Increased confidence in abilities Improved leadership skills Assertiveness Managing difficult staff Empowering staff Improved organisational skills Research skills Financial management Increased computer literacy * More than one response possible per participant Impact on day to day work A number of participants identified the ways in which ‘ttl’ had impacted on the day to day work in their unit. Of the 30 respondents, 14 either could not articulate the day to day impact of their participation in ‘ttl’ as separate it from other improvement strategies and changes or did not respond to the question. For those who could, the examples of the impact included: better negotiation skills; improvements in time and other forms of management; better relationships with staff; improved organisation of ward; increased skills in prioritising; increased focus on patients; improved ability to sell change to staff; thing working better in unit in general; staff ownership of problems and empowerment; better temper and less stressed; and better communication with managers. Management of staff Several participants (n = 3) did not answer this open-ended interview question (as opposed to the Likert scale) about changes in their management of staff. Of the remaining participants, seven (26%) said that ‘ttl’ had had no or minimal impact on their management of staff. The remaining participants identified that their involvement had resulted in a number of improvements in the way they manage staff (Table 7). 41 Report of the mid program evaluation of ‘take the lead’ Table 7: improvements in staff management as a result of ‘ttl’* IMPROVEMENTS IN STAFF MANAGEMENT Improvements in reflective listening More insight into own behaviour Better communication skills Enhances staff ownership of and accountability to, unit Improved handover Improved management of difficult conversations Improved management of difficult staff Confidence with staff appraisals More inclusive of and less prescriptive with staff, decrease of barriers Increased assertiveness Improved understanding of staff needs, expectations and motivations Better time management * More than one response possible per participant Improvements to care of patients Half of the respondents, when asked if their participation in ‘ttl’ had changed the way they responded to the needs of patients, said that it had not. However, most of these responses were qualified by statements that the N/MUM had ‘always been patient focused anyway’. An additional three people did not answer the question. Of the remaining 11, examples of improvements to care of patients are outlined in Table 8. Table 8: improvements in response to needs of patients IMPROVEMENTS IN RESPONSES TO NEEDS OF PATIENTS See things from patients’ experience, and aim to make their experience more efficient and less traumatic Increased focus on patient care and outcomes Listens to, and tries to meet patients’ needs: requires a different type of nursing Spends more time with patients and discussing their problems, needs, complaints, home situation Better management means happier staff, and therefore better care to patients Improved communication increased staff satisfaction which in turn leads to better patient care 42 Report of the mid program evaluation of ‘take the lead’ IMPROVEMENTS IN RESPONSES TO NEEDS OF PATIENTS Improved budgeting means new equipment could be purchased Increased efficiency leading to better patient care Increased number of family conferences Increased patient compliments which are displayed for staff to see Gift register and sharing of gifts Complaints register Increased awareness amongst staff of opportunities for improvement More time spent by N/MUM in ward Changes in N/MUM’s work Many of the changes to the N/MUM’s work had been addressed in previous questions. Over half (n = 22) of the participants said either that ‘ttl’ had not changed their work, did not respond, or said that they had nothing to add. Of the participants who said ‘ttl’ had affected their work: six had more time to undertake clinical work or time on the wards through better prioritising and management; two had more time to spend with staff; and one felt that the N/MUMs’ Conceptual Framework allowed them to delineate their role more clearly. Changes to work of team Half of the respondents to this question indicated that ‘ttl’ had not resulted in changes to the work of their team, or they did not respond to the question. Table 9 summarises the impact ‘ttl’ has had on the teams of the remaining participants. Table 9: changes to the work of N/MUM’s team as a result of ‘ttl’* CHANGES TO WORK OF TEAM Increase staff participation in problem solving and decision making (n = 4) Improvements in staff morale (n = 3) Higher quality care for patients (n = 2) Improved team work (n = 2) Improved handover (n = 1) Increased delegation (n = 1) * More than one response possible per participant 43 Report of the mid program evaluation of ‘take the lead’ 4.3.3 Impact of ‘ttl’ on N/MUM’s role One of the elements considered in the evaluation of ‘ttl’ was its impact on the role of N/MUMs. It was perceived to be largely positive. Of the 30 participants, two said ‘ttl’ had not had an impact on their role and another two did not answer the question. Of the remaining participants, all indicated that ‘ttl’ had had some impact. The types of impact are presented in Table 10. In addition to the improvements outlined below, N/MUMs also raised several issues in relation to ‘ttl’. These included: networking being as important as the content of the modules; and the modules being too long. Table 10: impact of ‘ttl’ on the role of N/MUMs* IMPACT OF ‘ttl’ ON ROLE OF N/MUM Able to apply content of some or all of the modules (n = 9) Increased confidence in and or enthusiasm for role as N/MUM (n = 6) Networking (n = 5) Better understanding of role (n = 3) Improved coping mechanisms (n = 1) Improved status of N/MUM in view of staff (n = 1) * More than one response possible per participant Attitude towards being a N/MUM Participants were asked whether their participation in ‘ttl’ had affected the way they felt about being an N/MUM. A total of seven participants said no and an additional six did not answer. Participants said that they: felt more positive about the role (n = 3); clarified expectations of the role (n = 3); decreased feelings of isolation (n = 2); gained insight into the contributions they made; felt more empowered; increased their enthusiasm for the role; reinforced current activities; staff more appreciative of role; felt valued by NSW Health (n = 1 for all the latter). One participant indicated that they had left the course with a greater enthusiasm for the role of N/MUM, but that this had waned subsequently. 4.3.4 N/MUMs’ managers and staff perceptions of capabilities and skills development in N/MUMs Managers of N/MUMs were asked to reflect on the capabilities and skills which they had seen their N/MUMs gain as a result of their participation in ‘ttl’ in open ended questions. They identified the following improvements in their staff’s skills: 44 Report of the mid program evaluation of ‘take the lead’ Communication skills in dealing with staff and managers (n = 14) Improved understanding budgeting and rostering (n = 8) Embraced other initiatives and new ideas, increased lateral and or lean thinking (n = 11) Built team work and peer support amongst the N/MUMs (n = 3) Improved management and leadership skills (n = 14) Time management (n = 2) Improved performance management (n = 2) More outcome focused (n = 1) More staff focused (n = 1) Increased empathy (n = 1) Improved ability to support staff (n = 1) Increased professionalism (n = 1) Changed approach to data and improved knowledge base (n=4). Changes to N/MUMs’ ability to manage as identified by staff included: more collaborative; implemented a series of improvement initiatives; increased attendance at ward rounds; delineated and delegated more; improved communication between N/MUM and staff, and between staff; increased accountability. One respondent noted that as a result of the: ”… ward NUM spending more time with patients [there have been] fewer complaints.” [Medical staff, tertiary hospital] 45 Report of the mid program evaluation of ‘take the lead’ 4.4 Key factors affecting changes implemented as a result of ‘ttl’ Participants were asked about factors which affect the successful implementation of changes. Questions included: which changes N/MUMs had been able to implement successfully; whether some changes had been easier to implement than others; and what were the factors that enabled or formed barriers to change. 4.4.1 Successful implementation of changes Of the 30 N/MUMs interviewed three did not implement changes. Of the remaining 27, three participants indicated that assessing the success of the changes was difficult: one because the change was undertaken in a new hospital and therefore it was difficult to assess the change from what had occurred previously; the second participant found it difficult to differentiate between the impact of the changes they had made post ‘ttl’ and the impact of the Essentials of Care program; and the last participant found it difficult to assess the impact of change in a unit with high staff turnover. One additional participant felt that the success was “50:50” but noted that there were improvements both in her staff’s abilities and her own. Table 11 presents changes which have been successfully implemented by N/MUMs. Table 11: changes successfully implemented as a result of ‘ttl’* SUCCESSFUL CHANGES Improved feedback from and communication with staff, improved relationships with staff, increased staff satisfaction (n = 18) Increased confidence and skills as manager (n = 8) Staff in control, more responsible, empowered and proactive (n = 7) Improved processes (handover, transport, flow management, rostering, organisation of equipment)(n = 5) Increased effectiveness and or productivity of staff (n = 3) Cost saving in storeroom supplies by applying lean thinking (n = 2) Development of improvements/innovations by staff (n = 2) Time saved in service delivery (n = 2) Increased patient satisfaction (n = 1) Increased interest in patients (n = 1) * More than one response possible per participant 46 Report of the mid program evaluation of ‘take the lead’ The following statement paraphrases the response of one N/MUM to the question about the successful implementation of changes. In their opinion, “ttl”: “… allows you to be more transparent in your decisions. This leads to an increase in the trust that staff have of your decisions … I was already doing some of the things so this was more about developing my understanding of it, now I don’t just do what my role entails because I have been told to do it, I now understand why I do it. [It has] given me more opportunities to communicate with staff why I do things – this has developed relationships with my staff. My relationships with my staff have improved because I am now confident and understand why and I can build the staff understanding of why. Being able to say “I learnt this at ttl” gives it more credibility and credence and therefore my managers are more supportive. Lean thinking [has been] successfully implemented.” [N/MUM, state-wide service] As each interview progressed, participants often provided more details about changes which they had made as a result of their participation in ‘ttl’. These are not counted above, as they appear irregularly throughout various interview questions. They are, however, important examples of change. The following are spontaneous examples of change which were reported: “Process mapping, changing paper work for patient going into day surgery are examples [of changes]. We removed duplication and unnecessary tasks in Day Surgery Unit. Also, eliminated some things not needed for patients being admitted, streamlining, so patients came in later and went home earlier, reducing ward times. Better communication with families and carers regarding patient care after surgery. Improved communication if surgery is cancelled. Whole skills got developed which gave confidence other NUMS concur. [N/MUM, metropolitan service] 4.4.2 Factors affecting implementation of changes N/MUMs’ opinions varied as to whether some of the changes they had implemented were easier to change than others. Of the participants who responded (n = 23), factors said to increase the ease of implementation included: Increased confidence as a manager (n = 2) Patient centred approach (n = 2) Champions of change (n = 1) 47 Report of the mid program evaluation of ‘take the lead’ ‘Selling’ the change as a benefit to staff (n = 1) Establishing a new ward (n = 1) Team approach to change (n = 1). Factors making the implementation of changes more difficult included: Changing old habits/changing culture in others (n = 5) Lack of resources including staff (n = 2) Lack of development opportunities (n = 1) Difficulty in sustainability of change (n = 1) Need for follow up after courses such as ‘ttl’(n = 1) Lacking in leadership skills required (n = 1) Difficulty in seeing results of change for staff (n = 1) Time required to be inclusive (n = 1) Physical environment (n = 1). A number (n = 5) of participants identified lean thinking specifically as being an easier change to implement. The response of this participant provides important insight as to why this may be: “lean thinking changes [are] easier but still need to be driven. Easier because [they are] practical and [you can] chip away at it and do even without a CSO. Staff feel overwhelmed with workload [and] so [are] resistant to evaluation of other projects.’ [N/MUM, regional hospital] The managers of N/MUMs identified a wide range of factors which affected their N/MUMs’ ability to implement change. These included: Support from senior management (n = 11) Support from staff (n = 7) Team work (n = 3) Timing/time (n = 4) Culture of unit and organisation (n = 2) Staff resistance (n=1) Understaffing/ workload (n = 4) 48 Report of the mid program evaluation of ‘take the lead’ Impact of organisational structures (n = 1) Small scale, incremental changes (n = 1) Concurrence with Essentials of Care and or other change strategies (n = 1) Practice development workshop (n = 1) Support from CSO position (n = 2) Effective communication (n = 1) Showing relevance of change to staff (n = 1) Reduced sense of isolation (n = 1) Clinical champions of ‘ttl’ (n = 1) Sharing learning (n = 2) Willingness to change (n = 1) Passion (n = 1) Effectiveness of ‘ttl’ tools (n = 1) Skills to make changes (n = 1). The perspective of staff was closely aligned to that of the N/MUMs and managers. Factors which enable their N/MUMs to successful implement changes include: being positive about change themselves; implementing new practices over a period of time; introducing changes with increased confidence and collegiality, including team involvement, meetings and ongoing staff input (n = 2); strong support from the Executive and Senior Management; meeting a need; co-ordinated implementation strategy; and good leadership and communication skills (all the latter are n = 1). Factors which hindered successful implementation included: workload; the same project being undertaken by several departments simultaneously; lack of time; lack of ongoing organisational support; and change fatigue, because so many changes implemented at once. 49 Report of the mid program evaluation of ‘take the lead’ 4.5 Quantitative improvements at the unit level This section reports on quantitative improvements at the level of N/MUM’s units as a result of their participation in ‘ttl’. A full list of figures is presented in Appendix 8.4. 4.5.1 Unit performance N/MUMs were asked to rate the quantitative improvements in their workplace as a result of their participation in ‘ttl’. Indicators examined included: perceptions of their unit’s overall performance; perception of their unit’s overall efficiency; and rate of adverse events. Unit performance and efficiency Just over half of the N/MUMs (58%) indicated that both their unit’s performance had improved significantly or somewhat, and 42% that it had remained the same. In relation to their unit’s efficiency, 67% felt that it had improved to some degree. No N/MUMs believed that their unit’s performance or its efficiency had worsened by any measure. Of the N/MUMs’ managers, 62% reported that their unit’s performance had improved significantly or somewhat, and 52% reported that their unit’s efficiency had increased since the N/MUMs’ had participated in ‘ttl’. There were 14% and 7% who indicated that these improvements may be partly attributable to other initiatives. A total of 38% of N/MUMs’ managers felt that their N/MUMs’ units’ performance had stayed the same, and 41% that their efficiency had stayed the same. There were 31% and 38% respectively who attributed the lack of change in these variables to factors other than ‘ttl’. No manager felt that their N/MUM’s unit’s performance or its efficiency had worsened by any measure. Exactly half of the staff (50%) indicated that the unit’s performance had improved, and the rest through it had stayed the same. A slightly lower proportion (46%) believed that their unit’s efficiency had stayed the same, with 45% reporting that it had improved either somewhat or significantly. The remaining 9% felt that it had decreased somewhat. Adverse events The majority of N/MUMs (72%) indicated that the number of adverse events since their participation had largely stayed the same. No participants indicated that adverse events had increased. The remaining participants (28%) indicated that 50 Report of the mid program evaluation of ‘take the lead’ adverse events had either decreased somewhat, or decreased significantly, in concert with ‘ttl’. A similar response was received from managers of N/MUMs participating in ‘ttl’. Two participants indicated that they were not sure that a decrease in adverse events could be attributed entirely to ‘ttl’. Of those who attributed a change to ‘ttl’, 27% identified that adverse events had decreased somewhat. Overall, 77% of managers reported that there had been no change in adverse events since ‘ttl’, with 50% identifying that the lack of change was not attributable to ‘ttl’ (e.g. “we don’t get that many anyway”). Of the staff that responded 59% felt that adverse events had stayed the same or decreased somewhat, 23% that they had increased somewhat. The rest were unsure. Patient flow A slightly higher number of N/MUMs (48%) felt that patient flow had improved either significantly or somewhat, compared to those who felt it had stayed the same (42%). An additional 10% indicated that patient flow had worsened somewhat or significantly. Overall, 37% of N/MUM managers reported a change in patient flow since N/MUMs participated in ‘ttl’. There was 22% of participating N/MUM managers who attributed an effect on patient flow to their N/MUMs’ participation in ‘ttl’. Of these 27% reported a significant improvement and 59% a slight (somewhat) improvement. While 56% of N/MUM managers reported no change in patient flow, 48% reported that the lack of change was due to factors outside ‘ttl’. Of the staff who replied to this question, 32% reported that patient flow had improved to some degree, 50% that it had stayed the same, and the rest indicated it has worsened somewhat. Time spent on administrative tasks N/MUMs were asked a series of questions relating to their performance and capacity. The first question related to changes in the time spent on administrative tasks. No participant identified that the time spent on administrative tasks had either increased or decreased significantly. The remaining participants accounted that it had either: increased somewhat (25%), stayed the same (35%) or decreased somewhat (40%). In the perception of N/MUM’s managers, 29% reported that the time spent on administration by their N/MUMs had stayed the same. A further 51% suggested that the time their N/MUMs spent on administration had decreased to some degree, although most of these attributed the decrease to a combination of the potential 51 Report of the mid program evaluation of ‘take the lead’ effect of ‘ttl’ and the introduction of CSOs, a similar response was made by the N/MUMs themselves. The remaining 16% reported that it had increased somewhat but that this was due to factors other than ‘ttl’ (e.g. ‘[there are] a lot of projects rolling through increasing admin time’). Of the N/MUM’s staff that responded, 41% felt that the amount of time their N/MUMs spent on administrative tasks had decreased either somewhat or significantly. Of the rest, 27% felt it had stayed the same, 14% that it has increased somewhat and the rest did not know. 4.5.2 Staff performance The majority of N/MUM participants, 62%, thought that staff performance had improved, and 38% that it had stayed the same. No participant suggested that it had worsened. N/MUMs’ managers had similar perceptions, with 51% believing that staff performance had improved: 41% attributed this improvement to ‘ttl’; 3% to a possible combination of ‘ttl’ with other factors; and 7% was attributed to factors other than ‘ttl’. Most of the surveyed staff (50%) specified that staff performance had stayed the same, or that it had improved slightly (32%). The rest of the staff denoted that it had decreased somewhat (18%). N/MUMs were asked about impacts of their changes post ‘ttl’ on the behaviour of their staff. Positive indicators were staff satisfaction and staff retention, negative indicators were staff absenteeism. Amongst N/MUMs the greatest increase identified was in staff satisfaction, where 69% of participants reported that staff satisfaction had increased either significantly or somewhat since ‘ttl’. No participants advised that staff satisfaction had decreased. A total of 26% of participants also believed that staff retention had increased; with most participants (70%) indicating that staff retention had stayed the same, and a further 4% that it had decreased. Of the N/MUMs’ managers 49% thought that staff satisfaction had increased somewhat (23% attributed this improvement to ‘ttl’; 20% attributed changes to ‘ttl’ in part or were unsure of the cause; and 6% did not attribute this change to ‘ttl’). Of the remaining N/MUM managers, 40% thought that staff satisfaction had stayed the same and 6% that it had worsened significantly (participants noted that this was not due to ‘ttl’ but factors such as ‘workload issues’). Almost all (90%) of N/MUM managers thought that staff retention had stayed the same, with 7% stating that it had increased somewhat due to ‘ttl’. Of the N/MUMs’ staff, 41% felt that staff satisfaction had improved. Of the remaining respondents, 23% said that it had stayed the same, 27% indicated that it 52 Report of the mid program evaluation of ‘take the lead’ had worsened either significantly (4%) or somewhat, and the rest were unsure. Most (41%) reported that staff retention had stayed the same, or that it had improved slightly (14%). The remaining staff were either unsure, or held that it had worsened (36%). Staff absenteeism was largely considered by N/MUMs to have stayed the same (70%). Of the remaining participants, 17% felt it has increased somewhat, and 13% that it had decreased either somewhat or significantly. Of the N/MUMs’ managers interviewed, 83% proposed that absenteeism had stayed the same and 3% that it had decreased somewhat (due to ‘ttl’). There were 14% who indicated that absenteeism had increased but that this was not attributable to ‘ttl’. The majority of N/MUMs’ staff indicated that staff absenteeism had stayed the same (45%). Of the rest, 9% stated that it has improved somewhat, 23% that it had decreased somewhat or significantly, and the remainder unsure. As well as staff satisfaction and retention, N/MUM participants were asked about changes to staff morale. Half of the N/MUMs, 52%, felt that staff morale had improved. The remaining 48% thought that it had stayed the same. Amongst N/MUM managers, 60% felt that staff morale had improved. Of those N/MUM managers who attributed the improvement to ‘ttl’ (37%), 8% identified a significant improvement and 83% reporting the improvement as ‘somewhat’. There were 10% who reported that staff morale had worsened somewhat but that this was due factors other than ‘ttl’. Of staff who completed the survey, 32% perceived that staff morale had stayed the same, 26% that it had improved somewhat, 37% that it had decreased to some degree, and the rest were unsure. 4.5.3 Impact on patients Three measures of patient impact were taken. These included: patient satisfaction, patient complaints and patient compliments. A total of 44% of N/MUMs estimated that patient satisfaction had increased and 41% believed that patient compliments had increased. No participant felt that either of these measures had decreased significantly, although 4% recorded that patient satisfaction had decreased somewhat. Most N/MUMs felt that both these measures, satisfaction (52%) and compliments (59%), had stayed the same. A further 64% indicated that patient complaints had also stayed the same. Of the remaining participants, 31% stated that patient complaints had decreased either somewhat or significantly and 5% that they had increased somewhat. No participant indicated that patient complaints had increased significantly. 53 Report of the mid program evaluation of ‘take the lead’ Of N/MUM’s managers, 37% indicated that patient satisfaction had increased (24% due to ‘ttl’; 10% partly ‘ttl’; 3% not ‘ttl’), and 33% said that patient compliments had increased (20% due to ‘ttl’; 6% partly ‘ttl’; 7% not ‘ttl’). Managers differed from N/MUMs on which of these measures had remained the same (62% for satisfaction, 67% for compliments and 61% for complaints). The majority of the respondents who reported that these variables had remained the same, identified that factors other than ‘ttl’ were responsible; (38%, 43%, 37% respectively). A total of 27%, however, felt that patient complaints had decreased due to ‘ttl’. Of the staff surveyed, 52% recorded that patient satisfaction had stayed the same, and 38% that it had improved to some degree and 10% were not sure. 4.5.4 Examples of improvements As well as rating their improvements, participants were asked for specific examples of improvements at a unit level. Questions addressed the issues of patient flow; reduction in errors and adverse events. Patient care and flow A total of 14 participants said that ‘ttl’ had not had a direct impact on patient care or flow or that the improvements were not directly or solely attributable to ‘ttl’. There were, in addition, four ‘no’ responses. Of the remaining participants, respondents asserted that ‘ttl’ had contributed to: Improvements in patient day surgery journey Improvements in patient flow as a result of improved communication with staff Improvements due to review of patient satisfaction surveys Increased focus on patient safety Increased focus on patients leading to improvements in continuity of care More time on wards by N/MUM improved patient care. Errors and adverse events Half of the participants indicated that there had not been a reduction in errors as a result of ‘ttl’ and a further three did not respond. Of the participants who had indicated that errors had not reduced, one stated that ‘there weren’t any problems with regards to errors anyway, so there were no changes’. 54 Report of the mid program evaluation of ‘take the lead’ In comparison, one participant claimed that errors had been reduced by 40% because of their participation in ‘ttl’ and another noted that there had been an increase in the error rate because staff were now more aware of the need to report. The remaining participants indicated that errors had been reduced by: Reduced errors through better communication Increased N/MUM presence on ward Improved retention of staff and fewer casual staff has contributed to reduction of errors. 4.5.5 Impact on day to day work of ‘ttl’ Impact of ‘ttl’ on day to day work of N/MUMs N/MUMs’ managers were asked about the impact of ‘ttl’ strategies on the day to day work of N/MUMs. A number (n = 6) reported that ‘ttl’ had not had a direct impact, or that the impact was mitigated or enhanced by other. The remaining respondents identified the following impacts: Improvement in N/MUMs’ capabilities overall (n = 4) Built team work amongst N/MUMs (n = 2) Improved ability to manage staff (n = 7) Improved communication skills (n = 4) Increased awareness of self and wider issues (n = 3) Increased confidence in their work (n = 3) Ability to translate ideas into action (n = 2). Factors prohibiting impact on day to day work included: Too many barriers to implement change (n = 1) No mechanism for changing staff (n = 1) Still cannot spend enough time on ward (n = 1) Expectations of the organisation (n = 1). 55 Report of the mid program evaluation of ‘take the lead’ Impact on N/MUM managers As well as the impact of ‘ttl’ on the N/MUMs themselves and their direct staff, changes to the N/MUMs’ skills were identified as having an impact on their managers. Not all N/MUMs’ managers perceived that changes to their N/MUMs had impacted on their daily work (n = 12), and others considered that it was too early to tell or that they were unsure (n = 4), a number of impacts (both positive and negative) were identified. These included: Better communication and management by N/MUMs means better handling of performance management issues before they become critical (n = 9) N/MUMs have become more independent and better at problem solving, reducing dependence on N/MUM manager (n = 9) Increased visibility of N/MUMs on wards means that their managers have picked up more of their administrative load (n = 3) Increased confidence, empowerment and more skills in their toolkit (n = 2) Less reliance on the Director of Nursing (DON) to initiate change at a unit level, although support still required (n = 3) Shorter meetings and less time needed to “sell projects” and less time spent chasing reports More resources needed for increased number of projects (viewed positively). 56 Report of the mid program evaluation of ‘take the lead’ 4.6 Barriers to the program’s implementation Participants were asked about several aspects of the barriers which may have impeded N/MUM’s ability to implement changes after participation in ‘ttl’. These included changes they would have liked to have made, but were unable to do so. Only a few N/MUMs identified changes which they would have liked to have made, but were unable to. Of 30 participants, 11 said explicitly that there was nothing they wished to implement that they could not. The others indicated a small number of specific projects they could not get underway, but most identified areas of further training or input. A few participants identified barriers to implementation of changes which N/MUMs would like to have made. These included: obstruction from medical staff (n = 1); lack of cross institutional collaboration (n = 1); need for more involvement of staff, including CSOs, in quality improvement (n = 2); time constraints (n = 2); and a lack of resources, both human and equipment (n = 4). The managers of N/MUMs identified a similar list of barriers. These included: time (n = 3); local courses already provided at a higher level (n = 2); inability to implement ideas in the workplace due to workload (n=3); participation seen as ‘tick box training’; lack of preparation of, and information provided to, DONs; structural limitations; staff resistance; antagonistic culture; and interdependence with other organisations (all the latter responses are n = 1). Overall, however, most comments from N/MUMs’ managers were positive about the impact of ‘ttl’. One participant gave a clear summation of the barriers affecting implementation of changes. They said that the biggest barrier to implementing change was the “… [the] stark reality that you come back to work and you are straight back in and up to your elbows in hard work.” [N/MUM manager, regional hospital] Surveyed staff also identified a series of barriers to improvement initiatives at a unit level. These included: staff attitudes (n = 1); ‘cultural aversion’ or reluctance to change (n = 2); initial organisational support for the initiative which then ‘petered out’ (n = 1) ; workload (n = 1); and several changes being implemented at once (n = 2). 57 Report of the mid program evaluation of ‘take the lead’ 4.7 Strategies required to ensure the sustainability of changes 4.7.1 N/MUMs’ perceptions of sustainability of change One element of the evaluation was to identify the factors which influenced the sustainability of changes made by N/MUMs after their participation in ‘ttl’. All participants responded to this question. A total of 25 said that the changes they had put in place had been sustainable. Of these participants four noted the changes were ‘sustainable so far’ and several indicated that the changes had been made were successful but did not relate the reasons why they thought this was so. Factors identified as affecting the sustainability of changes included: N/MUMs’ ability to drive and reinforce changes (n = 5) Difficulty in attaining and sustaining cultural and behaviour change (n = 2) The loudness of ‘change resistors’ (n = 1) Evidence of success and benefits, including results of audits (n = 4) Patient centred focus (n = 1) Staff becoming part of the process (n = 1) Positive feedback to staff (n = 1) Reducing negative messages to staff (n = 1) Support of management (n = 1) Cohesive teams (n = 1) Clear plans and processes (n = 1). An example of the factors needed to sustain changes is presented in the following quotation from an N/MUM. They describe the process of implementing changes as a result of the lean thinking module in the following way: “Yes the changes have been sustainable especially Lean Thinking. It worked because of supportive managers e.g. from the Leadership module (learning how to lead) enabled me to develop ideas e.g. I took the staff on a planning day at which we developed values (explicitly stated and shared) and we did team building activities. This has led to great changes on the ward that have come from the staff. The managers supported me. When I started ‘ttl’ I had a group of new staff who were very keen to change. Now the staff are stuck in their 58 Report of the mid program evaluation of ‘take the lead’ ways. It comes down to communication and how you communicate the need to change. The value of the changes need to be communicated - this could have been better covered (perhaps a module incorporated re the skills to communicate the value of change). Health is a constant change. An element in the communication module that focuses on change management would have been really useful. As there is ‘change fatigue’ among nurses and staff, keeping interest in new things in the light of constant change is very difficult e.g. changes from Garling etc.” [N/MUM, state-wide service] 4.7.2 N/MUM managers’ and staff perspectives on the sustainability of change Managers of N/MUMs identified a number of factors which they felt contributed to the sustainability of changes implemented by N/MUMs. These include: Practical approaches that can be applied in many areas (n = 3) Support from local managers (n = 2) Collaborative decision making and implementation (n = 3) Effective communication between staff at all levels (n = 3) Increased confidence (n = 2) Support of staff (n = 2) Identification of clear benefits for staff (n = 2) Small changes which are easily sustainable (n = 1) Need to maintain enthusiasm once returned from course (n = 1) Removal of systems and resources act like a barrier (n = 1) Peer support (n = 2) Resources including CSOs (n = 1) Coaching (n = 1) Pre-planning and integration into routine practice (n = 1) Focus on staff (n = 1) Focus on patient care (n = 1). 59 Report of the mid program evaluation of ‘take the lead’ N/MUMs’ staff were also able to identify a series of factors which they believed contributed to the sustainability of change within their units. These are presented in Table 12, below. Table 12: factors affecting the sustainability of change from staff perspective FACTOR EXAMPLE Support and recognition Support from the AHS in getting medical officers to change practice to fit in with the AHS priorities Support from management Resourcing ratios fairly and at benchmarked levels Structural and resources issues Ongoing financial support and support from organisational management and time to develop and implement staff and patient education programs Decrease workload. Increase CSO equitable across regional and rural sites Measurement of the changes and positive feedback from senior management Quality improvement Training N/MUM capabilities Continuously review the unit performance and stakeholders' comments Training in change management and leadership Education on managing change and how to work with resistance Good communication, team approach , quality activities Interpersonal skills, conflict resolution, people management skills 60 Report of the mid program evaluation of ‘take the lead’ 4.8 Essentials of Care and Caring Together: The health action plan for NSW 4.8.1 Essentials of Care (EOC) EOC is being implemented in every ward in NSW over a three year period. In the current study, the prevalence of implementation and perceived effect of EOC was examined. Of the N/MUMs who were interviewed, 17% stated that EOC had been introduced in their wards, 20% indicated that implementation had begun (and were at various stages of that implementation) and 63% had not begun implementing EOC. Within the group for whom EOC had been introduced, 100% (n=5) identified that there had been changes made at least some of which could be attributed to EOC. One N/MUM stated that all of the changes they had made had been due to EOC rather than ‘ttl’. Those who said that EOC had stimulated changes in their wards noted that the changes arising from EOC were focused on patient care (clinical) needs and driven by staff on the ward. These changes included the introduction of multidisciplinary ward rounds, handover, changes in medication administration process and the development of values and mission statement by staff. One N/MUM captured the difference between the effects of ‘ttl’ and EOC as one of focus. That is that while ‘ttl’ focused on the skills of the N/MUM (e.g. communication and leadership), EOC had a clinical focus. Another N/MUM reported that the effects of EOC included an: “… increased culture of staff wanting challenge and change [and an] increase in the amount of open discussion about change and attempting change as a team.” [N/MUM, tertiary hospital] Approximately half of the N/MUM managers (57%) and staff (48%) stated that EOC had been introduced in their organisations. Managers were able to identify the changes that the staff had made that were due to ‘ttl’ and those that were due to EOC. Table 13 depicts key elements of the managers’ responses that support their claim. Table 13: Key elements of managers’ comments about how they identified between effects due to EOC and ‘ttl’* KEY ELEMENTS RESPONDENTS EOC is more about the bedside care 2 EOC is patient focused 1 61 Report of the mid program evaluation of ‘take the lead’ KEY ELEMENTS RESPONDENTS ‘ttl’ is leadership focused and patient focused 2 EOC supports staff initiatives and staff driven change 4 ‘ttl’ supports N/MUMs to make change 1 * More than one response possible per participant “’ttl’ was purely managerial, EOC is purely basic nursing care related so it is not difficult to distinguish management of practice development ... need to know more about change management. This module was not included but should have been” [N/MUM manager, metropolitan hospital] 4.8.2 Caring Together: The health action plan for NSW The N/MUMs (47%) identified improvements that had been made in their ward in line with Caring Together. Examples of some of these initiatives other than attending ‘ttl’, introducing EOC or the employment of a CSO have been depicted below (Table 14). Some N/MUMs reported more than one improvement as a result of Caring Together. The most frequently cited changes included alternations in processes for handover and patient care plans and those stimulated by Between the Flags. It was noted by one N/MUM that: “Some [changes] are directly due to ‘ttl’, others a combination of Caring Together and Between the Flags...” [N/MUM, tertiary hospital] Table 14: Examples of improvements identified by N/MUMs to have been made in line with Caring Together* EXAMPLES OF IMPROVEMENTS MADE RESPONDENTS Handover changes, introduction of ISBAR (n=2) 7 Nursing case review/care plan/models of care 5 Between the Flags 4 Implemented patient/staff ratios and will not open beds if there are not enough staff according to this ratio 1 Gendered bathrooms 1 * More than one response possible per participant 62 Report of the mid program evaluation of ‘take the lead’ N/MUMs’ managers (70%) identified improvements that had been made in their ward in line with Caring Together. Examples of some of these initiatives other than attending ‘ttl’, introducing EOC or the employment of a CSO are presented below (Table 15). Usually N/MUMs’ managers reported more than one improvement as a result of Caring Together. The most frequently cited changes included changes in processes for handover and hand hygiene. Table 15: Examples of areas of improvement in line with Caring Together reported by managers* IMPROVEMENTS RESPONDENTS Handover changes, introduction of ISBAR 12 Hand hygiene 8 Between the Flags 5 Deteriorating patient 4 Picture of managers and staff in ward 4 Early DETECT program 3 Staff ID and colour coding 3 Normalising change 2 Discharge planning 2 Multidisciplinary rounds 2 Peer nursing review 1 Improved partnership with community service providers 1 Clinical check list 1 Equipment modifications 1 Improved communication 1 Team nursing 1 Peer nursing review meeting 1 Medication safety 1 Patient moved through ED within 4 hours 1 TLC program 1 Job description updates 1 * More than one response possible per participant 63 Report of the mid program evaluation of ‘take the lead’ 4.9 Conceptual Framework for the Nursing/Midwifery Unit Manager Role The Conceptual Framework for the Nursing/Midwifery Unit Manager Role had been read by 70% (n = 21) of the N/MUMs interviewed. Of those N/MUMs who had read it, 38% (n = 8) reported that the Conceptual Framework accurately represents the purpose, capabilities and core functions of the N/MUM’s role, 33% (n = 7) articulated that the Conceptual Framework could be strengthened, and 9% (n = 2) stated that it was not an accurate representation. One N/MUM asked about the Conceptual Framework evaluated it as “very clear and good, fitting and appropriate” [N/MUM, metropolitan hospital]. However, at the other end of the spectrum, another N/MUM stated that it “undervalued N/MUMs, there is no sense of how pivotal N/MUMs are” [N/MUM, tertiary hospital]. Suggestions of ways in which the Conceptual Framework could be improved fall into three overlapping categories. The first category proposes that the Conceptual Framework is too open and needs to define the role of the N/MUM more specifically. Comments in the second category suggest that the pivotal role of the N/MUM is not recognised, that the role of the N/MUM is undervalued and that administrative time demands of the role are not reflected. The third category included the comment that the Conceptual Framework for the N/MUM role was more relevant in some locations (rural versus metropolitan) than in others. Of the N/MUM managers interviewed, 66% had read the Conceptual Framework and thought that it accurately represented the role of the N/MUM. Some Managers described the document as very helpful: “Absolutely fantastic document. Cements all N/MUMs. *We are+ creating new job descriptions for positions based on the Framework” [Manager, rural hospital] Other managers had not read it (31%) or did not feel that it was a good representation of the role (3%), some describing it as too broad. In this N/MUM manager’s opinion, the Conceptual Framework is: “very worthy but quite broad, too broad, N/MUMs are expected to do too much.” [Manager, state-wide service] 64 Report of the mid program evaluation of ‘take the lead’ 4.10 Strengthening of role as N/MUM Participation in ‘ttl’ was perceived to have strengthened their role as an N/MUM by 80% (n=24) of the N/MUMs interviewed. The comments and examples of how ‘ttl’ strengthened the role of the N/MUM were categorised into six groups (Table 16). An improvement in skills, clarification of the role, and increased confidence in their ability to perform the role were identified as ways in which the interviewed N/MUMs had been strengthened in their role as an N/MUM. The importance of networking and sharing ideas was also identified as important in strengthening the N/MUM role. Table 16: Ways in which the N/MUM role was strengthened by ‘ttl’ (N/MUMs)* WAYS IN WHICH THE N/MUM ROLE WAS STRENGTHENED BY ‘ttl’ RESPONDENTS Skills improvement e.g. communication, lean thinking 8 Increased confidence in ability to perform role 6 Networking and sharing of ideas 6 Clarified role 5 Increase in staff respect and expectation of leadership 3 Reinforced existing skills, practices and knowledge 3 * More than one response possible per participant While the majority of N/MUMs perceived that their role had been strengthened through participation in ‘ttl’, 17% did not hold this view. According to one of these N/MUMs’ interviewed ttl’ was: “pitched too low, the topics were relevant topics but not content.” [N/MUM, tertiary hospital] N/MUMs’ managers reported that participation in ‘ttl’ was perceived to have strengthened the role of the N/MUM (90%). While 3% of the managers interviewed stated that they did not perceive that ‘ttl’ had strengthened the role of N/MUM, 7% reported being unsure if a strengthening of the role could be attributed to ‘ttl' or whether it was due to experience. N/MUMs’ managers gave examples of how they perceived that the N/MUM role had been strengthened through participation in ‘ttl’. Managers may have provided more than one example. An improvement in skills, increased confidence to in their ability to perform the role, and feeling valued and supported, were identified as ways in which ‘ttl’ strengthened in the N/MUM in their role. The importance of networking and sharing ideas was also identified as important in strengthening the N/MUM role. 65 Report of the mid program evaluation of ‘take the lead’ A renewed focus and invigoration, and sense of ownership of the unit in N/MUMs were also proposed as ways ‘ttl’ strengthened the role: “More confidence, more time on the floor, a role model. The more the person “walks the walk” the more it increases confidence” [N/MUM manager, state-wide service] “Made them leaders and taking accountability” [N/MUM manager, Rural/Regional Hospital] The comments and examples of how ‘ttl’ strengthened the role of the N/MUM were categorised into six groups. These are presented in Table 17. Table 17: Ways in which the N/MUM role was strengthened by ‘ttl’ (managers)* WAYS IN WHICH THE N/MUM ROLE WAS STRENGTHENED BY ‘ttl’ Skills improvement and strengthening communication, lean thinking existing skills RESPONDENTS e.g. 10 Increased confidence in ability to perform role 9 Networking and sharing of ideas 9 Clarified role 5 Invigorated and refocused 4 Supported and valued 3 Increased ownership of role/unit 4 * More than one response possible per participant 66 Report of the mid program evaluation of ‘take the lead’ 4.11 Introduction of the Clinical Service Officer’s position This section presents the N/MUMs’ views on the introduction of the CSO. Additional data from the perspective of the CSOs are presented in Appendix 8.5. 4.11.1 Introduction of the CSOs A CSO had been allocated to 20 (66.7%) of the N/MUMs interviewed. One N/MUM had been allocated but did not use the CSO. In light of this, the results are reported on the basis of 19 N/MUMs experience of utilising the CSO role. Of those N/MUMs five had been allocated a CSO who had since resigned, with (n=2) or without (n=3) being replaced at the time of interview. The length of time the same CSO had been employed for their unit ranged between one week and 12 months (average length of time = 7 months). All but one of the N/MUMs allocated a CSO identified that the CSOs reported to them with 45% of those CSOs also reporting to at least one other N/MUM or N/MUM manager. Of the NUMs to whom a CSO had been allocated, the CSO was employed on a full time basis. The hours of employment of the CSOs employed part time ranged between 12 to 32 hours per week. The recruitment process did not involve 74% of the N/MUMs who had been allocated a CSO and of those 43% stated that they would have liked to have been or that it was important that they were involved in the recruitment process. Of the five N/MUMs for whom the CSO position had to be refilled, three were not involved in the initial recruitment process but would be or were involved in the subsequent recruitment of a CSO. When asked if there was a CSO job description, two were unsure, six (32%) considered the position description to be too generic requiring local adaptation or development as the role unfolded. The N/MUMs to whom the CSO reported were responsible for the allocation their duties for 100% of CSOs. Two of the CSOs also had input into the allocation of their duties and for one CSO, the Deputy Director of Nursing allocated duties with the N/MUMs. Of the N/MUMs’ managers interviewed, 22 (73%) indicated that there had been a CSO employed in their organisation. The results reported in the remainder of this section in relation to the CSO role are based on the responses of those 22 managers. The number of CSOs employed was identified in FTEs. This ranged from 0.5 FTE to 14.4 FTEs. The length of time that the CSO had been employed ranged from two to 14 months with the average length of time being nine months. A similar percentage of N/MUMs’ staff (70%) stated that their organisation had CSOs. 67 Report of the mid program evaluation of ‘take the lead’ While 83% of the managers stated that the CSO duties were allocated by the N/MUM in their organisations, only 63% noted that the CSOs also reported to the N/MUM. Among the CSOs identified as reporting to the Director of Nursing (DON), Assistant or Deputy Director of Nursing (A/DON or D/DON), manager, and administrative supervisor (n=8), only one manager noted the tasks were allocated by someone other than the N/MUM. In this case, the CSO role was shared across two hospitals with two CSOs (job sharing, 1.47 FTE) reporting to the D/DON. Among the managers interviewed, 64% reported that the N/MUM with whom the CSO would work was involved in the selection process for the CSO position. Among the managers who reported that the N/MUM had not been involved, one commented that it was very important for the N/MUM to be involved in that process. The N/MUMs were asked to indicate whether or not the CSO was undertook a range of duties including data entry and reporting, workforce matters, resource management, documentation/records management, or general administrative activities. They were also asked to indicate any other activities that the CSO undertakes in their unit (Table 18). Table 18: Percentage of CSOs undertaking duties DUTY TYPE YES NO UNSURE/NOT YET and 19 (100%) 0 0 Workforce matters (rostering, recruitment, leave, payroll) 17 (89%) 3 (16%) 0 Resource management 14 (74%) 3 (16%) 2 (10%) Documentation/records management 15 (79%) 3 (16%) 1 CSO did documentation for one N/MUM to whom they reported but not the other General administrative activities 19 (100%) 0 0 Other activities 17 (89%) 3 (16%) 0 Data entry reporting The N/MUMs were asked to identify whether there were any additional duties undertaken by the CSO allocated to their unit. The additional role of the CSO in recording staff performance appraisal data, organising staff training in-services, 68 Report of the mid program evaluation of ‘take the lead’ Occupational Health and Safety activities, non-clinical audits and quality improvement documentation were reported by several of the N/MUMs (Table 19). Table 19: Types of additional duties undertaken by CSOs* ADDITIONAL AREAS IN WHICH CSOS ASSISTED RESPONDENTS Staff training and performance appraisal data 6 Non clinical audits documentation 5 and quality improvement Occupational Health and Safety activities 4 Check equipment e.g. buzzers 2 Liaise with donor families requisitions for patients and organizes flight 2 Mandatory reporting documentation 1 EQUIP documentation 1 Assistance with organization of referrals 1 Chases results 1 Assist with fundraising activities 1 * More than one response possible per participant While 91% of the N/MUMs’ managers interviewed indicated that the CSOs had had a positive impact on the work that the N/MUMs undertook, one N/MUM manager (4.5%) was ambivalent and one (4.5%) indicated no effect. However, 14% (n=3) of the managers stated that the impact had been limited. The reason offered was that they were not a large enough resource to make a big difference. Examples of types of duties the CSOs performed that impacted on the role of the N/MUM were volunteered by 64% of the interviewees. These are presented in Table 20 below. The most commonly identified duty impacting on the N/MUMs’ work was administrative assistance followed by duties associated with rostering and staffing. Stock ordering and duties associated with audits and KPI reports were also identified. Table 20: Examples duties the CSOs performed that impacted on the role of the N/MUM* EXAMPLES OF TYPES OF CSO DUTIES THAT IMPACTED ON N/MUMS’WORK RESPONDENTS Administrative (e.g. minutes, organizing meetings, data entry) 10 Rostering and staffing duties 8 Stock ordering 3 69 Report of the mid program evaluation of ‘take the lead’ EXAMPLES OF TYPES OF CSO DUTIES THAT IMPACTED ON N/MUMS’WORK RESPONDENTS Audits, KPI reports, report writing 3 Bed board and organizing patient transport 2 * More than one response possible per participant When specifically asked to identify whether the employment of the CSO had affected the amount of time the N/MUMs spent on administrative tasks, 82% of managers articulated that there had been a positive impact. Of these, there were two managers who claimed a limited impact on administrative tasks. No impact on the N/MUMs’ administrative tasks was reported by 9% of the interviewees and 9% were unsure (Table 21). Most (43%) of N/MUMs’ staff where the unit had a CSO, indicated that the CSO had had an impact on the N/MUMs’ time spent on administrative staff. The rest either felt that there had been no impact (13%) or were unsure (54%). Table 21: Impact of the CSO on administrative duties of N/MUM reported by managers IMPACT OF THE CSO ON TIME SPENT ON ADMINISTRATIVE DUTIES BY N/MUM RESPONDENTS PERCENTAGE Yes 16 73% Yes but limited 2 9% Unsure 2 9% No 2 9% 4.11.2 N/MUM’s perspective of the impact of CSOs on their role The majority of N/MUMs’ interviewed (63%) reported that the introduction of the CSO role had impacted on the type of work that they did and that this had been helpful particularly in relation to reducing the time they had previously spent doing administrative tasks, allowing more time to be spent: “to co-ordinate patient care and on higher level management tasks.” [N/MUM, tertiary hospital] The impact of the role was described by some of the N/MUMs as “dramatic”, “massive”, “fantastic”, “excellent”, and “huge”. There were 26% of the N/MUMs who were ambivalent about whether or not the CSO role had impacted on the type of work they do. Reasons offered included a lack of infrastructure and resources to support the work of the CSO (e.g. desk, computer) and the initial intensive training required. Two N/MUMs reported that the introduction of the CSO had not positively 70 Report of the mid program evaluation of ‘take the lead’ impacted on their work, with one explaining that a non-health professional was not helpful in the role. When asked whether the CSO role had decreased the amount of time the N/MUM spent specifically on administrative tasks, 15 (79%) responded that it had reduced the amount of time they spent on administrative tasks. “I have gone from being able to relieve staff on breaks for only one hour to about three hours ... I no longer have to work late.” [N/MUM, metropolitan hospital] Two of these N/MUMs indicated that while the time they had spent on administrative tasks had decreased, their workload had increased in the initial period of the CSO employment due to the training requirements. When the CSO left there was further time investment required to train the new CSO. Four of the N/MUMs reported that the employment of the CSO had not reduced their administrative workload with three of them stating that the CSO had caused an increase in their administrative workload because while the CSO role is valuable, the process of implementation was not and the wrong person for the role had been chosen (n=2) or the way the role had been set up was not helpful (e.g. the lines of reporting were not clear). 4.12 Impact of the CSO role on the clinical team In order to identify whether the CSO role also supported the work activities of nursing, medical and allied health staff, the N/MUMs were asked what, if any, impact they thought there had been on the work of these members of the clinical team. There were seven N/MUMs (37%) who reported that there had been no impact of the CSO role on the work of these members of the clinical team. Twelve N/MUMs (63%) recounted that there had been a positive impact of the CSO role particularly in relation to assistance they provided to allied health personnel. Educators, doctors, and nurses were also noted to have been positively affected by the CSO role. Some of the N/MUMs (21%) noted that in freeing them up to be more available the other members of the clinical team benefited from the CSO role. In order to identify whether the CSO role supported the work activities of nursing, medical and allied health staff, the N/MUMs’ managers were asked what, if any, support they thought there had been on the work of these members of the clinical team. There were five managers (28%) who reported that there had been no impact of the CSO role on the work of these members of the clinical team. A supportive impact of the CSO role on the work of other members of the clinical team 71 Report of the mid program evaluation of ‘take the lead’ was affirmed by 41% of the interviewed managers. A limited effect on the role of the clinical team was suggested by a further 18% of the managers interviewed. The CSO role was reported to indirectly support work activities of nursing, medical or allied health staff by 9% of N/MUM managers (Table 22). Of the staff themselves, 48% reported that the CSO contributed to their work, 22% said they did not, and the rest were either unsure (n = 1) or did not reply. Table 22: N/MUM managers’ perception of impact of the CSO on the role of the clinical team SUPPORT OF THE CSO ROLE ON THE WORK OF THE CLINICAL TEAM RESPONDENTS PERCENTAGE Yes 9 41% Yes but limited 5 18% Indirectly 2 9% No 5 28% No response 1 4% 4.12.1 Impact of the CSO role on patient care There were 37% of N/MUMs who reported that the CSO role had not impacted patient care. However, the CSO role was considered by the majority of N/MUMs to have positively impacted on patient care. The ways in which they suggested this occurred are tabulated below. They fall into two categories that can be summarised as ‘streamlined processes’ or ‘releasing the N/MUM for clinical care’ (Table 23). Table 23: The ways in which the CSO role impacts patient care THE WAYS IN WHICH THE CSO ROLE IMPACTS PATIENT CARE EXAMPLES Stream line processes: improved efficiency of patient care Discharge summaries faxed Nurses RESPONDENTS not looking 4 for documentation At weekly case conferences the CSO makes action items and so there is quicker follow up EDDs behind beds – patients are 72 Report of the mid program evaluation of ‘take the lead’ THE WAYS IN WHICH THE CSO ROLE IMPACTS PATIENT CARE EXAMPLES RESPONDENTS more involved Co-ordination of care improved Fewer loose ends Fewer things get missed Releasing N/MUM and nurses for clinical care 8 More time to focus on patient care N/MUM has more time on the floor with patients N/MUM is on the floor during morning rounds The majority of interviewed N/MUMs’ managers (73%) reported that the CSO role had positively impacted patient care. Three of the managers (14%) claimed that there had been no impact and 14% were unsure or ambivalent about the impact of the CSO role on patient care. Managers identified ways in which the CSO role affected patient care. These fall into two categories summarised as ‘administrative focus’ or ‘N/MUM clinical supervision’ (Table 24). For example, responses when asked if they perceived an impact on patient care as a result of the introduction of the CSO included: “Yes the NUMs are out there. If there is an issue with a patient, clinical or non clinical, they’re there. The can solve the problem because they are the most senior person on that ward.” [N/MUM manager, regional hospital] Table 24: The ways managers perceive that the CSO role impacts patient care* THE WAYS IN WHICH THE CSOEXAMPLES ROLE IMPACTS PATIENT CARE RESPONDENTS Auditing gets done Administrative focus 4 Better patient flow Better staffing and rostering Releasing N/MUM nurses for clinical care and More time to focus on patient care 73 15 Report of the mid program evaluation of ‘take the lead’ THE WAYS IN WHICH THE CSOEXAMPLES ROLE IMPACTS PATIENT CARE RESPONDENTS Better clinical management and supervision N/MUM available and more visible * More than one response possible per participant Just over a third of N/MUM’s staff (39%) said that CSOs had contributed positively to patient care, while 7% said that they did not. The rest either were unsure of the impact (23% or simply did not respond. Where the staff indicated that the CSO had had a positive impact on patient care the reasons provided included: N/MUMs spend more time on ward (n=2) and CSO had taken over administrative work, or is more efficient at administrative work (n=3). The following two comments were made by participants who indicated that the CSO had had a positive impact on patient care, and reflect the complexity of the situation. “Only for one NUM. We have one FTE CSO for 2 hospitals and 5 NUMs and 2 NM. It is ludicrous to think they are going to make a substantial difference.” [Staff member, regional health service] “CSO's have been very effective in providing useful support and assistance to the NUM. The role will grow further with time.” [Staff member, metropolitan service] 4.13 Unexpected impacts/outcomes of the CSO role There were no unexpected impacts of the CSO role reported by 47% of the N/MUMs interviewed. However, 53% reported both positive and negative unexpected impacts. Perceived negative impacts included the time spent training the new CSOs, the high turnover of CSOs, feeling out of the loop, and having no control over what the role of the CSO is. The positive unexpected impacts were a decrease in the number of lost items, assistance provided to other staff members including the ward clerk, and the support of consistency across units. To illustrate this latter point, one of the N/MUMs reported the following unintended consequence of the introduction of the CSO role: “The CSO is part time for two N/MUMs. She has played a role in connecting the N/MUMs and coordinating things around the hospital which has led to increased consistency e.g. if she sees one NUM doing something she reminds the other.” 74 Report of the mid program evaluation of ‘take the lead’ [N/MUM, state-wide service] While 50% of interviewed N/MUM managers reported that there were no unexpected impacts of the introduction of the CSO role, and 14% who identified unanticipated negative outcomes including friction with other staff (e.g. ward clerks) and an unrealistic expectation that as a result of the CSO position, (e.g. the expectation that ‘the N/MUM would [now] be available to be on the floor all of the time)’. There were 14% of N/MUM managers who identified unexpected benefits and offered suggestions about the CSO role (Table 25). In particular, managers identified benefits related to the aspect of the CSO role that allows them to share ideas across wards. This is illustrated by the comment of a Manager in a Tertiary Hospital: “Forces N/MUMs to consider whether their practices are optimal on account of CSOs who share wards and report back on how things are done differently.” [N/MUM manager, tertiary hospital] Table 25: Unexpected impacts of the introduction of the CSO role and managers’ suggestions about the role UNEXPECTED OUTCOMES Better communication Standardisation of on administrative tasks across wards Sharing of ideas on administrative tasks across wards SUGGESTIONS The job is too big for the number of hours allocated The efficacy of the CSO role is very dependent on the characteristics of the individual The expectations of the role must be kept in check with the N/MUM to retain managerial tasks In relation to the N/MUMs’ staff, 13% stated that there had been an unexpected impact as a result of the introduction of the CSOs, 22% felt that there had not been. All of the staff who reported there had been no unexpected impact, and who provided further information, said that this was because the CSOs were “spread too thin” to have any impact. For staff who said there had been an unexpected impact, all except for one (“increase in need for NUMS to be double checking roster and reroster staff“) were positive. “Better management of casual pool staff, prompt entry of rosters, second set of eyes to detect errors in rosters or documents, reduced time spent typing up data, documents created faster and delivered to appropriate places on time.” 75 Report of the mid program evaluation of ‘take the lead’ [Staff member, regional health service] “My personal recognition of tasks that can be completed by CSO and not myself. CSO is invaluable to allow time to not only spend with pts but also with the staff.” [Staff member, regional health service] 4.13.1 Ways in which the CSO role could be improved The N/MUMs identified ways in which aspects of the introduction of and the CSO role itself could be improved. The most frequently cited changes were an increase in the N/MUM-to-CSO ratio and hours that the CSO worked, and more input by N/MUMs into the position description for the CSO. Other suggestions included a training program for all CSOs before they commenced in the unit and a development of the aspect of the CSO role that co-ordinates and links units/wards. The N/MUM managers made recommendations of ways in which the CSO role could be improved. The most frequently made recommendations were to increase the number of CSOs and the hours that CSOs were available (27%) and to give them more training (18%). Other suggestions included that the role of the CSO be adapted to better suit the needs of the units (9%), that the CSO be included as a member of the unit team (4.5%) and that the position be better budgeted for (4.5%). Staff, in addition to N/MUMs and their managers had specific suggestions about improvements to the role of CSOs. Most of the suggestions related to increasing the CSOs time, or their distributed across services (n = 5): “All clinician managers should have access to a CSO. A competent CSO can double to productivity of a Clinician Manager.” [Staff member, regional health service] “Excellent position should have leave relief and we need to ensure they do not get taken up by other departments- some CSO are working primarily for Medical officers- not NUMs, need more we have only 2 for 7 NUMS.” [Staff member, regional health service] “They need to support more clinical departments than just nursing. There are a large number of other departments with the same issues of clinical staff doing administrative tasks that they are inefficient at and therefore make lots of mistakes that take even longer to fix.” [Staff member, regional health service] 76 Report of the mid program evaluation of ‘take the lead’ Two respondents mentioned that CSOs would benefit from additional training. Only one respondent, who knew about the role felt that it was “unclear if initiative is cost effective”. 4.14 Case studies The following section will describe the affect ‘ttl’ has had on two NUMS and their units that were identified as potential participants for an in-depth interview by NSW Health. The information the participants gave is of their personal experience and perspective. It is an opportunity to view two experiences of NUMs who have completed all five modules and what effect if any it has had on them and their units. A discussion follows the comparison that will attempt to tease out potential themes, whilst recognising the limits of generalisability of information. The two cases are briefly described, and a comparison follows in Appendix 8.6. N/MUM1 and N/MUM2 work in large hospitals, the former in a regional area and the latter in a metropolitan setting. Both have a similar number of staff, including a CSO, reporting to them. 4.14.1 Case 1 “It was something that had to happen to be honest” (N/MUM1) When N/MUM1 began her role on the ward, the ward was in disarray. Patient and staff satisfaction was low. Recruitment and retention was low. Her role was mainly administrative and had very few engaging characteristics or as N/MUM1 described it - “this is seriously one of the shittiest positions in the hospital, I do have to tell you – and it's quite recognised for that”. As she spent more and more time in her office she became more disengaged with staff and patients. This had a number of consequences that will be discussed in the analysis. Amongst them was exhaustion: “I was looking a bit beat and battered”. ‘ttl’ was an initiative that she perceived as necessary not only for herself, but for N/MUMs in general. N/MUMs had evolved into the role without formal and standardised training and there was a clear need for definition and clarity of the role, but also of providing management skills to nurses whom had clinical training and limited managerial training. She was initially identified to be a part of the piloting of the program and eventually became a champion for ‘ttl’. She was amongst the first to enrol in the program. 77 Report of the mid program evaluation of ‘take the lead’ 4.14.2 Case 2 “I did think it was a good program, and it's not often that you get together with other N/MUMs” (N/MUM2) N/MUM2 likens her unit to “a revolving door, there's people coming and going the whole time. So it's very hard to maintain any kind of practise or have standards, or have continuity in care”. This structural characteristic has strong implications on staff and patients. She describes a ward that has numerous managers across multiple levels of management and that “it's an environment where nobody knows what the rules are, the goalposts keep changing, and there's too many people ... it's like 'who is in charge?'””. N/MUM2 describes ‘ttl’ as a positive experience and was one of the first to enrol and participate. She believes that although the content was not beneficial to her, as she had already gained this knowledge in her post-graduate studies, it was important and relevant to N/MUM practice. The networking was what she found to be both interesting and beneficial. Overall, she sums the impact ‘ttl’ has had on her personally by stating that “I kind of felt that take the lead thing, maybe did not so much affect how I am a manager, but I think it's affected the management environment”. 4.14.3 Comparison N/MUM1 describes the factors that enabled her to create successful and sustainable change in her unit as: 1) having more time due to the implementation of the CSO; 2) having a better understanding of her role and where it fits in within the organisation; 3) increased confidence gained from the skills she learnt and were reinforced; 4) increased motivation that she felt as a result of participating in the program 5) increased awareness and ability to reflect on the impact her and others action have on patients and staff 6) ongoing support from N/MUMs that was achieved through networking at the workshops and as a result of her coaching role 7) ongoing support from her management team and staff. N/MUM2 describes ‘ttl’ as having less of an immediate impact on her everyday work, but the change it had made in the managerial environment, where N/MUMs now have a common language and an ability and opportunity to voice their needs and concerns as important. She describes leading her team to become more autonomous and capable to impact their work environment and patient care. This was achieved through participating in the EOC program that gave staff the structure through which to reflect, identify and initiate changes. 78 Report of the mid program evaluation of ‘take the lead’ Both N/MUMs describe this as an ongoing process that requires navigating complex systems with limited time and financial resources. Both have recognised the influence of their role as leaders and not just managers and have noted changes that have disseminated through the ward gradually through conversations and a change of attitude (e.g. the push for staff to be more self-sufficient in problem solving) and not only through formalised planned changes. 4.14.4 Discussion As was evident in the description above, at times, the N/MUMs discussed ‘ttl’ and EOC as both having a combined impact on their work and unit. A strong impression that arises from the interviews is that at times it will be impossible to tease out which intervention – ‘ttl’, EOC or other initiatives is the stimulus for changes. Many times the N/MUMs stated that it is a combination of ‘ttl’ and EOC or other clinical interventions. Some changes had been identified through internal initiatives or organisational directives before either ‘ttl’ or EOC. It is the combination of initiatives that created the strong impact described. On both these accounts the units are a better place to work and patients are receiving higher quality care. Both N/MUMs state that there is still much to do. They both feel confident that they have the skills to meet the challenges and have a clearer understanding of their role. They both believe that that there is more support and a shared language with the different stakeholders. They both note that there are issues that need to be addressed systemically and cannot be influenced directly. They agree that they have more ability and forums to voice those needs and concerns. 79 Report of the mid program evaluation of ‘take the lead’ 4.15 Reflections on ‘ttl’ 4.15.1 Has participation changed how you feel about being a N/MUM? When asked whether participation had changed the way they felt about being a N/MUM, 40% reported that there had been no change, 7% did not comment and 53% reported that it had positively changed the way they felt about being a N/MUM. To illustrate, one N/MUM stated that originally from a clinical background, they now feel: “… more empowered ... managing staff is different from managing patients.” [N/MUM, state-wide service] Reported changes in how they felt about being an N/MUM were grouped according to similarity of concepts (Table 26). The two most salient changes centred on perceived empowerment and confidence in their role as an N/MUM and feeling less isolated in that role. One N/MUM noted: “I have more job satisfaction because there is more clarity in what I should be doing. If you know what your goals are it is easier to know when you are doing a good job and this leads to improved satisfaction.” [N/MUM, state-wide service] Table 26: Changes in how N/MUMs perceived being an N/MUM following ‘ttl’* CHANGES IN N/MUM’S PERCEPTION OF BEING A N/MUM RESPONDENTS Feel more empowered/confident/clear/proud about my role 7 Don’t feel as isolated 5 Renewed enthusiasm 2 Feel more appreciated (e.g. by staff and NSW Health) 2 Improved skills increased job satisfaction 1 * More than one response possible per participant 4.15.2 N/MUM managers’ reflection on their participation in ‘ttl’ Those managers who had participated in ‘ttl’ were asked to reflect on their experiences participating in ‘ttl’. They identified improved leadership, consolidated knowledge, learning new skills, networking and refocussing as factors they found to be important. Some managers reported being better able to understand and support 80 Report of the mid program evaluation of ‘take the lead’ the N/MUMs who had done ‘ttl’. Much was enabled through their participation in ‘ttl’. It gave them a ‘common language’ and put them on the ‘same page’ as the N/MUMs. “Some of the NUMs had gone so we weren’t on the same page – they came back with great ideas. It was helpful that I went because when the others were going I could encourage them more and the conversations we then had about take the lead were on the same page.” [N/MUM manager, state-wide service] 4.15.3 Final insights on ‘ttl’ from N/MUMs When offered an opportunity for additional comments about ‘ttl’, only 20% of interviewed N/MUMs declined. The comments from the remaining N/MUMs (80%) were diverse and included suggestions for the way in which the delivery of ‘ttl’ could be improved including running the program over a shorter time span and tailoring the program for the different needs of N/MUMs and to include topics such as NSW Health’s principles on EEO. Other suggestions included the introduction of post ‘ttl’ refresher or regular debriefing sessions, and a greater focus on change management to better equip N/MUMs to help staff manage the many changes that are being made in their wards. Several N/MUMs proposed that it would be worthwhile designing a separate course or requiring managers of N/MUMs to attend so that they will be more supportive of the changes that the N/MUMs try to make as a result of ‘ttl’. The most frequently occurring comments were about the benefits of opportunities to network with other N/MUMs provided by ‘ttl’. 4.15.4 Final insights on ‘ttl’ and recommendations from N/MUM managers When offered an opportunity for additional comments about ‘ttl’, 91% of interviewed managers offered comments. These comments ranged from suggestions about increasing the number of CSOs and developing their role to the suggestion that there should be an equivalent program introduced for managers. The comments were grouped according to similarity of key points and are presented in Table 27 below. The comment offered the most frequently was that ‘ttl’ was an excellent program that should continue. Table 27: Managers’ comments and suggestions following ‘ttl’* COMMENTS AND SUGGESTIONS RESPONDENTS ‘ttl’ is an excellent program that should continue 13 CSO role needs to be developed and more CSOs employed 4 81 Report of the mid program evaluation of ‘take the lead’ COMMENTS AND SUGGESTIONS RESPONDENTS Revise content e.g. include clinical skill coordination and include a component on change management 3 Recognise prior learning with ‘ttl’ 2 Follow up with an advanced program post ‘ttl’ 3 Follow up with a ‘refresher’ 2 ‘ttl’ was particularly helpful for new N/MUMs 2 Encourage continued networking post ‘ttl’ 1 N/MUMs found the networking very helpful 3 Introduce an equivalent program for managers 1 Consistent approach and standardisation of role is excellent 2 Logistical problems with travel and accommodation 2 ‘ttl’ was more helpful for the N/MUMs of some units than others 1 * More than one response possible per participant 82 Report of the mid program evaluation of ‘take the lead’ 5. DISCUSSION 5.1 Overall findings The participants in this evaluation recognised that the role of N/MUMs has changed significantly over the last three decades, and that this change has involved increased managerial and administrative responsibilities. Most N/MUMs and their managers commented on the lack of preparation for N/MUMs to pursue their managerial and leadership roles. The changes suggested by the Garling Inquiry, including the formalisation of the role of N/MUMs, programs for their professional development, and the facilitation of their increased presence in their units, and ‘away from their desks’ was seen to form a new phase in this development. We found that ‘ttl’ had contributed to a considerable degree to the skills development of some of the participating N/MUMs. Of the N/MUM respondents, 60% said that ‘ttl’ was of some value to them. The value of each module, however, differed greatly. In some cases this was a structural issue: N/MUMs whose staff were centrally rostered found that module contributed little to their work. The financial module was open to the same criticisms. In several cases, participants noted that these were ‘a waste of time’. One of the most recounted determining factors of value of the ‘ttl’ modules was how much prior education or experience the N/MUM already had. This was not a universal however: individual attitudes and the manner in which the module presented meant that some people with extensive experience were able to gain value from the program. This general point is supported in educational studies and the literature (Leimbach, 2010, Kirkpatrick et al., 2006, Nijman et al., 2006, Alvarez et al., 2004). For those for whom ‘ttl’ was of value, the program was seen to have enabled and or empowered N/MUMs to implement changes in the workplace. It is important to note this distinction however: not all N/MUMs, N/MUMs’ managers or staff considered that ‘ttl’ had had an impact on N/MUMs. More common than the ‘no impact’ response, however, was respondents’ inability to identify whether ‘ttl’ had contributed to the N/MUM’s development or not: a range of confounding factors, including professional maturity, other development and change programs in the workplace, and the N/MUMs own background made it difficult to quantify the impact. Caution therefore has to be placed on too strong a representation of the Likert results. Almost half (n = 14) of the N/MUMs interviewed said that they could not identify a day to day impact of their participation in ‘ttl’. However, less than 20% of N/MUMs and N/MUM managers who participated in this evaluation stated either 83 Report of the mid program evaluation of ‘take the lead’ that they were unsure whether ‘ttl’ had strengthened or contributed to the role of N/MUMs, or that it had not. Respondents were more comfortable providing examples rather than quantitative measures of outcomes. Where ‘ttl’ had an impact, it appears to have influenced N/MUMs’ ability to change and in their own perceptions to improve, many aspects of their workplace, including efficiency, patient outcomes, change management, staff outcomes and capabilities and skills. Even though individual cases differ (both in response to the program and in its subsequent impact), the results overall show that for those N/MUMs who were able to implement changes in the workplace, ‘ttl’ was an important contributing factor. This is particularly, but not only, in cases where N/MUMs had little prior training and or experience. 5.2 Positive benefits N/MUMs have put in place identifiable changes as a result of their participation in ‘ttl’. The most commonly noted changes, by all participants (N/MUMs, their managers and staff) involved implementation of some aspect of lean thinking: this may be because, in the view of one participant, that model allows for small incremental changes which are highly visible. However, many N/MUMs have implemented a range of other changes ranging from the modification of their individual communication styles, to new approaches to the rostering of staff, to the creation of multi-method team based approaches to the co-ordination of care. Differences in the sophistication and range of changes meant that their impact was difficult to measure for many participants; however individual participants indicated cost and time savings as a benefit. Changes in N/MUMs’ capabilities and skills varied with individuals across the several measures which were taken. Of those N/MUMs who felt that ‘ttl’ had had an impact on their work, 67% believed that their job performance had improved to some degree since their participation in ‘ttl’. In comparison, 83% of N/MUMs’ managers felt that their job performance had improved (67% due to ‘ttl’, 13% due partly to ‘ttl’ and 3% due to other factors). A majority of N/MUMs (62%) recognised that their staff’s performance had improved also. However, across all participant groups, there were indications of improved communication by N/MUMs, particularly in critical contexts. This was reflected in the changes which were deemed to have been successfully implemented: the most common change related to N/MUMs ability to communicate with, and provide feedback to, their staff reportedly resulting in increased staff satisfaction. 84 Report of the mid program evaluation of ‘take the lead’ This was mirrored in their ability to handle complex situations: 80% of N/MUMs who felt ‘ttl’ had had an impact, thought that their ability to manage difficult situations had improved, and 71% said that their negotiation skills had improved. Supporting this, 82% N/MUMs and 65% of N/MUM managers felt that N/MUMs’ ability to manage staff had improved. This was borne out by several of the N/MUM managers who noted that one of the impacts on their own work as a result of their participation in ‘ttl’ was a reduction in the number of performance reviews which ‘progress up’ the ladder for attention. Other measures varied. Even with the N/MUMs who felt ‘ttl’ had had an impact, around 58% felt that their unit’s performance or efficiency had improved. Fewer felt that adverse events had changed: 72% indicated that post ‘ttl’ they had stayed the same, although some participants noted this was for reasons other than a lack of impact of ‘ttl’. About 49% of NUMs and 22% of N/MUMs’ managers claimed that patient flow had improved to any degree. There appeared to be minimal impact on patient satisfaction, compliments or complaints attributable to ‘ttl’. 5.3 Key factors The success of, and barriers to, N/MUMs attempts at change were attributed to a range of structural, cultural, organisational and relational factors. These factors were supported by the findings from the literature review. The three key elements to the successful transfer of learning into action relies on a combination of the clinicians’ own personal commitments and characteristics; the way in which the training did or did not prepare them for the transfer of that learning; and workplace climate and organisational support. Participants gave consistent examples of the importance of these factors across all participating respondent groups. The last of these factors, workplace climate and organisational support, were also said to support the sustainability of the changes implemented. This was also true of their perceptions of the sustainability of changes they had made. A combination of senior management, peer and staff support is considered essential to ensuring the continuation of change efforts. One of the intangible benefits of participation in ‘ttl’ emerges from the opportunity for N/MUMs to network and share solutions to common problems. Related to this, and identified both by the N/MUMs themselves and their managers, is an increase in their self-confidence. These are key future success factors. Overall, the role of the CSOs was said to have had a positive impact on reducing the administrative workload of most N/MUMs, although in some cases this was 85 Report of the mid program evaluation of ‘take the lead’ considered to be limited. From the CSOs perspective, undertaking a new, and at times not clearly defined role has posed some challenges, particularly for CSOs who are geographically or organisationally isolated, or those who are spread over several locations. This evaluation shows that the introduction of ‘ttl’, along with other improvement mechanisms, such as the Essentials of Care program and the introduction of CSOs, has enabled a range of N/MUMs to develop, implement and sustain changes to their workplace. In the cases where N/MUMs have been able to transfer their learning from ‘ttl’ effectively, these changes have resulted in improvements in finances, staff satisfaction and morale, and patient care. 86 Report of the mid program evaluation of ‘take the lead’ 6. CONCLUSION The mid program evaluation of ‘ttl’ shows clearly that while ‘ttl’ has had some impact and a range of positive effects, in some areas this impact is mixed. To use a metaphor from patient safety, much of the ‘low hanging fruit’ – the small incremental workplace changes and engagement of N/MUMs have been ‘picked’. Nonetheless, ‘ttl’ shows clearly the potential of a program to prompt and support workplace changes, even in the midst of major restructuring. While caution is required in interpreting the Likert scale responses too positively, across the board, in staff, N/MUM manager and N/MUM interviews, it is clear that ‘ttl’ has influenced change at a unit level and proven to be a catalyst for a range of improvement initiatives. The potential next steps are indicated in the recommendations. The major recommendation is that, like most development programs, ‘ttl’ must grow with its constituents and be subject to continuous improvement. 87 Report of the mid program evaluation of ‘take the lead’ 7. REFERENCES Alvarez, K., Salas, E. & Garofano, C. M. (2004) An integrated model of training evaluation and effectiveness. Human Resource Development Review, 3, 385-416. Blume, B. D., Ford, J. K., Baldwin, T. T. & Huang, J. L. (2010) Transfer of training: a meta-analytic review. Journal of Management, 36, 1065-1105. Braithwaite, J. (2004) An empirically-based model for clinician-managers' behavioural routines. Journal of Health Organization and Management, 18, 240-261. Braithwaite, J. & Mannion, R. (forthcoming) Managing change. in Walshe, K. & Smith, J. (Eds.) Healthcare Management. London, Open University Press/McGraw Hill. Brooks, I. (1999) Managerialist professionalism: the destruction of a non-conforming cubculture. British Journal of Management, 10, 41-52. Burke, L. A. & Hutchins, H. M. (2007) Training transfer: an integrative literature review. Human Resource Development Review, 6, 263-296. Care, W. D. & Udod, S. A. (2003) Perceptions of first-line nurse managers. What competencies are needed to fulfill this role? Nursing Leadership Forum, 7 (3), 109115. Carlson, S. (1951) Executive behaviour, Stockholm, Strombergs. Cashin, A. J. & Newman, C. (2010) The evaluation of a 12-month health service manager mentoring program in a corrections environment. Journal for Nurses in Staff Development, 26, 56-63. Chase, L. (1994) Nurse manager competencies. Journal of Nursing Administration, 24, 56-64. Chiok Foong Loke, J. (2001) Leadership behaviours: effects on job satisfaction, productivity and organizational commitment. Journal of Nursing Management, 9, 191-204. Clinical Excellence Commission & NSW Health (2010) Between the flags keeping patients safe. Sydney, Clinical Excellence Commission NSW Health. Colquitt, J. A., LePine, J. A. & Noe, R. A. (2000) Toward an integrative theory of training motivation: a meta-analytic path analysis of 20 years of research. Journal of Applied Psychology, 85, 678-707. 88 Report of the mid program evaluation of ‘take the lead’ Davis, E. (2005) Home study program. Educating perioperative managers about materials and financial management. AORN Journal, 81, 798. Denzin, N. K. (1989) The research act: a theoretical introduction to sociological methods, New York, McGraw Hill. Donaher, K., Russell, G., Scoble, K. B. & Chen, J. (2007) The Human Capital Competencies Inventory for developing nurse managers. Journal of Continuing Education in Nursing, 38, 277-283. Duffield, C. (1991) First-line nurse managers: issues in the literature. Journal of Advanced Nursing, 16, 1247-1253. Duffield, C. (2005) A master class for nursing unit managers: an Australian example. Journal of Nursing Management, 13, 68-73. Duffield, C. & Franks, H. (2001) The role and preparation of first-line nurse managers in Australia: where are we going and how do we get there? Journal of Nursing Management, 9, 87-91. Duffield, C. & O'Brien-Pallas, L. (2002) The nursing workforce in Canada and Australia: two sides of the same coin. Australian Health Review, 25, 136-144. Duffield, C., Roche, M., O'Brien-Pallas, L., Catling-Paull, C. & King, M. (2009) Staff satisfaction and retention and the role of the Nursing Unit Manager. Collegian: Journal of the Royal College of Nursing Australia, 16, 11-17. Duffield, C. M. & Lumby, J. (1994) Context and culture - the influence on role transition for first-line nurse managers. International Journal of Nursing Studies, 31, 555-560. Fayol, H. (1949) General and industrial management, London, Pittman. Ferlie, E. B. & Shortell, S. M. (2001) Improving the quality of health care in the United Kingdom and the United States: a framework for change. Milbank Quarterly, 79, 281315. Flottrop, S. & Oxman, A. D. (2003) Identifying barriers and tailoring interventions to improve the management of urinary tract infections and sore throat: a pragmatic study using qualitative methods. BMC Health Services Research, 3, doi:10.1186/1472-6963-3-3. Garling, P. (2008) Final report of the Special Commission of Inquiry into Acute Care Services in NSW Public Hospitals: overview report, Sydney, State of NSW through the Special Commission of Inquiry: Acute Care Services in New South Wales Public Hospitals. 89 Report of the mid program evaluation of ‘take the lead’ Georgenson, D. L. (1982) The problem of transfer calls for partnership. Training and Development Journal, 36. Gould, D., Kelly, D., Goldstone, L. & Maidwell, A. (2001) The changing training needs of clinical nurse managers: exploring issues for continuing professional development. Journal of Advanced Nursing, 34, 7-17. Greenhalgh, T., Robert, G., Macfarlane, F., Bate, P. & Kyriakidou, O. (2004) Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Quarterly, 82, 581-629. Grimshaw, J., Eccles, M. & Tetroe, J. (2004) Implementing clinical guidelines: Current evidence and future implications. Journal of Continuing Education in the Health Professions, 24, S31-S37. Hawe, S. (2009) "take the lead": etrengthening the Nursing/Midwifery Unit Manager role across NSW. Report phase one: August 2008. Sydney, NSW Department of Health. Hawkins, A., Carter, K. & Nugent, M. (2009) Symposium. Nurse manager orientation. AACN Advanced Critical Care, 20, 55-70. Hayes, L. J., O'Brien-Pallas, L., Duffield, C., Shamian, J., Buchan, J., Hughes, F., Spence Laschinger, H. K., North, N. & Stone, P. W. (2006) Nurse turnover: A literature review. International Journal of Nursing Studies, 43, 237-263. Hillier, F. J. (2005) Managing creative and health production processes : issues, similarities and differences. Sydney, University of New South Wales. Holladay, C. L. & Quiñones, M. A. (2003) Practice variability and transfer of training: the role of self-efficacy generality. Journal of Applied Psychology, 88, 1094-1103. Jennings, B. M., Scalzi, C. C., Rodgers, I. J. D. & Keane, A. (2007) Differentiating nursing leadership and management competencies. Nursing Outlook, 55 (4), 169175. Joyce, P. (2005) Developing a nursing management degree programme to meet the needs of Irish nurse managers. Journal of Nursing Management, 13, 74-82. Karsten, M. A. (2010) Coaching: an effective leadership intervention. Nursing Clinics of North America, 45, 39-48. Kellagher, M., Simpson, J., Flynn, B. & Armstrong, D. (2010) Workload and workforce planning: developing a learning toolkit. Nursing Management, 17, 32-4. Kennedy, R. (2008) 'How do we get the managers we need and the leaders we want?' A personal view. Journal of Nursing Management, 16, 942-5. 90 Report of the mid program evaluation of ‘take the lead’ Kirkpatrick, D. L. & Kirkpatrick, J. D. (2006) Evaluating training programs : the four levels, San Francisco, McGraw Hill. Kleinman, C. S. (2003) Leadership roles, competencies, and education: how prepared are our nurse managers? Journal of Nursing Administration, 33, 451-455. Kotter, J. (1982) The General Manager, New York, Free Press. Kowalski, K. (2004) Growing future leaders: developing perinatal managers from within. JOGNN - Journal of Obstetric, Gynecologic, & Neonatal Nursing, 33, 362-70. Krejci, J. W. & Malin, S. (1997) Impact of leadership development on competencies. Nursing Economics, 15, 235-41. Leimbach, M. (2010) Learning transfer model: a research-driven approach to enhancing learning effectiveness. Industrial and Commercial Training, 42, 81 - 86. Lewis, R., Yarker, J., Donaldson-Feilder, E., Flaxman, P. & Munir, F. (2010) Using a competency-based approach to identify the management behaviours required to manage workplace stress in nursing: a critical incident study. International Journal of Nursing Studies, 47 (3), 307-313. Lin, L.-M., Wu, J.-H., Huang, I.-C., Tseng, K.-H. & Lawler, J. J. (2007) Management development: a study of nurse managerial activities and skills. Journal of Healthcare Management, 52, 156-68; discussion 168-9. Locke, E. A. & Latham, G. P. (2002) Building a practically useful theory of goal setting and task motivation: a 35-year odyssey. American Psychologist, 57, 705-717. MacMillan-Finlayson, S. (2010) Competency development for nurse executives: meeting the challenge. Journal of Nursing Administration, 40, 254-7. MacPhee, M., Jewell, K., Wardrop, A., Ahmed, A. & Mildon, B. (2010) British Columbia's provincial nursing workload project: evidence to empowerment. Nursing Leadership, 23, 54-63. Maguire, M. P., Spencer, K. L. & Sabatier, K. H. (2004) The Nurse Manager Academy: an innovative approach to managerial competency development. Nursing Leadership Forum, 8, 133-7. Mass, H., Brunke, L., Thorne, S. & Parslow, H. G. (2006) Preparing the next generation of senior nursing leaders in Canada: perceptions of role competencies and barriers from the perspectives of inhabitants and aspirants. Nursing leadership, 19, 75-91. McCallin, A. M. & Frankson, C. (2010) The role of the charge nurse manager: A descriptive exploratory study. Journal of Nursing Management, 18, 319-325. 91 Report of the mid program evaluation of ‘take the lead’ McCarthy, G. & Fitzpatrick, J. J. (2009) Development of a competency framework for nurse managers in Ireland. Journal of Continuing Education in Nursing, 40 (8), 346350. McLarty, J. & McCartney, D. (2009) The nurse manager: the neglected middle. Healthcare Financial Management, 63, 74-8. Mintzberg, H. (1971) Managerial work: analysis from observation. Management Science, 18, B97-B110. Nijman, D.-J., J.M., Nijhof, W. J., Wognum, A. A. M. I. & Veldkamp, B. P. (2006) Exploring differential effects of supervisor support on transfer of training. Journal of European Industrial Training, 30, 529 - 549. NSW Department of Health (2009) Caring together: the health action plan for NSW. Sydney, New South Wales Government. NSW Health. "take the lead" - the Nursing/Midwifery Unit Manager Project. North Sydney: NSW Health; 2008. Accessed on: 22 November 2010. Available from:http://www.health.nsw.gov.au/nursing/projects/take_the_lead.asp. NSW Health. Implementation toolkit standard key principles for clinical handover. North Sydney: NSW Department of Health; 2009. Accessed on: 22 November 2010. Available from:http://www.archi.net.au/documents/e-library/qs/clinical/clinicalhandover/implementation-toolkit.pdf. NSW Health. A conceptual framework: the Nursing/Midwifery Unit Manager role. North Sydney: NSW Health; 2010a. Accessed on: 22 November 2010. Available from:http://www.health.nsw.gov.au/resources/nursing/projects/pdf/updated_conc eptual_framework.pdf. NSW Health. Public Health System Nurses' and Midwives' (State) Award. North Sydney: NSW Health; 2010b. Accessed on: 22 November 2010. Available from:http://www.health.nsw.gov.au/resources/jobs/conditions/awards/nurses.asp. NSW Health Nursing and Midwifery Office. Essentials of Care (EOC) program. North Sydney2008. Accessed on: 12 November 2010. Available from:http://www.health.nsw.gov.au/nursing/projects/eoc.asp. NSW Nurses' Association. Nurses support Nurse/Midwife in charge role. Sydney: NSW Nurses' Association; 2009. Accessed on: 31 March 2009. Available from:http://www.nswnurses.asn.au/news/18868.html. O'Donoghue, T. & Punch, K. (2003) Qualitative educational research in action: doing and reflecting, London, Routledge Falmer. 92 Report of the mid program evaluation of ‘take the lead’ Oroviogoicoechea, C. (1996) The clinical nurse manager: a literature review. Journal of Advanced Nursing, 24, 1273-1280. Palarca, C., Johnson, S., Mangelsdorff, A. D. & Finstuen, K. (2008) Building from within: identifying leadership competencies for future navy nurse executives. Nursing Administration Quarterly, 32, 216-25. Pearson, A., Laschinger, H., Porritt, K., Jordan, Z., Tucker, D. & Long, L. (2007) Comprehensive systematic review of evidence on developing and sustaining nursing leadership that fosters a healthy work environment in healthcare. International Journal of Evidence-Based Healthcare, 5, 208-253. Pillay, R. (2009) Perceived competencies of nurse managers: A comparative analysis of the public and private sectors in South Africa. African Journal of Business Management, 3, 495-503. Ponti, M. (2009) Transition from leadership development to succession management. Nursing Administration Quarterly, 33, 125-141. Productivity Commission. Australia’s health workforce: research report. Canberra: Productivity Commission; 2005. Accessed on: 10 October 2010. Quiñones, M. A. (1995) Pretraining context effects: Training assignment as feedback. Journal of Applied Psychology, 80, 226-238. Rosati, L. J. (2009) Nurse managers and the effectiveness of the management training: a quantitative cross-sectional survey study. University of Phoenix. Saks, A. M. (1995) Longitudinal field investigation of the moderating and mediating effects of self-efficacy on the relationship between training and newcomer adjustment. Journal of Applied Psychology, 80, 211—225. Shirey, M. R. (2006) Stress and coping in nurse managers: two decades of research. Nursing Economic$, 24, 193-211. Sprinks, J. (2010) Do ward sisters and charge nurses have the authority to do their job? Nursing Management, 17, 20-22. Stewart, R. (1998) Managerial work, Aldershot, Ashgate. Sutto, N. B., Knoell, M. D., Zucker, K., Finstuen, K. & Mangelsdorff, A. D. (2008) Executive competencies of nurses in the Veterans Health Administration. Military Medicine, 173, 47-53. Taylor, P. J., Russ-Eft, D. F. & Chan, D. W. L. (2005) A meta-analytic review of behavior modeling training. Journal of Applied Psychology, 90, 692-709. 93 Report of the mid program evaluation of ‘take the lead’ Thomas, J. & Herrin, D. (2008) The executive master of science in nursing program: competencies and learning experiences. Journal of Nursing Administration, 38, 4-7. Twigg, D., Duffield, C., Bremner, A., Rapley, P. & Finn, J. ((in press)) The impact of the nursing hours per patient day (NHPPD) staffing method on patient outcomes: A retrospective analysis of patient and staffing data. International Journal of Nursing Studies, In Press, Corrected Proof. 94 Report of the mid program evaluation of ‘take the lead’ 8. APPENDICES 8.1 Evaluation tools 8.1.1 N/MUMs interview schedule Interviews were opened with a scripted introductory statement. The researchers then asked the following questions: In these first questions, I would like to ask you about your overall impressions of the take the lead project. 1. Can you tell me about how your participation in the ‘ttl’ workshops came about? 2. Can you tell me about your experience of participating in the ‘ttl’ program? 3. Has participating in the ‘ttl’ program been useful to you in your role as a N/MUM? 4. Have you made any changes in your unit as a result of your participation in the ‘ttl’ program? a. If they answer yes ask: Can you please describe them? b. If they answer no ask: If you have not made any changes, could you tell me why? 5. Were the changes implemented successfully? a. What helped implement the change successfully ? b. Have some changes been easier to make than others? Why do you think this is so? 6. Have the changes you have implemented so far proven to be sustainable? Why do you think this is so? 7. What changes would you have liked to have made but have been unable to implement? 8. Can you tell me about any specific skills that you developed as a result of taking part in ttl? a. How has your participation in the ‘ttl’ program affected how you go about your day to day work in your unit? 9. Do you think that taking part in ‘ttl’ has changed your job performance? How? 95 Report of the mid program evaluation of ‘take the lead’ a. Has it changed the way you manage your staff? How? b. Has it changed the way you respond to the needs of patients? How? c. Has taking part in ‘ttl’ led to any changes in the type of work you do? Can you please tell me about them? d. Has your participation resulted in any changes to the type of work your team does? Can you please tell me about them? 10. Following each statement that I am about to make, I would like you to respond by answering, on a scale of one to five. Please give your immediate response. Thinking about your unit since you did the ‘ttl’ modules: Script Have the number of adverse events in your unit: one ‘increased significantly’, two ‘increased somewhat’, three ‘stayed the same’, four ‘decreased somewhat’ or five ‘decreased significantly’? Has staff satisfaction: one ‘increased significantly’, two ‘increased somewhat’, three ‘stayed the same’, four ‘decreased somewhat’ or five ‘decreased significantly’? Has staff retention: one ‘increased significantly’, two ‘increased somewhat’, three ‘stayed the same’, four ‘decreased somewhat’ or five ‘decreased significantly’? Has staff absenteeism: one ‘increased significantly’, two ‘increased somewhat’, three ‘stayed the same’, four ‘decreased somewhat’ or five ‘decreased significantly’? Has patient satisfaction: one ‘increased significantly’, two ‘increased somewhat’, three ‘stayed the same’, four ‘decreased somewhat’ or five ‘decreased significantly’? Have the number of patient complaints: one ‘increased significantly’, two ‘increased somewhat’, three ‘stayed the same’, four ‘decreased somewhat’ or five ‘decreased significantly’? Have the number of patient compliments: one ‘increased significantly’, two ‘increased somewhat’, three ‘stayed the same’, four ‘decreased somewhat’ or five ‘decreased significantly’? 96 Answer (circle) 1: Increased significantly 2: Increased somewhat 3: Stayed the same 4: Decreased somewhat 5: Decreased significantly 1: Increased significantly 2: Increased somewhat 3: Stayed the same 4: Decreased somewhat 5: Decreased significantly 1: Increased significantly 2: Increased somewhat 3: Stayed the same 4: Decreased somewhat 5: Decreased significantly 1: Increased significantly 2: Increased somewhat 3: Stayed the same 4: Decreased somewhat 5: Decreased significantly 1: Increased significantly 2: Increased somewhat 3: Stayed the same 4: Decreased somewhat 5: Decreased significantly 1: Increased significantly 2: Increased somewhat 3: Stayed the same 4: Decreased somewhat 5: Decreased significantly 1: Increased significantly 2: Increased somewhat 3: Stayed the same 4: Decreased somewhat 5: Decreased significantly Report of the mid program evaluation of ‘take the lead’ Script Has the amount of time you spend on administrative tasks: one ‘increased significantly’, two ‘increased somewhat’, three ‘stayed the same’, four ‘decreased somewhat’ or five ‘decreased significantly’? Answer (circle) 1: Increased significantly 2: Increased somewhat 3: Stayed the same 4: Decreased somewhat 5: Decreased significantly a. Can you attribute any of these changes to your participation in ‘ttl’ (if they can’t remember, the modules were critical communication; lean thinking and leadership; financial management; rostering for patient care). How and why? b. If you have made changes to the way you manage adverse events, staff, patient complaints or administrative tasks as a result of your participation in ‘ttl’ have you evaluated any of the changes? If so, can you tell me about the findings? 11. Following each statement that I am about to make, I would like you to respond by answering, on a scale of one to five. Please give your immediate response. Please note the scale has changed. Thinking about your unit since you did the ttl modules has: Script Your unit’s performance: one ‘improved significantly’, two ‘improved somewhat’, three ‘stayed the same’, four ‘worsened somewhat’ or five ‘worsened significantly’? Your unit’s overall efficiency: one ‘improved significantly’, two ‘improved somewhat’, three ‘stayed the same’, four ‘worsened somewhat’ or five ‘worsened significantly’? Patient flow: one ‘improved significantly’, two ‘improved somewhat’, three ‘stayed the same’, four ‘worsened somewhat’ or five ‘worsened significantly’? Staff performance: one ‘improved significantly’, two ‘improved somewhat’, three ‘stayed the same’, four ‘worsened somewhat’ or five ‘worsened significantly’? 97 Answer (circle) 1: Improved significantly 2: Improved somewhat 3: Stayed the same 4: Worsened somewhat 5: Worsened significantly 1: Improved significantly 2: Improved somewhat 3: Stayed the same 4: Worsened somewhat 5: Worsened significantly 1: Improved significantly 2: Improved somewhat 3: Stayed the same 4: Worsened somewhat 5: Worsened significantly 1: Improved significantly 2: Improved somewhat 3: Stayed the same 4: Worsened somewhat 5: Worsened significantly Report of the mid program evaluation of ‘take the lead’ Script Staff morale: one ‘improved significantly’, two ‘improved somewhat’, three ‘stayed the same’, four ‘worsened somewhat’ or five ‘worsened significantly’? Answer (circle) 1: Improved significantly 2: Improved somewhat 3: Stayed the same 4: Worsened somewhat 5: Worsened significantly a. Can you attribute any of these changes to your participation in ‘ttl’ (if they can’t remember, the modules were critical communication; lean thinking and leadership; financial management; rostering for patient care). How and why? b. If you have made changes to the way you manage adverse events, staff, patient complaints or administrative tasks as a result of your participation in ‘ttl’ have you evaluated any of the changes? If so, can you tell me about the findings? 12. Following each statement that I am about to make, I would like you to respond by answering, on a scale of one to five. Please give your immediate response. Please note the scale has changed. Thinking about you since you did the ttl modules has: Script Your overall job performance: one ‘improved significantly’, two ‘improved somewhat’, three ‘stayed the same’, four ‘worsened somewhat’ or five ‘worsened significantly’? Your ability to communicate with staff: one ‘improved significantly’, two ‘improved somewhat’, three ‘stayed the same’, four ‘worsened somewhat’ or five ‘worsened significantly’? Your ability to communicate with patients and their families: one ‘improved significantly’, two ‘improved somewhat’, three ‘stayed the same’, four ‘worsened somewhat’ or five ‘worsened significantly’? Your ability to communicate with other (non-nursing) staff: one ‘improved significantly’, two ‘improved somewhat’, three ‘stayed the same’, four ‘worsened somewhat’ or five ‘worsened significantly’? Your ability to manage difficult situations: one ‘improved significantly’, two ‘improved somewhat’, three ‘stayed the 98 Answer (circle) 1: Improved significantly 2: Improved somewhat 3: Stayed the same 4: Worsened somewhat 5: Worsened significantly 1: Improved significantly 2: Improved somewhat 3: Stayed the same 4: Worsened somewhat 5: Worsened significantly 1: Improved significantly 2: Improved somewhat 3: Stayed the same 4: Worsened somewhat 5: Worsened significantly 1: Improved significantly 2: Improved somewhat 3: Stayed the same 4: Worsened somewhat 5: Worsened significantly 1: Improved significantly 2: Improved somewhat Report of the mid program evaluation of ‘take the lead’ Script same’, four ‘worsened somewhat’ or five ‘worsened significantly’? Your ability to manage staff: one ‘improved significantly’, two ‘improved somewhat’, three ‘stayed the same’, four ‘worsened somewhat’ or five ‘worsened significantly’? Your ability to negotiate: one ‘improved significantly’, two ‘improved somewhat’, three ‘stayed the same’, four ‘worsened somewhat’ or five ‘worsened significantly’? Your ability to lead: one ‘improved significantly’, two ‘improved somewhat’, three ‘stayed the same’, four ‘worsened somewhat’ or five ‘worsened significantly’? Your ability to solve problems: one ‘improved significantly’, two ‘improved somewhat’, three ‘stayed the same’, four ‘worsened somewhat’ or five ‘worsened significantly’? Your ability to manage the finances and resources of your unit: one ‘improved significantly’, two ‘improved somewhat’, three ‘stayed the same’, four ‘worsened somewhat’ or five ‘worsened significantly’? Your ability to manage the rostering of staff: one ‘improved significantly’, two ‘improved somewhat’, three ‘stayed the same’, four ‘worsened somewhat’ or five ‘worsened significantly’? Has your ability to implement the principles of lean thinking: one ‘increased significantly’, two ‘increased somewhat’, three ‘stayed the same’, four ‘decreased somewhat’ or five ‘decreased significantly’? Answer (circle) 3: Stayed the same 4: Worsened somewhat 5: Worsened significantly 1: Improved significantly 2: Improved somewhat 3: Stayed the same 4: Worsened somewhat 5: Worsened significantly 1: Improved significantly 2: Improved somewhat 3: Stayed the same 4: Worsened somewhat 5: Worsened significantly 1: Improved significantly 2: Improved somewhat 3: Stayed the same 4: Worsened somewhat 5: Worsened significantly 1: Improved significantly 2: Improved somewhat 3: Stayed the same 4: Worsened somewhat 5: Worsened significantly 1: Improved significantly 2: Improved somewhat 3: Stayed the same 4: Worsened somewhat 5: Worsened significantly 1: Improved significantly 2: Improved somewhat 3: Stayed the same 4: Worsened somewhat 5: Worsened significantly 1: Improved significantly 2: Improved somewhat 3: Stayed the same 4: Worsened somewhat 5: Worsened significantly a. Can you attribute any of these changes to your participation in ‘ttl’. How and why? b. If you have made changes to the way you manage adverse events, staff, patient complaints or administrative tasks as a result of your participation in ‘ttl’ have you evaluated any of the changes? If so, can you tell me about the findings? 99 Report of the mid program evaluation of ‘take the lead’ 13. Has a CSO been allocated to assist you in your role? YES/NO a. When did the CSO begin their work? b. Does the CSO report directly to you? If not, then to whom do they report? Is this satisfactory from your perspective? c. What are their typical hours of duty? d. Were you involved in their recruitment? Do they have a position description? (can you send us their duty statement?) Is it based on the one issued by NSW Health? e. Who allocates their duties and tasks (you, centrally allocated) f. Do their duties involve: Data entry and reporting (rosters, HR) Yes No Workforce matters (rostering, recruitment, leave, payroll) Yes No Resource management Yes No Documentation/records management Yes No General administrative activities Yes No Are there any other duties they undertake? g. Has the employment of the CSO had any impact on the type or amount of work you undertake? h. Has the employment of the CSO affected the amount of time you spend on administrative tasks? If not, why not? If so, how? i. From your perspective, what has been the impact of the introduction of the CSO’s role on the work of other members of the clinical team ie doctors, nurses, allied health? j. Do you think there has there been any impact on patient care as a result of the introduction of the CSOs role? k. Have there been any unexpected outcomes/impacts as a result of the introduction of the CSO’s position? l. Please describe how the role of the CSO can be changed to further support you in your work and more specifically in successfully implementing change? 100 Report of the mid program evaluation of ‘take the lead’ 14. Has your unit has participated in the Essentials of Care program? Yes/No a. Can you tell me about changes in your practice that are a result of your participation in the ‘ttl’ program and those that are due to your unit’s participation in the Essentials of Care program? b. Can you tell me about any other improvements you have implemented which are in line with relevant recommendations in Caring Together? 15. Have you read the Conceptual Framework for the Nursing/Midwifery Unit Manager Role? Yes/ No 16. Do you feel it accurately represents the purpose, capabilities and core functions of the N/MUM’s role? Could you tell me more? 17. Has your participation in ‘ttl’ led to a strengthening of your role as a N/MUM? How? 18. Has your participation in ‘ttl’ led to any identifiable improvements in patient care and flow? How? 19. Has your participation in ‘ttl’ led to a reduction in errors in your unit? By what percentage? Ho 20. Has your participation in ‘ttl’ changed the way you feel about being a N/MUM? If so how? 21. Is there anything else you would like to say? 101 Report of the mid program evaluation of ‘take the lead’ 8.1.2 N/MUMs’ manager interview schedule How many N/MUMs report to you? _____________________________________ What level are the N/MUMs who report to you? __________________________ In these first questions, I would like to ask you about your overall impressions of the take the lead project. 1. Can you tell me what you know about the ‘ttl’ program? 2. Have any of your N/MUMs participated in ‘ttl’? a. Have you participated in ‘ttl’? 3. Do you know of any changes that your N/MUMs have made as result of their participation in the ‘ttl’ program? a. If they answer YES ask: Can you please describe them and were they successful? b. If they answer NO ask: If they have not made any changes, could you tell me why you think they have not made any changes? 4. What do you think helped your or your N/MUMs implement the change successfully (Prompt: management support, staff support, other N/MUMS, resources). Has/have the NUM/s discussed any particular enablers or barriers to implementing changes? 5. Have the changes implemented so far proven to be sustainable? Why do you think this is so? 6. Can you tell me about any specific skills that you saw your N/MUMS develop as a result of taking part in ‘ttl’? a. Do you think your N/MUMS participation in ‘ttl’ program has affected how they go about their day to day work of their units? b. Do you think that your N/MUMs participation in ttl has affected YOUR work? If so how? 7. Following each statement that I am about to make, I would like you to respond by answering, on a scale of one to five. Please give your immediate response. Thinking about units where the N/MUMs have undertaken the ‘ttl’ modules has: 102 Report of the mid program evaluation of ‘take the lead’ Script Have the number of adverse events: one ‘increased significantly’, two ‘increased somewhat’, three ‘stayed the same’, four ‘decreased somewhat’ or five ‘decreased significantly’? Is this attributable to ‘ttl’? How has this change been measured? Has staff satisfaction: one ‘increased significantly’, two ‘increased somewhat’, three ‘stayed the same’, four ‘decreased somewhat’ or five ‘decreased significantly’? Is this attributable to ‘ttl’? How has this change been measured? Has staff retention: one ‘increased significantly’, two ‘increased somewhat’, three ‘stayed the same’, four ‘decreased somewhat’ or five ‘decreased significantly’? Is this attributable to ‘ttl’? How has this change been measured? Has staff absenteeism: one ‘increased significantly’, two ‘increased somewhat’, three ‘stayed the same’, four ‘decreased somewhat’ or five ‘decreased significantly’? Is this attributable to ‘ttl’? How has this change been measured? Has patient satisfaction: one ‘increased significantly’, two ‘increased somewhat’, three ‘stayed the same’, four ‘decreased somewhat’ or five ‘decreased significantly’? Is this attributable to ‘ttl’? How has this change been measured? Have the number of patient complaints: one ‘increased significantly’, two ‘increased somewhat’, three ‘stayed the same’, four ‘decreased somewhat’ or five ‘decreased significantly’? Is this attributable to ‘ttl’? How has this change been measured? Have the number of patient compliments: one ‘increased significantly’, two ‘increased somewhat’, three ‘stayed the same’, four ‘decreased somewhat’ or five ‘decreased significantly’? Is this attributable to ‘ttl’? How has this change been measured? Has the amount of time the N/MUMS spend on administrative tasks: one ‘increased significantly’, two ‘increased somewhat’, three ‘stayed the same’, four ‘decreased somewhat’ or five ‘decreased significantly’? 103 Answer (circle) 1: Increased significantly 2: Increased somewhat 3: Stayed the same 4: Decreased somewhat 5: Decreased significantly 1: Increased significantly 2: Increased somewhat 3: Stayed the same 4: Decreased somewhat 5: Decreased significantly 1: Increased significantly 2: Increased somewhat 3: Stayed the same 4: Decreased somewhat 5: Decreased significantly 1: Increased significantly 2: Increased somewhat 3: Stayed the same 4: Decreased somewhat 5: Decreased significantly 1: Increased significantly 2: Increased somewhat 3: Stayed the same 4: Decreased somewhat 5: Decreased significantly 1: Increased significantly 2: Increased somewhat 3: Stayed the same 4: Decreased somewhat 5: Decreased significantly 1: Increased significantly 2: Increased somewhat 3: Stayed the same 4: Decreased somewhat 5: Decreased significantly 1: Increased significantly 2: Increased somewhat 3: Stayed the same 4: Decreased somewhat Report of the mid program evaluation of ‘take the lead’ Script Answer (circle) 5: Decreased significantly Is this attributable to ‘ttl’? How has this change been measured? 8. Following each statement that I am about to make, I would like you to respond by answering, on a scale of one to five. Please give your immediate response. Please note the scale has changed. Thinking about units where the N/MUMs have undertaken the ‘ttl’ modules has: Script The unit(s) performance: one ‘improved significantly’, two ‘improved somewhat’, three ‘stayed the same’, four ‘worsened somewhat’ or five ‘worsened significantly’? Is this attributable to ‘ttl’? How has this change been measured? The unit’s overall efficiency: one ‘improved significantly’, two ‘improved somewhat’, three ‘stayed the same’, four ‘worsened somewhat’ or five ‘worsened significantly’? Is this attributable to ‘ttl’? How has this change been measured? Patient flow: one ‘improved significantly’, two ‘improved somewhat’, three ‘stayed the same’, four ‘worsened somewhat’ or five ‘worsened significantly’? Is this attributable to ‘ttl’? How has this change been measured? Staff performance: one ‘improved significantly’, two ‘improved somewhat’, three ‘stayed the same’, four ‘worsened somewhat’ or five ‘worsened significantly’? Is this attributable to ‘ttl’? How has this change been measured? Staff morale: one ‘improved significantly’, two ‘improved somewhat’, three ‘stayed the same’, four ‘worsened somewhat’ or five ‘worsened significantly’? Is this attributable to ‘ttl’? How has this change been measured? 104 Answer (circle) 1: Improved significantly 2: Improved somewhat 3: Stayed the same 4: Worsened somewhat 5: Worsened significantly 1: Improved significantly 2: Improved somewhat 3: Stayed the same 4: Worsened somewhat 5: Worsened significantly 1: Improved significantly 2: Improved somewhat 3: Stayed the same 4: Worsened somewhat 5: Worsened significantly 1: Improved significantly 2: Improved somewhat 3: Stayed the same 4: Worsened somewhat 5: Worsened significantly 1: Improved significantly 2: Improved somewhat 3: Stayed the same 4: Worsened somewhat 5: Worsened significantly Report of the mid program evaluation of ‘take the lead’ 9. Following each statement that I am about to make, I would like you to respond by answering, on a scale of one to five. Please give your immediate response. Thinking about units where the N/MUMs have undertaken the ‘ttl’ modules has: Script Their overall job performance: one ‘improved significantly’, two ‘improved somewhat’, three ‘stayed the same’, four ‘worsened somewhat’ or five ‘worsened significantly’? Is this attributable to ‘ttl’? How has this change been measured? Their ability to communicate with staff: one ‘improved significantly’, two ‘improved somewhat’, three ‘stayed the same’, four ‘worsened somewhat’ or five ‘worsened significantly’? Answer (circle) 1: Improved significantly 2: Improved somewhat 3: Stayed the same 4: Worsened somewhat 5: Worsened significantly 1: Improved significantly 2: Improved somewhat 3: Stayed the same 4: Worsened somewhat 5: Worsened significantly Is this attributable to ‘ttl’? How has this change been measured? Their ability to communicate with patients and their families: one ‘improved significantly’, two ‘improved somewhat’, three ‘stayed the same’, four ‘worsened somewhat’ or five ‘worsened significantly’? 1: Improved significantly 2: Improved somewhat 3: Stayed the same 4: Worsened somewhat 5: Worsened significantly Is this attributable to ‘ttl’? How has this change been measured? Their ability to communicate with other (non-nursing) staff: one ‘improved significantly’, two ‘improved somewhat’, three ‘stayed the same’, four ‘worsened somewhat’ or five ‘worsened significantly’? 1: Improved significantly 2: Improved somewhat 3: Stayed the same 4: Worsened somewhat 5: Worsened significantly Is this attributable to ‘ttl’? How has this change been measured? Their ability to manage difficult situations: one ‘improved significantly’, two ‘improved somewhat’, three ‘stayed the same’, four ‘worsened somewhat’ or five ‘worsened significantly’? 1: Improved significantly 2: Improved somewhat 3: Stayed the same 4: Worsened somewhat 5: Worsened significantly Is this attributable to ‘ttl’? How has this change been measured? Their ability to manage staff: one ‘improved significantly’, two ‘improved somewhat’, three ‘stayed the same’, four ‘worsened somewhat’ or five ‘worsened significantly’? Is this attributable to ‘ttl’? How has this change been measured? 105 1: Improved significantly 2: Improved somewhat 3: Stayed the same 4: Worsened somewhat 5: Worsened significantly Report of the mid program evaluation of ‘take the lead’ Script Their ability to negotiate: one ‘improved significantly’, two ‘improved somewhat’, three ‘stayed the same’, four ‘worsened somewhat’ or five ‘worsened significantly’? Is this attributable to ‘ttl’? How has this change been measured? Their ability to lead: one ‘improved significantly’, two ‘improved somewhat’, three ‘stayed the same’, four ‘worsened somewhat’ or five ‘worsened significantly’? Is this attributable to ‘ttl’? How has this change been measured? Their ability to solve problems: one ‘improved significantly’, two ‘improved somewhat’, three ‘stayed the same’, four ‘worsened somewhat’ or five ‘worsened significantly’? Is this attributable to ‘ttl’? How has this change been measured? Their ability to manage the finances and resources of the unit: one ‘improved significantly’, two ‘improved somewhat’, three ‘stayed the same’, four ‘worsened somewhat’ or five ‘worsened significantly’? Answer (circle) 1: Improved significantly 2: Improved somewhat 3: Stayed the same 4: Worsened somewhat 5: Worsened significantly 1: Improved significantly 2: Improved somewhat 3: Stayed the same 4: Worsened somewhat 5: Worsened significantly 1: Improved significantly 2: Improved somewhat 3: Stayed the same 4: Worsened somewhat 5: Worsened significantly 1: Improved significantly 2: Improved somewhat 3: Stayed the same 4: Worsened somewhat 5: Worsened significantly Is this attributable to ‘ttl’? How has this change been measured? Their ability to manage the rostering of staff: one ‘improved significantly’, two ‘improved somewhat’, three ‘stayed the same’, four ‘worsened somewhat’ or five ‘worsened significantly’? 1: Improved significantly 2: Improved somewhat 3: Stayed the same 4: Worsened somewhat 5: Worsened significantly Is this attributable to ‘ttl’? How has this change been measured? Their ability to implement the principles of lean thinking: one ‘increased significantly’, two ‘increased somewhat’, three ‘stayed the same’, four ‘decreased somewhat’ or five ‘decreased significantly’? 1: Improved significantly 2: Improved somewhat 3: Stayed the same 4: Worsened somewhat 5: Worsened significantly Is this attributable to ‘ttl’? How has this change been measured? 10. Have you noticed any differences in these areas between N/MUMs who have and those who haven’t completed ‘ttl’? 11. Have you employed CSOs in your service? If so, how many? a. When did the CSOs begin their work? 106 Report of the mid program evaluation of ‘take the lead’ b. To whom does the CSO report? Is this satisfactory from your perspective? c. Who allocates their duties and tasks (you, centrally allocated) d. Do you think the employment of the CSO had any impact on the type or amount of work your N/MUMs undertake? e. Has the employment of the CSO affected the amount of time your N/MUMs spend on administrative tasks? f. From your perspective, what has been the impact of the introduction of the CSO’s role on the work of other members of the clinical team ie doctors, nurses, allied health? g. Do you think there has there been any impact on patient care as a result of the introduction of the CSOs role? h. Have there been any unexpected outcomes/impacts as a result of the introduction of the CSO’s position? i. Please describe how the role of the CSO can be changed to further support you in your N/MUMs and more specifically in successfully implementing change? j. Was the N/MUM with whom the CSO works involved in the selection process of the CSO? 12. Has your service participated in the Essentials of Care program? Yes/No a. We are trying to tease out whether changes that your N/MUMs have made are due to their participation in ‘ttl’ or their unit’s participation in the Essentials of Care program b. Can you tell me about any other improvements your N/MUMs have implemented which are in line with relevant recommendations in Caring Together? 13. Do you feel that the Conceptual Framework for the Nursing/Midwifery Unit Manager Role accurately represents the purpose, capabilities and core functions of the N/MUM’s role? 14. Has the participation of your N/MUMs in ‘ttl’ led to a strengthening and developing of their role as a N/MUM? How? 107 Report of the mid program evaluation of ‘take the lead’ 15. Has their participation in ‘ttl’ led to a reduction in errors? By what percentage? How? 16. Would it be possible for our team to examine your IIMS and complaints data pre and post your N/MUMS having undertaken ‘ttl’? 17. Has their participation in ‘ttl’ led to any savings in terms of resources or costs? If so how much? 18. If you participated in ‘ttl’ can you reflect on your experiences as a result of your participation? 19. Is there anything else you would like to say? 108 Report of the mid program evaluation of ‘take the lead’ 8.1.3 Staff survey questionnaire Demographics 1. Are you male or female? 2. What is your age? 3. In which Area Health Service do you primarily work? Greater Southern AHS Greater Western AHS Hunter New England AHS North Coast AHS North Sydney Central Coast AHS South Eastern Sydney Illawarra AHS Sydney South West AHS Sydney West AHS Children’s Hospital Westmead Ambulance Services NSW Justice Health 4. What is your professional background? Medicine Nursing Allied Health (please specify) Other (please specify) 5. How many years have you worked in health care post-graduation? (since you gained your initial qualification) 6. Where do you do most of your work? Tertiary referral hospital Regional hospital Rural health facility Community Health Centre Area Health Service (Office) 109 Report of the mid program evaluation of ‘take the lead’ Ambulance service Justice Health Other (please specify) 7. How many years have you worked in health care post-graduation? (since you gained your initial qualification) 8. Where do you do most of your work? Tertiary referral hospital Regional hospital Rural health facility Community Health Centre Area Health Service (Office) Ambulance service Justice Health Other (please specify) 9. What is your current position in your organisation? Please specify: Questionnaire 1. Have the any of the N/MUMs with whom you work completed the ‘ttl’ program? Facilitating Critical Communication Yes/No/Don’t know Lean Thinking and Leadership Yes/No/Don’t know Financial Management Yes/No/Don’t know Rostering for Patient Care Yes/No/Don’t know Leadership – making it happen Yes/No/Don’t know a. Thinking about the N/MUM’s you work with and in your personal opinion: Have any of the N/MUMs implemented changes to the way their unit operates as a result of their attendance at these courses? Yes/No/Don’t know b. If they have made one or more changes, could you please describe at least one change? 110 Report of the mid program evaluation of ‘take the lead’ c. Do you think these changes benefited the unit? Yes/No/Don’t know 2. Is your unit or service participating in the Essentials of Care Program? Yes/No/Don’t know a. Can you briefly describe what this participation has involved? 3. Do you think that your N/MUM’s ability to manage the unit has changed? Yes/No/Don’t know a. Do you think your N/NUM’s work practices have changed? Yes/No/Don’t know b. Has this led to any changes in your work practices? Yes/No/Don’t know c. Could you please give us one example of how you think your unit’s performance has changed as a result of changes made by your M/NUM? Yes/No/Don’t know d. Have the changes in your N/MUMs work practices led to any changes in how your team works? Yes/No/Don’t know e. Has your unit’s performance changed as a result of changes in your M/NUMs work practices? (eg management of resources, efficiency, financial performance, error rates) Yes/No/Don’t know f. Could you please give us one example of how you think your unit’s performance has changed as a result of changes made by your N/MUM? g. What type of impact do you think that any changes made to work practices by your N/MUM over the last year have had on patients? (eg patient satisfaction, complaints and compliments, patient centred care) 4. Think about a specific change to work practices which you N/MUM has attempted to implement over the last year. Were they successful in doing so? Yes/No/Don’t know a. Briefly describe the change the N/MUM tried to implement b. Why do you think your N/MUM was successful or unsuccessful in implementing this change? c. How did you, as a staff member, measure the effect of the change your unit? 111 Report of the mid program evaluation of ‘take the lead’ 5. Thinking about your unit over the last year (or as long as you have been at the unit) please rate each statement on the following scale, for example: “The number of days leave taken has decreased significantly” (Presented as a Likert scale with radio buttons) Have the number of adverse events changed? Has staff satisfaction changed? Has staff retention changed? Has staff absenteeism changed? Has the proportion of your N/MUMs’ time spent on transactional administrative tasks changed? a. In your opinion in what way, if any, are these changes attributable to your N/MUM(s) participation in the ‘take the lead’ program? 6. Thinking about your unit over the last year (or as long as you have been at the unit) please rate each statement on the following scale, for example: (Presented as a Likert scale with radio buttons) Has your unit’s performance overall changed? Has your unit’s efficiency overall changed? Has patient flow has changed? Has staff performance changed? Has staff morale changed? Has the communication and the management of difficult situations between the N/MUM and staff changed? Has patient satisfaction has changed? Has the financial management of your unit changed? a. In your opinion in what way, if any, are these changes attributable to your N/MUM(s) participation in the ‘take the lead’ program? 7. What do you think will assist N/MUMs (including future N/MUMs) to be able to identify and successfully implement needed changes to work practices? Yes/No/Don’t know 112 Report of the mid program evaluation of ‘take the lead’ 8. Do you have Clinical Support Officer (CSO) working in your unit(s)? a. Does the CSO contribute to your work? Yes/No/Don’t know b. Has the employment of the CSO affected the amount of time your N/MUM spends on administrative tasks? c. Do you think there has there been any impact to patient care as a result of the introduction of the CSO role? d. If yes, how? If not, why not? e. Have there been any unexpected outcomes/impacts as a result of the introduction of the CSO? Yes/No/Don’t know f. If yes, how? If not, why not? g. Has anything hindered the CSO’s ability to support your or your N/MUM’s work? h. If yes, how? If not, why not? 9. NSW Health is interested in supporting and developing the role of N/MUMs. 10. Is there anything else you would like to add about the role of CSOs? 11. Is there anything else you would like to add in general? 113 Report of the mid program evaluation of ‘take the lead’ 8.1.4 CSO survey Demographics 1. Are you male or female? 2. What is your age? 3. In which Area Health Service do you primarily work? Greater Southern AHS Greater Western AHS Hunter New England AHS North Coast AHS North Sydney Central Coast AHS South Eastern Sydney Illawarra AHS Sydney South West AHS Sydney West AHS Children’s Hospital Westmead Ambulance Services NSW Justice Health 4. What is your professional background? Clerical Other (please speciy) 5. What is your highest qualification? Year 12 or certificate II Certificate III Certificate IV Diploma Advanced Diploma Bachelor Degree Other (please specify) 6. Please specify the title of your highest qualification. 7. How many years have you worked in health care? 114 Report of the mid program evaluation of ‘take the lead’ Questionnaire 8. How long have you worked in the role of CSO? Less than one year One year Two years More than two years 9. Are you allocated to a single or multiple ward/area/services? a. Which one(s)? 10. How long have you worked in your current position? 11. What role did you have prior to coming into this position? a. To whom do you report? (please use position titles only and not individuals’ names) b. Is this satisfactory from a work perspective? (Yes/No) c. Can you please describe why this arrangement is satisfactory or unsatisfactory? 12. What are your typical hours of duty? Less than five hours 5-10 hours 10-15 hours 15-20 hours 20-25 hours 25-30 hours 30-35 hours 35-40 hours More than 40 hours a. On which days of the week do you typically work? Monday Tuesday Wednesday Thursday 115 Report of the mid program evaluation of ‘take the lead’ Friday Saturday Sunday b. Do you work outside of office hours? If so, when do you typically work these hours (eg Sunday 4pm to 8pm)? 13. On average what percentage of your time do you spend each week working with or for the following people/groups? The N/MUM(s) of your unit(s): _____% Other N/MUMS (or senior nursing staff): _____% Medical staff: _____% Nursing staff: _____% Allied health: _____% Other (please specify): _____% 14. What are your typical duties/tasks? 15. Please indicate which of the following are part of your roles and responsibilities (indicate as many as you wish) Data entry and reporting Data entry for ward/unit rosters into relevant IT system Updating the roster in line with any approved changes ie sick leave etc Entering information onto HR IT system once approved Entering information onto HR IT system once approved Data entry activities that relate to patient care activities and support any member of the health care team Registering births to the NSW Registry of Births, Deaths and Marriages Assisting the N/NUM in producing reports on finance and quality parameters/indicators Other, please specify: What percentage of your time (on a weekly basis) do you spend on data entry and reporting? : _____% 116 Report of the mid program evaluation of ‘take the lead’ Workforce matters Rostering Recruitment Leave Payroll Liaising with Health Support Services to clarify pay and leave enquiries Providing support for the recruitment of staff to the ward/unit Undertaking administrative activities related to the management of performance reviews for staff that the N/MUM and other ward based medical and allied health staff line manage within the unit Assisting with the replacement of staff as directed by the N/MUM Other, please specify: What percentage of your time (on a weekly basis) do you spend on workforce matters?: _____% Resource management Ensuring the ward/unit has adequate stock of medical supplies and equipment required by staff to perform their day to day duties in delivery of patient care. Purchasing and receiving new equipment for the ward/unit and equipment maintenance. Uniform ordering Other, please specify: What percentage of your time (on a weekly basis) do you spend on resource management? : _____% Documentation/records management Supporting and participating in the administrative aspects of activities Numerical profiling Quality accreditation processes Incident management Maintaining staff credentialing register Monitoring of nurses and midwives registration and enrolment 117 Report of the mid program evaluation of ‘take the lead’ Assisting the health care team in obtaining information, reports or correspondence related to patient care What percentage of your time (on a weekly basis) do you spend on documentation/records management? :_____% General administration activities Undertaking administrative tasks related to meetings that are held on the ward/unit involving medical, nursing and allied health staff including Scheduling Ensuring all relevant documents are available for the meeting Progression of action items where appropriate Assisting with the daily schedule for the health care team at ward/unit level Ensuring that multidisciplinary ward rounds are completed in a timely manner Ensuring relevant material is available to support the ward round Organising travel and accommodation for ward/unit staff where required Other general administrative tasks to support (please specify): What percentage of your time (on a weekly basis) do you spend on resource management? : _____% Any other tasks (please specify) What percentage of your time (on a weekly basis) do you spend on other tasks? : _____% 16. If you have access to your job description could you please upload it now? We are only interested in the scope of scope of tasks and duties across all CSOs and not in individuals. All information will be de-identified 17. Do you feel your job/position description accurately represents the purpose, capabilities and core functions of your role? Yes/No, if no, why not? 18. Has your role changed since you were first employed as a CSO? If so how? 19. Were you actively involved in the deciding how your role was to change? Can you describe how you were involved? Yes/No 20. Have you taken over tasks/duties that were once undertaken by the N/MUM? Yes/No 118 Report of the mid program evaluation of ‘take the lead’ 21. Can you briefly list the tasks that you now do, that were once undertaken by the M/NUM? 22. Can you briefly describe any tasks that you now do, that you know were once undertaken by other members of staff (e.g. doctors, allied health professionals, nurses)? 23. Are you undertaking activities/tasks allocated from somewhere other than the unit ward within which you work? (e.g. are you undertaking centralised rostering?) a. Can you briefly list the tasks that are allocated from outside your unit and who allocates them? b. How much of your time, on a weekly basis, is taken up by tasks allocated from outside your unit? 24. What type of tasks do you undertake that specifically support N/MUM(s)? 25. Do you think that the introduction of your role has reduced the amount of time your N/MUM spend on administrative tasks? Yes/No a. What type of tasks do you undertake that specifically support the doctors’ work? b. What type of tasks do you undertake that specifically support the nurses’ work? c. What impact do you think the introduction of your role on the allied health professionals’ work? (eg physiotherapists, psychologists, social workers, pharmacists etc) d. What impact do you think the introduction of your role on the work of other staff ?(please specify which staff) 26. Do you think there has there been any impact on patient care as a result of the introduction of your role? Yes/No 27. What type of impact? 28. From your perspective there been any unexpected outcomes/impacts as a result of the introduction of your role? Yes/No a. Can you please describe these? 119 Report of the mid program evaluation of ‘take the lead’ 29. What, if anything, helps or hinders your ability to support your unit’s work? 30. Is your unit participating in the Essentials of Care Program? Yes/No/Don’t know 31. Can you briefly describe what this participation has involved? 32. Thinking about your unit over the last year (or as long as you have been at the unit) please rate each statement: (Presented as a Likert scale with radio buttons) Number of adverse events Staff satisfaction Patient satisfaction Staff retention Staff absenteeism Number of patient complaints Number of patient compliments 33. Thinking about your unit over the last year (or as long as you have been at the unit) please rate each statement: (Presented as a Likert scale with radio buttons) Your unit’s performance Your unit’s overall efficiency Patient flow Staff performance Staff morale Communication and management of difficult situations with staff Communication with patients and their families Management of staff Rostering of staff Financial management 34. What are the three biggest barriers you face doing your work? 35. What are the three things that might make your job easier or more effective? 120 Report of the mid program evaluation of ‘take the lead’ 36. Do you have the opportunity to meet with other CSOs in order to share information and provide support to each other? Yes/No 37. Have you undertaken any training to prepare you or develop you in your role as a CSO? Yes/No If yes, what kind of training? 38. Is there any other comment you would like to make specifically about the role of CSO? 39. Is there any other comment you would like to make? 121 Report of the mid program evaluation of ‘take the lead’ 8.2 Literature review In this section we provide further discussion of the issues raised in the literature review. These are presented in order to provide a context for readers who may not be familiar with the origins of the ‘ttl’ program and factors affecting its implementation. 8.2.1 Examples of concurrent initiatives to improve patient safety During the implementation period of the ‘take the lead’ other initiatives, also aiming to improving patient care, have been introduced. These initiatives have stimulated change and so it is important to recognise the potential effect of these initiatives when evaluating the ‘take the lead’ project. As there have been numerous initiatives, only a sample of these are briefly outlined below. The Essentials of Care Program The New South Wales Government declared stage one support for Recommendation 38 in the Garling Report through the implementation of the Essentials of Care Program over a three year period in every ward in New South Wales. The Essentials of Care (EOC) Program commenced in February 2008. EOC is an evaluation framework to develop, support and continuously evaluate essential patient care that is fundamental to each patient’s health and wellbeing. Involvement of the patient and their carers in discussions and decisions about their care is pivotal to achieving effective essential care. EOC utilises transformational practice development methodologies and aims to improve patient safety and outcomes, and enhance the experiences of patients and all involved in their care. It aims to enable nurses and midwives to “focus on the development of clinical environments that enhance patient care, teamwork and individual satisfaction.” (NSW Health Nursing and Midwifery Office, 2008). Recommendation 38 “The Chief Nursing and Midwifery Officer of NSW Health should supervise the preparation within 6 months of and ensure over a 2 year period the implementation of a program across all public hospitals in NSW which is designed to achieve an improvement in the efficiency and design of nursing work practices in each ward or unit having regard to the principles of shared care and team-based work practices. The NSW program should take into account the improvements made by the Productive Ward Program in the United Kingdom and the Essentials of Care Program.” (Garling, 2008: 43) 122 Report of the mid program evaluation of ‘take the lead’ Recommendation 38 New South Wales Government Response: (Stage One Supported) “The Essentials of Care program provides nurses and other health professionals with a method to explore and understand current clinical practice and practice environments and to develop ways to further enhance them. It is already being established across Area Health Services with a focus on patients’ experience, as well as what the patients, their families and health professionals value about effective and relevant patient care. Building on this, the Chief Nursing and Midwifery Officer will supervise a program designed to achieve greater efficiency and design of nursing work practices, giving consideration to shared care and teamwork principles. To ensure successful implementation, NSW Health will achieve this in every ward over a 3 year period.”(NSW Department of Health, 2009: 25) Between the Flags Initiative Between the Flags, an initiative of the Clinical Excellence Commission, has been implemented in hospitals across New South Wales (Clinical Excellence Commission et al., 2010). This initiative aims to improve and standardise the response to and the identification of the deteriorating patient. Standardised colour coded observation charts have been introduced to track observations and trigger a response when observations fall within identified parameters. If the patient’s observations fall within the yellow and red zones on the observation chart, the need for initiation of assessment or rapid response is indicated. Safe Clinical Handover The Garling Report specifically addressed the need to improve policies and procedures on clinical handover. Specifically, Garling recommended that a mandatory shift handover policy be designed and introduced in each hospital. The handover policy must require that part of the handover is to be conducted at the bedside, sufficient time for handover be incorporated when rostering, that required information is included in handover, and that an electronic or written record be made of the handover (Recommendation 56, Garling Report 2008). These recommendations were supported and an action plan developed including the development of key principles and strategies for clinical handover (NSW Health, 2009). 123 Report of the mid program evaluation of ‘take the lead’ 8.2.2 The role of the Nursing/Midwifery Unit Manager within NSW Health NSW Health comprises the Department of Health, eight Area Health Services, statutory health corporations and affiliated health organisations. Public hospitals contain patient ward areas or units. N/MUMs are in charge of all aspects of designated ward or unit environments and are responsible for the standard of patient care in those wards or units. He or she coordinates patient services, unit management, and nursing/midwifery staff management to ensure efficient use of resources and delivery of high quality patient care. N/MUMs have a key role in influencing the culture of a unit, the satisfaction of their staff, the quality of care patients receive, and the experience of the patient and their carer. As a result, expectations of N/MUMs are increasing. They are now ‘expected to provide not only clinical leadership within their units but also deal with an increasing number of organisational and administrative requirements and at the same time ensure the maintenance of high standards of nursing and midwifery care’ (Hawe, 2009: 2). i. NSW Public Health System Nurses’ and Midwives’ State Award Within the New South Wales public health system, Nursing/Midwifery Unit Managers are defined as the “registered nurse in charge of a ward or unit or group of wards or units in a public hospital or health service or public health organisation” (NSW Health, 2010b:4). The NSW Public Health System Nurses’ and Midwives’ State Award classifies NUM/MUMs as Level 1, 2 or 3. The responsibilities of the Nursing/Midwifery Unit Manager Level 1 include: (a) CO-ORDINATION OF PATIENT SERVICES liaison with all health care disciplines for the provision of services to meet patient needs: the orchestration of services to meet patient needs after discharge; monitoring catering and transport services. (b) UNIT MANAGEMENT implementation of hospital/health service policy: dissemination of information to all personnel; ensuring environmental safety; monitoring the use and maintenance of equipment; monitoring the supply and use of stock and supplies; 124 Report of the mid program evaluation of ‘take the lead’ monitoring cleaning services. (c) NURSING STAFF MANAGEMENT direction, co-ordination and supervision of nursing activities; training, appraisal and counselling of nursing staff; rostering and/or allocation of nursing staff; development and/or implementation of new nursing practice according to patient need. Provided that the classification of Nursing/Midwifery Unit Manager Level 1 shall include those registered nurses who, as at 27 June 1986, were appointed as Charge Nurses or Supervisors of 20 but less than 50 beds or who were appointed at a rate of pay equal to the latter. Nursing/Midwifery Unit Manager Level 2 whose responsibilities in relation to patient services, ward or unit management and staff management are in excess of those of a Nursing/Midwifery Unit Manager Level 1. Nursing/Midwifery Unit Manager Level 3 whose responsibilities in relation to patient services, ward or unit management and staff management are in excess of those of a Nursing/Midwifery Unit Manager Level 2. Provided further, in relation to those nurses classified in accordance with this definition as Nursing/Midwifery Unit Managers on the basis of their former appointment as Charge Nurses or Supervisors, as the case may be, that nothing in this definition shall prevent them from being considered for regrading at any time after 27 June 1986.” (NSW Health, 2010b:6) 8.2.3 From Charge Sister to Nursing/Midwifery Unit Manager As the demands on, and from, the health workforce have changed over the last decade, so too have the demands placed on nurse managers (Productivity Commission, 2005). An overview of the literature reports the evolution of the nurse manager role from the traditional head nurse role (1980-1991), through early expansion of the role (1992-1999) to an expanded nurse manager role (2000-2003) (Shirey, 2006). While the role of Nurse/Midwifery Unit Managers was originally intended to provide clinical leadership, increasing expectations to undertake administrative tasks has detracted from this important role (NSW Nurses' Association, 2009). Nursing leadership is essential in developing and sustaining a healthy work environment (Pearson et al., 2007) and is correlated with productivity, 125 Report of the mid program evaluation of ‘take the lead’ organisational commitment (Chiok Foong Loke, 2001) and job satisfaction (Duffield et al., 2009). In particular, knowledge of leadership principles, an ability to communicate, motivate and manage conflict among staff, a commitment to personal and staff professional development, and being honest and supportive of staff, are important characteristics of the successful nurse leader (Pearson et al., 2007). As early as the mid 1990s graduate programs designed to prepare nurse managers for the leadership positions were introduced or being developed in Sweden and the United Kingdom (Kleinman, 2003). The N/MUM roles and responsibilities have changed extensively over the last 25 years as “nursing increasingly bases its claim to professional status upon a managerialist discourse: it seeks legitimacy and power by embracing both a managerial ideology and management practices” (Brooks, 1999: 41). The clinical leadership role on a ward or unit was once fulfilled by the Charge Sister. This role was based on clinical experience and expertise until 1986 when in New South Wales, the N/MUM role was created to replace the Charge Sister role. The Clinical Nurse Specialist role was simultaneously introduced to take over the clinical role leadership role that was surrendered by the Nurse Unit Manager for a focus on managerial responsibilities (Duffield et al., 2001). The shift from hospital to tertiary based nursing education underscored the emphasis on clinical autonomy among nurses and a resultant perceived decrease in the need for clinical expertise among their managers (Duffield et al., 2001). This has led to the development of a nursing managerial role that is less and less traditional and more diverse, encompassing more and more non-nursing responsibilities with the risk that with an increasing span of control, nurse managers may become ineffective with their clinical credibility eroded (Duffield et al., 2001). A recognised difficulty for Nurse Unit Managers was the lack of formalised training in management skills and an absence of role models, particularly given the dominance of role model based learning in nursing (Duffield et al., 2001). Decentralisation and the introduction of primary nursing impacted the role of nurse unit manager requiring new types of managerial skills (Duffield, 1991). Uncertainty over role definition and a perceived gap in management skills is problematic not only in Australia (Duffield et al., 1994) but internationally (e.g. New Zealand (McCallin et al., 2010), South Africa (Pillay, 2009), and the United Kingdom (Gould et al., 2001). The development of leadership and management skills have replaced clinical skills identified as necessary for the nurse unit manager role (Oroviogoicoechea, 1996, Gould et al., 2001) and concern about whether individuals in healthcare are adequately prepared for their management role has been expressed (Kleinman, 2003). A priceless contribution that a nurse brings to the N/MUM role is undoubtedly 126 Report of the mid program evaluation of ‘take the lead’ their ability to factor in the intricate complexities and demands of patient care in management decisions (Duffield et al., 2001). An overview of the literature reports the evolution of the nurse manager role from the traditional head nurse role (1980-1991) through early expansion of the role (1992-1999) to an expanded nurse manager role (2000-2003) (Shirey, 2006). Stress among nurse managers is understood in relation to the staff shortages, increased responsibility and exigent work environment (Shirey, 2006). In summary, concerns for NUMs identified in the literature include: a lack of recognition, overtime, isolation, staff shortages, numerous meetings, increasing administrative load, lack of training for managerial role, competing clinical and managerial responsibilities (Hillier, 2005). The nurse manager role continues to evolve and in Australia managing the competing demands of clinical leadership and managerial roles poses ongoing challenges for nurse/midwifery unit managers. N/MUMs must straddle technical, managerial and clinical demands in a highly demanding and continuously and rapidly changing environment. While aiming to provide compassionate care and clinical leadership they are simultaneously required to manage finances, administrative demands, performance manage, and staff their unit often within the context of staff shortages, increasing litigation, demand for decreased elective waiting lists, publicised adverse events (e.g. Vanessa Anderson, St George Hospital epidural event), disquiet among their nursing staff (e.g. industrial action over patient to staff ratios (NSW, Nov 2010)) and financial restraints. They are required to ensure and measure the delivery of quality care in their unit quantified with indicators such as adverse events, patient complaints, patient compliments, length of stay and patient flow. The literature identifies that when financial restrictions are imposed, the work life concerns of nurses are often the first to be sacrificed (Duffield et al., 2002) catalysing an exodus of nurses further compromising staff satisfaction. Nurse shortages contribute to job dissatisfaction and negatively impact quality of care. Research suggests that patients in environments where there is a high nurse turnover are more physically and emotionally compromised (Hayes et al., 2006). Appropriate staff skill mix based patient needs is significantly correlated with patient outcomes (Twigg et al., (in press)). It is within this context that N/MUMs are navigating the competing demands of their role. 8.2.4 Ongoing development of nurse managers As the role of N/MUMs developed both in Australia and internationally, so too did the range of mechanisms utilised to facilitate that development. In many cases, 127 Report of the mid program evaluation of ‘take the lead’ including the United Kingdom (Sprinks, 2010, Kellagher et al., 2010), Canada (MacPhee et al., 2010) and New Zealand (McCallin et al., 2010) development strategies are intended to address very similar issues to those identified by ‘ttl’. Most common among these are issues relating to N/MUMs (or their equivalents’) role ambiguity, workload and appropriate preparation for, and development of, their role, including competencies relating to management and leadership skills (MacMillan-Finlayson, 2010, Lewis et al., 2010, Kennedy, 2008). As part of the formalisation of nurse managers’ roles, there is an ongoing international interest in the development of specific sets of nurse manager competencies (Thomas et al., 2008, Chase, 1994). Competencies provide two functions for professional development: they act both as the basis for the development of educational/training strategies, and as the basis for assessments and reviews (Sutto et al., 2008, Care et al., 2003, Donaher et al., 2007). As the development of specific nurse manager competencies progresses, so too has the sophistication of the competencies themselves (Lin et al., 2007). Ireland, for example, now has specific nurse manager competencies aimed at managers-director, middle manager and front line manager levels (McCarthy et al., 2009). Although each competency set varies, reflecting national priorities as much as professional requirements, they generally include elements such as: ethical behaviour and integrity, effective decision making skills, change management, leadership, human and financial management skills, lifelong learning, communication skills, conflict resolution and negotiation skills (Sutto et al., 2008, Palarca et al., 2008, Jennings et al., 2007, Krejci et al., 1997, Care et al., 2003, Davis, 2005). While a range of nurse manager development strategies currently being implemented in health services around the world, the most common include: role induction (McCallin et al., 2010, Hawkins et al., 2009); in-house, ‘hands-on’ training(Maguire et al., 2004, Kowalski, 2004), coaching or mentoring programs (Karsten, 2010, Cashin et al., 2010, Rosati, 2009, McLarty et al., 2009); clinical supervision; succession planning (Ponti, 2009, Mass et al., 2006); and postgraduate training (McCallin et al., 2010, Joyce, 2005, Duffield, 2005). 8.2.5 Transfer of learning to the workplace The transfer of learning, from training and educational contexts, into the workplace remains a central concern for health and other industries. This is partly because estimates that the effective transfer of learning (as measured by behavioural change) occurs only in between 10 – 20% of cases, with about 40% of trainees failing to transfer what they learn once they return to the workplace, growing to about 70% a 128 Report of the mid program evaluation of ‘take the lead’ year after their attendance at a training program. It is generally accepted that only 50% of training investments actually result in improvements for either the individuals or the organisation (Leimbach, 2010, Burke et al., 2007, Georgenson, 1982, Saks, 1995). Three key characteristics are said to affect learners’ abilities to transfer what they learn into their workplace. These include: learner characteristics and readiness; training design and delivery; and the workplace environment (Leimbach, 2010, Kirkpatrick et al., 2006, Nijman et al., 2006, Alvarez et al., 2004). At an individual level, characteristics said to predict the transfer of learning include cognitive ability, self-efficacy, motivation (both to attend and to transfer what is learnt) openness to experience, perceived utility of the training and career planning. There is mixed evidence for the influence of extrinsic versus intrinsic motivation, conscientiousness, and internal versus external control (Blume et al., 2010, Burke et al., 2007, Colquitt et al., 2000, Holladay et al., 2003, Quiñones, 1995). At the intervention level, predictors included appropriate learning goals, content relevance, practice and feedback behavioural-modelling, and error based examples. There is some evidence for the influence of self-management strategies (Blume et al., 2010, Burke et al., 2007, Taylor et al., 2005, Locke et al., 2002). There were a number of predictors of learning transfer at an organisational level. These include: a supportive work environment, a strong transfer climate, supervisory support, peer support, opportunity to perform and organisational commitment (Blume et al., 2010, Burke et al., 2007, Colquitt et al., 2000). 8.2.6 Factors supporting and inhibiting workplace change Healthcare environments are ‘busy, complex and chaotic’ (Grimshaw et al., 2004). Managerial responsibilities in healthcare environments include pressures additional to those in most other industries, such as as life and death decisions, clinical complexities and strong autonomy of individual professionals (Braithwaite et al., forthcoming). Researchers have tried to identify and describe the manager’s role and more specifically, how managers conduct their work (Fayol, 1949, Carlson, 1951, Mintzberg, 1971, Kotter, 1982, Stewart, 1998). Managing change is a particularly important element of the healthcare ‘managerial routine’ (Braithwaite, 2004). Managers can be viewed as continuously attempting to make sense of their complex professional environments, whilst initiating and spearheading progress and improvement (Braithwaite et al., forthcoming). This constant striving for change and improvement is at the core of all managerial work. Change takes on different forms 129 Report of the mid program evaluation of ‘take the lead’ from implementing new IT solutions to managing a budget or dealing with staff performance. In this context, change can be defined as an “innovation in service delivery and organization as a novel set of behaviours, routines, and ways of working that are directed at improving health outcomes, administrative efficiency, cost effectiveness, or users' experience and that are implemented by planned and coordinated actions” (Greenhalgh et al., 2004: 582). In order for change to be implemented successfully the intervention chosen needs to be tailored to the specific situation. It is essential that in each and every intervention, the potential barriers for implementation are identified and addressed (Flottrop et al., 2003) Four levels of change in health care have been identified: the whole healthcare system; institutional/organisational level; groups and teams; and the individual (Ferlie et al., 2001). Multiple hierarchical domains are a part of the context that underpins the management of change in healthcare (Braithwaite et al., forthcoming). On the one hand there is the formal hierarchy as depicted by the organisational chart, on the other an informal, internal hierarchy within and across professions. This less formal hierarchy can be based on “political and professional rankings according to status, reputation, power or importance, or a combination of these” (Braithwaite et al., forthcoming). For example, doctors often outrank nurses in terms of power. In order to coordinate and implement change, managers need to navigate this complex environment. In the past, it was commonly assumed that most barriers to implementation of change were at an individual level (e.g. negative attitudes or lack of knowledge and skills). There is now increasing recognition that there are multiple levels in which barriers exist, many of which are not within the control of the individual (Grimshaw et al., 2004). Greenhalgh, Robert, Macfarlane, Bate, Kyriakidou (2004) provide a comprehensive description and analysis of how innovation is distributed within service organisations. The authors describe a model that includes multiple components that interact with each other. These components include characteristics of: the innovation itself; the adopter; the readiness of the system; the process chosen for implementation; the external context; the type of communication and influence used to transfer the innovation; and the linkages (see model). The existence or lack of a certain characteristic does not guarantee the adoption or rejection of an innovation. It is imperative that change agents remember that “the attributes are neither stable features of the innovation nor sure determinants of their adoption or assimilation. Rather, it is the interaction among the innovation, the intended adopter(s), and a particular context that determines the adoption rate.” (Greenhalgh et al., 2004: 598). 130 Report of the mid program evaluation of ‘take the lead’ There is variance with the rate at which change is adopted. This can be ascribed to a number of different attributes of the innovation itself. For example, innovations that have a clear relative advantage in effectiveness or cost effectiveness are more easily and more willingly adopted. If the advantage of the innovation is not clear to the individuals involved there is no chance that the innovation will be adopted. On the other hand, there is no guarantee that when the advantage is clear, that adoption will be widespread. Other examples that increase the chance that an innovation will be adopted are low complexity; high compatibility with the norms and values and needs of potential adopters; high visibility; easy to trial; and high relevance to the task. (Greenhalgh et al., 2004). The adoption of innovations by individuals is an interactive process. Individuals are not passive recipients of change. Individuals negotiate, experiment, evaluate, emotionally react to,, and modify innovations. Greenhalgh et al (2004) argue against applying wide ‘adopter categories’ as there is little support for them in the literature. The authors articulate seven adopter categories that influence uptake of innovations. For example the meaning of the innovation for the individual has been shown to impact on the likelihood of change. When there is congruence between the meaning intended by the managerial level initiating the innovation and the meaning perceived by the individual, there is more chance that the innovation will be adopted. The meaning can also be negotiated and reframed within and between organisational levels (Greenhalgh et al., 2004). Other examples of individual attributes that increase the chance of adoption are psychological antecedents such as traits that increase the likelihood an individual will try and use innovations; context-specific psychological antecedents such as strong motivation and congruence with values, goals and skills; having a say in the decision process; awareness of concerns regarding the innovation or its consequences and an ability to address them; having information, training and support during early stages of adoption; when feedback regarding implications of the innovation are communicated to users and that the individuals can adapt the innovation according to the feedback (Greenhalgh et al., 2004). 131 Report of the mid program evaluation of ‘take the lead’ 8.3 Demographic characteristics of participants Table 28: demographic characteristics of participants~ DEMOGRAPHIC VARIABLES Gender Number of ‘ttl’ modules completed Participation in Essentials of Care Current role Years in health post graduation N/MUM INTERVIEWS N = 30 M=3 F = 27 5 CASE STUDIES N=2 STAFF SURVEY N = 23 CSO SURVEY N=92 TOTAL N = 177 M=0 F=2 5 (N=2) MANAGER INTERVIEWS N = 30 M=4 F = 26 n/a M=7 F=16 n/a M=6 F=86 n/a M= 20 F= 157 10 2 12 11 n/a N/MUM N/MUM, Nurse Manager N/MUM Level 3 to DON Nursing/ Midwifery (13) Medicine (4) Allied Health (6) Range: 1-42 Average: 22 years CSO Range: 8-40 years Average: 24 years Range: 2-20 Average: 6 years Range: 10-26 Range: 8-45 Range: 1 -37* years Average: 26 Average: 7 Average: 16 years years years Years in current Range: 5-9 Range: 1-26 n/a Less than one role years years year = 79 Average: 7 Average: 9 years One year= 12 years Two years = 1 Years in current Range: 1-34 Range: 7-11 Range: 1-35 n/a n/a unit/hospital years years years Average: 8 years Average: 9 Average: 11 years years Years in current Range: 1-15 Range: 1-7 Range: 1-15 n/a Range: 1 – 25 role in current years years years months unit/hospital Average: 5 years Average: 4 Average: 5 years Average: 8 years months % of work on Range: 20-100 Range: 60-100 n/a n/a n/a management Average: 56 Average: 80 % of work on Range: 1-80 Range: 1-40 n/a n/a n/a clinical duties Average: 44 Average: 20 ~ all years rounded up to the nearest whole year (except for CSOs), *Years in health total 132 Report of the mid program evaluation of ‘take the lead’ 8.4 Changes to N/MUMs’ capabilities and skills since ‘ttl’ 8.4.1 NUMS’ responses to changes in their capabilities and skills since ‘ttl’ Figure 2: changes in N/MUM’s job performance since ‘ttl’ 60 50 40 30 20 10 0 Increased significantly Increased somewhat Stayed the same Decreased somewhat Decreased significantly Job performance Figure 3: changes in N/MUMs communication skills since ‘ttl’ 60 50 40 30 20 10 0 Increased significantly Increased somewhat Stayed the same Decreased somewhat Ability to communicate with own staff Ability to communicate with other staff Ability to communicate with patients and family 133 Decreased significantly Report of the mid program evaluation of ‘take the lead’ Figure 4: changes in N/MUMs ability to manage complex situations since ‘ttl’ 70 60 50 40 30 20 10 0 Increased significantly Increased somewhat Stayed the same Management of difficult situations Decreased somewhat Negotiation skills Decreased significantly Problem solving Figure 5: changes in N/MUMs ability to manage staff since ‘ttl’ 60 50 40 30 20 10 0 Increased significantly Increased somewhat Stayed the same Decreased somewhat Ability to manage staff 134 Decreased significantly Report of the mid program evaluation of ‘take the lead’ Figure 6: changes in N/MUMs’ leadership abilities since ‘ttl’ 60 50 40 30 \ 20 10 0 Increased significantly Increased somewhat Stayed the same Decreased somewhat Decreased significantly Leadership abilities Figure 7: changes in N/MUMs’ management skills since ‘ttl’ 70 60 50 40 30 20 10 0 Increased significantly Increased somewhat Stayed the same Decreased somewhat Application of lean thinking Management of finances and resources Rostering of staff 135 Decreased significantly Report of the mid program evaluation of ‘take the lead’ 8.4.2 NUMS’ managers’ responses to N/MUMs changes in their capabilities and skills since ‘ttl’ Figure 8: Managers’ perceptions of changes in N/MUM’s job performance since ‘ttl’ 40 35 30 25 20 15 10 5 0 Improved significantly Due to ttl Improved somewhat Stayed the same Worsened somewhat Unsure of cause or partly due to 'ttl' Worsened significantly Not due to ttl Figure 9: Managers’ perceptions of changes in N/MUMs communication skills with staff 50 45 40 35 30 25 20 15 10 5 0 Improved significantly Due to ttl Improved somewhat Stayed the same Worsened somewhat Unsure of cause or partly due to 'ttl' 136 Worsened significantly Not due to ttl Report of the mid program evaluation of ‘take the lead’ Figure 10: Managers’ perceptions of changes in N/MUMs communication skills with patients and their families since ‘ttl’ 60 50 40 30 20 10 0 Improved significantly Due to ttl Improved somewhat Stayed the same Worsened somewhat Unsure of cause or partly due to 'ttl' Worsened significantly Not due to ttl Figure 11: Managers’ perceptions of changes in N/MUMs communication skills with other staff since ‘ttl’ 50 45 40 35 30 25 20 15 10 5 0 Improved significantly Due to ttl Improved somewhat Stayed the same Worsened somewhat Unsure of cause or partly due to 'ttl' 137 Worsened significantly Not due to ttl Report of the mid program evaluation of ‘take the lead’ Figure 12: Managers’ perceptions of changes in N/MUMs ability to manage difficult situations since ‘ttl’ 45 40 35 30 25 20 15 10 5 0 Improved significantly Due to ttl Improved somewhat Stayed the same Worsened somewhat Unsure of cause or partly due to 'ttl' Worsened significantly Not due to ttl Figure 13: Managers’ perceptions of changes in N/MUMs negotiation skills since ‘ttl’ 50 45 40 35 30 25 20 15 10 5 0 Improved significantly Due to ttl Improved somewhat Stayed the same Worsened somewhat Unsure of cause or partly due to 'ttl' 138 Worsened significantly Not due to ttl Report of the mid program evaluation of ‘take the lead’ Figure 14: Managers’ perceptions of changes in N/MUMs ability to problem solve since ‘ttl’ 35 30 25 20 15 10 5 0 Improved significantly Due to ttl Improved somewhat Stayed the same Worsened somewhat Unsure of cause or partly due to 'ttl' Worsened significantly Not due to ttl Figure 15: Managers’ perceptions of changes in N/MUMs ability to manage staff since ‘ttl’ 45 40 35 30 25 20 15 10 5 0 Improved significantly Due to ttl Improved somewhat Stayed the same Worsened somewhat Unsure of cause or partly due to 'ttl' 139 Worsened significantly Not due to ttl Report of the mid program evaluation of ‘take the lead’ Figure 16: Managers’ perceptions of changes in N/MUMs’ leadership abilities since ‘ttl’ 60 50 40 30 \ 20 10 0 Improved significantly Improved somewhat Due to ttl Stayed the same Worsened somewhat Unsure of cause or partly due to 'ttl' Worsened significantly Not due to ttl Figure 17: Managers’ perceptions of changes in N/MUMs’ management skills since ‘ttl’: application of lean thinking 60 50 40 30 20 10 0 Improved significantly Due to ttl Improved somewhat Stayed the same Worsened somewhat Unsure of cause or partly due to 'ttl' 140 Worsened significantly Not due to ttl Report of the mid program evaluation of ‘take the lead’ Figure 18: Managers’ perceptions of changes in N/MUMs’ management skills since ‘ttl’: ability to manage finances 45 40 35 30 25 20 15 10 5 0 Improved significantly Improved somewhat Due to ttl Stayed the same Worsened somewhat Unsure of cause or partly due to 'ttl' Worsened significantly Not due to ttl Figure 19: Managers’ perceptions of changes in N/MUMs’ management skills since ‘ttl’: ability to manage rostering 35 30 25 20 15 10 5 0 Improved significantly Due to ttl Improved somewhat Stayed the same Worsened somewhat Unsure of cause or partly due to 'ttl' 141 Worsened significantly Not due to ttl Report of the mid program evaluation of ‘take the lead’ 8.5 Improvements at the unit level since ‘ttl’ 8.5.1 N/MUMs’ perceptions of improvements at unit level since ‘ttl’ Figure 20: N/MUMs’ perceptions of unit performance and efficiency since ‘ttl’ 60 50 40 30 20 10 0 Improved significantly Improved somewhat Stayed the same Unit's performance Worsened somewhat Worsened significantly Unit's efficiency Figure 21: N/MUMs’ perceptions of changes in number of adverse events since ‘ttl’ 80 70 60 50 40 30 20 10 0 Increased significantly Increased somewhat Stayed the same Decreased somewhat Number of adverse events 142 Decreased significantly Report of the mid program evaluation of ‘take the lead’ Figure 22: N/MUMs’ perceptions of changes to patient flow since ‘ttl’ 45 40 35 30 25 20 15 10 5 0 Improved significantly Improved somewhat Stayed the same Worsened somewhat Worsened significantly Patient flow Figure 23: N/MUMs’ perceptions of time spent of administrative tasks since ‘ttl’ 40 35 30 25 20 15 10 5 0 Increased significantly Increased somewhat Stayed the same Decreased somewhat Time spent on administrative tasks 143 Decreased signficantly Report of the mid program evaluation of ‘take the lead’ Figure 24: N/MUMs’ perceptions of changes in staff performance since ‘ttl’ 50 45 40 35 30 25 20 15 10 5 0 Improved significantly Improved somewhat Stayed the same Worsened somewhat Worsened significantly Staff performance Figure 25: N/MUMs’ perceptions of staff satisfaction and retention since ‘ttl’ 70 60 50 40 30 20 10 0 Increased significantly Increased somewhat Stayed the same Staff satisfaction 144 Decreased somewhat Staff retention Decreased significantly Report of the mid program evaluation of ‘take the lead’ Figure 26: N/MUMs’ perceptions of staff morale since ‘ttl’ 50 40 30 20 10 0 Improved significantly Improved somewhat Stayed the same Worsened somewhat Worsened significantly Staff morale Figure 27: N/MUMs’ perceptions of staff absenteeism since ‘ttl’ 70 60 50 40 30 20 10 0 Increased significantly Increased somewhat Stayed the same Decreased somewhat staff absenteeism 145 Decreased signficantly Report of the mid program evaluation of ‘take the lead’ Figure 28: N/MUMs’ perceptions of patient measures since ‘ttl’ 70 60 50 40 30 20 10 0 Increased significantly Increased somewhat patient satisfaction Stayed the same Decreased somewhat patient compliments Decreased significantly patient complaints 8.5.2 Managers of N/MUMs’ perceptions of improvements at unit level since ‘ttl’ Figure 29: Manager’s perceptions of unit performance since ‘ttl’ 40 35 30 25 20 15 10 5 0 Improved significantly Due to ttl Improved somewhat Stayed the same Worsened somewhat Unsure of cause or partly due to 'ttl' 146 Worsened significantly Not due to ttl Report of the mid program evaluation of ‘take the lead’ Figure 30: Manager’s perceptions of unit efficiency since ‘ttl’ 40 35 30 25 20 15 10 5 0 Improved significantly Due to ttl Improved somewhat Stayed the same Worsened somewhat Unsure of cause or partly due to 'ttl' Worsened significantly Not due to ttl Figure 31: Managers’ perceptions of changes in number of adverse events since ‘ttl’ 50 45 40 35 30 25 20 15 10 5 0 Increased significantly Due to ttl Increased somewhat Stayed the same Decreased somewhat Unsure of cause or partly due to 'ttl' 147 Decreased significantly Not due to ttl Report of the mid program evaluation of ‘take the lead’ Figure 32: Manager’s perceptions of changes to patient flow since ‘ttl’ 50 45 40 35 30 25 20 15 10 5 0 Improved significantly Due to ttl Improved somewhat Stayed the same Worsened somewhat Unsure of cause or partly due to 'ttl' Worsened significantly Not due to ttl Figure 33: Manager’s perceptions of time spent of administrative tasks since ‘ttl’ 25 20 15 10 5 0 Increased significantly Due to ttl Increased somewhat Due to ttl + CSO Stayed the same Due to CSO alone 148 Decreased somewhat Unsure of cause Decreased significantly Not due to ttl Report of the mid program evaluation of ‘take the lead’ Figure 34: Managers’ perceptions of changes in staff performance since ‘ttl’ 35 30 25 20 15 10 5 0 Improved significantly Due to ttl Improved somewhat Stayed the same Worsened somewhat Unsure of cause or partly due to 'ttl' Worsened significantly Not due to ttl Figure 35: Managers’ perceptions of staff satisfaction since ‘ttl’ 25 20 15 10 5 0 Increased significantly Due to ttl Increased somewhat Stayed the same Decreased somewhat Unsure of cause or partly due to 'ttl' 149 Decreased significantly Not due to ttl Report of the mid program evaluation of ‘take the lead’ Figure 35: Managers’ perceptions of staff retention since ‘ttl’ 80 70 60 50 40 30 20 10 0 Increased significantly Due to ttl Increased somewhat Stayed the same Decreased somewhat Unsure of cause or partly due to 'ttl' Decreased significantly Not due to ttl Figure 36: Manager’s perceptions of staff absenteeism since ‘ttl’ 60 50 40 30 20 10 0 Increased significantly Due to ttl Increased somewhat Stayed the same Decreased somewhat Unsure of cause or partly due to 'ttl' 150 Decreased significantly Not due to ttl Report of the mid program evaluation of ‘take the lead’ Figure 37: Manager’s perceptions of staff morale since ‘ttl’ 35 30 25 20 15 10 5 0 Improved significantly Due to ttl Improved somewhat Stayed the same Worsened somewhat Unsure of cause or partly due to 'ttl' Worsened significantly Not due to ttl Figure 38: Managers’ perceptions of patient compliments since ‘ttl’ 45 40 35 30 25 20 15 10 5 0 Increased significantly Due to ttl Increased somewhat Stayed the same Decreased somewhat Unsure of cause or partly due to 'ttl' 151 Decreased significantly Not due to ttl Report of the mid program evaluation of ‘take the lead’ Figure 39: Managers’ perceptions of patient satisfaction since ‘ttl’ 40 35 30 25 20 15 10 5 0 Increased significantly Due to ttl Increased somewhat Stayed the same Decreased somewhat Unsure of cause or partly due to 'ttl' Decreased significantly Not due to ttl Figure 40: Managers’ perceptions of patient complaints since ‘ttl’ 40 35 30 25 20 15 10 5 0 Increased significantly Due to ttl Increased somewhat Stayed the same Decreased somewhat Unsure of cause or partly due to 'ttl' 152 Decreased significantly Not due to ttl Report of the mid program evaluation of ‘take the lead’ 8.6 CSO Survey 8.6.1 Background The CSO survey explored the introduction of the CSOs from their perspective. This is a preliminary analysis of the results. A total of 92 CSOs who were invited to participate, responded to the survey (48%). CSOs have a range of educational backgrounds and qualifications. Of the 90 CSOs who responded, 73% indicated that they had clerical backgrounds. Of the remainder, two had previously worked as nurses; four had worked in welfare or education; and the rest (n = 18) had a combination of customer service, administration, business and legal backgrounds. Table 29 lists the CSO’s current qualifications. Table 29: CSO’s qualifications QUALIFICATION RESPONDENTS (n = 70) Advanced diploma N = 3, (4%) Bachelor degree N = 14, (20%) Certificate III N = 24, (34%) Certificate IV N = 15, (22%) Diploma N = 7, (10%) Post graduate degree N = 3, (4%) Other N = 4, (6%) 8.6.2 Allocation to wards Slightly more of the CSOs were allocated to a single (58%) rather than multiple wards. All except two of the CSOs who responded (n = 89) said that they were allocated to direct care units (eg theatres, geriatrics, surgical, Emergency and Allied Health Departments etc). The two remaining CSOs were allocated to a centralised staff unit. An accurate summary of locations is difficult, because many respondents simply identified the number of the unit, such as Ward 10e or Rose Unit. 8.6.3 Satisfaction with reporting arrangements Most CSOs who responded currently respond directly to one or more N/MUMs (n = 57). The remaining CSOs report to senior nursing managers (DONMs) (n = 8), other senior managers (n = 1), mixed nursing (eg N/MUM and DONM) (n = 12), mixed nursing and non-nursing managers (n = 7) and other managers (n = 4). 153 Report of the mid program evaluation of ‘take the lead’ A number (n = 7) of the CSOs said they were not satisfied with their lines of reporting. Of these, one did not give a reason for their dissatisfaction. Table 30 outlines reasons for CSOs dissatisfaction with current lines of reporting. Table 30: Reasons for dissatisfaction with lines of reporting SUPERVISOR(S) REASON FOR DISATISFCATION N/MUM(s) The NUM was not interested in handing over the required tasks of the CSO. The DON is not interested in any progression of the CSO role and allows the NUM's to work as per usual prior to the introduction of the CSO role Senior staff member, nursing Many more skills are need than what I have Senior member nursing) staff I do not feel that I am progressing in the role of CSO as I had originally (non- anticipated. Senior (staffing) They're focussed on staffing, and doesn't have the skills nor the time to manage staff Multiple (nursing and non-nursing) It seems to be cumbersome and messages can be crossed or mixed. Other manager (clinical information) I think it would be better to report to the NUM as she can see what is happening on the job Six participants who report to N/MUMs, three that report to senior staff, two that report to other managers and one that reports to multiple staff did not give a reason for their satisfaction. Table 31 provides a sample of the reasons given by CSOs for their satisfaction with current lines of reporting. Table 31: Reasons for satisfaction with lines of reporting SUPERVISOR(S)* N/MUM(s) REASON FOR SATISFACTION Relationships I report directly to the NUM, from whom I receive most of my direction regarding the flow and type of work she wants me to accomplish in any given day. I have developed a wonderful working relationship with her and that was important in my role Because I have worked with this person previously and have a good relationship with her I work with a wonderful team who have made me feel welcome Very supportive , hands on always available 154 Report of the mid program evaluation of ‘take the lead’ SUPERVISOR(S)* REASON FOR SATISFACTION I am happy to report to my NUM Normal manager/subordinate relationship My NUM is very helpful and friendly They seem to appreciate my skills. Access/communication She is always accessible and nearby when needed I am grouped with the other Support services & Nursing staff on the ward Direct communication It is satisfactory as the NUM is the most in charge on the ward and I am working under them also available to give direction Easily able to prioritise workload in consultation with manager I can discuss work directly with the [department] head and their specific requirements My office is situated 5 metres from NUM's office on the ward so I am close to the NUM, Allied Health, doctors and staff if they need my assistance It is satisfactory as she is close by and approachable I spend 80% of my time here Because I work in direct contact with NUM on a daily basisgood feedback available NUM is my manager and we work closely together Most of my duties are carried out on behalf of the NUM therefore reporting back to same maintains communication flow. Structural issues It is satisfactory because most of my work is to assist the NUM The NUM provides me with all my jobs to do Because I am working under NUM supervision so for me it's satisfactory It suits me and my workload to report to the one person Multi tasking, lots of opportunities The NUM of [the department] has held the position for many years and has vast knowledge and experience in all areas of this department My direct supervisor whom I obtain my daily workload from My job is divided between the two units and the NUMs are my direct supervisors/managers They are the people who see me on a regular basis and know what work I am doing It's satisfactory because I support the NUM in most of her duties The NUM is the in charge on the ward she knows what is going on and what needs to be done this makes her the best person 155 Report of the mid program evaluation of ‘take the lead’ SUPERVISOR(S)* REASON FOR SATISFACTION Senior Nursing Multiple managers (nursing) Multiple managers (Nursing and non nursing) Other manager(s) to direct the CSO in her duties The NUM manages the ward They provide the majority of tasks NUM allocates task for me to complete. Role The purpose of the role is to take the burden of administration off the NUMs. Any other arrangement would be unsatisfactory I work closely with my NUM's daily and assist in all areas of their working load when able It is simple and clear and therefore easy to communicate and manage workload/expectations There is a clear line of management and they are approachable and reasonable Working on a ward the NUM is the person in charge of the ward and therefore they are also the person who you assist I have a mix of duties which overlap as well. It is challenging and rewarding The NUM is in control of the smooth running of the ward, so she directs me to help her with that. Because I am allocated to multiple wards and multiple hospital having one manager is better as there is less conflict when I am given instruction on how to deal with Issues Full support from the DoNM. Both managers work together It is satisfactory because these are the people that provide me with work Communicate well with both managers. Work mostly with the NUM Depending on what role I am doing for the day depends on which manager I report to Variety of work Work well with each other As there are two people to report to it gives the opportunity to be able to speak to the most appropriate person with regards to any issues; due to their different positions within the hospital It covers both the aspect of pay etc and work locations Report directly to NUMs, who allocate tasks, and Executive Unit who hold administrative resources They are my boss - who else could I report to? It is satisfactory as if helps the NUM so that they have more time with patients, nurses and doctors. I am a relief CSO: manager covers all clerical areas. 156 Report of the mid program evaluation of ‘take the lead’ * Supervisor as N/MUMs refers to CSOs who report to one or more N/MUMs at the same level. Multiple managers (nursing) refers to CSOs who stated they reported to N/MUMs and DONs or other senior nursing staff as well as N/MUMS. A small number of respondents said that they were happy with their lines of reporting, but made qualifying statements. These provide some insight into the tensions in the role: Reporting to N/MUMs It is satisfactory but it would be good to have a general person to go to about issues Satisfactory because answering to nursing staff would be too confusing Mostly ok, but re definition of work a bit problematic some times, as no precedence. Reporting to multiple managers (nursing) Only two now, used to reporting to more - it gets difficult at times when too many bosses. 8.6.4 Hours and days of work Most CSOs worked between five and 40 hours a week. Only six of the CSOs work on weekends: three CSOs work both Saturdays and Sundays, two work on Saturdays and one indicated that they work on Sundays in addition to weekdays. Table 32: Hours of work HOURS PER WEEK RESPONDENTS (n = 81) 5-10 N = 20, (25%) 15 -20 N = 4, (5%) 20-25 N = 5, (6%) 25-30 N = 1, (1%) 30-35 N = 7, (9%) 35 – 40 N = 40, (49%) More than 40 hours N = 4, (n = 5%) CSOs were asked about the proportion of time each week they spend working with different professional groups. Table 33 outlines the results. 157 Report of the mid program evaluation of ‘take the lead’ Table 33: Hours of work OWN N/MUM OTHER N/MUMS MEDICAL STAFF NURSING STAFF ALLIED HEALTH OTHER Mean* 65% 11% 4% 13% 2% 5% Median 70% 5% 0% 10% 0% 0% Mode 80% 5% 0% 0% 0% 0% Highest percentage 100% (n = 6) 80% (n = 1) 50% (n = 1) 60% (n = 1) 20% (n = 1) 95% (n = 1) Lowest percentage 0% (n = 1) 0 (n = 37) 0 (n = 52) 0 (n = 23) 0 (n = 58) 0 (n = 65) 8.6.5 CSOs’ duties In addition to these questions, a sample of 27 CSOs duty statements were collected and reviewed. All of these closely mirrored the NSW Health duty statement for CSOs, with only minor differences (whether the CSO was to have a Certificate III or Certificate IV, some additional duties). More information about duties was gained through the survey questions below. Participants were asked about their roles and responsibilities, based on the NSW Health statement of duties for CSOs. Tables 34 to 38 outline the number of participants undertaking each task. Table 34: Number of CSOs undertaking data entry and reporting* ROLE OR RESPONSIBILITY NUMBER OF RESPONDENTS (N = 82) Data entry for ward/unit rosters into relevant IT system N = 73, (89%) Updating the roster in line with any approved changes ie sick leave etc N = 75, (91%) Entering information onto HR IT system once approved N = 33, (40%) Data entry activities that relate to patient care activities and support any member of the health care team N = 48, (59%) Registering births to the NSW Registry of Births, Deaths and Marriages N = 6, (7%) 158 Report of the mid program evaluation of ‘take the lead’ ROLE OR RESPONSIBILITY NUMBER OF RESPONDENTS (N = 82) Assisting the N/NUM in producing reports on finance and quality parameters/indicators N = 55, (67%) * More than one response possible per participant Table 35: Number of CSOs undertaking duties relating to workforce matters* ROLE OR RESPONSIBILITY NUMBER OF RESPONDENTS (N = 85) Rostering N = 64, (75%) Recruitment N = 58, (68%) Leave N = 73, (86%) Payroll N = 49, (58%) Liaising with Health Support Services to clarify pay and leave enquiries N = 64, (75%) Providing support for the recruitment of staff to the ward/unit N = 57, (67%) Undertaking administrative activities related to the management of performance reviews for staff that the N/MUM and other ward based medical and allied health staff line manage within the unit Assisting with the replacement of staff as directed by the N/MUM N = 52, (61%) N = 57, (67%) * More than one response possible per participant Table 36: Number of CSOs undertaking duties relating to resource management* ROLE OR RESPONSIBILITY NUMBER OF RESPONDENTS (N = 69) Ensuring the ward/unit has adequate stock of medical supplies and equipment required by staff to perform their day to day duties in delivery of patient care N = 53, (77%) Purchasing and receiving new equipment for the ward/unit and equipment maintenance. N = 61, (88%) Uniform ordering N = 28, (41%) * More than one response possible per participant 159 Report of the mid program evaluation of ‘take the lead’ Table 37: Number of CSOs undertaking duties relating to documentation/records management* ROLE OR RESPONSIBILITY NUMBER OF RESPONDENTS (N = 85) Supporting and participating in the administrative aspects of activities N = 78, (92%) Numerical profiling N = 29, (34%) Quality accreditation processes N = 42, (49%) Incident management N = 30, (35%) Maintaining staff credentialing register N = 39, (46%) Monitoring of nurses and midwives registration and enrolment N = 56, (66%) Assisting the health care team in obtaining information, reports or correspondence related to patient care N = 43, (51%) * More than one response possible per participant Table 38: Number of CSOs undertaking duties relating general administration activities * ROLE OR RESPONSIBILITY NUMBER OF RESPONDENTS (N = 72) Undertaking administrative tasks related to meetings that are held on the ward/unit involving medical, nursing and allied health staff N =62, (86%) Scheduling N = 43 (60%) Ensuring all relevant documents are available for the meeting N = 62, (86%) Progression of action items where appropriate N = 47, (65%) Assisting with the daily schedule for the health care team at ward/unit level N = 29, (40%) Ensuring that multidisciplinary ward rounds are completed in a timely manner N = 8, (11%) Ensuring relevant material is available to support the ward round N = 24, (33%) Organising travel and accommodation for ward/unit staff where required N = 18, (25%) * More than one response possible per participant 160 Report of the mid program evaluation of ‘take the lead’ 8.6.6 Impact of CSOs CSOs were asked if they had taken over tasks which had once been undertaken by their N/MUMs. Of the 76 CSOs who replied, 63 (83%) said they now undertook tasks which were once completed by their N/MUMs, and 89% thought that they had reduced the amount of time their N/MUMs spent on administrative tasks. Most of the tasks indicated reflected those outlined in the previous tables, for example rostering and entering Kronos. CSOs were also asked if they believed that their work had an impact on patient care. Of the 69 who replied, 59 (86%) felt that their work had not impacted on patient care. 8.6.7 Impact of CSOs on the work of other staff CSOs were asked about the duties that they were undertaking that supported the work of other (non N/MUM) staff. Examples are presented in Table 39. Table 39: Duties undertaken by CSOs EXAMPLES OF DUTIES CONDUCTED BY CSOS PREVIOUSLY UNDERTAKEN BY OTHER STAFF Allied health minutes. Allied health databases, allied health stock/stationery ordering. Database for Medical staff. Stay tuned, more to come Arrange family conferences for social worker. Do Pathlore database entry and other admin tasks to support CNE As a CSO in nursing admin, we have assumed roles that previous and current admin officers were/are doing Clinical ordering, they come to me when needing anything Entering courses into Pathlore, talking to nursing administration Faxing; Minutes; Filing; Booking venue; organising appointments Go to meeting and taking minutes for the health professionals Hand hygiene audits; updating Pathlore; updating registrations; taking minutes; typing minutes; web requisition orders; office max orders. Helping out the nurse educator, producing staff accreditation booklets for each staff member, keeping records of their training, basic admin tasks I have taken over for her I act as backstop to the Ward Clerk and to a lesser extent Ward Assistant. Answering telephones, cleaning wards, general running around I support the Ward Secretary by answering phones and liaising with relatives when required. I support Allied Health in regard to updating FIMs (Functional Independence Monitoring assessment forms)on a daily basis - this is particular to Aged Care and Rehabilitation 161 Report of the mid program evaluation of ‘take the lead’ EXAMPLES OF DUTIES CONDUCTED BY CSOS PREVIOUSLY UNDERTAKEN BY OTHER STAFF Minutes, ordering, communication between different staff, booking transport, ordering supplies, calling up for maintenance Ordering stock used to be undertaken by the ward clerk on one ward. The ID audit used to be undertaken by the CNE on one ward. Taking minutes of the falls meeting used to be taken by the CNC. Audit reports used to be prepared by the CNE on one ward Ordering stock. Updating staff health on Riskmate Ordering/tracking stock, performance reporting, data collation Photocopying; booking out staff; faxing documents; obtaining medical records Send request to and follow up with BIMS for the repair of medical equipments Signage, minutes, documentations, ordering, tracking Stores orders; retrieval of medical records; clerical support to other staff Surveys, flyers Taking minutes of meeting, entering request rosters Taking minutes of meetings, creating spreadsheet for Diabetes data There are many tasks as mentioned above once done by nurses now regularly undertaken by me: updating patient results and filing, culling old results, task spreadsheets, shift replacements for in charge when NUM is not working, typing a variety of documents for nurses, answering the telephone and assisting with non clinical enquires and delegating clinical enquiries, departmental systems and equipment rearranging for staff, communication and information support for Nurses Update bed summary sheets, Pathlore, order dressings and keep dressing trolley updated Updating the pt boards, stationary orders, multidisciplinary meeting stickers CSOs were then asked about the specific tasks that they perform to support the work of doctors, nurses and allied. Of the three groups, allied health received the most comments, rather than descriptions of tasks. CSOs were quite clear as to their contribution (or not) for doctors and nurses: they either gave examples, or indicated that they did not work with these groups. In relation to allied health, however, CSOs provided a number of reflective responses: either providing examples of tasks, or reflecting on why they have not contributed to the work of this group. Examples are presented in Tables 40 to 42 below. Table 40: Examples of tasks undertaken by CSOs to support medical staff SUPPORT OF MEDICAL STAFF Booking transport Complete the Intern roster on a 10 week rotation 162 Report of the mid program evaluation of ‘take the lead’ SUPPORT OF MEDICAL STAFF Creation of printed material - Signage, pamphlets, brochures Data collation for reporting and research Discharge scripts taken to pharmacy, collating notes and getting patient information for doctors Faxing pathology/Xray and ultrasound request forms I have only assisting one doctor the whole time I have worked here. It involved preparing a data sheet to which the doctors complete. I enter the results of the data sheet into a data base that If in rehabilitation I prepare paperwork for case conference Keep track of patients going to operating theatre, keep track of patient information coming through fax Library requests; faxing; organising new laptop, telephone Ordering medical stock Patient discharges, liaising with pharmacy, organising follow-up consultations Preparation of results for signing, liaison with Nursing staff on behalf of the doctors for follow throughs required. Maintenance of an orderly and efficient filing system Printing bedlists, ordering other tests Providing forms, making sure computer room is tidy and functional for the doctors This does not occur in theatres as such. By supporting the theatre manager I support the doctor's work by default (i.e. prosthesis reports, VMO payments) Word processing where necessary, some purchasing Table 41: Examples of tasks undertaken by CSOs to support nursing staff SUPPORT OF NURSING STAFF Ad hoc matters relating to pay and leave etc. Also ensuring the registration is updated. Organise performance reviews Alleviating the NUM of administrative tasks gives them more time to spend on the floor therefore supports the nurses Answering phone enquiries Any administrative queries re rosters, sick, FACS or A/L. Assisting in printing labels, getting patient folders, taking scripts to pharmacy, changing Diets for patients Check their roster and pay, make sure overtimes are noted by nursing salaries, support them with registration, filling out of forms, ordering medical supplies, help them to find information on the intra or internet 163 Report of the mid program evaluation of ‘take the lead’ SUPPORT OF NURSING STAFF Conduct audits; format forms, leaflets, policies etc; follow up on HR issues; IT support and advice Co-coordinating vacant shifts with casual and part-time staff looking for extra hours. Proacting specific shifts for CNE's, ie. EOC hours. Assisting new employees with recruitment documentation, orientation etc. Maintaining and updating an availability spreadsheet for casual staff Daily staffing, laminating. love laminating. Creating signs and posters, pay queries. Leave queries Data collation, organise maintenance, transcribe/write minutes, order/track stock EMS , phototyping , phone answering , filing patient notes I help them with any general pay questions; finding forms online; making signs ; ordering transport/meal etc online I help with their portfolios and anything they need I report maintenance problems. I regularly check that supplies are orderly and check general supplies around the patient beds eg gloves and cleaners Locating products, suppliers and purchasing details of equipment and supplies, maintenance issues on ward Make sure there are stethoscopes, signs for falls risks/fluid restriction/nil by mouth signs are put up Only organising the ward, having emergency bags clearly marked and labelled next to every bed, have charts labelled easier for bed changes Ordering clinical stock, notification of educational programs available to them, management of portfolios etc Ordering medical stock/ensuring obstetrics and midwife data collection data are correct Ordering, collecting and preparing notes for patients who have presented. Stock is available for their use Photocopying and printing of front sheet once patient being transferred to our ward, transferring/discharging patients, transport booking. Powerchart, patient discharges and taking patients to discharge lounge Purchasing medical supplies, payroll talk, keeping track of their accreditation/training/registration Queries they may have about their pay and entitlements. ; Print off information they make require for education or day to day tasks Supero uniforms courses Typing whatever they may need, and compiling and updating relevant work as needed. 164 Report of the mid program evaluation of ‘take the lead’ SUPPORT OF NURSING STAFF Updating roster on both hard copy and electronic systems with changes (ie sick leave, OT, filling shifts), adding staff to roster, changing shifts for nurses following approval by NUM) to ensure they are paid correctly. Assist them with the completion of forms such as sick leave, annual and study leave forms are all completed accurately and in a timely manner. Assisting them with pay queries, assisting casuals to work shifts Updating the patient boards Table 42: Examples of tasks undertaken by CSOs to support allied health staff SUPPORT OF ALLIED HEALTH STAFF A little help dependent on where I work - if there is an bedboard meeting where all the professionals go I prepare paperwork to assist them daily Administration cover for holiday leave Allied health professionals never asked me to help a lot but I helped whenever they need any As I am not fully covering the CSO role my contact with the above professionals is the same as it was as a ward clerk I support them as best I can administratively when asked Assist in purchasing Better relationship between NUM and all this professional workers Depends on how/if they use CSO. Slight but minimal impact Good documentation due to maintain acceptable level of stationery especially stock of form for documentation Has provided them with more clerical support so they are able to spend more time with patients and patient care I assist with ordering for the physiotherapists and other than that I don't help allied health at all I have had no impact on the role of allied health I have not really done too much work for the allied health team. I'm not sure why, maybe they don't that they can approach me. I have booked meetings for them I haven’t been involved with allied staff at all I suppose it reduces their work load It has some impact as all of these link in with our department and all are part of the multidisciplinary team. I am able to assist at all levels with provision of information and there are benefits to those staff also More time is spent on the patients instead of administrative tasks Not enough - they would like to use me more but I have been limited in the amount of time I am allowed to give them 165 Report of the mid program evaluation of ‘take the lead’ SUPPORT OF ALLIED HEALTH STAFF Not much in regards to my role Not much, I am present at Allied Health Bed Board meetings and make sure referrals are entered on the Ward Summary sheet. Ordering stock for the physiotherapy department, collecting patient information for discharges Prepare case conference info, arrange family conferences / occasionally assist with ad hoc tasks or projects Smoothing communication between NUM and allied health professionals The NUM is available and on the floor for allied health professionals to speak to. Access easier. NUM is in greater touch with what is going on in the ward There isn't much of an impact. I powerchart requests for them when they have been given a referral by the NUM in either the daily morning meeting or the allied health meeting once a week Timely communication Try to assist where I can, sometimes order things, get notes communicate details etc. 166 Report of the mid program evaluation of ‘take the lead’ 8.7 Details of case study Similarities Both NUMs describe the program as having a positive impact on them and their units. The impact they described: 1) ‘ttl’ identified and addressed core skills that NUMs need to succeed in their role. Both NUMs describe the process of nurses moving into the role of the NUM as an evolutionary process. “Nearly every NUM has come from a nursing background, and they have been a bedside nurse at some point or another – and then through a whole pile of reasons, whether it's natural progression, or whether they've done extra courses, or for what people have gone on maternity leave, or whatever happens – they find themselves in the nurse unit manager role. Some people actively seek it, but I think it happens to a lot of people…” (NUM1). This process left a gap in the skills that are required for management. “There's no training and there's really no guidelines and you know, a job description is just that, it's just a job description, but it doesn't tell you what the job is... it was interesting listening to a lot of them say, yeah, that they hadn't had any educational training or support – somebody says to them, 'where's your (whatever you call it) – Nets, or whatever, and they're like 'well what's that'….” (NUM2). One example of a learning opportunity was the role of leadership in the NUMs role. Previously NUM1, for example, had not realised the impact of organisational politics on her performance. “The thing I really liked about leadership, and I think again that's something that is very foreign to nurses now, is we do have to become a bit politically savvy. We do have to…. and I'd be the worst offender of that – I have absolutely no interest in politics, whatsoever, but I've realised that through having an increased awareness and being impressed by some of these people I've seen be involved in this course in running it, being involved in it and some of the NUMs you meet in the process of it – that you know you need to pick up your game was the message for me in that area. You can't just stick your head in the sand and think it's not going to impact on you – because as bedside nurses it doesn't, it doesn't impact on us in any shape or form, or not that we're aware of…. I'm sure it does to a degree, but we're completely unaware of it – but as managers you have to become a bit politically savvy. And you have to be able to have those talks – if you want to be heard, you need to present yourself professionally and educationally, and you know 167 Report of the mid program evaluation of ‘take the lead’ you can't do that if you're going to stay in the dark about it…. so I must admit when I left leadership, I thought 'I need to pick up my game a bit”. This skill gap had some obvious consequences, such as lower efficiency in running the wards. But it also brought unintended consequences such as lack of clarity of role and authority, as in the situation NUM2 described in her unit. But also as NUM1 describes it limits your power and influence in the organisation. “So you can go in there and have an opinion, because what happens if you don't feel comfortable with the knowledge that you have or if you have a lack of knowledge, or you feel like you can professionally present, then you don't seem so, and everybody else's voice gets heard and yours doesn't – and I think as nurses we under-estimate our power sometimes. You know we are the biggest workforce in the health and I think we can influence a lot of things, and I think we need to be aware of that, and raise that a bit more, but we need to be able to do that in a succinct and educated way – which we haven't been good at in the past I don't think” (NUM1). Both NUMs described modules that were more or less beneficial to them. NUM1, for example has been in her role for several years and has had a lot of experience handling the financial aspects of the unit. NUM2 has recently finished her postgraduate degree and felt that she received the information she needed through those studies. Overall, both accepted that ‘ttl’ had a different impact on each participant based on individual differences (such as breadth of managerial experience, previous knowledge and personality) and different unit needs and characteristics, but that it did not diminish the value of the program. “And I think look the difference has been that there were 700 and something NUMs I think across the state if I remember rightly at the time, and it was like, you were never going to be able --- there were going to be people in there that didn't need rostering, and there were people in there that didn't need financial management, because they'd been doing it to death for several years, and they were comfortable with it – but there was also going to be probably an equally large, if not larger group of people that were new to positions that didn't know that its format had changed who were being asked to take on extra things that they didn't know how to do, so they were desperate for rostering and financial management” (NUM1). 2) ‘ttl’ has reinforced and focused attention on concepts that have always been a part of nursing and health care management. One such example was the organisation skills that were discussed as a part of the lean thinking module.“...so I guess with the Take the Lead, it was interesting that other people started to see the concepts that have probably been around, you know have always been there, that they just haven't taken note of…. So even just going to 168 Report of the mid program evaluation of ‘take the lead’ the first one, one of the first things they said was about cleaning up – you know what I mean. Like just cleaning up and organising your work environment, and I've always been clean and tidy. But now when I go around the other areas are now clean and tidy and their marking their floors as a place for this, and so it's interesting – perhaps it's not affecting in my environment, but it's certainly taking effect in the areas around me” (NUM2). NUM1 expressed a similar view regarding her communication skills... “I think I had very good approachable communication skills, that stuff was all there basically, but it's that higher finesse thing like bigger bang for your buck I suppose. I felt quite comfortable having conversations and things with my staff and my patients, but perhaps not so much with hierarchy, and not so much on a major area level for example. Definitely through Take the Lead and EOC, my profile has been raised in this area health service, and I have been asked to step up and present at quite a few things I would have found reasonably intimidating before – but I can do that quite confidently now, and I feel quite comfortable with that, it doesn't concern me at all”. It was not only the skill that was reinforced but an awareness of unintended consequences of behaviours, such as the example given by NUM1 that described increased awareness regarding communicating style with patients and families. “... and I think when you have those conversations with patients or relatives that can be angry….. Like I was okay at that already, but I guess it's more teaching those skills to be still and listen. And one of the biggest things I learned was about being present in the room with the person you're with. That was a big thing for me. I would be a typical NUM, I'd be sitting here listening to someone, but I'd also have one eye on the computer and so on – and one on the floor to see what they're up to – so that was a big learning thing for me.” The program reinforced that knowledge and education can equate to more power in the organisation. For example NUM2 stated “I think if people have the knowledge and the skills, I think it puts them in a better position not to be that 'yes' person all the time, and often people want to argue, or don't agree with the decisions that are made and the things they're told to do, or feel that they have the capacity to argue a point or voice an opinion or express a different point of view – so I think the more educated and more skilled that people are…..”. Another concept that was reinforced by ‘ttl’ and EOC was that of prioritising and continuously striving for excellence in patient care. Both NUMs stated, that while patient care has always been at the heart of their role, the attitude toward care and interaction with patients and families has changed for the better: “I think the 169 Report of the mid program evaluation of ‘take the lead’ attitude, the patient care has changed, and I think it is great and there's a lot of interaction with families and patients ...“ (NUM2). 3) ‘ttl’ gave N/MUMs recognition and acknowledgement of the importance and contribution of their role. Both NUMs describe their role as one that was previously not overtly visible or recognised in the organisation. It was suggested that this could be because of the gradual evolution from charge nurse to NUM, but that the role and workload kept growing without any change in support or training. ‘ttl’ was the first time that NUMs needs and impact as leaders was recognised and brought to the forefront. “Yes, I think that was the first and foremost thing, someone had recognised that NUMs around the place were drowning, absolutely drowning, but you know the upshot of that is that I believe patient care was suffering in a lot of places” (NUM1). The NUMs were also recognised by other professional disciplines that work with the unit. “There was this total recognition from other disciplinarians as well and I think in particular medical staff here I would have to say, and I'm sure it's the same in other places, where they just wanted this person, this charge nurse that they knew to be able to run this, with no recognition of how much that role has changed and evolved and what else was being required from that person. You know, the time had gone where you could just be here to see every doctor that was associated with your unit …. So yeah… I think it was a process that had to happen, and I think the recognition from the nursing and midwifery office is really positive” (NUM1). One dimension of the recognition was the fact that considerable resources had been put towards this program. This manifested itself, for example, in the fact that rural NUMs were flown into metropolitan centres and provided accommodation. Another issue was that wards had to find replacements for the NUM while she was away. Whilst this created certain upheaval for the units, it also highlighted that the NUMs education and training is a priority to NSW Health, which added to the recognition of their importance to the organisation. 4) ‘ttl’ provided increased role clarity, shared experiences and a shared language for participating NUMs and also their colleagues and their managers. The ‘ttl’ program, along with the role definition and EOC gave the NUMs a shared understanding and clarity of their role despite unit and organisational specific differences. The fact that the program was mandatory meant that many (eventually all) NUMs had gone through a similar experience. This gave the NUMs a common language. NUM2 described how this effected her interactions with management: “... a lot of the things we've been doing is we've been saying to management, we don't 170 Report of the mid program evaluation of ‘take the lead’ like this, this is why we don't like it, and this is how it impacts on us, and this is how it impacts on our care, and until recently there's been no forum for that, because as I say with management it's top heavy - with the whole Take the Lead and introduction of the Essentials of Care, they're recognising that at various levels, you do need to listen…. so we've managed to get some changes, but I think had we tried to do this a year ago, before Essentials of Care, there's no way they would have listened”. One example of shared language was the prioritisation of patient care. As discussed in the section describing reinforcement, patient care was always a part of the unit and its’ priorities, for both NUMs. NUM1 describes how when issues arise the focus is on problem solving so that patient care is enhanced. Through ‘ttl’ and the EOC programs it has become a part of the ‘language’ of the unit. “There is always a patient focus for some staff, not necessarily for all staff. What we've done is a lot of work around values and things through EOC and one of the amazing things that came out I think for the staff is that when you brought them all together, they were all here for the same reason, and they all wanted the same outcome. So whether or not they liked each other, they actually all had this common thing that they wanted to reach, and that was good patient outcomes and patient care and all of those things. Even that recognition of bringing that enormous amount of people together and saying 'this is what you said, you're all on the same pay, you all want the same outcome, so why don't you all work together to get there' and so I think that's probably raised that a lot. What you find is that people are less tolerant of staff who don't have that focus” (NUM1). The recognition, together with the increased awareness of their roles not just as managers, but as influential leaders also had an effect on empowering the NUMs to take more initiative to represent their perspective on patient care, staff needs and their own needs. NUM1 commented that “It's definitely given me, and it's made me realise that it's a reasonably powerful position, it didn't feel like that before, but it is you influence a lot of people by how you manage yourself really, and I guess I didn't realise the impact that that had beforehand. You know you think you come in here and you do a job and that's it, but you know the way you speak, the way you speak to patients, the way you speak to staff the way you speak to visitors, the way you speak to other departments, the working relationships you build with those different people and departments, you set the standard very much I think, and you're actually very influential on a lot of peoples' lives and you don't realise that. I certainly didn't realise that before. So it's made me much more aware of that, and much more respectful of that”. 5) Networking was identified as one of the strong benefits of the program 171 Report of the mid program evaluation of ‘take the lead’ Both NUMs identified that the N/NUM role is very isolated and that it is difficult to ascertain whether you are doing your job well or not. The NUM support network that resulted from the program was a safe place to ask questions and a source of ideas and information. 6) CSO were a much needed addition to enable and sustain the ability of the NUM to engage with core clinical and managerial roles rather than administrative tasks. Although, each NUM had a different experience with their CSO, both NUMs viewed the impact of the CSO as a positive one. NUM1, who has had a full time CSO for the last 10 months stated that once the CSOs were deployed “you'd never get a NUM to give one back, that's for sure” and maybe even more convincingly that “I'd give you my child before I gave you my CSO…”. NUM2 that shares her CSO with another unit, and has only had the position filled recently, is still learning how to best utilise the CSO in her specific situation. “I guess it's been, we're just trying to work out what we can give her. It's very hard to give over some of the tasks that you do when you've been doing them for so long, and often you don't realise that these are tasks that you could…”. Both have had less administrative tasks to do which has freed them up to do other things like being on the ward more and interact with staff and patients. Differences The differences identified in the interviews were in the perceived source of the change catalyst and the types of changes made. 1) Source of change -NUM2 believes that she had previously gained the content knowledge that was in ‘ttl’ from post-graduate studies, and that ‘ttl’ did not directly influence any specific changes in her unit. Most of the changes are attributed to EOC and staff initiatives that resulted from it. NUM1 has instituted a number of ‘simple changes that have had a big impact’ that she attributes to ‘ttl’. She too recognises the benefits of other programs on the positive changes in her unit. 2) Changes implemented and sustained – each of the units had different challenges and different needs that stem from, amongst other things, their function, their organisation, their staff characteristics and their managers’ leadership style. Time and staff were resources that were scarce in both cases, but both describe multiple changes that have occurred since ‘ttl’ and EOC. Below are some 172 Report of the mid program evaluation of ‘take the lead’ examples from each unit. Some examples of the changes that were implemented in NUM2’s unit are: Better collaboration between her and her staff – “I think there's definitely much more, as I said, yes, better collaboration, and I think that I feel like I have a goal for them, which I want them to achieve... and I think that my approach is to try and work towards that goal”. Empowers and encourages her staff to be more autonomous – “My ultimate goal is to have a completely, well not completely, but a nursing driven unit that is autonomous and self-sufficient, and can function with/without me, and is not dependant on individual members ... And I guess having that in mind, I've changed…like I feel like I'm endeavouring to give them more autonomy on how the unit functions”. A number of staff initiatives were described, such as a unit ‘think tank and employee of the month was created as an initiative to boost morale...”because as I said, morale was so bad. And now employee of the month is like, like a status ... the doctors are even wanting to know are they, can they be voted employee of the month”. Other initiatives were instigated through discussing issues that the ward could improve and by “Letting them talk about how they want to, how they're going to drive it – so they have done 101 things that are ultimately influencing how they practise. So they've done a mission statement. They've come up with new ideas all the time to consider what are issues, so for instance, simple things like ---- you know the bed areas weren't being cleaned properly after a patient was discharged and before a new patient came in, so they did these little admission packs – so basically even when they're pushed for time, they can bin everything, they've got an admission pack ready to go….. um, so basic stuff like that”. Overall, NUM2 feels that there has been considerable change in the unit and in her managerial style. “There's been a huge change in my work… like in my unit, and I don't know if that's related to the take the lead. I don't feel that my management technique, or style, or whatever has changed – but I do feel that the environment in the last 12 months has started to change, and I mean I still do what I do, but I kind of let the staff --- my idea of management is not telling people what to do, but letting, you know, letting them do what… letting them run the show”. Some examples of changes made in NUM1s’ unit are: Lean thinking – this module is described as having had a huge impact on her work and unit. Firstly it was about awareness and reflection on practices that part of the day to day in the unit. “There was a lot of wastage. There was a 173 Report of the mid program evaluation of ‘take the lead’ lot of waste of time, there was a lot of stuff we did, just because we always did it like that, or you know where you were bombarded with these things that you thought that you had to do, because that's what you were told you had to do…. So being able to realise that that may not be the case, and realising that you can have the power to say 'well I'm not doing it that way it's a bit of a waste of time, can't we do it that way' that sort of stuff. So that was good” (NUM1). The change she describes she made is simple, she now begins her day on the ward and does not turn her computer on until 10am in the morning. Before ‘ttl’ she was overwhelmed with the office work and emails. The module initially made her aware of the impact of prioritising different roles and more importantly, it gave her the confidence and opportunity to try and change it. “So you know that was something very simple to change and very easy to change, and you know why did I not think of that before. I think I was so bogged in it, and it just was this thing of giving you the time to look at it from outside, giving you some skills to look at it with, and making a decision to do something and see how it went. Because it was quite frightening. I know that sounds stupid, but you think to yourself, 'oh if I'm not there on the emails I'll get a 'bolicking' and I'm meant to be somewhere where I'm not'”. “...but certainly I guess that was the big thing and big change for me when I first came back from Take the Lead, that simple making that contact with my staff and patients in the morning, as opposed to being completely office driven”. The impact was significant as there have been less staff complaints, less patient and family complaints and more compliments. Personally, her job satisfaction rose and importantly “the other thing that that did for me was made me remember why I was a nurse in the first place. Why I wanted to do that. Because you know I think nearly everyone becomes a nurse for the same reason. Nobody wants to do any harm, and people want to help people and you know it's a privilege to be a nurse and to be involved with people, intimately at times, in peoples' lives – but as a manager you become more and more disengaged from that, and more and more dissatisfied I think – because that's not why you came into nursing, and you forget those bits, so it's so nice to go out there and chat to patients, and chat to staff and realise they're not all wicked witches who're trying to make your life unbearable...” . Through ongoing communication with staff regarding her experience in the program, especially around critical communication, some staff were inspired to try and increase communication with the ward and began an internal newsletter. This caught on and has created a more open team environment. 174 Report of the mid program evaluation of ‘take the lead’ Leadership and succession planning had always been an issue in her ward, as her role is very difficult. The leadership module encouraged creating a succession plan so that if she needs to be away from the unit, there are people who can take over seamlessly. This is currently a work in progress but as she stated: “when I first started in this job there was nobody who wanted to relieve as the NUM 3 and there was nobody who wanted to relieve as the NUM 1, and I now have two people who have expressed interest to relieve as the NUM 3, and we have four people who have had expressions of interest to relieve as the NUM 1 ---- so that succinct planning is starting to happen, and people are starting to recognise, because we try to set it up so that people don't fail”. This is a part of a slowly evolving change in attitude towards professional development and training. Whereas previously the attitude was that professional development was negative, as it will lead to extra work and responsibilities, now there is a shift in attitude as discussed previously, that knowledge is power and provides opportunities. Coaching- a local initiative that began in their regional area was to have continued support through coaching for NUMs that have finished the ‘ttl’ modules. NUM1 was one of the first in the program and currently coaches 6 other NUMs that have finished ‘ttl’. “I got a coach out of it as well, which I find invaluable. But certainly the feedback from the coachees I've had as well, and it's really nice to watch people start to develop through their issues and come up with the solution themselves, you know it's very powerful for you personally, but it's very gratifying when you can help someone else do that too. So that's been a fantastic thing as well”. This initiative is a result of the need that was identified for continued support in order to identify, enable and sustain change initiatives as well as to maintain the high levels of motivation that follow the program. NUM1 relates this network support to the powerful impact that the networking aspect has had on her motivation and work. “I think a sharing of knowledge will come out of it …. Because sometimes what happens is in my experience, my own personal and other peoples' is when you've worked in a place for a while and you've moved up into these positions, you feel very unable to ask for help maybe in that environment. Like if it's an environment that's reasonably intimate, and it's very difficult to look like the dumb, dumb, NUM for a while, once you go to work and go 'I don't know what you're talking about', or 'I don't know how to do that' and people can feel quite threatened by that. Sometimes it's much easier when it's a face that you've met at something, that you've networked with that doesn't directly work with you, that's not in 175 Report of the mid program evaluation of ‘take the lead’ your same hospital, and lots of cases not in your area health services, you can be much more open and honest with those people I think in some cases. So I definitely think there's a sharing of knowledge about that. I've had several phone calls from other NUMS in this stage that I've met through Take the Lead myself”. The descriptions above have focused on the impact that ‘ttl’ has had on two NUMs and their units. It has attempted to compare the experiences of the two, by identifying differences and similarities. It is clear from both NUMs, that ‘ttl’ has had a positive impact on them and their units. They differ in the perceived personal impact. NUM1 identified several significant changes that she made that were due to ‘ttl’ and described how they were related to the program. NUM2 felt that it was important as it enabled much needed attitude and cultural change regarding the N/MUM position. Change is a multi-faceted process and both NUMs describe the need for change in their role and in their units. Each was experiencing multiple challenges due to organisational and situational characteristics of their units. To both it was clear that change was and still is needed. 176