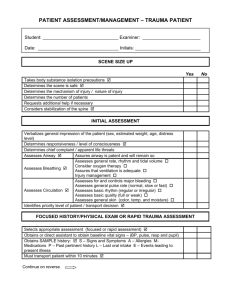
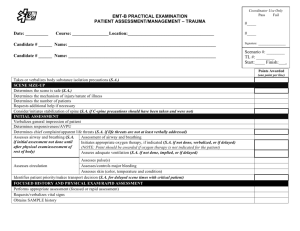
PATIENT ASSESSMENT/MANAGEMENT – TRAUMA PATIENT
advertisement

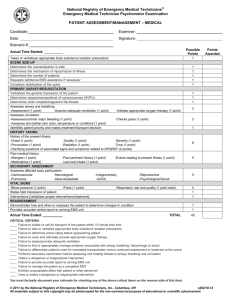
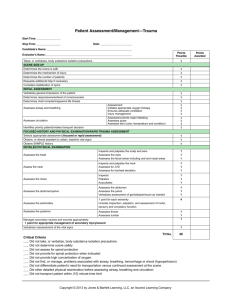
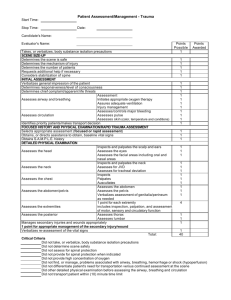
PATIENT ASSESSMENT/MANAGEMENT – MEDICAL PATIENT Student: ______________________________ Examiner: _______________________ Date: ________________________________ Initials: __________________________ SCENE SIZE UP Yes No Takes body substance isolation precautions ; Determines the scene is safe ; Determines the mechanism of injury / nature of injury Determines the number of patients Requests additional help if necessary Considers stabilization of the spine ; INITIAL ASSESSMENT Verbalizes general impression of the patient (sex, estimated weight, age, distress level) Determines responsiveness / level of consciousness ; Determines chief complaint / apparent life threats Assesses Airway ; Assures airway is patent and will remain so Assesses general rate, rhythm and tidal volume Consider oxygen therapy Assesses Breathing ; Assures that ventilation is adequate Injury management Assesses for and controls major bleeding Assesses general pulse rate (normal, slow or fast) Assesses Circulation ; Assesses basic rhythm (regular or irregular) Assesses basic quality (full or weak) Assesses general skin (color, temp. and moisture) Identifies priority level of patient / transport decision ; FOCUSED HISTORY/PHYSICAL EXAM Signs and Symptoms (assesses history of present illness) Respiratory Cardiac Onset Provokes Quality Radiation Severity Time Interventions Onset Provokes Quality Radiation Severity Time Interventions Continue on reverse Altered Mental Status Described Onset Duration Associated symptoms Any trauma Interventions Seizures Fever Allergic Reaction Poisoning / Overdose Environmental Emergency Obstetrics Behavioral Hx of Allergies What exposed to Exposure length Effects Progression Interventions Substance When How much Time period Interventions Pt weight Effects Source Environment Duration Conscious Effects – general or local Pregnant? How long? Contractions? Bleeding or discharge Need to push? LMP Crowning How do you feel Suicidal? Treat to self or others Medical problem? Interventions PATIENT ASSESSMENT/MANAGEMENT – MEDICAL PATIENT Continued SAMPLE HISTORY CONTINUED Yes No Allergies ; Medication ; Past pertinent history ; Last oral intake ; Events leading to present illness (rule out trauma) ; Performs focused physical examination Assesses affected body part / system or, if indicated, completes rapid assessment Baseline vital signs (BP, pulse, respiration’s, pupils) ; Interventions (oxygen, med assistance, shock mgt, etc) Transport ; Detailed physical examination – verbalizes the consideration of: ONGOING ASSESSMENT (VERBALIZED) Repeats initial assessment Repeats vital signs Repeats focused assessment regarding patient complaint or injuries Checks interventions Must complete patient assessment within 10 minutes ; ATTEMPTS 1 2 3 INSTRUCTOR COMMENTS: ; = CRITICAL CRITERIA. NOTE: PASS _____ FAIL _____ Denote whether: MidTerm or ASST. INSTRUCTORS, PLEASE MAKE SKILL LOG ENTRY. Final