Bringing Nurses and Caring Back to the Bedside with the Virginia
advertisement

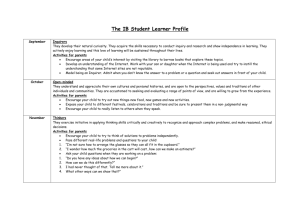
Reigniting the Caring Fever in Nursing Nursing Leadership Institute, South Carolina June 5-7, 2013 Dana Nelson-Peterson, DNP, MN, RN Virginia Mason Medical Center, 2013 © Objectives By the end of this session the participant will be able to : List the five caring principles of Swanson’s Nursing Caring Theory Describe one way to use a caring principle in daily nursing practice Understand how one medical organization is using a management system and nursing theory to implement a nursing professional practice model Virginia Mason Medical Center Strategic Plan © 2011, Virginia Mason Medical Center Virginia Mason Medical Center •Integrated health care system •501(c)3 not-for-profit •336-bed hospital •Nine locations •500 physicians •5,500 employees •Graduate Medical Education •Research Institute •Foundation •Virginia Mason Institute Virginia Mason Production System The Virginia Mason Production System (VMPS) is a management method that seeks to continually improve how work is done by identifying and eliminating waste and inefficiency in the processes that are part of the health care experience. Foundational Elements • Geographic assignments • Documentation near the patient • In room handoffs • RN:PCT integration • Huddles every shift • Hourly rounds by caregivers • Daily Leader rounds • People Link Boards updated and staff huddles done monthly © 2011 Virginia Mason Medical Center Results Decreased walking Decreased “hunting and gathering” Decreased time for morning cycle of care Decreased falls Increased throughput Increased communication with RN, PCT, and Patients Increased patient and staff satisfaction Conditions were optimized for the extraordinary patient experience… What’s missing at VM? • No common language for talking about caring • No shared model of professional nursing • • practice at VM Many models of professional nursing practice to choose from Opportunity for VM to define what our model of nursing care is using the tools of VMPS Great Thinkers Nursing: What it is and What it is not Nursing Theory Nursing theory is the term given to the body of knowledge that is used to define or explain various aspects of the profession of nursing Dorothea Orem (Self Care Deficit theory) Virginia Henderson (Need Theory) Rosemarie Rizzo Parse (Human Becoming Theory) Hildegard Peplau (Interpersonal relations) … and many others Nursing theory In general… • Provides a basis to improve practice • Provides standards for practice • Shared mental model Purpose for nursing Guides education, research Caring “A nurturing way of relating to a valued other towards whom one feels a personal sense of commitment and responsibility.” Kristen Swanson, 1991 Caring • Patients and their families • Teams • Self Caring Principles • Knowing • Being With • Doing For • Enabling • Maintaining Belief Knowing • Striving to understand an event as it has meaning in the life of the other • Avoiding assumptions Assessing thoroughly Seeking cues Centering on the other Engaging the self of both Being With • Being emotionally present to the other Being there Conveying availability Enduring with Sharing feelings Not burdening Doing For • Doing for others what they would do for themselves if it were at all possible Performing competently, skillfully Comforting Anticipating Protecting Preserving dignity Enabling • Facilitating the other’s passage through life events and transitions Informing/explaining Validating/giving feedback Supporting/allowing Focusing Generating alternatives/ thinking it through Maintaining Belief • Sustaining faith in the other’s capacity to get through an event or transition and face a future with meaning Believing in/holding in esteem Offering a hope filled attitude Going the distance Offering realistic optimism Helping find meaning Project Proposal Bringing Nurses and Caring Back to the Bedside with the Virginia Mason Production System Goals: Improve Patient Experience Improve Staff Satisfaction and Engagement Improve Patient Outcomes What We Have Done So Far: • Curriculum development and education using the tools of VMPS Innovation, visioning, idea generation, standard processes, newspapers • All inpatient units and across Oncology • • • Service line 12 Off Site Retreats with Kristen Swanson 14- 2 Day Off Site Collaboratives ~550 team members have participated Putting it all Together Bringing it all to practice Concierge Cart Huddle Cards Applause Cards Examples Badge Hangers Internal Website Further Work • Unit Level Caring • • • Boards Caring Moments in Daily Huddles Caring Exemplars Caring Standards Team Pledges Unit Quiet Time “Get to know your team members” monthly exercise Virginia Mason Nursing Model of Care © Bringing Caring Back to the Bedside Connie Hirnle, MN, RN-BC; Deborah Kelly, MN, RN; Niki Kirby, BSN, RN; Shirley Klakken, BSN, RN; Dana Nelson–Peterson, MN, RN OVERVIEW/BACKGROUND Virginia Mason Medical Center is developing an innovative nursing model of care that integrates key elements of The Caring Theory, created by nurse theorist Kristen Swanson RN, PhD, FAAN, with the Virginia Mason Production System© (VMPS) 1.Virginia Mason Medical Center has used the tools of VMPS to reduce waste so that nursing staff can increase time spent at the bedside. Swanson’s Caring Theory 2 RESULTS Before you began the Retreat: After you completed the Retreat: I had a good understanding of how my caring impacts I have a good understanding of how my caring the patient experience. impacts the patient experience. Strongly Disagree Agree Strongly Agree Strongly Disagree Agree Strongly Disagree 2 27 8 Disagree 0 2 Agree 1 0 36 I had a good understanding of the caring concepts and felt I role-modeled them well. Strongly Disagree 0 Disagree 12 Agree 23 Strongly Agree 3 I have a good understanding of the caring concepts and feel I can role model them well. Strongly Disagree 0 Disagree 0 Agree 13 Strongly Agree 25 I was comfortable in maximizing caring moments and I am comfortable in maximizing caring moments coaching opportunities as they relate to service and coaching opportunities as they relate to excellence. service excellence. Strongly Disagree Agree Strongly Agree Strongly Disagree Agree Strongly Disagree 11 24 3 Disagree 0 17 Agree 0 0 21 Patient Experience: GOALS The goals for the project focused on three areas: •Improve Patient Experience •Improve Staff Satisfaction and Engagement •Improve Patient Outcomes METHODS • “ staff worked really well together, everyone pitched in regardless of their job description or title” • “you definitely took care of my concerns and I thank you for hearing me, and taking my concerns seriously: • “every staff member were professional, caring and encouraged me every step of the way” Staff Satisfaction and Engagement: • Renewed passion and engagement for nursing practice • A tangible change in the culture of caring on the units • Significant change in staff engagement scores (Press Ganey) across all units •Identified three inpatient medical-surgical nursing units as pilot areas; the Unit teams consisted of Unit Nursing Directors, Clinical Nurse Leaders, RNs, and Patient Care Technicians •Participants attended two day off-site Caring retreats with follow-up via cohort learning collaboratives where they report their progress •Reflective practice strategies were used to role model caring experiences and elicit reflective narratives from participants •Teams designed caring practices using VMPS tools during the retreat for testing and implementation on their units •Guidance team conducted on-going Caring Rounds CONCLUSION In a highly technical and fast paced medical environment it is possible and imperative to include basic caring principles to improve patient care and staff satisfaction. An unexpected outcome is the engagement of staff to create a legacy for future professional nursing practice at our organization. C. (2011). Transforming Health Care. Virginia Mason Medical Center’s pursuit of the perfect patient experience. Productivity Press , New York, NY. 2 Swanson, K.M. (1991). Empirical development of a middle range theory of caring. Nurs Res. May-June 40(3) pp 161-66. 1Kenny, This work was made possible through a grant from the Arthur Vining Davis Foundation Compassion Fatigue (CF): Evaluation of a CF Intervention Using Swanson’s Theory of Caring and The Virginia Mason Production System (VMPS) Dana Nelson-Peterson, DNP, MN, RN; Deborah Kelly, MN, RN; Niki Kirby, MSN, RN OVERVIEW/BACKGROUND Caregivers of patients who are facing life-limiting illnesses are particularly prone to compassion fatigue, a gradual lessening in compassion over time due to inability to help their patient’s disease progression (Vachon & Huggard, 2010). Compassion fatigue remains a fairly new phenomenon in nursing. As a model of care was implemented across the Oncology service line, education and strategies to recognize and alleviate symptoms of compassion fatigue were included to optimize our team’s ability to care for patients/family, team members and self. RESULTS The following questions were asked of the Oncology Service Line participants to evaluate the effectiveness of the intervention surrounding compassion fatigue. I have a good understanding of how my caring impacts the patient experience. Before Retreat Strongly Agree 36% The project focused on development, planning, implementation and evaluation of an intervention to address compassion fatigue and care for self, teams and patients across the oncology service line at Virginia Mason. The intervention focused on creating a shared model of nursing care blending Dr. Kristen Swanson’s (1991) Theory of Caring with interventions for addressing compassion fatigue using the principles of the Virginia Mason Production System (VMPS). After Retreat Strongly Agree Agree 33% Agree 62% 66% I am comfortable in maximizing caring moments and coaching opportunities as they relate to service excellence. After Retreat Before Retreat Strongly Agree Agree 18% Study Question: Does an educational intervention influence the participants’ ability to understand the impact of caring and compassion fatigue on both the patient’s experience and the participant’s delivery of care? Strongly Agree 38% 60% Agree 74% I have a good understanding of compassion fatigue and the impact it might have on my care delivery. DESIGN/ METHODS Before Retreat After Retreat Strongly Agree 23% Agree Strongly Agree 36% Agree 64% 63% I have a good understanding of the caring concepts and feel I can role-model them well. After Retreat Before Retreat 19% Design: Descriptive non-experimental pre-post design Strongly Agree Agree Strongly Agree Agree 39% 61% 68% Methods: Oncology service line (Hematology-Oncology clinic, Oncology Infusion Center, Radiation Oncology Clinic and the Oncology inpatient nursing unit) team members (n=111) participated in a two day retreat that included education regarding compassion fatigue while creating a model of care delivery incorporating the theoretical framework for caring using the tools of VMPS. • During these retreats and subsequent collaboratives, opportunity for self-renewal and team building was created through individual and group work. • Creation of a shared vision and definition of foundational elements of a care delivery model that focus on caring for patients, self and teams occurred. • Identification of strategies to identify, mitigate and prevent compassion fatigue were developed. I have a good understanding of compassion fatigue and how it might impact the patient experience. Before Retreat 24% Strongly Agree Agree 64% After Retreat Strongly Agree Agree 37% 62% OUTCOMES/CONCLUSIONS Outcomes: The effect of the intervention was evaluated through data analysis using the 2 x 4 chi square test applied to the pre-post evaluation questions surrounding caring and compassion fatigue which resulted in statistically significant shifts at the p<.0002 on all data points with an enhanced awareness and application of incorporating strategies around demonstration of caring and mitigation of compassion fatigue into their practice. Visioning Exercise Implementation Plan Conclusions: Results of this project suggest the need to be cognizant of the burden and consequences associated with compassion fatigue that may be experienced by the oncology caregiver. Designing interventions directed towards addressing and alleviating compassion fatigue has a positive effect on both the delivery of care and the patients’ experience Swanson, K.M. (1991). Empirical development of a middle range theory of caring. Nurs Res. May-June 40(3) pp 161-66. © 2013 Virginia Mason Medical Center Vachon, M., & Huggard, J. (2010). The experience of the nurse in end-of-life care in the 21st century: Mentoring the next generation. In B. Ferrell & N. Coyle (Eds), Oxford textbook of palliative nursing (pp. 1131-1155). New York: Oxford University Press. Results • Standards for care developed around: Building a caring environment Creating a climate of emotional support Developing caring relationships Mistake proofing communication and commitments to optimize care Results Staff Satisfaction and Engagement: • Renewed passion and engagement for nursing practice • A tangible change in the culture of caring on the units • The “Caring Fever” • Significant change in staff engagement scores (Press Ganey) across all units Patient Experience: • “Staff worked really well together, everyone pitched in regardless of their job description or title” • “You definitely took care of my concerns and I thank you for hearing me, and taking my concerns seriously” Professional Practice Model • Using VMPS tools, creating a Professional Practice Model for nursing care delivery throughout organization: American Academy of Critical Care Nurses (AACN) Synergy Model for Patient Care + Swanson’s Theory of Caring Principles of the AACN Synergy Model for Patient Care • “a conceptual framework describing a patientnurse relationship that acknowledges the primary importance of nursing care based on the needs of patients and their families.” • “The fundamental premise of the Synergy Model is that patients’ characteristics drive nurse competencies. When patient characteristics and nurse competencies are in synergy, optimal patient outcomes are more likely to occur.” AACN Synergy Model Patient Characteristics • Stability • Complexity • Predictability • Resiliency • Vulnerability • Participation in • • decision making Participation in care Resource availability The eight patient characteristics span the continuum from health to illness. AACN Synergy Model Nurse Competencies • Clinical Inquiry • Caring Practice • Response to Diversity • Advocacy/Moral • • • Agency Facilitation of Learning Collaboration Systems Thinking The eight nurse competencies span the continuum of skill levels from competent to expert. AACN Synergy Model In the synergy model, when the skills of the nurse are matched with the needs of the patient, the care is “synergized” and optimal patient outcomes are achieved. Innovation event • 2 day event • 18 Nurse leaders throughout organization • Attention, escape, movement exercises Voice of the patient Current state Word play 7 Ways from Nature Fishbone exercise Conceptual Model for Care Management Services-draft . The Future • Service Lines/Organizational Spread • Nursing practice throughout VMMC Orientation/On-boarding/Residency Program Integrated plan of care Professional Development and Recognition Program Nursing Documentation … and beyond Nursing through Regional presentations, Publications, Academic partnerships, GME, Virginia Mason Institute and others Questions? Thank You!