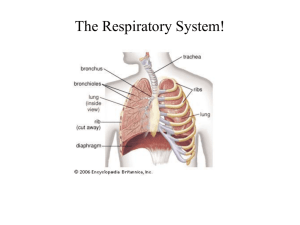
Respiratory System
advertisement
Anatomy RS #27 September 3, 2008 1:00-2:00 PM J. R. Churchill, Ph.D. judy.churchill@drexelmed.edu TOPIC: RESPIRATORY SYSTEM Suggested Readings: Ross Chapter 19, Wheater Chapter 12 OBJECTIVES: 1. Describe the various portions of the respiratory system and relate each region’s histology to its function. RESPIRATORY SYSTEM: DELIVERS OXYGEN FROM AIR TO BLOOD AND REMOVES CARBON DIOXIDE FROM BLOOD. Two Functional Components: 1. Conducting Portion : nasal cavities and associated sinuses, pharynx, larynx, trachea, bronchi and conducting bronchioles including the terminal bronchioles. Air is warmed, moistened and freed of particulate matter ("conditioned"). Olfaction occurs in the nasal cavities. 2. Respiratory Portion: respiratory bronchioles, alveolar ducts, alveolar sacs and alveoli. Interface for the passive exchange of gases between air and blood. Structure maximizes surface area in contact with air and has a large number of capillaries for gas exchange. Overview of conducting airways: 1. Lined by a mucosa that consists of the lining epithelium and the immediate underlying layer of connective tissue, the lamina propria. The lamina propria consists of loose fibro-elastic connective tissue (FECT) and may contain lymphoid aggregations of variable size. A mucosal layer is always present along the conducting airways. 2. A submucosa formed of CT and/or support elements formed by bone or cartilage or a smooth muscle layer encircle the conducting airways and show major variations depending upon the region. These variations often permit recognition of the class of airway that is seen in a micrograph. 3. In areas not immediately resting upon bone, an outermost layer of connective tissue (the adventitia) merges with surrounding tissues. THE NOSE IS A HOLLOW ORGAN COVERED WITH SKIN, SUPPORTED BY CARTILAGE AND BONE, AND LINED WITH A MUCOUS (MOIST) MEMBRANE 1. A nasal septum formed of hyaline cartilage separates it into two passages and forms the medial wall of each nostril 1 2. The vestibule is a dilated entryway continuous with surface skin. It has many coarse hairs near its external opening to filter out larger particles from incoming air. Sebaceous glands and eccrine sweat glands are also present. 3. Paranasal sinuses are sacculations from the nasal cavity that extend into nearby bones. There are 4: frontal, sphenoidal, maxillary, and ethmoidal sinuses. 4. The surface area of the lateral wall is increased by shelf-like conchae (turbinates) NASAL CAVITIES HAVE 2 DIFFERENT MUCOSAE: Respiratory mucosa: 1. Pseudostratified ciliated columnar epithelium containing goblet cells ("respiratory epithelium") formed of five cell types: ciliated cells, goblet cells, brush cells, small granule cells, and basal cells 2. Highly vascular lamina propria containing numerous tubuloacinar, seromucous glands. 3. Mucosa rests directly on the bone or cartilage tissue that forms walls of nasal cavity and paranasal sinuses. 4. Deeper levels of the lamina propria contain a type of cavernous erectile tissue formed by a plexus of large, thin-walled veins that normally serve to warm incoming air. In response to irritation the plexus can distend, blocking passage of air through that nostril. Olfactory mucosa: 1. Lines roof of nasal cavity over superior concha and adjacent nasal septum. 2. Olfactory epithelium is thicker than respiratory epithelium (more layers of nuclei are visible), and is free of goblet cells. 3. Four cell types - olfactory receptor cells (bipolar primary olfactory neurons), sustentacular (supporting) cells, brush cells and basal cells. 4. Lamina propria contains Bowman's glands (tubuloalveolar serous glands that provide fresh solvent for aromatic substances for detection and removal) and olfactory nerves formed entirely of large diameter unmyelinated axons. PHARYNX CONNECTS THE NASAL AND ORAL CAVITIES TO THE LARYNX AND ESOPHAGUS 1. The pharynx is a passageway for food and air and is divided into the nasopharynx and oropharynx. 2. The nasopharynx is lined regionally either with respiratory epithelium (mostly) or a stratified epithelium in more inferior regions where the soft palate comes into contact with the posterior pharyngeal wall (stratified columnar then stratified squamous) 3. The surfaces of the oropharynx may come into contact with each other or by passing food and is lined by a minimally keratinized stratified squamous epithelium EPIGLOTTIS AND LARYNX ARE SPECIALIZED STRUCTURES FOR PROTECTION AND VOCALIZATION: 1. Epiglottis is mostly covered by stratified squamous epithelium; the central core is of elastic cartilage that often is replaced by fat with age. 2 2. Larynx is a box-like structure framed by cartilage and bound together by ligaments and muscles. Laryngeal epithelium is pseudostratified and ciliated (except at points of wear and tear such as over the vocal folds); chiefly contains ciliated cells, basal cells and goblet cells. 3. From superior to inferior the lumen of the larynx presents three regions - the vestibule, ventricle and the infraglottic cavity. Ventricular and vocal folds are superior and inferior boundaries of the ventricle respectively. 4. Ventricular (vestibular) fold (false vocal cord) is a fold in the mucous membrane that is covered by pseudostratified columnar epithelium and contains a large number of seromucous glands. 5. Vocal fold (true vocal cord) is covered by stratified squamous epithelium and contains vocal ligament and vocalis muscle (voluntary, skeletal muscle type). TRACHEA AND EXTRAPULMONARY PRIMARY BRONCHI FORM SEMI-RIGID TUBES FLATTENED POSTERIORLY: 1. Trachea extends from the larynx to middle of thorax; divides into primary bronchi of lung. 2. Mucosa - ciliated pseudostratified columnar epithelium supported by a characteristic thick basement membrane and containing three main cell types (ciliated cells, goblet cells and basal cells). - lamina propria consists of loose fibro-elastic connective tissue which also contains lymphoid aggregations of variable size - boundary with submucosa marked by an elastic lamina that is not obvious with H&E stains 3. Submucosa contains mixed seromucous glands, blood vessels and larger lymphatics of tracheal wall. 4. Adventitia includes a cartilaginous/smooth muscle layer consisting of C-shaped rings of hyaline cartilage that are incomplete dorsally where the trachea contacts the esophagus. Fibroelastic tissue and smooth muscle (trachealis muscle) bridge gap between free ends of the C. The outer adventitia is rich in fat cells and carries nerves and blood vessels to the trachea. Blends into the tissue of the neck and mediastinum. BRONCHI FORM A VAST BRANCHING STRUCTURE; THEY HAVE CARTILAGE AND GLANDS: 1. Trachea divides to form two primary bronchi external to the lung. Trachea and extrapulmonary bronchi have C-shaped rings of cartilage, the intrapulmonary primary bronchi have a complete, but broken ring of overlapping plates of cartilage. Bronchus, together with main pulmonary vessels and nerves enters the hilum of the lung. 3 2. Within lung, primary bronchi divide into lobar (secondary) bronchi and then into tertiary (segmental) bronchi. A tertiary bronchus supplies a bronchopulmonary segment. The tertiary bronchus divides repeatedly into smaller branches that retain similar histological features until the airways have a caliber of about 1 mm where the bronchioles begin. • Bronchial Mucosa is similar to that in the trachea but the lamina propria is thinner. • A spiral layer of smooth muscle (muscularis) separates mucosa from submucosa in the bronchi. Tone in the smooth muscle of the airways is altered by the autonomic nervous system and by mediators released from mast cells, inflammatory cells, and neuroendocrine cells. • Bronchial Submucosa of CT underlies smooth muscle layer and contains serous and mucous glands which become less numerous as airway branches. • Bronchial Adventitia: Irregular plates of cartilage lie outside of submucosa and diminish in prominence as caliber of airway decreases; a layer of smooth muscle replaces it in bronchioles. CT of adventitia is continuous with that of adjacent structures (pulmonary and bronchiolar arteries and the lung parenchyma). 3. Bronchial glands in submucosa are seromucous. Bronchial fluid contains water admixed with variety of mucins, serum proteins filtered from blood, secretory IgA, some secretory IgM and lactoferrin. Lamina propria and submucosa contains lymphoid aggregations of variable size (the BALT or bronchial-associated lymphatic tissue). 4. With each generation of bronchial branching: pseudostratified epithelium becomes lower, lamina propria decreases, muscularis increases then attenuates to become discontinuous, seromucous glands become sparse, and cartilage decreases. BRONCHIOLES ARE THE SMALLEST CONDUCTING PASSAGES; THEY LACK CARTILAGE OR GLANDS: 1. Generally, when the cartilage and submucosal glands are no longer present in walls, conducting passages are called bronchioles; diameter 1 mm and smaller. 2. Epithelium is ciliated, simple columnar and contains goblet cells only in the larger bronchioles. 3. Smooth muscle is the major component of the wall. 4. Bronchioles are attached to surrounding lung tissue by elastic fibers radiating from their circumference. 5. Terminal bronchioles - walls consist of cuboidal epithelium of ciliated cells and Clara cells. Goblet cells not present in healthy lungs. This is the last part of a purely conducting system. One can only say with assurance that a given bronchiole is a terminal bronchiole if one also sees a respiratory bronchiole branching from it. 6. Respiratory bronchioles are the junction between conducting function and the exchange function of this system. Their walls consist of cuboidal epithelium interrupted by alveoli. Distally, the ciliated cells disappear and the Clara cell becomes chief epithelial cell type. 4 Clara cells secrete a lipoprotein to prevent collapse of these small conducting airways on expiration. Small amount of connective tissue and smooth muscle lies under epithelium. ALVEOLAR DUCTS, ALVEOLAR SACS AND ALVEOLI ALLOW GAS EXCHANGE: 1. Each respiratory bronchiole divides into several alveolar ducts. 2. Ducts are lined by simple squamous epithelium but often all that can be seen of walls are aggregations of smooth muscle cells and associated collagen and elastic fibers. 3. Near termination of alveolar duct, clusters of alveoli share a common opening referred to as an alveolar sac. 4. Alveoli are small air sacs with thin walls that allow for diffusion of gases between air space and blood. STRUCTURE OF THE ALVEOLAR WALL (SEPTUM): 1. Epithelial and connective tissue layers are very thin and blood vessels form an enormous capillary network (remember that the total cardiac output passes through the lungs). 2. Connective tissue consists of delicate reticular and elastic supporting elements filling the spaces between the capillaries in the interstitial tissue between alveoli. 3. Capillary endothelium simple squamous, non-fenestrated type. 4. At the air surface, interalveolar septum covered by two types of epithelial cells -alveolar type I cells (squamous pulmonary epithelial cell or small alveolar cell) and alveolar type II cells (great alveolar cell or septal cell). All cells joined by tight junctions. 5. Alveolar type I cells cover about 95% of alveolar surface. Main role is to provide intact surface-of minimum thickness readily permeable to gases. Have a lifespan of about 3 weeks; do not divide. 6. Alveolar type II cells are a cuboidal cell located chiefly at septal junctions. Are as numerous as type I cells but cover only about 2-5% of alveolar surface. Cytoplasmic lamellar bodies release their contents by exocytosis and are the source of pulmonary surfactant whose main role is to decrease surface tension and thus prevent collapse of the alveoli. Can divide and can develop into type I cells for alveolar repair. 7. A third cell type, brush cells, is found very infrequently in alveolar epithelium; they are thought to be sensory receptor cells. 8. Alveolar pores (Pores of Kohn) permit airflow between adjacent alveoli, keeping pressures equalized. Pores may also be important when obstructive lung disease prevents normal passage of air to some alveoli. Alveolar macrophages, pathogens and neoplastic cells can also use the pores. 5 ALVEOLAR CAPILLARY COMPLEX: 1. Both the alveolar epithelium and capillary endothelium rest on basal laminae. Can divide the interalveolar septum into thin and thick regions. 2. Thin region - basal lamina of alveolar epithelium and capillary endothelium fuse. Barrier between air and blood consists of surfactant, type I cell, fused basal lamina and capillary endothelium. Diffusion of gases occurs mainly through this portion. 3. Thick region - each epithelium retains its own basal lamina and in addition the connective tissue septum contains some fibers and cells. This region may be the major site for accumulation and lymphatic drainage of extracellular fluid. ALVEOLAR MACROPHAGE: 1. Also called alveolar phagocyte and the dust cell. 2. Derived from monocytes and enter lung via bloodstream. 3. Not only in connective tissue of the alveolar septum but also on alveolar surface where it scavenges the surface for particles and pathogens. 4. Also phagocytose red blood cells that have leaked into the alveolar air sacs in heart failure. These macrophages become filled with a yellow, iron-containing pigment, called hemosiderin, from the breakdown of hemoglobin. They are called "heart failure cells" when they are coughed out in sputum. 5. Many macrophages ride up the bronchial tree to the pharynx and then are disposed of by being swallowed. Have an average lifespan in the lungs of about 4 days. LUNGS HAVE A DUAL BLOOD SUPPLY - THE PULMONARY AND BRONCHIAL SYSTEMS: 1. Major system is from the pulmonary artery that brings deoxygenated blood from heart via a large pulmonary artery to each lung. 2. Pulmonary arteries enter at the hilum, divide, travel in parallel with the respiratory passages and deliver blood to the pulmonary capillaries in the alveolar septa. 3. Low pressure pulmonary arterial system differs from (high pressure) systemic arterial system - vessels are relatively thin walled and of large diameter, and they are generally musculo-elastic through most of their length (compared to muscular systemic arteries). 4. Oxygenated blood ultimately leaves lungs via the thin walled pulmonary veins that run separately from the airways at peripheral regions of the bronchopulmonary segment, but join bronchi and arteries at higher levels. Each bronchopulmonary segment has its own blood supply and is divided from the others by connective tissue septa. 5. Bronchial arterial system (systemic circulation, high pressure) is a branch from the aorta that supplies oxygenated blood to tissues of airway walls and to the pleura. Arteries 6 are similar in structure to other systemic arteries. Branches extend as far as terminal bronchioles, then anastomose with pulmonary arteries. Bronchial veins only drain the CT of the hilar region of the lungs. LUNGS HAVE AN EXTENSIVE LYMPHATIC DRAINAGE THAT TAKES TWO ROUTES: 1. 2. 3. A deep path follows the air passages to the hilum; it is formed by lymph vessels and lymph nodes draining excess tissue fluid from the parenchyma of the lungs. The surface of the lung, just deep to the visceral pleura, also conveys a second set of lymph vessels to the pulmonary ligament and hilar region. The visceral pleura has extensive lymphatics, but they do not connect to the pleural space. No lymph vessels are found in the alveolar wall. THE LUNG SURFACE, INNER SURFACE OF THE CHEST WALL AND THE SUPERIOR SURFACE OF THE DIAPHRAGM ARE COVERED BY A SLIPPERY SEROUS MEMBRANE SURFACED BY MESOTHELIAL CELLS. 1. 2. 3. 4. The pleura consists of two membranes, the visceral pleura covering the lung and the parietal pleura covering the chest wall and diaphragm. These two pleural membranes meet at the hilar root of the lung. Pleural mesothelial cells rest on a thin layer of collagenous and elastic CT and can vary in shape from flat to cuboidal or columnar. The lymphatics in the parietal pleura connect to the pleural space via stomas, holes 8 to 10 µm in diameter formed in the mesothelial layer where it joins to the underlying lymphatic endothelium. The stomas can accommodate particles as large as erythrocytes. The parietal pleura lymphatics are the major route of exit of liquid from the pleural space. From the stomas, liquid drains to collecting lymphatics, to infracostal lymphatics, to parasternal and periaortic nodes, to the thoracic duct, and into the systemic venous system. The visceral pleura does not contain sensory nerve fibers; therefore, pain indicates involvement of the adjacent parietal pleura. 7