Benefits
advertisement

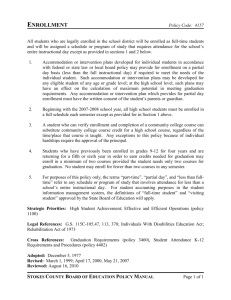
Benefitsthe choice is in my hands. 2013 SOUTHWEST AIRLINES ANNUAL ENROLLMENT Table of Contents Important Enrollment Information............................................................5 Eligibility Documentation.........................................................................5 Eligibility Chart.......................................................................................6 BenefitsPlus Summary.............................................................................7 Health Savings Account............................................................................8 BenefitsPlus 2013 Monthly Medical Contributions.......................................9 BenefitsPlus 2013 Medical Program Options Comparison Chart...................10 BenefitsPlus Prescription Coverage..........................................................12 BenefitsPlus Dental Program...................................................................13 BenefitsPlus Vision Program...................................................................13 Regular Plan….......................................................................................14 Flexible Spending Accounts.....................................................................16 Life Insurance........................................................................................18 Optional Accidental Death & Dismemberment (AD&D) Insurance.................20 Beneficiary Designation.........................................................................20 Long Term Disability (LTD) Insurance........................................................21 BenefitsPlus Voluntary Benefits.............................................................22 ClearSkies/Employee Assistance Program................................................23 Wellness Programs................................................................................23 Important Phone Numbers and Websites....................................back page 2013 ANNUAL ENROLLMENT 3 2013 SOUTHWEST AIRLINES Annual Enrollment October 25, 2012 - November 14, 2012 Closes at 11:59 P.M. Central Time Important note: The online enrollment system will be closed on Saturday, November 10, 2012 from 6:00 a.m. - 7:00 p.m. Central Time. BIG CHANGES: Employee benefit options have been redesigned for 2013 to give you more choices. READ CLOSELY: This Annual Enrollment guide provides an overview of the information and tools that you need to understand these choices and select the options that will work best for you and your family. The benefits described in this 2013 Annual Enrollment guide will be effective January 1, 2013. Please read all of the information in this guide and be sure to call or e-mail the Benefits Team if you have questions. ASK QUESTIONS: Health & Welfare Benefits Monday – Friday 8:00 a.m. – 5:00 p.m. Central Time 1-800-551-1211 askbenefits@wnco.com 4 2013 ANNUAL ENROLLMENT ADDITIONAL INFORMATION— SUMMARY OF BENEFITS COVERAGE: As an Employee, the health benefits available to you represent a significant component of your compensation package. They also provide important protection for you and your family in the case of illness or injury. The Southwest Airlines Co. Welfare Benefit Plan offers a series of health coverage options. Choosing a health coverage option is an important decision. To help you make an informed choice, your plan makes available a Summary of Benefits and Coverage (SBC) for each option, that summarizes important information in a standard format to help you compare across options. SBCs are available on the online enrollment tool as well as at SWALife>My Benefits>Benefits Information and Resources>Summary of Benefits Coverage. A paper copy is also available, free of charge, by e-mailing askbenefits@wnco.com or calling 1-800-551-1211. IMPORTANT ENROLLMENT INFORMATION YOU MUST ENROLL ONLINE. To enroll, go to SWALife >About Me >My Benefits and click on the Annual Enrollment link. For detailed step-by-step instructions on how to enroll, please refer to the 2013 Online Enrollment User guide included in this packet. ENROLL EARLY! Annual Enrollment begins on October 25 and ends on November 14 at 11:59 p.m. Central Time. Late enrollments, changes, or corrections will not be accepted. The online enrollment system will be closed on Saturday, November 10, 2012 from 6:00 a.m. - 7:00 p.m. Central Time. YOU MUST SAVE YOUR ELECTIONS, when you complete the online enrollment process. REVIEW THE BENEFITS CONFIRMATION STATEMENT. You are not enrolled until you see the Benefits Confirmation Statement on the computer screen and receive it in your Company e-mail inbox. It is your responsibility to carefully review the Benefits Confirmation Statement to confirm that it matches your selections and print a copy of your Benefits Confirmation Statement for your records. DEADLINE-ELIGIBLITY DOCUMENTATION REQUIRED. December 31, 2012 is the deadline to submit forms and documentation for newly enrolled Family Members. FLEXIBLE SPENDING ACCOUNT ELECTIONS DO NOT CARRY OVER YEAR-TO-YEAR. If you would like to enroll in the Health Care Flexible Spending Account or the Dependent Care Flexible Spending Account then you must make affirmative elections during Annual Enrollment. REGISTRATION REQUIREMENT WHEN CHANGING FROM THE REGULAR PLAN TO BENEFITSPLUS (OR FROM BENEFITSPLUS TO THE REGULAR PLAN). Reminder: There are two programs available for benefits coverage— BenefitsPlus and the Regular Plan. If you would like to switch coverage from the Regular Plan to BenefitsPlus or from BenefitsPlus to the Regular Plan, you must contact Health & Welfare Benefits before using the online enrollment tool so that you can be registered with the desired program. You will be required to complete a Benefits Request for Program Change Form. You must allow 24 hours to process your Benefits Request for Program Change Form before you enroll in the desired program using the online enrollment tool. Note: If you switch from the BenefitsPlus program to the Regular Plan, you and your family members over the age of 19 may be subject to a three-month pre-existing condition limitation. AUTOMATIC ENROLLMENT IF YOU DO NOT ELECT 2013 OPTIONS. Choice Plus PPO and Choice EPO are being combined to form the Choice Plus Plan, and Medical Plan C is being renamed Choice Plan C, all effective January 1, 2013. If you do not make an election online during Annual Enrollment and you are currently enrolled in these options then, effective January 1, 2013 you will be automatically enrolled as follows: 2012 Election Defaults to Choice Plus PPO Choice EPO Medical Plan C 2013 Election Choice Plus Plan Choice Plus Plan Choice Plan C ELIGIBILITY DOCUMENTATION Southwest offers benefit coverage in the Medical, Dental, Vision and Life Insurance programs to eligible dependents provided that you submit all required documentation upon enrollment and at any time upon request. To enroll a new Family Member for coverage effective January 1, 2013, you must complete a Family Member Documentation Form and provide required documentation no later than December 31, 2012. If your documentation is not received prior to this deadline, then the family member will not be eligible for coverage in 2013. INSTRUCTIONS FOR SUBMITTING DOCUMENTATION: 1. Obtain Family Member Documentation Form through the online enrollment tool. 2. Complete the Family Member Documentation Form – including your dependent’s social security number. 3. Review the eligibility chart, gather all required documents and write your Employee ID number on each document. 4. Ask questions! 5. Deliver, fax, or e-mail the documentation to: Health & Welfare Benefits 1st Floor of Headquarters in the People Department FAX: 214-792-4216 askbenefits@wnco.com 6. Confirm receipt with Health & Welfare Benefits. 7. Keep a copy of documentation and proof of submission for your records. 8. Be prepared to provide additional information if needed upon request. 2013 ANNUAL ENROLLMENT 5 ELIGIBILITY CHART Southwest Airlines and its third party administrators may audit dependent eligibility at any time. It is each Employee’s responsibility to provide any and all information requested. Falsifying eligibility documentation, claims, or otherwise attempting to obtain benefits or coverage inappropriately could result in denial of claims, termination of benefits, and other disciplinary measures, up to and including termination of employment. Family Member Description Required Documentation Spouse 1. Copy of Marriage Certificate issued by a governmental agency (certified translated copy if in a foreign language); 2. Social Security Number; 3. And ONE document from the options below: Option 1 Page 1 of your current year’s filed Federal tax return that lists your Spouse and filing status. Option 2 Page 1 of your previous year’s filed Federal tax return that lists your Spouse and filing status AND a copy of your current year IRS Form 4868 requesting a filing extension. Option 3 One item from the list below. • Joint Ownership Document - examples include: mortgage statement, credit card statement, car note, bank statement, school taxes, or utility bills dated any time in the last three months listing you and your Spouse • Rental/lease agreement, deed, or property tax statement/appraisals dated anytime in the last 12 months listing you and your Spouse • Homeowner’s insurance policy currently in effect listing you and your Spouse • Auto insurance policy currently in effect listing you and your Spouse • Automobile registration currently in effect listing you and your Spouse Your lawful Spouse (if not legally separated from you, the Employee) who qualifies as a Spouse for purposes of the Internal Revenue Code of 1986 (as in effect on January 1, 2004). **If you were married within the last 12 months, then you only need to submit a copy of your Marriage Certificate and do not need to submit the documents listed in the options. Marriage License alone is not adequate. Natural Child Your natural child up to age 26. 1. Copy of Birth Certificate issued by a governmental agency, Hospital Birth Record (for newborns), or other legal document establishing parentage. (Employee must be listed on the birth certificate, hospital birth record or other legal document). 2. Social Security Number Stepchild Your stepchild, up to age 26 and who is a child of your current Spouse by a previous union. 1. Copy of Birth Certificate issued by a governmental agency or other legal document establishing parentage. Employee’s Spouse must be listed on birth certificate or other legal document. 2. Social Security Number. Your legally-adopted child, including child placed for adoption Legally Adopted Child (or Child Placed up to age 26. for Adoption) 1. Copy of Adoption (or Adoption Placement) Orders proving legal obligation and issued by a Court or other legal authority. 2. Social Security Number. Child for Whom You Have a Legal Obligation Child for whom you (or, alternatively, you and your Spouse) have been appointed by a court of competent jurisdiction as the person(s) having custody of the child and the sole legal right and obligation to provide support and medical care for the child, but only if the child resides in your household on a permanent basis and the child’s parents are deceased, or the parental rights of the child’s parents are permanently terminated, or the Plan Administrator determines, in its sole discretion, that the child’s parents are totally disabled and financially unable to provide any support or care for the child. 1. Copy of Birth Certificate issued by a governmental agency; 2. Court Documentation proving your custody and the sole legal right and obligation to provide support and medical care for the child; proof the child lives in your household on a permanent basis; proof the child’s parents are deceased or have had their parental rights permanently terminated (or proof the child’s parents are totally disabled and financially unable to provide any support or care for the child); and 3. Social Security Number. Disabled Child Your disabled child up to the age of 26 is covered under the eligibilty guidelines described above. Your disabled child over age 25 may be eligible for continued coverage. For disabled children over age 25, a physician’s statement showing proof of incapacity is required. Contact Health & Welfare Benefits for the appropriate forms. Committed Partner Your Committed Partner must satisfy all of the requirements as stated in the Committed Partner Policy. Your eligible Committed Partner may only be enrolled in BenefitsPlus, as well as the Dental Plan and the Vision Plan. You may enroll in the Committed Partner Program for Medical Coverage and/or Passes at any time during the calendar year. You may find the Committed Partner Enrollment Packet on SWALIfe>About Me>Launch Self Service>My Benefits>Benefits Information and Resources>Information and Forms. See the Southwest Airlines Co. Committed Partner Benefits Policy for required proof of eligibility (available at www.swalife.com or upon request from the Health & Welfare Benefits). Registered Partner (Passes Only) Your Registered Partner must satisfy all of the requirements stated in the Registered Partner Policy and you must complete the appropriate paperwork. You may find the Registered Partner Enrollment Packet on SWALife>About Me>Launch Self-Service>My Benefits>Benefits Information and Resources>Information and Forms. See the Southwest Airlines Co. Committed Partner Benefits Policy for required proof of eligibility (available at www.swalife.com or upon request from the Health & Welfare Benefits). 6 2013 ANNUAL ENROLLMENT BENEFITSPLUS summary Effective January 1, 2013, there will be three options for medical coverage available under the BenefitsPlus program designed to give you the ability to make choices that best fit your family’s needs. All BenefitsPlus programs will be administered by UnitedHealthcare in 2013. All Employees will receive new insurance ID cards in early January. Choice Plus Plan: The BenefitsPlus EPO and PPO options are being combined to form the Choice Plus Plan. The Choice Plus Plan offers network benefits and non-network benefits, although it pays more for services provided by network providers. It includes copays for office visits and generic drugs and pays a percentage of the costs for other medical care as well as non-generic drugs. Choice Plan C: Medical Plan C is being renamed Choice Plan C. Modifications include but are not limited to: • Employees will pay monthly contributions (see Medical Monthly Contributions chart). • The Out-of-pocket maximum for Employee coverage will decrease while the Out-of-pocket maximum for Family coverage will increase. • Generic and non-preferred prescription drugs coinsurance remains unchanged, however the amount the Employee pays for preferred brand prescriptions will increase. Health Savings Plan (HSP): The Health Savings Plan (HSP): The Health Savings Plan is a new medical option that offers low monthly contributions, but notably higher deductible and higher coinsurance requirements. Employees in the Health Savings Plan are responsible for the full cost of all healthcare expenses (other than qualified preventive care) until the higher deductible and coinsurance are satisfied. The Health Savings Plan has: • The option to contribute to a tax-advantaged Health Savings Account (HSA). See below for more details • Lower monthly upfront contributions compared to the other BenefitsPlus options. The amount saved on monthly contributions can be contributed to a Health Savings Account. • Higher deductibles compared to the other BenefitsPlus options. The deductible in the Health Savings Plan works differently than the deductibles in the other BenefitsPlus medical options. With “Employee Only” coverage in the Health Savings Plan, the Employee will be subject to the “Employee Only” deductible of $1,500. With any other coverage level besides “Employee Only” (including any Committed Partner coverage), the “Family” deductible of $3,000 must be met. Unlike the other BenefitsPlus options, there is no deductible for individual Family members. There is only one deductible for the entire Family that is significantly higher than the other BenefitsPlus options. • Out-of-Pocket maximums. Your Out-of-pocket maximum is the maximum amount you pay during a calendar year for covered charges. The Out-ofpocket maximum is applied to you and each covered Dependent you add to coverage. Once you have paid your deductible, and in addition, reached the coinsurance annual Out-of-pocket maximum, the Health Savings Plan will cover 100% of all eligible expenses for the reminder of the calendar year. The Out-of-pocket maximum excludes deductibles. • A unique prescription drug benefit. Under the Health Savings Plan, certain preventive prescription BenefitsPlus drugs are covered at 80% before the deductible is met. For a list of these preventive prescriptions, go to SWALife on About Me>My Benefits>Information and Forms. For all other prescriptions, the Employee is responsible for the full cost until the medical deductible is met. • Coverage for eligible benefits on the autism spectrum, including Applied Behavioral Analysis (ABA) Therapy. This coverage is only available under the Health Savings Plan option. Treatment associated with autism may be covered, including speech therapy, occupational therapy, and physical therapy subject to any plan coverage limitations. Benefits may be denied or shortened for persons not progressing in goal-directed rehabilitation services or if rehabilitation goals were previously met. Benefits under this section are not available for maintenance/ preventive manipulative treatment. All services under this benefit for both in and out-of-network providers require pre-notification or coverage will be denied. To access benefits for autism coverage and to meet the pre-notification requirement, call Clear Skies at 1-800-742-8911. 2013 ANNUAL ENROLLMENT 7 health savings account A Health Savings Account (HSA) is only available under the BenefitsPlus Health Savings Plan option. If you enroll in the Health Savings Plan, you will have the option, if you meet IRS requirements, of opening a Health Savings Account (HSA) to save money for qualified health care expenses. You may choose to open an HSA with any bank. If you open your account with OptumHealth Bank, then the amount that you choose to save can be withheld from your paycheck before taxes and direct deposited to your HSA. If you open an HSA with another bank, you may make contributions directly (for example, by personal check) but payroll deductions will not be available to you. The amount in your HSA is yours to use for qualified medical expenses, including your deductible under the Health Savings Plan. You do not lose amounts in your HSA at the end of the year or when your employment with Southwest ends. It’s your money! You may also choose for amounts in your HSA to earn interest and grow tax-free for use on qualified medical expenses in the future. How to Open a Health Savings Account (HSA): To participate in the HSA, you will need to personally open your own account. You can either (i) choose to have Southwest deduct your HSA contributions directly from your paycheck, in which case you must open your own account with OptumHealth Bank (see details below), or (ii) choose to make direct contributions (for example, by personal check) to your HSA in which case you may open a Health Savings Account with the bank of your choice. To open a Health Savings Account with OptumHealth Bank, you must go to www.OptumHealthBank.com to complete the bank’s online application including Southwest Airlines’ Group Number 199409. Your elected pre-tax payroll contributions will not begin until you open your account with OptumHealth Bank. Note: You must open an HSA and have funds in your HSA before you can use your account to pay for qualified medical expenses. You may only use your HSA to pay for medical expenses incurred after the account is opened. 8 2013 ANNUAL ENROLLMENT HSA Eligibility: Most Southwest Employees will be eligible to open a Health Savings Account; however, federal tax law limits participation in a Health Savings Account in some circumstances. Make sure you understand these limitations before you make your elections. These eligibility requirements only apply to the Health Savings Account—not the Health Savings Plan option. If you enroll in the Health Savings Plan intending to open a Health Savings Account, but then determine you are not eligible for the Health Savings Account, you will not be able to change to another medical option until Annual Enrollment for 2014. To be eligible to open a Health Savings Account (HSA): • You may ONLY have medical coverage under an eligible high deductible health plan (HDHP)—the Southwest Health Savings Plan. o You may not have coverage under a spouse’s non-HDHP. o You may not be enrolled in Medicare (Part A or B), TRICARE or TRICARE for Life, even as secondary coverage. (If you are eligible for Medicare, but not enrolled, then you are eligible to contribute to an HSA.) o You must not have received Veteran Administration (VA) Benefits within three months of making any contribution to your Health Savings Account. • You may not be claimed as a dependent on someone else’s tax return. • You, and your spouse (if any), may not contribute to a Health Care Flexible Spending Account (including Southwest’s Health Care Flexible Spending Account). However, you may contribute to a Dependent Care Flexible Spending Account. Note: Although a Committed Partner can be covered under the Health Savings Plan, under federal tax rules, the Committed Partner’s medical expenses usually will not constitute qualified medical expenses that can be paid or reimbursed out of a Health Savings Account. BenefitsPlus 2013 Monthly medical Contributions You may enroll in medical, dental, and vision options independently of each other and each option selected has its own monthly contribution as shown in the charts below. For example, you may elect Employee + Family coverage for medical, Employee Only coverage for dental, and Employee + Spouse for vision. By carefully choosing the options that are the best fit for your family, you can structure your benefits to minimize your monthly contributions. If you select NO COVERAGE for medical, then you will receive a $50.00 credit in your paycheck each month ($60.00 for eligible SWA to SWA no coverage election). Fulltime Employees Benefitsplus Medical Monthly Contributions Choice Plus Plan Choice Plan C Health Savings Plan EE ONLY $49.00 $20.00 $5.00 EE + SPOUSE EE + COMMITTED PARTNER $150.00 $70.00 $9.00 EE + CHILDREN $133.00 $66.00 $7.00 EE + FAMILY EE + COMMITTED PARTNER + CHILDREN $221.00 $113.00 $11.00 SWA EE + SWA EE $98.00 $40.00 $9.00 SWA EE + SWA FAMILY $182.00 $86.00 $11.00 Parttime Employees Benefitsplus Medical Monthly Contributions Choice Plus Plan Choice Plan C Health Savings Plan EE ONLY $49.00 $20.00 $5.00 EE + SPOUSE EE + COMMITTED PARTNER $510.85 $455.15 $406.34 EE + CHILDREN $377.30 $329.60 $290.94 EE + FAMILY EE + COMMITTED PARTNER + CHILDREN $842.16 $767.75 $695.29 SWA EE + SWA EE $98.00 $40.00 $9.00 SWA EE + SWA FAMILY $426.30 $349.60 $294.94 2013 ANNUAL ENROLLMENT 9 2013 benefitsplus MEDICAL Program options COMPARISON Annual Deductible BenefitsPlus CHOICE PLUS(5) Network: $300/Per Person; $750/Family Non-Network: $600/Per Person; $1,500/Family (does not apply to Out-of-pocket maximum) 100% After appropriate copay or coinsurance. In Network: Co-Pays/Services Performed by Physician Convenience Care Clinic; $15 (2) Office Visit $25; Specialist $40; Urgent Care $40; Emergency Room $150 Other Services after annual deductible 15% coinsurance Non-Network: 60% coverage, no co-pay (non-surgical do not apply towards deductible or Out-of-pocket maximum) General Level of Benefit Coverage Network Provider: 85%; Non-Network Provider: 60% (after annual deductible) (inpatient and outpatient) Preventive Care (no deductible) Network Provider: 100% Non-Network Provider: 100% of Reasonable and Customary (Adult and Children) Newborn Care (inpatient) Network Provider: 85%; Non-Network Provider: 60% (after annual deductible) Includes: circumcision, room and board, general nursing care, and Doctor’s fees. See chart on page 12 for more information. Prescriptions Services(1): 50% coinsurance after $500 separate lifetime deductible (infertility treatment only), Employee and spouse combined; $10,000 lifetime maximum — You and your Spouse/Committed Partner combined Infertility Treatment (Pre-treatment authorization required by UHC) Prescription Drugs: • Network Provider: 50% coinsurance, $5,000 lifetime maximum—You and your Spouse/ Committed Partner combined • Non-Network Provider: No Coverage Applied Behavorial Analysis (ABA) Therapy ClearSkies Employee Assistance Program (EAP) No Coverage Network Provider: Up to five appointments per person, per issue with ClearSkies at no charge. Non-Network: no coverage Mental, Emotional, Behavioral and Chemical Abuse/Dependency Benefits Prenotified(3) Prescription Drugs are covered under the Network: Outpatient/Inpatient 85% Non-Network: Outpatient/Inpatient 60% (after annual deductible) Prescription Drug Card Program. Annual Out-of-Pocket Maximum (excludes deductibles and all copays except emergency room copays) Network: $3,200 per person; $6,400 family Non-Network: $6,400 per person; $12,800 family (excludes deductibles) Lifetime Maximum (combined Medical and Mental Health and No Limit Chemical Dependency) (1) Charges for all prescription drugs and infertility treatment will not apply to the Choice Plus Plan annual out-of-pocket maximum or annual medical deductible. Certain provider and coverage limitations apply to infertility treatment. You must contact Unitedhealthcare prior to receiving infertility treatment. (2) List of Convenience Care Clinics available at www.myuhc.com. 10 2013 ANNUAL ENROLLMENT BenefitsPlus CHOICE PLAN C(5) Network: $800/Per Person; $2,000/Family Non-Network: $1,500/Per Person; $3,750/Family (does not apply to Out-of-pocket maximum) HEALTH SAVINGS PLAN (HSP)(6) Network/Non-Network - $1,500/Employee Only - $3,000/Family(6) (does not apply to Out-of-pocket maximum) Co-pays not available Co-pays not available Network Provider: 80%; Non-Network Provider: 60% Network Provider: 80% Non-Network provider: 60% (after annual deductible) (after annual deductible) Network Provider: 100% Network Provider: 100% Non-Network Provider: 100% of Reasonable and Customary Non-Network Provider: 100% of Reasonable and Customary No Coverage Network Provider: 80%; Non-Network Provider: 60% (after annual deductible) See chart on page 12 for more information. See chart on page 12 for more information. No Coverage No Coverage No Coverage Network Provider: 80% Non-Network provider: 60% (after annual deductible) Network Provider: Up to five appointments per person, per issue with ClearSkies at no charge. Non-Network: no coverage Network Provider: Up to five appointments per person, per issue with ClearSkies at no charge. Non-Network: no coverage Network: Outpatient/Inpatient 80% Network: Outpatient/Inpatient 80% Non-Network: Outpatient/Inpatient 60% Non-Network: Outpatient/Inpatient 60% (after annual deductible) (after annual deductible) Network: $4,000 per person; $8,000 family Network: $4,500/per person - $9,000/per family Non-Network: $6,000 per person; $12,000 family Non-Network: $6,750/per person - $13,500/per family (excludes deductibles) (excludes deductibles) No Limit No Limit (3) Refer to the Summary Plan Description on SWALife>About Me for prenotification rules for each medical plan. (4) List of Specified Preventive medications may be found at SWALIfe>About Me>My Benefits. (5) For the Choice Plus Plan and Choice Plan C, when an individual in a family meets the individual deductible, coinsurance applies. When the family deductible amount is met, the rest of the family will receive benefits. One participant can never incur deductible expenses above the individual limit. Family deductible may be reached with any combination of expense incurred by any Family Member. (6) For the HSP, if you have anything other than Employee Only coverage, then you will be subject to the entire family deductible before any Family Member receives a benefits. 2013 ANNUAL ENROLLMENT 11 BENEFITSPLUS PRESCRIPTION COVERAGE When you enroll in a BenefitsPlus medical option you are automatically enrolled in the corresponding prescription coverage. Described below are the amounts the Employee is required to pay for prescription coverage. BenefitsPlus Prescription Choice Plus Plan Choice Plan C Health Savings Plan 30 Day Retail 90 Day Retail/ Mail Order 30 Day Retail 90 Day Retail/ Mail Order 30 Day Retail 90 Day Retail/ Mail Order Catamaran Catamaran Catamaran Catamaran OptumRx OptumRx $10 $25 10% ($10 min/$35 max) 7% ($25min/$88 max) 20% 20% 25% ($25 min/$50 max) 20% ($45 min/$125 max) 25% ($25 up to $100) 20% ($63 up to $250) 20% 20% Non-Preferred Brand 45% ($40 up to $150) 45% ($60 up to $375) 45% ($40 up to $150) 45% ($125 up to $375) 20% 20% Specialty Drug 25% ($20-$150) 90 day not available 25% ($20-$150) 90 day not available 20% 90 day not available 20% (deductible waived for core list of medications) Administrator Generic Preferred Brand Preventive Medications (applies N/A N/A N/A N/A 20% (deductible waived for core list of medications) Covered at 100% by plan Covered at 100% by plan Covered at 100% by plan Covered at 100% by plan 20% 90 day not available $0.00 $0.00 $50 separate annual deductible $50 separate annual deductible $1,500/$3,000 (Combined w/Health Plan Deductible) $1,500/$3,000 (Combined w/Health Plan Deductible) to HSP Plan only) Diabetic Testing Supplies Deductible (annual) Infertility Medications 12 50% with $5,000 lifetime maximum 2013 ANNUAL ENROLLMENT BENEFITSPLUS dental program The Southwest dental program is administered by Delta Dental and is separate from your medical program. You may go to any dentist that you choose; however, you will have lower coinsurance requirements if you select a network provider. To print a dental ID card or locate a network provider go to www.deltadentalins.com/southwest. If you select NO COVERAGE for dental, then you will receive an $8.50 credit in your paycheck each month. Dental Monthly Contributions Parttime Employees Fulltime Employees Benefitsplus Basic Optional Basic Optional EE ONLY $1.00 $10.00 $1.00 $10.00 EE + SPOUSE EE + COMMITTED PARTNER $3.00 $26.00 $31.02 $56.52 EE + CHILDREN $3.00 $30.00 $37.02 $65.82 EE + FAMILY EE + COMMITTED PARTNER + CHILDREN $5.00 $42.00 $61.04 $103.04 SWA EE + SWA EE $2.00 $20.00 $2.00 $20.00 SWA EE + SWA FAMILY $4.00 $40.00 $38.02 $75.82 BENEFITSPLUS vision program EyeMed Vision Care will be the new vision program provider effective January 1, 2013. The vision program is an insured plan (not self-insured by Southwest) and Southwest has negotiated lower rates compared to prior years. EyeMed Vision Care offers an expansive network of doctors and vision care centers including popular convenient retail locations (e.g., LensCrafters, Sears, Target Optical, Pearl Vision, JCPenney Optical). For a comprehensive summary of vision benefits and network providers go to www.strata-g.com/eyemed/ swa. If you elect vision coverage, a vision ID card will be mailed in January 2013 to your home address on record. As a general matter, you may only enroll in the vision program if you are enrolled in BenefitsPlus. Although some collectively bargained work groups have the option to enroll in the Vision Program through the Regular Plan. BenefitsPlus Vision Monthly Contributions Fulltime and Parttime Employees EE ONLY $4.92 EE + SPOUSE EE + COMMITTED PARTNER $9.35 EE + CHILDREN $9.84 EE + FAMILY EE + COMMITTED PARTNER + CHILDREN $14.47 2013 ANNUAL ENROLLMENT 13 regular plan REGISTRATION REQUIREMENT WHEN CHANGING FROM THE REGULAR PLAN TO BENEFITSPLUS (OR FROM BENEFITSPLUS TO THE REGULAR PLAN): Reminder: There are two programs available for benefits coverage—BenefitsPlus and the Regular Plan. If you would like to switch coverage from the Regular Plan to BenefitsPlus or from BenefitsPlus to the Regular Plan, you must contact Health & Welfare Benefits before using the online enrollment tool so that you can be registered with the desired program. You will be required to complete a Benefits Request for Program Change Form. You must allow 24 hours to process your Benefits Request for Program Change Form before you enroll in the desired program using the online enrollment tool. Note: If you switch from the BenefitsPlus program to the Regular Plan, you and your family members over the age of 19 may be subject to a three-month pre-existing condition limitation. Effective January 1, 2013, UnitedHealthcare will administer the Regular Plan (not Blue Cross Blue Shield of Texas). You will receive a new medical ID card in January 2013. HEALTH CARE REFORM REQUIRED LEGAL NOTICE: The Southwest Airlines Co. Funded Welfare Benefit Plan believes the Regular Plan Benefit Program is a “grandfathered health plan” under the Patient Protection and Affordable Care Act (the “Affordable Care Act”). As permitted by the Affordable Care Act, a grandfathered health plan can preserve certain basic health coverage that was already in effect when that law was enacted. Being a grandfathered health plan means that coverage under the Regular Plan Benefit Program may not include certain consumer protections of the Affordable Care Act that apply to the BenefitsPlus program options, for example, the requirement for the provision of preventive health services without any cost sharing. However, grandfathered health plans must comply with certain other consumer protections in the Affordable Care Act, for example, the elimination of lifetime limits on benefits. Questions regarding which protections apply and which protections do not apply to a grandfathered health plan and what might cause a plan to change from grandfathered health plan status can be directed to Health & Welfare Benefits by e-mailing askbenefits@ wnco.com or phoning 1-800-551-1211. You may also contact the Employee Benefits Security Administration, U.S. Department of Labor at 1-866-444-3272 or www. dol.gov/ebsa/healthreform. This website has a table summarizing which protections do and do not apply to grandfathered health plan. 14 2013 ANNUAL ENROLLMENT IMPORTANT INFORMATION TO CONSIDER ABOUT THE REGULAR PLAN: The Regular Plan either does not offer, or offers but limits, many of the benefits that may be available under BenefitsPlus. You should carefully review these limitations before selecting this option. • Preventive services such as physicals, mammograms, and colonoscopies are not covered. • Basic medical and dental coverage is available but it is more limited than under BenefitsPlus. • Mail order prescriptions are not available. • The Vision Program is only offered to some work groups under the Regular Plan. • You may not enroll in the Flexible Spending Account programs (i.e., Health Care Flexible Spending Account and Dependent Care Flexible Spending Account). • Optional Life Insurance is limited to the amount equal to your Basic Life Insurance • Spouse Life Insurance is limited to a maximum of $10,000. • Child Life Insurance is limited to a maximum of $1,000 for each child less than six months of age, or $5,000 for each child six months of age or older. • Optional Accidental Death and Dismemberment Insurance (AD&D) is limited to the amount equal to your Basic Life Insurance. • You may not enroll in optional Accidental Death & Dismemberment coverage for Family. • Long Term Disability is not automatically provided by Southwest when enrolled in the Regular Plan. • The new voluntary benefit programs (i.e., auto/ home/pet/supplemental hospital insurance) are only available under BenefitsPlus and are not available under the Regular Plan. • Committed partner benefits are not offered in the Regular Plan. Medical Regular Plan Monthly Contributions Dental Vision Fulltime Parttime Fulltime Parttime Fulltime Parttime EE ONLY $0 $0 $0 $0 $3.83 $3.83 EE + SPOUSE EE + COMMITTED PARTNER $0 $572.76 $0 $28.00 $7.28 $7.28 EE + CHILDREN $0 $400.93 $0 $33.60 $7.67 $7.67 EE + FAMILY EE + COMMITTED PARTNER + CHILDREN $0 $973.69 $0 $56.00 $11.27 $$11.27 SWA EE + SWA EE $0 $0 $0 $0 $7.28 $7.28 SWA EE + SWA FAMILY $0 $400.93 $0 $33.60 $11.27 $11.27 You are automatically enrolled in prescription drug coverage administered by OptumRx when you enroll in the Regular Plan. Preferred brand, non-preferred and specialty medications are available in either a 30 day or 90 day retail supply (no mail order option). You may refer to the chart below for the schedule of prescription benefits. Regular Plan Prescription Chart Deductible (annual) $200/$300 (Combined w/Health Plan Deductible) Generic Covered at 100% (after deductible) Preferred Brand 20% (after deductible) Non-Preferred Brand 20% (after deductible) Specialty Drug 20% (after deductible) Diabetic Testing Supplies 20% (after deductible) Preventive Medications N/A Infertility N/A 2013 ANNUAL ENROLLMENT 15 flexible spending accounts If you are electing BenefitsPlus Choice Plus Plan or Choice Plan C medical options then you may choose to participate in the Health Care Flexible Spending Account program. If you are electing BenefitsPlus Choice Plus Plan, Choice Plan C, or the Health Savings Plan medical option then you may choose to participate in the Dependent Care Flexible Spending Account program. All flexible spending programs are administered by UnitedHealthcare. Expenses Eligible for Reimbursement Health Care Flexible Spending Account Dependent Care Flexible Spending Account Qualified medical expenses ONLY. Qualified dependent day care expenses ONLY. Choice Plus Plan YES YES Choice Plan C YES YES Can be elected if enrolled in the Health Savings Plan Option? NO YES What is this benefit used for? To participate in the flexible spending account programs, you must make an election each year. Your 2012 elections will not rollover to 2013. If you choose to participate, then you must determine the amount that you would like to contribute annually and elect this contribution amount during Annual Enrollment. The annual contribution amount will be prorated across your paychecks throughout the year. Your monthly flexible spending account contribution(s) will be withheld from your paychecks before taxes. Amounts contributed to flexible spending accounts do not carry-over from year-to-year. Both flexible spending accounts operate as use-it-or-lose-it programs. If you don’t use all your Flexible Spending Account contributions by December 31st, then the remaining balance is forfeited. You have until March 31st of the following year to file claims, but the eligible expenses must be incurred by December 31st of the prior year. 16 2013 ANNUAL ENROLLMENT HEALTH CARE FLEXIBLE SPENDING ACCOUNT: The Health Care Flexible Spending Account is a way for you to save money tax-free to use on eligible healthcare expenses, including co-pays and coinsurance, for you and members of your family that qualify as dependents for federal income tax purposes. For a complete and current detailed listing of eligible healthcare expenses and ineligible expenses you may go to www.irs.gov and review Publication 502. As a result of healthcare reform, effective January 1, 2013, the maximum amount that you may contribute to a Health Care Flexible Spending Account in 2013 is $2,500. The minimum amount you may contribute for the year is $120. The Health Care Flexible Spending Account program is different than the Health Savings Account (HSA). You may not participate in the Health Care Flexible Spending Account if you are enrolled in the BenefitsPlus Health Savings Plan medical option. The chart below reflects the differences: Comparison Chart Health Care Flexible Spending Account Health Savings Account BenefitsPlus Choice Plus Plan and Choice Plan C ONLY BenefitsPlus Health Savings Plan (HSP) ONLY YES NO $2,500 $3,250 Employee Only Coverage $6,450 Family Coverage (Family Coverage includes: Employee + Spouse/ Committed Partner, Employee + Children) Roll-over option when Terminate or Retire? NO YES Qualified Medical Expenses only? YES YES Pre-Tax Contributions? YES YES* Can be elected if enrolled in the BenefitsPlus Health Savings Plan Option? NO YES Medical Program Requirement Must be Used by Year End? (“Use it or Lose it”) Annual Contribution Limit? * Pre-tax payroll contributions can only be made to a Health Savings Account with OptumHealth Bank. If you open your Health Savings Account with another bank, contributions cannot be pre-tax payroll deducted, although they may be considered a tax deduction when filing your annual tax return. Consult your tax advisor for details. DEPENDENT CARE FLEXIBLE SPENDING ACCOUNT: The Dependent Care Flexible Spending Account allows you to set aside money each year from your pay to reimburse yourself for eligible expenses for the child or adult daycare or other qualifying care of your family members that qualify as a dependent for federal income tax purposes. For 2013, you may contribute any amount from an annual minimum of $120 up to annual maximum of $5,000 (or $2,500 if you are married and filing separate tax returns) to pay for eligible dependent care expenses. If you do not have child or adult daycare or other qualifying care expenses, then you should not enroll in the Dependent Care Flexible Spending Account. If you enroll in the Dependent Care Flexible Spending Account in error, contributions will not be refunded. 2013 ANNUAL ENROLLMENT 17 LIFE INSURANCE Southwest offers a choice of life insurance options to help provide for your family in the event of your death. The Life Insurance program is an insured product and, effective January 1, 2013, will be provided by MetLife (not The Standard). The transition to MetLife will offer additional benefit levels and lower rates. EMPLOYEE BASIC LIFE INSURANCE: As an Employee at Southwest you automatically receive Basic Life Insurance coverage at no cost to you. Basic life insurance is equal to your base annual pay up to a maximum of $50,000. EMPLOYEE OPTIONAL LIFE INSURANCE: You may elect Optional Life Insurance coverage in addition to Basic Life Insurance coverage. Effective January 1, 2013, if you are enrolled in BenefitsPlus, then you may purchase Optional Life Insurance up to ten times your base annual pay (increased from six times in 2012) and if you are enrolled in the Regular Plan, then you may purchase Optional Life Insurance up to a maximum of $50,000. This means that at the time of your death, your beneficiary will receive a cash payout from MetLife that is equal to the level of coverage you selected. The cost of your premium depends on your age as of December 31 of the Plan Year. Age Bands BenefitsPlus that determine premium level Optional Life Insurance Premiums < 25 $.023 per $1,000 of coverage 25-29 $.023 per $1,000 of coverage 30-44 $.028 per $1,000 of coverage 45-49 $.051 per $1,000 of coverage 50-54 $.079 per $1,000 of coverage 55-59 $.147 per $1,000 of coverage 60-64 $.255 per $1,000 of coverage 65-69 $.493 per $1,000 of coverage 70+ $.793 per $1,000 of coverage SPOUSE/COMMITTED PARTNER LIFE INSURANCE: Southwest offers this life insurance option to help provide for your family in the event of the death of your Spouse/Committed Partner. You may elect the Spouse/Committed Partner Life Insurance coverage level of your choice and upon the death of your Spouse/Committed Partner you or the beneficiary will receive a cash payout from MetLife in that amount. If you are enrolled in BenefitsPlus, then coverage level choices for Spouse/Committed Partner BenefitsPlus are $10,000, $20,000, $30,000, $50,000, $100,000, $150,000, or $250,000. If you are enrolled in the Regular Plan, then you may only purchase Spouse Life Insurance at the $10,000 coverage level and you may not purchase Committed Partner Life Insurance. Age Bands 18 BenefitsPlus that determine premium level Spouse/Committed Partner Insurance Premiums < 25 $.04 per $1,000 of coverage 25-29 $.04 per $1,000 of coverage 30-44 $.05 per $1,000 of coverage 45-49 $.09 per $1,000 of coverage 50-54 $.14 per $1,000 of coverage 55-59 $.26 per $1,000 of coverage 60-64 $.45 per $1,000 of coverage 65-69 $.87 per $1,000 of coverage 70+ $1.40 per $1,000 of coverage 2013 ANNUAL ENROLLMENT LIFE INSURANCE (continued) CHILD LIFE INSURANCE: Southwest offers this life insurance option to help provide for unexpected expenses that may arise in the event of your child’s death. If you are enrolled in BenefitsPlus, then you may elect Child Life Insurance coverage in the amount of $10,000 with a monthly premium of $.50 or $20,000 with a monthly premium of $1.00. If you are enrolled in the Regular Plan, then you may elect Child Life Insurance coverage for a monthly premium of $.26 and your coverage level will be $1,000 for each child less than six months of age and $5,000 for each child six months of age or older. Upon the death of your eligible child you will receive a cash payout from MetLife in the amount of coverage you chose. Eligible children include any children from live birth up to age 25 that qualify as an: unmarried child; disabled child; foster child; child placed with you for adoption; or child living in your home as your grandchild, your stepchild, or the child of your Spouse. IMPORTANT NOTE ABOUT CHILD LIFE INSURANCE: A number of Employees are paying for Child Life Insurance who DO NOT have an eligible child. Removing a child as a dependent for benefits coverage DOES NOT stop the child life insurance deductions. You must also go through the Online Annual Enrollment Tool to remove child life insurance coverage. It is your responsibility to remove the child from coverage. Statement of Health (SOH) Requirements: To increase Optional Life Insurance and/or Spouse/Committed Partner Life Insurance from the level you selected for 2012, you and/or your Spouse/Committed Partner must complete a Statement of Health (SOH) with MetLife after you complete the Annual Enrollment process. It is your responsibility to complete this step following enrollment. Your coverage level(s) will not be increased if you do not submit the SOH(s) in accordance with MetLife’s requirements. To make the transition process to MetLife a little easier, for the 2013 Annual Enrollment period, the SOH will be a short form consisting of only five questions. Responses to the short form will determine if you and/or your Spouse/Committed Partner need to complete the long form and/or be required to submit a medical exam. Any increase in Optional Life Insurance and/or Spouse/Committed Partner Life Insurance will be suspended until MetLife approves or denies your increased coverage. You will receive a notification from MetLife once a determination has been made. Statement of Health Process: If you increase Optional Life Insurance and/or Spouse/Committed Partner Life Insurance, then a web link for the Statement of Health will be e-mailed to your Company e-mail address within five business days. The SOH must be completed within thirty days of when the e-mail is delivered to your Company e-mail address. If not completed, then your 2012 life insurance elections will carry-over to 2013 and your new elections will not take effect. Age 70 Limitations: MetLife limits Optional Life Insurance, Spouse/Committed Partner Life Insurance, and Accidental Death and Dismemberment coverage for individuals over age 70; therefore, effective January 1 of the year you or your Spouse will reach age 70, as applicable, your coverage amount for the applicable program will be reduced by 50% (regardless of whether your election rolls over or you affirmatively elect a coverage level during Annual Enrollment) and your premiums will be adjusted accordingly. 2013 ANNUAL ENROLLMENT 19 optional accidental death and dismemberment (ad&D) insurance Southwest offers the option to purchase Accidental Death and Dismemberment (AD&D) Insurance as part of the life insurance program to help provide for your family in the event of accidental death or dismemberment. You may elect AD&D Insurance coverage level of your choice and (i) upon the death of you or your Family Member you will receive a cash payout from MetLife equal to your coverage level, and (ii) upon the dismemberment of you or your Family Member you will receive a cash payout from MetLife that is equal to a percentage of your coverage level subject to certain limits. If you are enrolled in BenefitsPlus, you may purchase AD&D Insurance coverage up to ten times your annual base pay (increased from six times in 2012). If you are in the Regular Plan, then you may purchase AD&D Insurance up to your level of Basic Life Insurance. For the first time in 2013, if you are enrolled in BenefitsPlus, in addition to an Employee Only Coverage option, you will have the option to purchase Employee + Family Coverage. The Employee + Family option is not available to Employees enrolled in the Regular Plan. You may review your applicable monthly premium rates for AD&D Insurance in the online Annual Enrollment tool. beneficiary designation Updating your Beneficiary Designation: It is very important that MetLife have up to date beneficiary designations for Life Insurance and Accidental Death and Dismemberment Insurance. This ensures that MetLife can timely distribute the cash payments in the event of a death or dismemberment under the Life Insurance or Optional Accidental Death and Dismemberment Insurance programs. If you would like to update your beneficiary designations, access the MetLife website at www.metlife.com/mybenefits. Once registered on the MetLife website, you may change your beneficiary designation during Annual Enrollment or at any other time you would like to update this information. 20 2013 ANNUAL ENROLLMENT long term disability insurance (ltd) The Long Term Disability Insurance program is an insured product and, effective January 1, 2013, will be provided by CIGNA (not Aetna). Southwest offers you the opportunity to purchase Long Term Disability Insurance to help provide for you and your family in the event that you become disabled and cannot work for an extended period of time. Pilots are not eligible but may elect long term disability coverage through SWAPA. CIGNA is offering reduced rates for coverage in 2013. You can go to the online Annual Enrollment tool to calculate your 2013 premiums. Transition to CIGNA: The coverage option you currently have under the Aetna Long Term Disability program will automatically transfer to the Cigna Long Term Disability program if you do not make a new election. If you become disabled January 1 or later, your claim will be actively managed by Cigna’s Long Term Disability claims unit. If you currently have an active claim or become disabled prior to January 1, 2013, Aetna’s claims unit will continue to manage your claim until you return to work. Southwest will continue to offer the following long-term disability coverage options: BASIC LONG TERM DISABILITY INSURANCE: If you are enrolled in BenefitsPlus, you will be automatically enrolled in Basic Long Term Disability Insurance at no cost to you. If you have a qualifying disability, you would receive forty percent of your base salary. Basic Long Term Disability Insurance is not available if you are enrolled in the Regular Plan. OPTIONAL LONG TERM DISABILITY INSURANCE: If you are enrolled in BenefitsPlus or the Regular Plan and you would like to purchase Optional Long Term Disability Insurance, depending on your work group, you may purchase coverage that would provide you with up to sixty percent of your base salary. If you are enrolled in BenefitsPlus, then you may choose whether you would like to purchase this as a taxable benefit (your premiums will be deducted on an after-tax basis, a portion of the benefit you receive from the insurance carrier will be subject to tax) or a non-taxable benefit (your premiums will be deducted on an after-tax basis, the benefit you receive from the insurance carrier will not be subject to tax). If you are enrolled in the Regular Plan then your Optional Long Term Disability Insurance is a non-taxable benefit (your premiums will be deducted on an after-tax basis, the benefit you receive from the insurance carrier will not be subject to tax). If you need additional information about selecting the Long Term Disability Insurance option that is best for your family, please contact Health & Welfare Benefits. 2013 ANNUAL ENROLLMENT 21 benefitsplus voluntary benefits NEW FOR 2013! Southwest expanded the insurance programs available to Employees that enroll in BenefitsPlus. You now have the choice to purchase Supplemental Hospital Insurance, Auto Insurance, Homeowners Insurance, and/or Pet Insurance. All premiums are paid through payroll deductions. SUPPLEMENTAL HOSPITAL INSURANCE: During Annual Enrollment, Southwest Employees who enroll in BenefitsPlus will have the option of enrolling in Supplemental Hospital Insurance Plan effective January 1, 2013. Supplemental Hospital Insurance is an insured product provided by Combined Worksite Solutions. Southwest offers this option to Employees enrolled in the BenefitsPlus program to provide an additional cash resource in the event that you or a qualified family member is hospitalized. There are no health questions or medical exams required to purchase this insurance. Numerous exclusions apply to Supplemental Hospital Insurance including, but not limited to: (i) an individual that is pregnant as of the coverage effective date will not be eligible for a Supplemental Hospital Insurance benefit for days in the hospital in connection with maternity and (ii) treatment for being overweight, gastric bypass or stapling, intestinal bypass, and any related procedures, including complications is also excluded. For a complete list of exclusions you may review details in the materials from Combined Worksite Solutions that are posted on SWALife>About Me>My Benefits> Information and Forms. If you purchase supplemental Hospital Insurance, you will be eligible for up to $2,500 in payments per year for you and each qualified family member. Upon your or a qualified family member’s initial confinement to the hospital, you will receive $750. For each additional day in a regular hospital room during the year, you will receive an additional $250 per day up to three days. For each additional day in an ICU hospital room during the year, you will receive an additional $250 per day up to four days. Note: Supplemental Hospital Insurance does not replace coverage that you have under your BenefitsPlus medical option. Supplemental Hospital Insurance benefits are paid directly to you in cash to help you cover costs that may arise during your time in the hospital. You could use the money to pay deductibles or coinsurance in connection with your hospital stay or you could use the money to pay for any other need (e.g., your mortgage). Benefitsplus Supplemental Hospital Insurance Program Monthly Premium Rates EE ONLY $11.44 EE + SPOUSE EE + COMMITTED PARTNER $26.72 EE + CHILDREN $25.42 EE + FAMILY EE + COMMITTED PARTNER + FAMILY $39.68 AUTO/HOME INSURANCE: Effective January 1, 2013, Southwest Employees who enroll in BenefitsPlus will have the option of purchasing auto or homeowners insurance at discounted rates. The Auto/Home Insurance program is an insured product provided by MetLife Auto & Home (although note that home insurance is not offered in Florida or Massachusetts). Southwest used its sizable purchasing power to give Employees enrolled in the BenefitsPlus program the opportunity to purchase Auto Insurance and/or Homeowners Insurance at discounted rates. January 1, 2013, Employees enrolled in BenefitsPlus may call MetLife to request a quote and enroll. MetLife Auto & Home will obtain quotes from multiple insurance companies to determine your proposed rate. Additional information will be provided soon! PET INSURANCE: Effective January 1, 2013, Southwest Employees who enroll in BenefitsPlus will have the option to purchase pet insurance at discounted rates. The Pet Insurance program is an insured product provided by Veterinary Pet Insurance (VPI). Southwest used its sizable purchasing power to give Employees enrolled in the BenefitsPlus program the opportunity to purchase Pet Insurance at discounted rates. VPI policies cover wellness care as well as significant medical incidents. Pet Insurance offers you the chance to manage the risk associated with your pet’s medical issues. Additional information will be provided soon! 22 2013 ANNUAL ENROLLMENT clear skies employee assistance program ClearSkies Employee Assistance Program is a confidential program available to all Southwest Employees and family members from the day you join the Company. You do not have to be covered through one of the medical programs to be eligible. Southwest offers you the ClearSkies program so that you have a confidential resource to help you and your family deal with any personal problem that may affect your health, family life, or work including relationships, financial concerns, alcohol, drugs, stress, depression, and emotional distress. When you contact ClearSkies at 1-800-742-8911, a licensed counselor will assess your situation, determine what assistance is needed, and provide you possible resources for treatment. You may also access ClearSkies via the web at www.liveandworkwell.com and use pin number: swa737. wellness programs Southwest encourages you and your family to live well! In the coming months you will see more opportunities to participate in Wellness Programs including fitness challenges, fitness center discounts, weight management programs, and more! Additional information is online at SWALife>AboutMe>MyWellness. 2013 ANNUAL ENROLLMENT 23 IMPORTANT PHONE NUMBERS AND WEB SITES Would you like to check the status of a claim or the services that are available to you? The chart below lists web sites and phone numbers for your benefit administrators and providers. You may also access these from SWALife>AboutMe. BENEFIT PROGRAM NAME & PHONE NUMBER Medical Programs UnitedHealthcare (UHC) 877-246-0857 Group # 199409 ChOIce Plus Plan, Choice Plan C, Health Savings Plan, and ReguLAr Plan WEB SITE Find a Network Provider if not a member of UHC: www.myuhc.com/groups/nhswa To become a UHC member: Enter your Social Security number and desired password for access to www.myuhc.com Catamaran 800-451-3101 To find Network pharmacies in your area WalgreensHealth.com Optum Rx 877-246-0857 To find Network pharmacies in your area www.myuhc.com UnitedHealthcare (UHC) 877-311-7849 www.myuhc.com You must be enrolled in myuhc.com. Enter your Social Security number and desired password for instant access. OptumHealth Bank 800-791-9361 www.optumhealthbank.com You must provide a group number when opening an account: 199409 OptumHealth Behavioral Solutions 800-742-8911 Find a Provider www.liveandworkwell.com Use Pin Number: swa737 life events live and work well Life Events OptumHealth Behavioral Solutions (United Behavioral Health) 800-538-8310 Provides information for EAP, MHCD and Life Events www.liveandworkwell.com Use Pin Number: swa737 dental program Delta Dental 866-204-5502 Find a Network Dentist and Print ID Card www.deltadentalins.com/southwest vision program EyeMed Vision Care 855-219-4451 http://www.strata-g.com/eyemed/swa Long term disability PROGRAM Cigna 888-873-2127 www.cigna.com life insurance MetLife Call Center: 866-492-6983 Claims: 800-638-6420 #2 Statement of Health: 800-638-6420 #1 www.metlife.com/mybenefits Combined Worksite Solutions 800-964-7096 Web site coming January 1. 2013 Wage Works 877-924-3967 www.getwageworks.com/southwest Prescription drug program Choice Plus plan and choice Plan c Prescription drug program health savings plan and regular plan Flexible Spending Accounts health care FLEXIBLE spending account (available for Choice Plan Plus and Choice Plan C) dependent care FLEXIBLE spending account (Available for choice pLus plan, CHoice Plan C, and Health Savings Plan) health savings account (HSA) Health savings plan (HSP) only Clearskies employee assistance plan (EAP) and Mental health chemical dependency supplementAL hospital insurance BENEFITSPLUS commuter benefits Please note: The web site addresses included in this publication are accurate as of the printing of this piece. However, it is possible for site addresses to change from time to time.