The malleus, the heart of the tympanic
advertisement
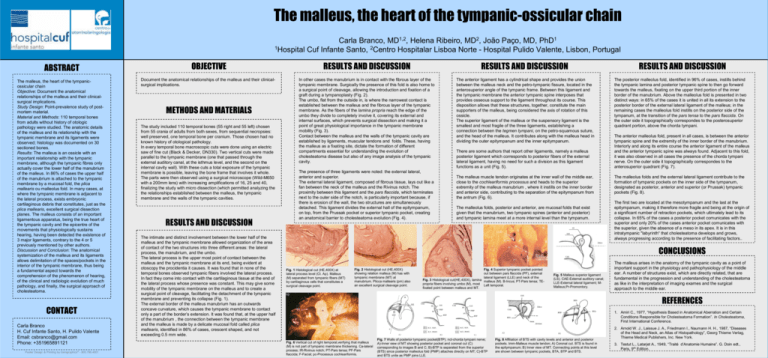
The malleus, the heart of the tympanic-ossicular chain Carla Branco, MD1,2, Helena Ribeiro, MD2, João Paço, MD, PhD1 1Hospital Cuf Infante Santo, 2Centro Hospitalar Lisboa Norte - Hospital Pulido Valente, Lisbon, Portugal ABSTRACT OBJECTIVE RESULTS AND DISCUSSION RESULTS AND DISCUSSION The malleus, the heart of the tympanicossicular chain Objective: Document the anatomical relationships of the malleus and their clinicalsurgical implications. Study Design: Point-prevalence study of postmortem material. Material and Methods: 110 temporal bones from adults without history of otologic pathology were studied. The anatomic details of the malleus and its relationship with the tympanic membrane and its ligaments were observed; histology was documented on 30 sectioned bones. Results: The malleus is an ossicle with an important relationship with the tympanic membrane, although the tympanic fibres only actually cover the lower half of the manubrium of the malleus. In 86% of cases the upper half of the manubrium is attached to the tympanic membrane by a mucosal fold, the plica mallearis ou malleolus fold. In many cases, at where the tympanic membrane is adjacent to the lateral process, exists embryonic cartilaginous debris that constitutes, just as the plica mallearis, excellent surgical dissection planes. The malleus consists of an important ligamentous apparatus, being the true heart of the tympanic cavity and the epicentre of the movements that physiologically sustains hearing, having been detected the existence of 3 major ligaments, contrary to the 4 or 5 previously mentioned by other authors. Discussion and Conclusion: The anatomical systemization of the malleus and its ligaments allows delimitation of the spaces/pockets in the interior of the tympanic membrane, thus being a fundamental aspect towards the comprehension of the phenomenon of hearing, of the clinical and radiologic evolution of much pathology, and finally, the surgical approach of cholesteatoma. Document the anatomical relationships of the malleus and their clinicalsurgical implications. In other cases the manubrium is in contact with the fibrous layer of the tympanic membrane. Surgically the presence of this fold is also home to a surgical point of cleavage, allowing the introduction and fixation of a graft during a tympanoplasty (Fig. 2). The umbo, flat from the outside in, is where the narrowest contact is established between the malleus and the fibrous layer of the tympanic membrane. As the fibers of the lamina propria reach the edge of the umbo they divide to completely involve it, covering its external and internal surfaces, which prevents surgical dissection and making it a point of great physiological importance in the tympanic membrane mobility (Fig. 3). Contact between the malleus and the walls of the tympanic cavity are established by ligaments, muscular tendons and folds. These, having the malleus as a fixating site, dictate the formation of different compartments essential for understanding the evolution of cholesteatoma disease but also of any image analysis of the tympanic cavity. The anterior ligament has a cylindrical shape and provides the union between the malleus neck and the petro-tympanic fissure, located in the anterosuperior angle of the tympanic frame. Between this ligament and the tympanic membrane the anterior tympanic spine interposes that provides osseous support to the ligament throughout its course. This disposition allows that these structures, together, constitute the main supporters of the malleus, being considered the axis of rotation of this ossicle. The superior ligament of the malleus or the suspensory ligament is the smallest and most fragile of the three ligaments, establishing a connection between the tegmen tympani, on the petro-squamous suture, and the head of the malleus. It contributes along with the malleus head in dividing the outer epitympanum and the inner epitympanum. CONTACT Carla Branco H. Cuf Infante Santo, H. Pulido Valente Email: csbranco@gmail.com Phone: +351965891121 Poster Design & Printing by Genigraphics® - 800.790.4001 METHODS AND MATERIALS The study included 110 temporal bones (55 right and 55 left) chosen from 55 crania of adults from both sexes, from sequential necropsies: well preserved, one temporal bone per cranium. Those chosen had no known history of otological pathology. In every temporal bone macroscopic cuts were done using an electric saw of fine cut (Black & Decker, DN330). Two vertical cuts were made parallel to the tympanic membrane (one that passed through the external auditory canal, at the isthmus level, and the second on the internal cavity wall). With these cuts a total exposure of the tympanic membrane is possible, leaving the bone frame that involves it whole. The parts were then observed using a surgical microscope (Wild-M650 with a 200mm lens) with increasing amplifications of 16, 25 and 40, finalizing the study with micro dissection (which permitted analyzing the the relationships established between the malleus, the tympanic membrane and the walls of the tympanic cavities. RESULTS AND DISCUSSION The intimate and distinct involvement between the lower half of the malleus and the tympanic membrane allowed organization of the area of contact of the two structures into three different areas: the lateral process, the manubrium, and the umbo. The lateral process is the upper most point of contact between the malleus and the tympanic membrane at its end, being evident at otoscopy the procidentia it causes. It was found that in none of the temporal bones observed tympanic fibers involved the lateral process. In fact they come into contact with the cartilaginous tissue at the end of the lateral process whose presence was constant. This may give some mobility of the tympanic membrane on the malleus and to create a surgical point of cleavage, facilitating the detachment of the tympanic membrane and preventing its collapse (Fig. 1). The external border of the malleus manubrium has an outwards concave curvature, which causes the tympanic membrane to contact only a part of the border’s extension. It was found that, at the upper half of the manubrium , the connection between the tympanic membrane and the malleus is made by a delicate mucosal fold called plica mallearis, identified in 86% of cases, crescent shaped, and not exceeding 0.5 mm wide. The presence of three ligaments were noted: the external lateral, anterior and superior. The external lateral ligament, composed of fibrous tissue, lays out like a fan between the neck of the malleus and the Rivinus notch. The proximity between this ligament and the pars flaccida, which terminates next to the outer side of the notch, is particularly important because, if there is erosion of the wall, the two structures are simultaneously detached. This ligament divides the external hall of the epitympanum, on top, from the Prussak pocket or superior tympanic pocket, creating an anatomical barrier to cholesteatoma evolution (Fig. 4). There are some authors that report other ligaments, namely a malleus posterior ligament which corresponds to posterior fibers of the external lateral ligament, having no need for such a division as this ligament functions as a unit (Fig. 5). The malleus muscle tendon originates at the inner wall of the middle ear, close to the cochleariformis processus and heads to the superior extremity of the malleus manubrium , where it instills on the inner border and anterior side, contributing to the separation of the epitympanum from the antrum (Fig. 6). The malleolus folds, posterior and anterior, are mucosal folds that exist given that the manubrium, two tympanic spines (anterior and posterior) and tympanic lamina meet at a more internal level than the tympanum. RESULTS AND DISCUSSION The posterior malleolus fold, identified in 96% of cases, instills behind the tympanic lamina and posterior tympanic spine to then go forward towards the malleus, fixating on the upper third portion of the inner border of the manubrium. Above the malleolus fold is presented in two distinct ways: in 65% of the cases it is united in all its extension to the posterior border of the external lateral ligament of the malleus; in the remaining cases the malleolus fold instills on the posterior side of the tympanum, at the transition of the pars tensa to the pars flaccida. On the outer side it topographically correspondes to the posterosuperior quadrant portion, above the chorda tympani. The anterior malleolus fold, present in all cases, is between the anterior tympanic spine and the extremity of the inner border of the manubrium. Interiorly and along its entire course the anterior ligament of the malleus and the anterior tympanic spine was always found. Adjacent to this fold, it was also observed in all cases the presence of the chorda tympani nerve. On the outer side it topographically correspondes to the anterosuperior quadrant (Fig. 7). The malleolus folds and the external lateral ligament contribute to the formation of tympanic pockets on the inner side of the tympanum, designated as posterior, anterior and superior (or Prussak) tympanic pockets (Fig. 8). The first two are located at the mesotympanum and the last at the epitympanum, making it therefore more fragile and being at the origin of a significant number of retraction pockets, which ultimately lead to its collapse. In 65% of the cases a posterior pocket comunicates with the superior and only 20% of the cases anterior pocket comunicates with the superior, given the absence of a meso in its apex. It is in this intratympanic "labyrinth“ that cholesteatoma develops and grows, always progressing according to the presence of facilitating factors.. CONCLUSIONS Fig. 1 Histological cut (HE,400X) at lateral process level (Ct. Ap). Malleus (M) separated from tympanic fibers (MT) by cartilaginous cells that constitutes a surgical cleavage point. Fig. 2 Histological cut (HE,400X) showing relation malleus (M) has with tympanic membrane (MT) at manubrium. Plicca mallearis (pm) also an excellent surgical cleavage point. Fig. 4 Superior tympanic pocket pointed out between pars flaccida (PF), external lateral ligament (LLE) and neck of the Fig. 3 Histological cut(HE,400X), lamina malleus (M). B-Incus; PT-Pars tensa; TEpropria fibers involving umbo (M), most Left temporal. fixated point between malleus and MT. Fig. 5 Malleus superior ligament (LS). CAE-External auditory canal; LLE-External lateral ligament; MMalleus;Pr-Promontory. The malleus arises in the anatomy of the tympanic cavity as a point of important support in the physiology and pathophysiology of the middle ear. A number of structures exist, which are directly related, that are fundamental in the progression and understanding of the cholesteatoma as like in the interpretation of imaging exames and the surgical approach to the middle ear. REFERENCES 1. Amiri C., 1977, “Hypothesis Based in Anatomical Aberration and Certain Conditions Responsible for Cholesteatoma Formation”. In Cholesteatoma, First International Conference. Fig. 6 Vertical cut of right temporal,verifying that malleus (M) is not part of tympanic membrane thickening. Ca-lateral process; IR-Rivinus notch; PT-Pars tensa; PF-Pars flaccida; F-Facial; pc-Processus cochleariformis. Fig. 7 Walls of posterior tympanic pocket(BTP). nct-chorda tympani nerve; A)-Inner view of MT showing posterior pocket and coronal cut (C) corresponding to images B and C; B)-BTP is separated from the superior (BTS) since posterior malleolus fold (PMP) attaches directly on MT; C)-BTP and BTS unite as PMP joins LLE. Fig. 8 Affiliation of BTS with cavity levels and anterior and posterior pockets. tmm-Malleus muscle tendon; A) Coronal cut. BTS is found in the epitympanum; B) Inner view of MT. Connecting points at this level are shown between tympanic pockets, BTA, BTP and BTS. 2. Arnold W. J., Laissue J. A., Friedmann I., Naumann H. H., 1987, “Diseases of the Head and Neck, an Atlas of Histopathology”, Georg Thieme Verlag, Thieme Medical Publishers, Inc. New York. 3. Testut L., Latarjet A., 1949, “Traité d’Anatomie Humaine”. G. Doin edt., Paris, 9th Edition.