Schizophrenia
advertisement

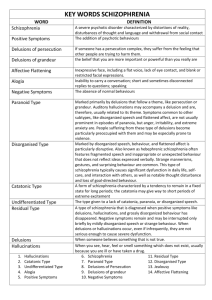
Schizophrenia Davison, G.C. and Neale, J.M. Abnormal psychology. (2001). Chapter 11. (pp.282-316) Diagnosis • Is based entirely upon psychiatric history and MSE History Emil Kraepelin • In 1898 19th century • described the disorder as dementia praecox • As a dementia early in life – so distinguished from dementia in older ages Eugen Bleuler • In 1908 created the term schizophrenia for this disorder • Means split mind schizein = split and phren=mind Bleuler Four As • • • • Association Autism Affect Ambivalence Schneider first rank symptoms • • • • Audible thoughts Arguing or discussing voices Somatic hallucination Thought withdrawal, Broadcasting, insertion • Delusional perception How common is it? Lifetime prevalence • Is approximately 1% (0.7-2%) • Equally affects males and females • But it starts early in males (teens, early 20s) • And later in females (20s-30s) When it starts? • it starts early in males (teens, early 20s) • And later in females (20s-30s) • Sometimes in childhood • Have several acute episodes and less severe episodes between the acute episodes Infection and birth season • • • • • Born in the winter and early spring Exposure to influenza Maternal starvation Rh incompatibility Age of the father Biochemical Factors • Dopamine Hypothesis • Serotonin…. Positive and negative symptoms • Norepinephrine……. Anhedonia • GABA….. Regulate the dopaminergic system • Glutamate…….. Phencyclidine Excessive pruning • Pruning of synapses during adolescence Is it one disorder? No.… • heterogeneity • Has 5 subtypes • 2 symptom clusters (positive and negative) Doctor-patient interaction…. D.: Have you been nervous or tensed lately? P.: No, I got a head of lettuce. D.: You got a head of lettuce? I do not understand. P.: Well, lettuce is a transformation of a dead cougar that suffered a relapse on the lion’s toe. And he swallowed the lion and something happened. See. Tommy and Gloria they are two heads and they are not whales. But they escaped with herds of vomit and things like that…. POSITIVE SYMPTOMS Characteristics: • Excesses or distortions • Have sudden onset /acute episodes/ • And good response to medication • 2 symptom clusters (positive and negative) What these symptoms are? 1. Disorganized speech 2. Incoherence 3. Loos associations 4. Delusions 5. Hallucinations 6. Bizarre behaviour Disorganized speech • Problems in organizing ideas and telling them so others could also understand it • Once these symptoms were central • many patients’ speech is not disorganized • And speech can be disorganized in other psychoses as well (mood disorders, manic state) • It is a diagnostic symptoms but not the principal symptom D: Who are Tommy and Gloria? P.:there is Joe DiMaggio, Tommy Henrich, Bill Dickey, Phil Rizzuto, John Esclavera, Del Grandell, Ted Williams… D.: Who are they? P.: Dead people… they want to be fucked …. By this outlaw… Incoherence • Many times it is hard to follow their speech • They might make references to their central ideas but it is not connected to the other part of their speech Loose associations • Patient has difficulty sticking to one topic • Trains of associations – very difficult to follow • “my thoughts just jumbled up. I start thinking about something but I never get there. My trouble is that I have got too many thoughts.” Delusions • Beliefs held contrary to the reality • Very common symptoms in schizophrenia 65% • Also found in mania, delusional depression • But delusions are schizophrenia are the most bizarre from all of these • • • • • • • Delusions that people are spying them Bodily sensations by external agency Own Thoughts had been replaces by others’ Their thoughts are broadcast or transmitter Thoughts are stolen from them Feeling or behaviour is controlled by external force Impulses to do something (again not exclusive to schizophrenia • “I am thinking about my mother and suddenly my thoughts are sucked out of my mind by a phrenological vacuum extractor and there is nothing in my mind, it is empty.” • “I look out the window and I think the garden looks nice and the grass looks cool, but the thoughts of Eemonn Andrews come into my mind There are no other thoughts there, only his. He treats my mind like a screen and flashes his thoughts on it like you flash a picture” Disorders of perception and Hallucinations • The world is unreal • Depersonalised feeling from the body • Hallucinations: sensory experiences in the absence of any stimulation from the environment • Hallucinations are mainly auditory (74% and can be frightening • A patient reports hearing a man;s voice speaking with intense whisper to her. The voice repeats most of the patient’s goal-directed thinking. • A housewife experienced a voice was commenting her behaviour from a house across the road with critical comments. NEGATIVE SYMPTOMS Characteristics: • Behavioural deficits • Chronic course • poor good response to medication • Many negative symptoms are predictors of poor prognosis • (side effect of medications!) What these symptoms are? 1. Avolition - apathy 2. Alogia 3. Anhedonia 4. Flat affect 5. Asociality Avolition – apathy • Lack of energy • Absence of interest • Patients do not care with themselves just sitting around doing nothing Alogia • Poverty of speech • Or they speak enough, but without content Anhedonia • Inability to experience pleasure • Do not enjoy recreation, or others’ company • Usual pleasure activities are not enjoyable for these persons Flat affect • No stimulus can elicit emotions • 66% of patients have this symptom • EMG while watching emotions: patients with schizophrenia had less intense facial activity, while the same self-report of feelings Asociality • Some patients have severe impairment in their social relationships • Fewer friends • Poor social skills • Sometimes these symptoms are present before the other symptoms even in childhood OTHER SYMPTOMS Catatonia • Motor abnormality • Repeated gestures with peculiar movements • Sometimes unusual activity and lots of energy in movements (similarly as in mania) • At the other end : catatonic immobility – patients stay in unusual postures for long time • Waxy flexibility :you can place the patients’ limbs in any position, then they will maintain it for long time OTHER SYMPTOMS Inappropriate affect • Rapid shift from one emotional state to other • Inappropriate affect – laughing at sad stories or anger at a simple question • Not frequent, but if present an important diagnostic symptom Consequences • Of these symptoms are devastating • Loss of friends • Job • Money, home • Substance abuse • suicide Suicide & Homicide • 20-50% of patients • 80% have a MMD episode • Best prognosis related to highest risk of suicide • 2/3 have seen the clinician 72 hours before death • The patients are no more commit homicide than general population HOW TO DIAGNOSE? DSM-IV diagnosis At least two of these symptoms must present for at least one month: • Delusion • Hallucinations • Disorganized speech • Disorganized behaviour or catatonic • Negative symptoms One symptoms is enough if • That symptoms is hallucination of voices • Or bizarre delusions HOW TO DIAGNOSE? DSM-IV diagnosis Diagnosis require 6 month of disturbance (including the one month with the specific symptoms) in the rest of the time symptoms are: • Social withdrawal • Lack of initiative • Vague or circumstantial speech • Impairment in hygiene • Odd beliefs • Magical thinking • Unusual perceptual experiences HOW TO DIAGNOSE? DSM-IV diagnosis What is NOT schizophrenia? • Mood disorders • Schizoaffective disorder • And not drug induced symptoms • Delusional disorder related but not schizophrenia SUBTYPES 1. Disorganized Incoherent speech and thoughts 2. Catatonic Negative symptoms are dominant 3. Paranoid Presence of prominent delusions 4. Undifferentiated Meet the diagnostic criteria of schizophrenia but do not fit to subtypes 5. Residual No longer schizophrenic but shows symptoms of the illness Disorganized schizophrenia Main symptoms: • Disorganized speech difficult to follow • Incoherence • Inventing new words • Labile affect – flat affect or shifts in moods • Behaviour is disorganized and not goal directed • Neglects his/her appearance, hygiene Characteristics • Rare • Poor prognosis • More typical to schizophrenia with early onset Catatonic schizophrenia Main symptoms: • Motor symptoms ranging from • excitement to (talks continuously, shouts, nervous, etc.) • Immobility (can be waxy rigidity, mute) Characteristics • Sudden onset • Good prognosis to medications • Similarities to encephalitis lethargica Paranoid schizophrenia Main symptom: • Present of delusions • Grandiose delusions – exaggerated sense of their own importance • Delusional jealousity (about their partners’ faith) • Persecution, being spied on, etc. • Ideas of reference: unimportant events get unrealistic importance in their thought • Agitated, emotional, sometimes violent • Language is not disorganized Characteristics • Good prognosis to medication Cognitive-Behavioral Classification • Sensitivity disorder Genetically weighted, begin in adolescence, low stress, negative symptoms • Anxiety disorder delusions arise after intense anxiety, middle life, systematized delusion, positive symptoms • Traumatic psychosis trauma, often sexual assault, borderline traits(2/3 of female chronic hallucinators have suffered from childhood sexual abuse) • Drug-induced psychosis High EE in family, poor comliance • Catatonia oxford texbook of psychotherapy ETIOLOGY OF SCHIZOPHRENIA 1. 2. 3. 4. 5. 6. Genetics Biochemical/biological Abnormal brain function and structure Stress and schizophrenia Some other factors and predictors And we basically do not know exactly… GENETIC FACTORS Schizophrenia has a genetic component • Increased risk as the genetic relationship is closer • • • • • first cousins, nieces, uncles, aunts – 2-3% Parents : 9% Siblings : 7% Dizygotic twins 12% Monozygotic twins 44% - but not 100% so genetic factors are not solely responsible for schizophrenia GENETIC FACTORS Schizophrenia has a genetic component Adoptions studies • 50 children of schizophrenic women separated and adopted at birth compared with 50 children of non-schizophrenic women adopted at birth • Later assessed: none control but 16.6% of the schizophrenic group did have schizophrenia In general •Not a single gene but more genes are responsible •Genetically based factors (such as eye-tracking) are impaired in schizophrenia and in their relatives too BIOCHEMICAL FACTORS Dopamine theory • Antipsychotic drugs are effective treatment for Sch. They block postsynaptic dopamine (D2) receptors • Amphetamines – cause release of catecholamines including dopamine and prevent their inactivation – can induce psychosis How the dopamine theory works? • People with Sch do not have more dopamine in their brain but • More D2 receptors and oversensitive receptors Neurotransmitters Presynaptic neuron Terminal Buttons (end of the presynaptic cell) Synapsic cleft Receptors Postsynaptic membrane Postsynaptic neuron BIOCHEMICAL FACTORS Brain injury in the prefrontal cortex DA neurons underactive in the PFC Negative symptoms Mesolimbic dopamine system is Out of inhibitory control Positive symptoms BIOCHEMICAL FACTORS Dopamine theory • Controversial • Long time (more weeks) until the antipsychotics start to be effective, however, blockade of dopamine starts immediately • Receptor activity must be brought below normal for therapeutic effect – why normal activity is not enough? catecholamines including dopamine and prevent their inactivation – can induce psychosis BIOCHEMICAL FACTORS Serotonergic theory Role of the glutamates • Low level of glutamate • Low level of enzymes to produce glutamate • Decrease of glutamate from the prefrontal cortex could produce increased dopaminerg activity in the limbic system and in the striatum THE BRAIN IN SCHIZOPHRENIA Abnormalities on series of tests testing attention memory emotions social behaviour perceptual/motor integration Other abnormalities • Abnormal eye-tracking (low level neural systems) • Abnormal habituation (sensory gating) • Abnormal facial muscle activity (affect) THE BRAIN IN SCHIZOPHRENIA Where is the problem in the brain structure? studies with various neuroimaging methods (MRI, fMRI, PET, EEG, MEG) Enlarged ventricles • Probably from increased subcortical cell loss Frontal cortex • Reduced grey matter Temporal lobe • Amygdala (reduced volume) • Hippocampus (reduced volume) Reduced volume of basal ganglia Prefrontal theory 1. impairments in series of neuropsychological test (Wisconsin test for example) 2. Frontal cortex plays role in speech, decision making – disrupted in schizophrenia 3. Reduced grey matter in the frontal cortex with structural imaging 4. Neuroimaging (PET and fMRI) studies show less activation in the frontal cortex 5. Frontal activation is related to negative symptoms of schizophrenia Major difference between controls and patients with schizophrenia In this word-encoding task is the activation of the frontal cortex In control, but the lack of the activation in schizophrenic subjects Temporal lobe dysfunction 1. Volume reduction in the temporal lobes 2. Volume reduction in the left posterior temporal gyrus (language processing) 3. Volume reduction in the superior temporal gyrus (auditory cortex – hallucinations) 4. Reduced volume of hippocampus (related to memory problems) 5. Abnormal activity of the amygdala – in positive symptoms (problems with emotion) PSYCHOLOGICAL STRESS How stress can be related to schizophrenia? Stress HPA axis (hypothalamic-pituitary-adrenerg) Cortisol DOMAPINE INCREASED SYMPTOMS OF SCHIZOPHRENIA Middle and superior temporal gyrus activation is reduced with The increasing severity of schizophrenia. Contributes to incoherent Speech (Kircher et al.; Arch. Gen. Psyxhiatry, 2001, 58:769-774) STRESS AND SCHIZOPHRENIA 1. Life-stress increases the likelihood of relapses 2. People with the lowest social class have the highest prevalence for schizophrenia 1. Sociogenic hypothesis – stress comes from the social status 2. Social selection-theory (people with schizophrenia will drift to the poverty sooner or later 3. Studies with immigrants supports more the social-selection hypothesis FAMILY AND SCHIZOPHRENIA 1. Theory of schizophrenogenic mother – and double-bind theory is not supported by research cold, rejecting, overprotective, rigid, moralistic, fearful about intimacy Double-bind: apparent gap between verbal and nonverbal communication and expectations 2. Level of expressed emotions in the family introduce a vicious circle family members criticise bizarre thoughts of patients this in turn elicit to express more bizarre thoughts from patients! DEVELOPMENTAL MODELS 1. Influenza infection in pregnancy seasonal changes in birth of schizophrenic people: there is a winter-spring excess of births higher rate of schizophrenia in children neurodevelopmental model. Virus disrupts the developing brain 2. Complications at birth hypooxygenia, acidaemia Prognosis • 20-30% somewhat normal life • 70% achieved remission • First episode: 1-2 years treatment may not adequate • Multiepisode: 5 years or for lifetime THERAPY 1. Biological therapy 1. Surgery, shock 2. Drug therapies 2. Psychological therapy 1. Psychodynamic therapy 2. Social-skill training 3. Family therapy 4. Cognitive-behavioural therapy Surgery and shock therapy Electroconvulsive (ECT) therapy rarely used Insulin coma (not used) Prefrontal lobotomy – not used 1. Neuroleptic drugs 1. Block the postsynaptic dopaminerg receptors 2. Reduce positive symptoms (but not the negatives) 3. For example phenotiazine and chlorpromazine 4. 70% of patients respond well 5. Maintainance doses are needed continusouly 6. Extrapyramidal side effects (similar to Parkinson disorder) tremor, gait, akasthesia, tardive dyskinesia, neuroleptic malignant syndrome Atypical neuroleptic drugs 1. Clozapine (Clozaril) 1. Fewer motor side effects 2. But destroys the immune system 2. Olanzapine (Zyprexa) and risperidone (Risperdal) 1. Fewer side effects 2. Affect memory, cognition, attention 3. Affects the serotonergic system too