Zaky SS, Seif J, Abd-Elsayed AA, Bashour CA
advertisement

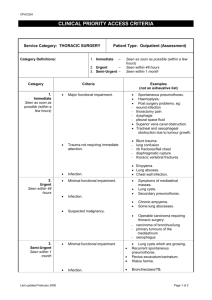
5471 MAS MINERVA MEDICA COPYRIGHT® MINERVA ANESTESIOL 2009;75 CLINICAL CASES Recurrent lung collapse due to unidentified phrenic nerve injury after cardiac surgery S. S. ZAKY 1, J. SEIF 1, A. A. ABD-ELSAYED 2, C. A. BASHOUR 3 1Department of Anesthesia, Cleveland Clinic, Cleveland, OH, USA; 2Department of Outcomes Research, Anesthesia, Cleveland Clinic, Cleveland, OH, USA; 3Department of Cardiothoracic Anesthesia, Cleveland Clinic, Cleveland, OH, USA ABSTRACT Partial or complete recurrent lung collapse after cardiac surgery is one cause of failure to wean from ventilator support, and frequently leads to multiple reintubations and prolonging intensive care unit and hospital stays. A 79-year-old female underwent uneventful coronary artery bypass surgery and was extubated on the first postoperative day (POD). On POD 2, a routine portable chest X-ray (CXR) revealed complete opacification of the left hemithorax. The patient was readmitted to the Cardiovascular Intensive Care Unit (CVICU) and electively intubated, and bronchoscopy revealed a left mainstem bronchus mucous plug. The patient was extubated uneventfully the same day. A CXR on the next day revealed recurrent total collapse of the left lung, which this time was successfully treated non-invasively with intermittent CPAP mask, percussive therapy, and respiratory treatments using acetylcysteine solution. After several days, the left lung collapsed again, necessitating reintubation and repeat bronchoscopy. With Pulmonary medicine present, the patient was subsequently extubated so that bronchoscopy could be performed while the patient was breathing spontaneously. This examination revealed dynamic collapse of the left lower lobe bronchus. A sniff test was performed and revealed an immobile left hemi-diaphragm. The patient gradually became stronger, and as the airway edema subsided, she was able to be managed on the regular nursing floor with intermittent CPAP mask treatments and mucolytics. Although uncommon, one documented cause of failure to wean from mechanical ventilation is diaphragmatic dysfunction. This finding is often delayed because it requires a sniff test in an extubated patient to make the diagnosis. Key words: Phrenic nerve - Thoracic surgery - Heart, surgery - Postoperative complications. P artial or complete recurrent lung collapse after cardiac surgery is one cause of failure to wean from ventilator support and usually leads to multiple reintubations. This prolongs cardiovascular intensive care unit (CVICU) and hospital lengths of stay, and increases the risks of airway injury and ventilator acquired pneumonia. Common causes of single episodes of postoperative lung collapse include right or left mainstem bronchus intubation, atelectasis, and pneumonia.1 Less commonly, the collapse can recur either due to airway pathology and/or diaphragmatic dysfunction.2-5 Recurrent lung collapse due to paralysis of the diaphragm may occur because of a phrenic nerve Vol. 75 - 2009 injury, especially after the repair of complex congenital anomalies, or due to topical heart cooling.6-9 We describe a case of recurrent total collapse of the left lung of a 79-year-old female after cardiac surgery due to both dynamic airway collapse and diaphragmatic dysfunction. Case report A 79-year-old female with a past medical history significant for 50 years of smoking up until one month before surgery, coronary artery disease, and hypertension underwent MINERVA ANESTESIOLOGICA 1 MINERVA MEDICA COPYRIGHT® ZAKY RECURRENT LUNG COLLAPSE Figure 1.—Complete collapse of the left lung. Figure 3.—Left main bronchus with the patient breathing spontaneously (No PEEP). Figure 2.—CXR after bronchoscopy and pulmonary treatment. an uneventful coronary artery bypass surgery and aortic valve replacement for aortic valve stenosis. A mediastinal tube was inserted in the operating room. On the first postoperative day (POD 1), her chest x-ray (CXR) was unremarkable and blood gases were normal. She was transferred to the step down floor. On POD 2, the mediastinal tube was removed. A routine portable CXR revealed complete opacification of the left hemithorax (Figure 1). The provisional diagnosis was collapse due to mucous plugging of the left main bronchus, given the patient’s long history of smoking. Pleural effusion was not suspected as this usually develops slowly. A hemothorax was also considered less likely due to the rapid change in the CXR without significant change in the hematocrit or hemodynamic stability. A computed tomography scan of the chest showed lung collapse without extrinsic airway compression and no pleural effusions. The patient was readmitted to the CVICU and elective- 2 Figure 4.—Left main bronchus after application of PPV and PEEP of 5. ly intubated, and bronchoscopy revealed a left mainstem bronchus mucous plug that was removed and sent for culture and sensitivity. An immediate CXR after bronchoscopy showed re-expansion of the left lung (Figure 2). The patient was extubated that day uneventfully and observed in the CVICU overnight. A CXR on the next day revealed recurrent total collapse of the left lung, this time successfully treated using non-invasive ventilation with intermittent CPAP mask, percussive therapy, and respiratory treatments using acetylcysteine solution. After several days, however, the left lung again collapsed, MINERVA ANESTESIOLOGICA Vol. 75 - 2009 MINERVA MEDICA COPYRIGHT® RECURRENT LUNG COLLAPSE ZAKY the patient was reintubated, and repeat bronchoscopy was performed to reexpand the lung. Due to the recurrent nature of the left lung collapse with no extrinsic compression and no episodes of collapse of the right lung, intrinsic pathology of the left lung was at this point thought to be more likely. Pulmonary medicine was consulted and the patient was subsequently extubated so that awake bronchoscopy could be performed with the patient breathing spontaneously. This examination revealed dynamic collapse of the left lower lobe bronchus (Figures 3, 4). This finding, together with the postoperative course of the patient, suggested the diagnosis of left diaphragmatic paralysis secondary to phrenic nerve palsy after the surgery. A fluoroscopic sniff test was performed with the patient extubated, revealing an immobile left hemi-diaphragm. The patient gradually became stronger and as the airway edema subsided, she could be managed on the regular nursing floor with intermittent CPAP mask treatments and mucolytics. The patient was eventually discharged home on postoperative day 27 in stable condition. The patient had outpatient follow-up at six months with stable respiratory function at that time. the airway caused by paralysis of the diaphragm on the same side. In this case, the bronchus to the left lower lobe could be seen collapsing while the patient breathed spontaneously. The collapse could be due to an intrinsic abnormality in the airway secondary to her long-standing bronchitis and tissue edema, and then made worse by diaphragmatic dysfunction. This leads to the generation of increased negative pressure on the opposite side, which rapidly sucks air out of the affected lung collapsing the ipsilateral airway. Due to recurrent narrowing of the airway with each breath, a mucous plug can form that then leads to lung collapse. As in this case, the patient must be supported with aggressive respiratory therapy that includes mucolytics, CPAP mask, and percussive therapy until they become strong enough to match the increased work of breathing required to overcome the deficit.11, 12 Discussion Although uncommon, one cause of failure to wean from mechanical ventilation after cardiac surgery is diaphragmatic dysfunction.3 The diagnosis is often delayed because it happens infrequently and the diagnostic fluoroscopic sniff test usually requires a patient to be extubated as positive pressure ventilation can potentially obscure the x-ray. Postoperative lung collapse after surgery is frequently due to mucous plugging, but must be differentiated from a hemothorax, which has a similar appearance.10 Distinguishing features of collapse versus hemothorax typically include an “overnight” change in the CXR with lung collapse in a patient without significant change in the hemodynamic status or hematocrit. The volume require for a hemothorax to give the same appearance as a collapsed lung is over two liters in an adult, and should be associated with changes in either the hemodynamics or the hematocrit. If a pleural effusion is suspected, chest ultrasound can make the diagnosis. In this case, collapse was considered more likely and thus chest CT was more useful as an initial study. Awake bronchoscopy is a valuable tool in this situation, as it can demonstrate dynamic collapse of Vol. 75 - 2009 Conclusions Although uncommon, one documented cause of failure to wean from mechanical ventilation is diaphragmatic dysfunction. This finding is often delayed because the diagnosis requires a sniff test in an extubated patient. References 1. Göran H. When shall the lung be opened up: During or after cardiac surgery? Crit Care Med 2005;33:2425-6. 2. Joho-Arreola AL, Bauersfeld U, Stauffer UG, Baenziger O, Bernet V. Incidence and treatment of diaphragmatic paralysis after cardiac surgery in children. Anesthesiology 2005;102:690-2. 3. Mertens L. Diaphragmatic paralysis after cardiac surgery: how to look at it? Pediatr Crit Care Med 2006;7:491-2. 4. Dagan O, Nimri R, Katz Y, Birk E, Vidne B. Bilateral diaphragm paralysis following cardiac surgery in children: 10-years’ experience. Intensive Care Med 2006;32: 1222-6. 5. Miñambres E, García García A, Rodriguez Borregan J, Antolínez Eizaguirre X, Gutiérrez Morlote J, San José Garagarza J. Bilateral diaphragm paralysis after cardiac surgery. Arch Bronconeumol 2001;37:454-6. 6. Akay TH, Ozkan S, Gultekin B, Uguz E, Varan B, Sezgin A et al. Diaphragmatic paralysis after cardiac surgery in children: incidence, prognosis and surgical management. Pediatr Surg Int 2006;22:341-6. 7. Xu WD, Gu YD, Lu JB, Yu C, Zhang CG, Xu JG. Pulmonary function after complete unilateral phrenic nerve transection. J Neurosurg 2005;103:464-7. 8. Lemmer J, Stiller B, Heise G, Hübler M, Alexi-Meskishvili V, MINERVA ANESTESIOLOGICA 3 MINERVA MEDICA COPYRIGHT® ZAKY RECURRENT LUNG COLLAPSE Weng Y et al. Postoperative phrenic nerve palsy: early clinical implications and management. Intensive Care Med 2006;32:1227-33. 9. McCaul JA, Hislop WS. Transient hemi-diaphragmatic paralysis following neck surgery: report of a case and review of the literature. J R Coll Surg Edinb 2001;46:186-8. 10. Piccini JP, Nilsson KR. The Osler Medical Handbook. 2nd edition. Philadelphia: Saunders Elsevier; 2006.p.5. 11. Hoch B, Zschocke A, Barth H, Leonhardt A. Bilateral diaphragmatic paralysis after cardiac surgery: ventilatory assistance by nasal mask continuous positive airway pressure. Pediatr Cardiol 2001;22:77-9. 12. Takeda S, Miyoshi S, Maeda H, Minami M, Yoon HE, Tanaka H et al. Ventilatory muscle recruitment and work of breathing in patients with respiratory failure after thoracic surgery. Eur J Cardiothorac Surg 1999;15:449-55. Received on December 5, 2008 - Accepted for publication on March 05, 2009. Corresponding author: A. A. Abd-Elsayed, MD, MPH, Outcomes Research Department, 9500 Euclid Avenue/P77, Cleveland, OH 44195, USA. E-mail: Abd-ela@ccf.org 4 MINERVA ANESTESIOLOGICA Vol. 75 - 2009