Anatomy and Physiology of Eye Movements
advertisement

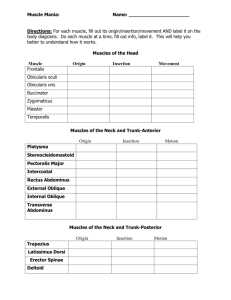
2 Anatomy and Physiology of Eye Movements Kenneth W. Wright OCULAR POSITION Within the orbit, the eye is suspended by six extraocular muscles (four rectus muscles and two oblique muscles), suspensory ligaments, and surrounding orbital fat (Fig. 2-1). A tug-of-war exists between the rectus and oblique muscles. The four rectus muscles insert anterior to the equator, and pull the eye posteriorly, while the two oblique muscles insert posterior to the equator providing anterior counterforces. Posterior orbital fat also pushes the eye forward. If rectus muscle tension increases, the eye will be pulled back causing enophthalmos and lid fissure narrowing. Simultaneous cocontraction of the horizontal rectus muscles in Duane’s syndrome, for example, can cause significant lid fissure narrowing and enophthalmos. In contrast, decreased rectus muscle tone causes proptosis and lid fissure widening. Conditions such as muscle palsies or a detached rectus muscle allow the eye to move forward and result in lid fissure widening. Rectus muscle tightening procedures such as resections tend to cause lid fissure narrowing whereas loosening procedures such as rectus recessions induce lid fissure widening. When the eye is looking straight ahead with the visual axis parallel to the sagittal plane of the head, the eye is in primary position. The vertical rectus muscles follow the orbits and diverge from the central sagittal plane of the head by 23°. Thus, the visual axis in primary position is 23° nasal to the muscle axis of the vertical rectus muscles (Fig. 2-2). This discrepancy between the vertical rectus muscle axis and the visual axis of the eye explains the secondary and tertiary functions of the vertical rectus muscles (see muscle functions, following). 24 Whitnall's lig. Superior oblique m. Levator palpebrae Müller's m. Superior rectus m. Intraconal fat Lateral rectus m. Inferior rectus m. Lockwood's lig. Extraconal fat Inferior oblique m. FIGURE 2-1. Side view of extraocular muscles. Note that the rectus muscles pull the eye posteriorly while the oblique muscles pull the eye anteriorly. FIGURE 2-2. Diagram shows visual axis versus muscle/orbital axis. Note that the visual axes parallel the central sagittal plane, while the orbital axis of each eye diverges 23° from the visual axis. 25 26 handbook of pediatric strabismus and amblyopia The term position of rest refers to the position of the eyes when all the extraocular muscles are relaxed or paralyzed. Normally, the position of rest is divergent (i.e., exotropic), with the visual axis in line with the orbital axis. The eyes of a patient under general anesthesia are usually deviated in a divergent position. OCULAR MOVEMENTS Ductions The term ductions is used to describe monocular eye movements without regard for the movement of the fellow eye (Fig. 2-3). Ductions result from an extraocular muscle contraction A B E C F D G FIGURE 2-3A–G. Diagram of ductions, which are monocular eye movements. 27 chapter 2: anatomy and physiology of eye movements TABLE 2-1. Extraocular Muscles. Muscle Medial rectus Lateral rectus Superior rectus Approximate muscle length (mm) Origin 40 40 40 Annulus of Zinn Annulus of Zinn Annulus of Zinn Anatomic insertion (mm) Tendon Arc of length contact (mm) (mm) Action from primary position 5.5 4 6 Adduction 7.0 8 10 Abduction 8.0 6 6.5 6.5 7 7 26 12 1 15 Inferior rectus 40 Annulus of Zinn Superior oblique 32 Inferior oblique 37 Orbit apex From above temporal annulus pole of of Zinn superior rectus to within 6.5 mm of optic nerve Lacrimal Macular fossa area Elevation Adduction Intorsion Depression Adduction Extorsion Intorsion Depression Abduction Extorsion Elevation Abduction that pulls the scleral insertion site toward the muscle’s origin while the opposing extraocular muscle simultaneously relaxes. The contracting muscle is referred to as the agonist and the relaxing muscle as the antagonist. An upward movement of an eye is referred to as supraduction or sursumduction, a downward movement is termed infraduction or dorsumduction, a nasal-ward movement is termed adduction, and a temporal movement is termed abduction. Torsional rotations (twisting movements) are known as cycloductions, with incycloduction (intorsion) referring to a nasal rotation of the 12 o’clock position of the cornea and excycloduction (extorsion) referring to a temporal rotation of the 12 o’clock position. Muscle Action Versus Field of Action The terms “muscle action” and the “field of action” are often confused. Muscle action refers to the effect of muscle contraction on the rotation of the eye when the eye starts in primary position. Table 2-1 lists the muscle actions of each extraocular muscle. Horizontal rectus muscles have but one action: horizontal rotation of the eye. Vertical rectus and oblique muscles, 28 handbook of pediatric strabismus and amblyopia however, have three actions: vertical, horizontal, and torsional. The most robust action is termed the primary action, followed by the less obvious secondary and tertiary actions. It is important to remember the classic descriptions of primary, secondary and tertiary muscle actions as they relate to the eye when it is in primary position. In contrast, the field of action of a muscle is the position of gaze when an individual muscle is the primary mover of the eye. Granted, virtually all eye movements are the result of combined contraction and relaxation of multiple muscles, but there are eight positions of gaze where one muscle provides the dominant force (Fig. 2-4). For example, when one looks up, the brain recruits both the superior rectus and the inferior oblique muscles. Looking up and nasal, however, is the primary function of the inferior oblique muscle, so this is the field of action of the inferior oblique muscle. A muscle’s function is best evaluated by having the patient look into the field of action of the FIGURE 2-4. Diagram of the field of action of the extraocular muscles. Arrows point to the quadrant where the specified muscle is the major mover of the eye. SR, superior rectus; IR, inferior oblique; MR, medial rectus; SO, superior oblique; IO, inferior oblique; IR, inferior rectus; LR, lateral rectus. chapter 2: anatomy and physiology of eye movements 29 muscle. Thus, even though the secondary action of the inferior oblique muscle is abduction, evaluate inferior oblique function by having the patient look “up and nasal.” A patient with an inferior oblique palsy will show limitation of eye movement up and nasal. Note, for straight upgaze, the superior rectus muscle is the major elevator, and for straight down-gaze the inferior rectus is the major depressor, with the oblique muscles contributing little. Smooth Pursuit Versus Saccadic Eye Movements There are two basic forms of eye movements: smooth pursuit and saccadic. Smooth pursuit eye movements are generated in the occipital parietal temporal cortex, with the right cortex controlling movements to the right and the left cortex controlling movements to the left. In humans, smooth pursuit first occurs at 4 to 6 weeks of age. These are slow accurate eye movements requiring visual feedback from central foveal fixation. Smooth pursuit eye movements can follow visual targets moving at velocities up to 30° per second (30°/s). Clinically, accurate smooth pursuit indicates central fixation and in preverbal children is an indication of good vision. Saccadic movements are rapid eye movements with velocities usually ranging from 200° to 700°/s, but saccades have been recorded up to 1000°/s. The peak velocity increases as the amplitude of the movement increases, and this relationship is termed the main sequence. Saccades are movements used to keep up with targets moving too fast for smooth pursuit and for quick refixation from one target to another. Saccadic eye movements develop before smooth pursuits, occurring as early as 1 week of age. Saccadic eye movements are generated in the frontal lobes and are under contralateral control; that is, right frontal lobe stimulation will result in a saccadic eye movement to the left. Saccadic movements can be voluntarily initiated, but they are not voluntarily controlled, and there is no significant visual feedback to adjust the amount of movement. It is thought that the amplitude of a saccadic movement is preprogrammed based on the degree of retinal eccentricity of the target; this is why saccadic movements are termed ballistic, analogous to the ballistic trajectory of a cannon ball. The neuronal signal that initiates a saccade consists of a burst of high-frequency discharge or pulse to the agonist and inhibition of the antagonist. Because all neurons available are activated for eye movements greater than 30 handbook of pediatric strabismus and amblyopia 5°, the magnitude of a saccade is determined by the duration of the pulse. At the end of a saccade, tonic neuronal firing of the agonist and antagonist muscles occurs to hold the eye position referred to as the step. Vision during a saccadic eye movement is suspended or suppressed. Some have used the term saccadic omission for the process of cortical suppression.1 A tremendous force is required to produce a saccadic eye movement; therefore, the presence of saccadic eye movements indicates “good” muscle function. Only rectus muscles generate saccadic eye movements. When evaluating a patient with limited ductions, look for the presence of a normal saccadic eye movement into the field of limited ductions. If there is a brisk saccade in the direction of the limitation, this indicates good muscle function and suggests the limited movement is caused by restriction, not a muscle paresis. Optokinetic nystagmus (OKN) can be generated by a slowly rotating drum with stripes and used to evaluate smooth pursuit and saccadic eye movements. As the drum rotates toward the patient’s right, there is a smooth pursuit eye movement to the right to follow the stripe. As the end of the stripe passes, there is a fast saccadic movement to the left to refixate on the next stripe. At target velocities less than 30°/s, smooth pursuit keeps pace with the target. At velocities between 30° and 100°/s, smooth pursuit movements progressively lag behind the target. At velocities greater than 100°/s, OKN is not evoked. OKN can be used to evaluate saccadic and smooth pursuit eye movements. Look at the fast phase of OKN to evaluate saccadic movements and the slow phase to evaluate smooth pursuit. ANATOMY OF THE EYE MUSCLES Rectus Muscles The four rectus muscles originate at the orbital apex at the annulus of Zinn and course anteriorly to insert on the anterior aspect of the globe. The “straight” course of the rectus muscles gives rise to the term rectus. The rectus muscle insertions form a progressive spiral termed the spiral of Tillaux around the corneal limbus. The medial rectus muscle is the closest to the limbus (5.5 mm), then the inferior rectus (at 6.5 mm), the lateral rectus (at 7.0 mm), and the superior rectus is the furthest from the limbus (8.0 mm). The muscle–scleral insertion line has chapter 2: anatomy and physiology of eye movements 31 FIGURE 2-5. Diagram of distance of the rectus muscle insertions from the limbus (in millimeters, mm). Note that the medial rectus muscle inserts closest to the limbus and the distances increase, going counterclockwise from the medial rectus toward the superior rectus, which inserts furthest from the limbus. a horseshoe configuration with the rounded apex pointing toward the cornea (Fig. 2-5). One can remember this as the horseshoes are always galloping toward the cornea. The scleral thickness behind the rectus insertions is the thinnest of the eye, being only 0.3 mm thick. Hooking a rectus muscle requires passing the hook several millimeters behind the central muscle insertion to clear the posterior aspect of the horseshoe insertion. The widths of the insertions are all approximately 10 mm, and the distance between insertions or intermuscle spacing is only 6 to 8 mm. Because of the proximity of the rectus muscle insertions, it is easier than you might think to hook the wrong muscle during strabismus surgery. An important number to remember is the rectus muscle length, which is 40 mm for all rectus muscles and is also the length of the orbit. Rectus muscles are innervated from the intraconal side of the muscle belly at the junction of the anterior two-thirds and posterior one-third of the muscle. 32 handbook of pediatric strabismus and amblyopia HORIZONTAL RECTUS MUSCLES The horizontal rectus muscles consist of the medial and lateral rectus muscles. In primary position, each muscle has one action: the medial rectus is an adductor and the lateral rectus is an abductor (Fig. 2-6). When the eye elevates or depresses away from primary position, however, the horizontal rectus muscles take on secondary vertical functions. When the eye is “up,” the horizontal rectus muscles take on a secondary action of supraduction, and when the eye is “down,” the secondary action is infraduction (Fig. 2-7). In addition, if one surgically transposes a horizontal rectus muscle insertion up, the muscle becomes an elevator in addition to the horizontal function. Supraplacing the horizontal rectus insertions during strabismus surgery will induce a hyperdeviation whereas infraplacement induces a hypodeviation. Vertically displacing the medial and lateral rectus muscle insertion is an excellent way to correct small vertical deviations when performing a recession/resection procedure. In Duane’s syndrome, the common finding of upshoot and downshoot is probably caused by the secondary elevator and depressor actions of the cocontracting horizontal rectus FIGURE 2-6. Diagram of simple function of the medial rectus (MR) and lateral rectus (LR) muscle with the eye in primary position. chapter 2: anatomy and physiology of eye movements 33 A B C FIGURE 2-7A–C. Diagram of secondary actions of the medial rectus when the eye rotates up or down. These secondary actions also relate to the lateral rectus. (A) Globe rotated superiorly; now the medial rectus acts as an elevator in addition to its adduction or horizontal function. (B) In the center part of the figure, the medial rectus is a pure adductor. (C) Globe rotated down; in this position, the medial rectus acts as a depressor and an adductor. 34 handbook of pediatric strabismus and amblyopia muscles. Remember, the secondary vertical functions of the horizontal rectus muscles occur only when the eye is rotated vertically off primary position. MEDIAL RECTUS MUSCLE The medial rectus muscle is innervated by the lower division of the oculomotor nerve (third cranial nerve) and, in primary position, is a pure adductor. The medial rectus is uniquely diminutive. It has the shortest arc of scleral contact (6 mm) and the shortest tendon length of the rectus muscles (4 mm). The inferior oblique muscle actually has the shortest tendon (1 mm) of the extraocular muscles, but it is not a rectus muscle. (Be careful; this could be the basis of a trick question.) Of the extraocular muscles, the medial rectus inserts closest to the limbus and is therefore susceptible to insult during anterior segment surgical procedures. Inadvertent removal of the medial rectus muscle is a well-known complication of pterygium removal. The medial rectus is also unique, as it is the only rectus muscle without fascial connections to an adjacent oblique muscle. This lack of oblique muscle connection makes the medial rectus the most difficult to surgically retrieve if lost. Once disinserted, the medial rectus is free to retract completely off the globe into the orbital fat, making retrieval extremely difficult and, in some cases, almost impossible. LATERAL RECTUS MUSCLE The lateral rectus muscle is innervated by the sixth cranial nerve and is a pure abductor. In direct contrast to the medial rectus muscle, the lateral rectus has the longest tendon (8 mm) and the longest arc of scleral contact (10 mm) of the rectus muscles. Be careful, the “longest” cited above refers to only rectus muscles, as the superior oblique tendon has the longest arc of contact and tendon length of all the extraocular muscles. (This could be the source of another trick question.) The long arc of contact occurs because the lateral rectus muscle initially has a divergent course following the lateral wall of the orbit. Then, in the anterior orbit, it turns nasally, wrapping around the globe to its scleral insertion point (see Fig. 2-6). This temporal to nasal wrap around the globe accounts for the long arc of contact. The inferior border of the lateral rectus muscle courses above the inferior oblique insertion, and there are connective tissue bands connecting the lateral rectus muscle to the inferior oblique muscle.13 This is an important anatomic relationship, because a lost lateral rectus chapter 2: anatomy and physiology of eye movements 35 muscle will come to rest at the insertion of the inferior oblique muscle. The surgeon can often find a lost lateral rectus muscle by tracing the inferior oblique muscle back to its insertion. VERTICAL RECTUS MUSCLES EA XIS VISUAL AXIS The superior and inferior rectus muscles are the vertical rectus muscles and are the major elevators and depressors of the eye, respectively. The vertical rectus muscles have secondary and tertiary actions because, in primary position, the muscle axis is 23° temporal to the visual axis of the eye (Figs. 2-2, 2-8A). MU SC L 23° TEMPORAL VI MUSUA SC L & LE A XIS NASAL MU SC LE AX IS A B VISUAL AXIS C FIGURE 2-8A–C. Functions of the vertical rectus muscles with the eye in various positions of gaze. (A) The eye is in primary position with the visual axis 23° nasal to the muscle axis. (B) The eye is abducted 23° from the primary position, and the visual axis is in line with the muscle axis. (C) The eye is abducted more than 23° from the primary position, and the visual axis is now temporal to the muscle axis. 36 handbook of pediatric strabismus and amblyopia Their secondary action is adduction, and it occurs because the vertical rectus muscles pull the front of the eye nasal to the visual axis. Tertiary actions are torsional, consisting of intorsion for the superior rectus muscle and extorsion for the inferior rectus muscle. These secondary and tertiary muscle actions are dependent on eye position. If the eye is abducted 23°, for example, the muscle and visual axes will be in line, and the vertical rectus muscles lose their secondary and tertiary actions, leaving only their vertical actions (Fig. 2-8B). In this position of 23° abduction, the superior rectus acts purely as an elevator, and the inferior rectus purely as a depressor. With further abduction past 23°, the secondary and tertiary actions of the vertical rectus muscles return, but they are different. The secondary action for both vertical rectus muscles becomes abduction, and the tertiary functions reverse, becoming extorsion for the superior rectus and intorsion for the inferior rectus muscle (Fig. 2-8C). SUPERIOR RECTUS MUSCLE The upper division of the oculomotor nerve innervates the superior rectus muscle. It is the major elevator of the eye, and its actions include supraduction (primary), adduction (secondary), and intorsion (tertiary). The superior rectus muscle overlies the superior oblique tendon and has connective tissue connections to the superior oblique tendon below and the levator palpebrae muscle above (Fig. 2-9). This anatomic relationship to the levator palpebrae is important because a large superior rectus recession can cause upper lid retraction and lid fissure widening. On the other hand, a superior rectus resection pulls the upper lid down, resulting in lid fissure narrowing. Lid fissure changes associated with superior rectus surgery can be minimized by surgically removing the fascial connections between the levator and the superior rectus muscles. INFERIOR RECTUS MUSCLE The inferior rectus muscle is innervated by the lower division of the oculomotor nerve and is the principal depressor of the eye. Actions of the inferior rectus muscle include infraduction (primary), adduction (secondary), and extorsion (tertiary). The inferior rectus is sandwiched between the inferior oblique below chapter 2: anatomy and physiology of eye movements 37 FIGURE 2-9. Diagram of the eye and orbit from a top view looking down on the superior rectus (SR) muscle. Note that the superior rectus muscle overlies the superior oblique (SO). T, temporal; N, nasal. and the sclera above (Fig. 2-10). The fascial connection between the inferior rectus muscle, the inferior oblique muscle, and the lower lid retractors (capsulopalpebral fascia) is termed Lockwood’s ligament (Fig. 2-11).17 These fascial connections are responsible for the eyelid changes that often occur after inferior rectus surgery. An inferior rectus recession results in lower lid retraction with lid fissure widening, and a resection causes lid advancement with lid fissure narrowing. If the inferior rectus is inadvertently disinserted or lost during surgery, these connections will hold the inferior rectus to the inferior oblique and keep it from retracting posteriorly. The surgeon who is in search of a lost inferior rectus muscle can usually find it lying between the inferior oblique and sclera. FIGURE 2-10. Diagram of the eye and orbit viewed from below. Note that the inferior oblique (IO) underlies the inferior rectus (IR) muscle. Conjunctiva Tarsus Fornix Tenon's capsule Orbicularis m. Inf. rectus m. ITM CPF Orbital septum CPH Lockwood's lig. Inf. oblique m. 38 chapter 2: anatomy and physiology of eye movements 39 FIGURE 2-12. Diagram of the superior oblique (SO) muscle and tendon. The functional muscle axis extends from the trochlea to the superior oblique insertion. The muscle axis is 54° nasal to the visual axis. OBLIQUE MUSCLES Like the vertical rectus muscles, the oblique muscles have primary, secondary and tertiary actions. In the case of the oblique muscles, this is because the functional muscle axis is approximately 50° nasal to the visual axis, and the insertion extends posterior to the equator of the eye (Figs. 2-12, 2-13). By FIGURE 2-11. Diagram of the relationship between the inferior rectus, inferior oblique, lower lid retractors, and Lockwood’s ligament. The inferior tarsal muscle (ITM) courses from the posterior border of the tarsus toward the inferior oblique muscle. It then passes between the inferior oblique muscle and the inferior rectus muscle to insert at the capsulopalpebral head (CPH). The CPH extends posteriorly to connect the inferior oblique to the inferior rectus muscle. The capsulopalpebral fascia (CPF) is the anterior extension of the CPH and courses from the inferior oblique anteriorly to the tarsus along with the ITM. “Lockwood’s ligament” (Lockwood’s lig.) consists of these fascial attachments that connect the lower lid, inferior rectus, and inferior oblique muscles. 40 handbook of pediatric strabismus and amblyopia FIGURE 2-13. Diagram of the inferior oblique (IO) from a view from below. The inferior oblique muscle axis is 51° nasal to the visual axis. comparing Figures 2-12 and 2-13, one can see that the oblique muscles have an almost identical functional course with both muscle axes at approximately 50°. The posterior muscle–scleral insertion gives the oblique muscles their seemingly paradoxical vertical functions, with the superior oblique being a depressor and the inferior oblique an elevator. The oblique muscles have no anterior ciliary blood supply, and they do not contribute to the anterior segment circulation. Remember that the “oblique muscles always course below the corresponding vertical rectus muscle” (Fig. 2-14). SUPERIOR OBLIQUE MUSCLE The primary action of the superior oblique muscle is intorsion, but it also acts as a depressor (secondary) and an abductor (tertiary). Depression and abduction occur as the back of the eye is pulled up and in toward the trochlea. The superior oblique chapter 2: anatomy and physiology of eye movements 41 muscle originates at the orbital apex just above the annulus of Zinn and gradually becomes tendon at the trochlea (see Fig. 2-12). After passing through the trochlea, the superior oblique tendon reverses course and turns in a posterior temporal direction to pass under the superior rectus muscle to insert on sclera along the temporal border of the superior rectus muscle (Fig. 2-14). Even though the anatomic origin is at the apex of the orbit, the functional origin of the superior oblique is at the trochlea. This tendon is the longest tendon of the extraocular muscles, 26 mm in length. The tendon insertion fans out broadly under the superior rectus muscle, extending from the temporal pole of the superior rectus muscle to 6.5 mm from the optic nerve.13 Fascial attachments connect the superior oblique tendon to the superior rectus muscle above and to the sclera below.13 The tendon insertion can be functionally divided into two basic parts: the anterior one-third and the posterior two-thirds. Posterior fibers are responsible for depression and abduction whereas tendon fibers anterior to the equator are devoted to intorsion. This distinction between anterior and posterior superior oblique tendon fibers is important because one can FIGURE 2-14. Diagram of posterior anatomy of the eye and muscles. Note the proximity of the inferior oblique to the macula and vortex veins (vv). The posterior aspect of the superior oblique insertion is in proximity to the superior temporal vortex vein and is approximately 6 to 8 mm from the optic nerve. 42 handbook of pediatric strabismus and amblyopia manipulate these functions surgically to correct specific motility disorders. The Harada–Ito procedure, for example, involves tightening the anterior fibers of the superior oblique tendon. Because the anterior tendon fibers intort the eye, the Harada–Ito procedure can be used to treat extorsion associated with superior oblique palsy. The trochlear nerve innervates the superior oblique muscle at its midpoint from outside the muscle cone. The superior oblique muscle is, in fact, the only eye muscle innervated on the outer surface of the muscle belly. This unique innervation explains why a retrobulbar anesthetic block results in akinesia of all the eye muscles except the superior oblique muscle. TROCHLEA The trochlea (Latin for pulley) is a cartilaginous U-shaped structure attached to the periosteum that overlies the trochlear fossa of the frontal bone in the superior nasal quadrant of the orbit. It has been taught that the superior oblique tendon moves through the trochlea much like a rope through a pulley. Anatomic studies have shown, however, that tendon movement is not that simple. Within the trochlea is a connective tissue capsule with connective tissue bands that unite the superior oblique tendon to the surrounding trochlea (Fig. 2-15).46 Some of the tendon slackening distal to the trochlea may come from a telescoping elongation of the central tendon (Fig. 2-16).19 This telescoping elongation of the tendon appears to be caused by movement of the central tendon fibers that have scant interfiber connections. Thus, the mechanism for tendon movement is complex, with at least two mechanisms: (1) tendon movement through the trochlea (pulley and a rope) and (2) tendon elongation (telescoping). INFERIOR OBLIQUE MUSCLE It is the principal extortor of the eye; however, other actions include elevation (secondary) and abduction (tertiary). The inferior oblique muscle originates at the lacrimal fossa located at the anterior aspect of the inferior nasal quadrant of the orbit (see Fig. 2-13). Starting at the lacrimal fossa, the inferior oblique muscle courses posteriorly and temporally underneath the inferior rectus muscle to its scleral insertion, which is adjacent to the inferior border of the lateral rectus muscle (see Fig. 2-14). The inferior oblique muscle has fascial connections to the lower chapter 2: anatomy and physiology of eye movements 43 A B FIGURE 2-15A–B. Histology of the trochlea. (A) Low-magnification cross section of midtrochlea. H&E stain. Note horseshoe shape of cartilaginous tissue and the fibrous connective tissue ring that surrounds the superior oblique muscle. At this cross section, the superior oblique is two-thirds muscle and one-third tendon. (B) High-magnification cross section of superior oblique muscle in midtrochlea shows fibrous connective tissue ring connecting to muscle via fine fascial septae. 44 handbook of pediatric strabismus and amblyopia C D FIGURE 2-15C–D. (C) Low-magnification cross section of superior oblique tendon exiting the trochlea. Note small area of cartilage and larger ring of fibrous connective tissue that surrounds the superior oblique tendon as the tendon capsule. At this section, the superior oblique is onethird muscle and two-thirds tendon. (D) High magnification of the superior oblique tendon exiting the trochlea. Note the superior oblique tendon capsule consists of circumferential onionskin layers of fibrous connective tissue. The tendon capsule is attached to the superior oblique tendon capsule by circumferential connective tissue fibers. (From Wright et al., Ref. 46, with permission.) chapter 2: anatomy and physiology of eye movements 45 FIGURE 2-16. Diagram of anatomy of the trochlea. Note the central fibers of the tendon expand and retract more than the peripheral tendon fibers. (From Ref. 19, with permission.) border of the lateral rectus muscle and to the overlying inferior rectus muscle via Lockwood’s ligament (see Fig. 2-11). When the inferior oblique muscle contracts, it pulls the back of the eye down and in toward the insertion at the lacrimal fossa. This action produces elevation, abduction, and extorsion (Fig. 2-14). Important structures near the inferior oblique insertion include the macula and inferior temporal vortex vein (Fig. 2-14). The inferior oblique muscle has only 1 mm of tendon at its insertion. The inferior oblique muscle is innervated by the inferior branch of the third nerve at a point just lateral to the inferior rectus muscle. Innervation occurs at the posterior aspect of the inferior oblique muscle belly, and the nerve is accompanied by blood vessels forming a neurovascular bundle. This neurovascular bundle is surrounded by an inelastic capsule of collagen tissue that protects the inferior oblique nerve from damage caused by stretching.39 The neurovascular bundle with its insertion into the posterior aspect of the muscle is an important structure in regard to inferior oblique surgery. Anterior transposition of the inferior oblique muscle is an effective surgical 46 handbook of pediatric strabismus and amblyopia procedure used to treat inferior oblique muscle overaction; however, the complication of postoperative limited elevation has been reported.5,25,26,47 This complication is caused by anteriorizing the posterior muscle fibers at, or anterior to, the inferior rectus muscle insertion, because this tightens the inelastic neurovascular bundle.38 The tight neurovascular bundle acts as the functional origin of the inferior oblique muscle and changes the action of the inferior oblique muscle from an elevator to a depressor (Fig. 2-17A).16 This author has coined the term J-deformity for this acute bend of the anteriorized inferior oblique.47 When the patient looks up, the inferior oblique muscle contracts along with the superior rectus muscle, but the anteri- Inferior oblique muscle Neurofibrovascular bundle Maxillary bone Inferior rectus muscle FIGURE 2-17A,B. (A) Diagram of inferior oblique muscle anteriorization with “J-deformity.” The J-deformity is caused by anterior placement of the posterior inferior oblique muscle fibers to the level of the inferior rectus muscle insertion. Because the neurovascular bundle of the inferior oblique muscle inserts in the posterior muscle belly, anteriorization of the posterior muscle fibers produces a tight neurovascular bundle; this causes limited elevation of the eye as active contraction of the anteriorized inferior oblique muscle pulls against the tight neurovascular bundle.16 chapter 2: anatomy and physiology of eye movements 47 Vortex vein Inferior oblique muscle Inferior rectus muscle FIGURE 2-17A,B. (B) Diagram of the “graded anteriorization” technique described by Guemes and Wright that is effective in reducing inferior oblique overaction but avoids the postoperative complication of limited elevation.16 The new inferior oblique muscle insertion is shown being placed 1 mm behind the inferior rectus muscle insertion, and the posterior muscle fibers are placed an additional 4 to 5 mm further posterior, and parallel to the inferior rectus muscle axis. Note that the posterior placement of the posterior muscle fibers avoids the J-deformity. By keeping the posterior muscle fibers posterior to the anterior fibers and avoiding the J-deformity, the neurovascular bundle remains loose, preventing postoperative limitation of elevation. orized inferior oblique muscle now depresses the eye and limits elevation; this is an active leash caused by inferior oblique contraction, and forced ductions on patients with this complication of limited elevation often show only slight restriction to supraduction. The complication of limited elevation can be avoided while maintaining excellent results by anterior transposition of the anterior muscle fibers at, or a millimeter or two behind, the inferior rectus insertion. Be sure to keep the posterior fibers back, behind the anterior fibers. Placing the posterior muscle fibers several millimeters posterior to the inferior rectus insertion and in line with the inferior rectus muscle prevents the J-deformity (Fig. 2-17B).16,47 48 handbook of pediatric strabismus and amblyopia EXTRAOCULAR MUSCLE HISTOLOGY As are other skeletal muscles, extraocular muscles are made up of striated fibers that, on electron microscopy, show the typical banding pattern of sarcomeres with overlapping threads of actin and myosin. Also resembling other muscles, the strength of an extraocular muscle contraction is dependent on the number of motor units activated (recruitment) and the frequency of muscle fiber stimulation. Extraocular muscles, however, do show some interesting anatomic and physiological differences from other skeletal muscles. The fibers are variable in size, are considerably smaller, and contract more than 10 times faster than other skeletal muscle. Extraocular muscle fibers are innervated at a high nerve fiber to muscle fiber ratio (almost 1:1), whereas other skeletal muscle can have up to 100 muscle fibers for every nerve fiber. This rich innervation, teamed with a fast muscle reaction time, contributes to the precision, accuracy, and control of eye movements. Another distinction of extraocular muscles is the presence of two distinct muscle fiber types: fast muscle fibers and slow muscle fibers. The fast, or twitch, fibers are single innervated fibers (SIF), innervated by a large motor neuron with “en plaque” neuromuscular junctions and are typical of mammalian skeletal muscle. The SIF can be classified into three types: red, intermediate, and white. Red SIF have the highest density of mitochondria and are the most fatigue resistant, while the white SIF have fewer mitochondria and are less resistant to fatigue. Intermediate and white fibers provide the high transient force needed for the extremely fast saccadic eye movements. Slow, or tonic muscle fibers, are multiple innervated fibers (MIF) innervated by small-diameter motor nerves with “en grappe” neuromuscular endings characteristic of avian and amphibian muscles. MIF are thought to participate in smooth pursuit movements and static muscle tone to hold and maintain eye position, and SIF probably also play a supportive role in tonic control of eye position and pursuit eye movements. The exact functions of the variety of specific muscle fiber types are unknown, and it is likely that various fibers have overlapping functions.28 Within extraocular muscle tissue are neuromuscular spindles that are concentrated at the muscle–tendon junction. Neuromuscular spindles are thought to be sensory organs providing information on muscle tone to the brain.9 The exact role chapter 2: anatomy and physiology of eye movements 49 of the muscle spindles is unknown, but they may provide proprioceptive feedback to motor centers in the brain regarding muscle tone and eye position. Muscle spindles may explain why many adult patients experience transient spatial disorientation after strabismus surgery on the dominant eye. ARCHITECTURE OF THE EXTRAOCULAR MUSCLES AND PULLEYS Extraocular muscles have two distinct muscle layers seen on transverse sections (cross section). There is a peripheral layer closest to the orbital wall called the orbital layer (OL) and an inner layer closest to the eye globe called the global layer (GL).33,37 OL muscle fibers contain small-diameter fibers with many mitochondria and abundant vessels, staining dark red by Masson’s trichrome. The GL, in contrast, contains larger fibers with variable numbers of mitochondria and fewer vessels; it stains bright red by Masson’s trichrome. Approximately 90% of GL muscle fibers are fast-twitch SIF, with one-third of the SIF being fatigue-resistant red SIF; 80% of OL muscle fibers are twitch-generating SIF and 20% are MIF.33 In humans, OL muscle fibers do not appear to run the entire course of the muscle and do not insert in sclera, as there is a gradual decline in the OL in the anterior aspect of the muscle.11,28 Elastic fibers connect the OL to a fibromuscular pulley sleeve that surrounds each extraocular muscle close to the muscle insertion (see Muscle Pulleys, following) (Fig. 2-18).11 There are also muscle-to-muscle-fiber junctions (myomyous junctions) within the OL. GL fibers, on the other hand, are continuous from their origin in the orbital apex to their insertion by tendon into sclera.28 Most GL fibers act in saccadic eye movements and function only in the field of action of the muscle whereas OL fibers are active throughout the oculomotor range, providing continuous muscle tone to the pulley system.7 Collins hypothesized that OL muscle fibers might have a role in maintaining fixation whereas GL muscle fibers participate in dynamic eye movements.7 An alternative hypothesis proposed by Demer is that OL muscle fibers actively control pulley position, thereby influencing the rotational force vectors during eye movements.11,28 A FIGURE 2-18A–C. Masson’s trichrome stain of 10-m-thick transverse section of medial rectus at the level of the pulley ring of a 17-month-old human. (A) Low power shows the overall architecture of the pulley (P) that surrounds the medial rectus muscle. Fibers in the orbital layer (OL) (arrowheads) insert in the pulley, shown at high power in (B). The OL muscle layer takes the form of a C-shape and is on the left, delineated by the large arrows; the global layer (GL) fibers are to the right. OL on the left is shown on the bottom. 50 chapter 2: anatomy and physiology of eye movements 51 B C FIGURE 2-18A–C. (B) High-power magnification shows the insertion of the OL into the pulley (taken from the upper left box on A). (C) Highpower magnification of the GL and pulley relationship. The GL does not insert into the surrounding pulley (taken from the middle right box on A).11,28 52 handbook of pediatric strabismus and amblyopia EXTRAOCULAR MUSCLE FASCIA A smooth white connective tissue, Tenon’s capsule, underlies the conjunctiva and envelops the globe and extraocular muscles. This delicate membrane partitions the orbital contents, isolating the globe and extraocular muscles from the surrounding orbital fat. Another fascial structure interconnected with Tenon’s capsule is the muscle sleeve or extraocular muscle pulley, which suspends the extraocular muscles. Muscle Pulley (Muscle Sleeve) Each of the rectus muscles passes through a pulley system consisting of a sleeve or ring of collagen, elastic, and smooth muscle fibers. Previously, this structure was termed muscle sleeve. The medial rectus muscle pulley has the most fibroelastic tissue and smooth muscle. Muscle pulleys connect to the orbital layer (OL) of the rectus muscle, to the orbital wall, to adjacent extraocular muscles, and to Tenon’s capsule.10 The pulley or sleeve extends for approximately 10 mm from the equator of the globe anteriorly to approximately 6 mm from the muscle insertion. During strabismus surgery, one can see these bands as they connect the surrounding muscle sleeve or pulley to the OL of the rectus muscle. Similar to the trochlea and superior oblique tendon, the pulleys guide the rectus muscles to their insertion point. In contrast to the superior oblique muscle, which changes direction after passing through the trochlea, rectus muscle pulleys keep the muscle in line with their anatomic origin. Demer has suggested that in secondary gaze positions the extraocular muscle path is “discretely inflected by the pulley.”6 Demer et al. also hypothesized that OL muscle fibers insert into the pulley system and actively influence pulley position and the mechanics of ocular rotation.11,28 Tenon’s Capsule Tenon’s capsule is a collagen-elastic tissue that is a continuous membrane surrounding the eye and extraocular muscles.22 This membrane separates surrounding orbital fat from the globe and extraocular muscles. The elastic nature of Tenon’s capsule allows free rotation of the globe and unrestricted muscle relaxation and contraction. For clinical and surgical purposes, it is useful to subdivide it into the following categories: chapter 2: anatomy and physiology of eye movements 53 1. Intermuscular septum 2. Anterior Tenon’s capsule 3. Posterior Tenon’s capsule 4. Check ligaments 5. Muscle sleeve (see Pulley System, earlier) INTERMUSCULAR SEPTUM This thin tissue lies sandwiched between the conjunctiva and sclera, spanning between the rectus muscles (Fig. 2-19).30,40 During strabismus surgery, intermuscular septum can be identified as the white membrane on each side of the rectus muscles. When elevated with muscle hooks, the intermuscular septum takes on the appearance of the wings of a manta ray (Fig. 2-20).45 The intermuscular septum can be safely incised during strabismus surgery, as it is not a barrier to orbital fat. ANTERIOR TENON’S CAPSULE This tissue is the subconjunctival membrane anterior to the muscle insertions. It proceeds forward with the intermuscular septum and fuses with the conjunctiva at 2 to 3 mm posterior to the corneal limbus (Figs. 2-18, 2-20). When suturing a muscle during strabismus surgery, it is important to dissect anterior Tenon’s capsule off the tendon insertion to avoid the complica- Reflected conjunctiva SR IMS IMS MR LR Anterior Tenon's Capsule FIGURE 2-19. Anterior ocular fascia. Intermuscular septum (IMS) is the connective tissue that spans between the rectus muscles underneath the conjunctiva. Anterior Tenon’s is that tissue anterior to the rectus muscle insertions; it fuses with the conjunctiva 3 mm posterior to the limbus. 54 handbook of pediatric strabismus and amblyopia A B FIGURE 2-20A,B. (A) Lateral rectus muscle with intermuscular septum and check ligaments. Check ligaments overlie the rectus muscle and connect the muscle to the overlying conjunctiva. Intermuscular septum is seen on either side of the lateral rectus muscle, spanning between the superior and inferior rectus muscles. (B) Photograph shows the Jameson hook under the lateral rectus muscle and Desmarres retractor pulling the conjunctiva posteriorly. (Figure published with permission of J.B. Lippincott Co. from Wright KW. Color Atlas of Ophthalmic Surgery: Strabismus. Philadelphia: Lippincott, 1991.) chapter 2: anatomy and physiology of eye movements 55 Anterior Tenon's capsule Medial rectus Anterior ciliary muscle artery FIGURE 2-21. Anterior Tenon’s capsule is the white tissue retracted anteriorly with a small Steven’s hook (bottom left hook). During strabismus surgery, it is important to remove the anterior Tenon’s capsule to visualize the muscle tendon for suturing. Note the anterior ciliary vessels on the tendon insertion. tion of a slipped muscle (Fig. 2-21). If anterior Tenon’s capsule is left on the tendon, the surgeon may inadvertently suture and secure anterior Tenon’s capsule, missing all or part of the tendon. The unsuspecting surgeon then disinserts the unsutured tendon and allows the muscle to slip posteriorly while anterior Tenon’s capsule is placed at the intended recession site.31 A slipped muscle is a frequent cause of unexpected overcorrection after recession procedures, as it often goes unrecognized at the time of surgery. Remember that some slipped muscles involve only part of the muscle and can present as a mild overcorrection with relatively good muscle function.48 POSTERIOR TENON’S CAPSULE This tissue lines the posterior globe and functions to separate orbital fat from the sclera (Fig. 2-22). Just anterior to the equator of the eye, the four rectus muscles penetrate Tenon’s capsule and become surrounded by intra- and extraconal orbital fat. At this juncture, Tenon’s capsule unites with the capsule of the rectus muscle to form a muscle pulley or muscle sleeve (see Muscle Pulley, earlier). The muscle sleeve is an important surgical 56 handbook of pediatric strabismus and amblyopia Posterior Tenon's capsule Extraconal fat Anterior Tenon's capsule Muscle sleeve (pulley) Conjunctiva Fused anterior Tenon's and conjunctiva Intraconal fat Medial rectus muscle FIGURE 2-22. Drawing of a rectus muscle showing fascial relationships. Note that the muscle penetrates posterior Tenon’s capsule; the capsule at this point forms a muscle sleeve or muscle pulley. Intraconal and extraconal fat are isolated from the globe by Tenon’s capsule. landmark when looking for a slipped or lost rectus muscle. A lost muscle is a rectus muscle that has become completely detached from the globe because of trauma or a surgical mistake.32,48 Once lost, the muscle will slip posteriorly within the muscle sleeve to be surrounded by intra- and extraorbital fat. To find a lost muscle, first find the muscle sleeve located between the intraand extraconal fat; then, carefully follow the sleeve to retrieve the muscle. When looking for a lost medial rectus muscle, avoid the tendency to follow the sclera posteriorly, as this leads to the optic nerve. An important complication of attempted retrieval of a lost medial rectus muscle is inadvertent transection of the optic nerve that is enshrouded in postoperative scar tissue. Together, posterior Tenon’s capsule, anterior Tenon’s capsule, and the muscle sleeve are very important structures as they are the barrier that keeps orbital fat from the globe and extraocular muscles. If posterior Tenon’s capsule or muscle sleeve is traumatically or surgically violated, fat adherence can occur because orbital fat prolapses through the torn Tenon’s capsule and scars to the sclera or an extraocular muscle (Fig. 2-23). The scarring of orbital fat produces a restrictive scar, which extends from the periosteum to the eyeball. As the scar chapter 2: anatomy and physiology of eye movements 57 contracts over weeks to several months, the scar pulls the eye, producing a restrictive strabismus associated with limitation of eye movements. Fat adherence can occur as a complication of almost any extraocular surgery (e.g., strabismus surgery, retina surgery) or periocular trauma.31,49 Extreme care must be taken when operating in the area of orbital fat, which starts 10 mm posterior to the limbus. Once fat adherence occurs, it is almost impossible to correct. Surgically induced fat adherence can usually be avoided if the surgeon carefully dissects close to muscle belly or sclera, thus preserving the integrity of the overlying posterior Tenon’s capsule and muscle sleeve. CHECK LIGAMENTS These are fine falciform webs that overlie the rectus muscles and join the muscle capsule with overlying bulbar conjunctiva A B FIGURE 2-23A,B. Diagram modified after Parks and published in Ophthalmology by Wright (1986)49 shows the pathophysiology of the fat adherence syndrome. (A) Normal anatomy with orbital bone, periorbita, extraconal fat, muscle, and intermuscular septum. Note that the fat is isolated from muscle and sclera by intact Tenon’s capsule and intermuscular septum. (B) Violation of Tenon’s capsule with fat adherence to the globe and muscle (to right). 58 handbook of pediatric strabismus and amblyopia at the muscle tendon (see Fig. 2-20). More posteriorly, check ligaments are probably the bands that connect the OL muscle fibers to the surrounding muscle sleeve (muscle pulley). In the case of the superior and inferior rectus muscles, check ligaments also connect to the levator muscle and lower lid retractors, respectively. A recession or resection of vertical rectus muscles requires removal of these ligaments to avoid lid fissure changes after surgery. VASCULAR SUPPLY TO THE ANTERIOR SEGMENT The anterior segment and iris are supplied by the anterior ciliary arteries, conjunctival vessel, and the long posterior ciliary arteries (Fig. 2-24). Approximately 50% of the anterior segment circulation comes from the long posterior ciliary arteries and FIGURE 2-24. Diagram of circulation of the anterior segment with the rectus muscle supplying the anterior ciliary arteries (aa); the deep long posterior arteries are also shown. (Figure published with permission of J.B. Lippincott Co. from Wright KW. Color Atlas of Ophthalmic Surgery: Strabismus. Philadelphia: Lippincott, 1991.47) chapter 2: anatomy and physiology of eye movements 44 59 50% from the anterior ciliary arteries. The conjunctival vessels also contribute to anterior segment circulation.14 Anterior ciliary arteries and the conjunctival vessels merge at the limbus to form the episcleral limbal plexus.27 These vessels in turn connect with the major arterial circle of the iris, which is also fed by the two long posterior ciliary arteries. The superior rectus, inferior rectus, and medial rectus muscles have at least two anterior ciliary arteries and are major contributors to the anterior segment circulation.18 The lateral rectus has a single anterior ciliary artery and, of the four recti muscles, the lateral rectus probably provides the least in the way of anterior segment circulation.20,41 The oblique muscles do not have anterior ciliary arteries, and they do not contribute to the anterior segment circulation. Iris angiograms can be used to assess anterior segment circulation in blue-eyed patients. Removal of a vertical rectus muscle will cause hypoperfusion in that area that relates to the vascular input.18 It is interesting that this hypoperfusion lasts only 1 to 2 months because its collateral circulation and vasodilatation will replenish the hypoperfused area.45 Additionally, infants and children do not typically show hypoperfusion even when multiple rectus muscles are removed. Removal of a rectus muscle during strabismus surgery will permanently interfere with vascular supply of the anterior ciliary arteries unless the surgery is performed specifically to maintain anterior segment circulation. Surgeries have been devised that attempt to maintain anterior segment circulation despite manipulations of the muscle position.24,45 Iris angiograms can be used to document anterior segment blood flow from the anterior ciliary arteries in nonhuman primates. A muscle-to-sclera plication developed by this author (Wright plication) is designed to tighten a rectus muscle but spare the anterior ciliary arteries. Instead of resecting the muscle, as is done in the standard muscle tightening procedure, the Wright plication folds the muscle, suturing muscle to sclera without disrupting the anterior ciliary vessels. Figure 2-25 shows an iris angiogram after inferior rectus muscle plication and surgical removal of the other three rectus muscles in a nonhuman primate. The iris angiogram demonstrates intact perfusion from the inferior rectus muscle and hypoperfusion superiorly because the arteries of the other three rectus muscles had been sacrificed on surgical removal. Anterior segment ischemia can be a consequence of strabismus surgery, most often after a three- or four-muscle 60 handbook of pediatric strabismus and amblyopia FIGURE 2-25. Monkey fluorescein iris angiogram, early phase after Wright plication of the inferior rectus muscle and removal of the other three rectus muscles. Note the hypoperfusion superiorly (black area of iris) as the medial, lateral, and superior rectus muscles have been removed. The perfusion from the inferior rectus remains intact after the Wright plication because fluorescence is seen inferiorly (white vessels on iris).46 transposition procedure.35,42 This is a rare occurrence, as collateral circulation from the long posterior ciliary arteries can usually maintain adequate perfusion to the anterior segment even when three or four rectus muscles have been removed.36 Factors that predispose to anterior segment ischemia include arteriosclerosis, hyperviscosity of the blood, and scleral encircling elements such as 360° retinal buckles posteriorly, all of which can compromise the long posterior ciliary arteries. Older patients have a higher likelihood for developing anterior segment ischemia, whereas infants and children are generally protected from this condition.15 Anterior segment ischemia has even been reported after removing as few as two rectus muscles in high-risk patients.12,15 It is important to remember, however, that disruption of anterior ciliary arteries associated with strabismus surgery is permanent, and anterior segment ischemia can occur years or decades later, as the collateral circulation diminishes with age.34 chapter 2: anatomy and physiology of eye movements 61 PHYSIOLOGY OF OCULAR ROTATIONS Donder’s and Listing’s Laws Ocular movements are a result of contraction and relaxation of multiple muscle groups that act to rotate the eye around a fixed center of rotation. There are three axes that pass through the center of rotation, termed the axes of Fick (Fig. 2-26). The axes of Fick include the Z axis (vertical orientation) for horizontal rotation, the X axis (horizontal orientation) for vertical rotation, and the Y axis (oriented with the visual axis) for torsional rotation. Listing’s plane is a vertical plane that includes the X, Z, and oblique axes that pass through the center of the eye (Fig. 2-26). Listing’s law states that virtually all positions of gaze can be achieved by rotations around axes that lie on Listing’s plane. Donder’s law is related to Listing’s law and states that there is a specific orientation of the retina and cornea for every position of gaze. This corneal orientation is specific for each position of gaze regardless of the path the eye took to achieve that position of gaze. Figure 2-27 demonstrates Listing’s and Donder’s laws, showing the specific corneal orientations for ocular rotations around various axes on Listing’s plane. Note that when rotations B A C FIGURE 2-26A–C. The three axes of Fick allow horizontal rotation. (A) Vertical axis (Z axis): horizontal rotations. (B) Horizontal axis (X axis): vertical rotations. (C) Visual axis (Y axis): torsional rotations. 62 handbook of pediatric strabismus and amblyopia FIGURE 2-27. Listing’s plane is shown in the center diagram, which includes the Z and X axes of Fick. Diagram shows that the eye can reach all positions of gaze by rotations around axes that are on Listing’s plane. In the center diagram, the O axes represent oblique axes that are on Listing’s plane and are oriented between the Z and X axes of Fick. Note that the oblique axes of rotation seen on the four corners of the diagram allow the eye to rotate obliquely, up and in, up and out, down and in, and down and out. Also, observe the pseudotorsion of the cornea when the eye rotates around the oblique axis. are directly around the X axis (pure vertical movement) or directly around the Z axis (pure horizontal movement) there is no associated torsional rotation of the cornea. In contrast, oblique ocular rotations cause a torsional shift in the corneal orientation relative to the planar coordinates of Listing’s plane. This torsional shift relative to Listing’s plane is not due to true rotation around the Y axis and is therefore referred to as pseudotorsion. Active, or true, torsional rotations around the Y axis (cycloduction) are created by contraction of vertical and oblique muscles. True torsional movements normally occur to keep the eyes aligned during head tilting23 or occur pathologically when a vertical or an oblique muscle over- or underacts.21 chapter 2: anatomy and physiology of eye movements 63 TABLE 2-2. Agonist–Antagonist Muscle Pairs. Medial rectus—Lateral rectus Superior rectus—Inferior rectus Superior oblique—Inferior oblique Sherrington’s Law: Agonist and Antagonist Muscles As described in this chapter previously, ductions are monocular rotations and are clinically examined with one eye occluded to force fixation to the eye being tested. Table 2-2 lists agonist– antagonist pairs for the primary function of the muscles. This relationship between agonist (contracting muscle) and antagonist (relaxing muscle) muscles is referred to as Sherrington’s law of reciprocal innervation. Sherrington’s law can be demonstrated by using electromyography (EMG). The EMG measures electrical potential changes within a muscle as the muscle fibers contract and indicates the degree of overall neuromuscular activity. The EMG is performed by placing a needle electrode in the muscle (extracellularly) and then recording the amplified electrical activity from the muscle. Figure 2-28 shows results of EMG for agonist and antagonist muscles that demonstrates Sherrington’s law. The needle electrode is placed in the medial and lateral rectus muscles. At the beginning of the EMG tracing, there is lowamplitude tonic activity that maintains the eye position in FIGURE 2-28. Sherrington’s Law: Electromyographic (EMG) tracing from the lateral rectus muscle (LR) and medial rectus muscle (MR). Note that when the eye adducts, the medial rectus muscle increases EMG activity as the muscle contracts. EMG activity from the lateral rectus muscle diminishes as the antagonist lateral relaxes. 64 handbook of pediatric strabismus and amblyopia primary position. As the eye is adducted, the medial rectus contracts, resulting in increasing EMG activity, while the lateral rectus muscle simultaneously relaxes and EMG activity is inhibited. At the end of the tracing, both muscles show tonic activity to maintain eye position. In patients with motor neuron misdirection syndromes such as Duane’s retraction syndrome, Sherrington’s law is violated. In Duane’s syndrome, the lateral rectus muscle is innervated by a branch of the third nerve that also supplies the medial rectus muscle. When the patient adducts the eye, instead of the medial rectus contracting and the lateral rectus relaxing, both the medial and lateral rectus muscles contract simultaneously. It should be remembered that Sherrington’s law of reciprocal innervation refers strictly to monocular eye movements, as does the term ductions. A trick to remember this, is the S in Sherrington stands for Single eye. Synergist The term synergist is used for muscles of the same eye that act to move the eye in the same direction. In other words, synergist muscles have common actions. For example, the superior oblique and the inferior rectus muscles both act as depressors; therefore, they are synergists for infraduction. These muscles are not, however, synergists for horizontal or torsional rotations, as the inferior rectus muscle is an adductor and extortor whereas the superior oblique muscle is an abductor and intortor. Table 2-3 lists synergist muscles for various duction movements. Note that synergist muscles relate to monocular rotations, not to be confused with yoke muscles involved with binocular eye movements (see Hering’s Law of Yoke Muscles, below). Like the S trick in Sherrington’s law, remember the S in Synergist stands for Single eye. TABLE 2-3. Synergist Muscles. Duction Primary mover Secondary mover Supraduction Infraduction Adduction Abduction Extorsion Intorsion Superior rectus Inferior rectus Medial rectus Lateral rectus Inferior oblique Superior oblique Inferior oblique Superior oblique Superior rectus/inferior rectus Superior oblique/inferior oblique Inferior rectus Superior rectus chapter 2: anatomy and physiology of eye movements 65 Oculomotor Reflexes Two important oculomotor reflexes are the vestibulo-ocular reflex (VOR) and optokinetic nystagmus (OKN). The vestibuloocular reflex functions to keep the eyes steady when the head moves. Vestibular stimulation, induced by turning the head, results in a compensatory movement of the eyes to maintain the position of gaze. If the head is rapidly turned to the left, the eyes move to the right with the same velocity. A similar reflex, the orthostatic reflex, is responsible for keeping the eyes torsionally aligned when the head is tilted. This reflex is the basis of the Bielschowsky head tilt test for vertical muscle palsies. Optokinetic nystagmus is a visually mediated reflex consisting of smooth pursuit alternating with saccadic refixation as a series of objects cross the visual field. The eyes follow a moving object with smooth pursuit, then use a saccadic movement in the opposite direction to refixate on the next approaching target. The stimulus most commonly used to produce OKN is a pattern of black and white stripes presented on a rotating drum or moving tape. The best OKN stimulus fills the visual field so there are no stationary objects for the subject to fixate. Hering’s Law of Yoke Muscles Normally, our two eyes move together in the same direction; this is termed a version movement. Coordinated binocular eye movements require symmetrical innervation of each eye. For example, when one looks to the left, the left lateral rectus and right medial rectus muscles simultaneously contract as the left medial and right lateral rectus muscles relax (Fig. 2-29). The paired agonist muscles from each eye are referred to as yoke muscles. In Figure 2-29, the left lateral and right medial rectus muscles are yoke agonist muscles whereas the left medial and right lateral are yoke antagonists. Hering’s law states that yoke muscles receive equal innervation. Remember, Hering’s law relates to yoke muscles and binocular eye movements (versions), whereas Sherrington’s law explains agonist–antagonist relationships and monocular eye movements (ductions). Figure 2-30 shows the yoke agonist muscles responsible for various fields of gaze. In most situations, the term yoke muscles refers to yoke agonist muscles. FIGURE 2-29. Hering’s Law: Diagram of version movements to the left. As the left lateral rectus (LR) contracts (), the contralateral medial rectus (MR) simultaneously contracts (). Also note that the left medial rectus relaxes () and the right lateral rectus also relaxes (). FIGURE 2-30. Yoke muscles are shown for specific field of gaze. Top: gaze up and to the side with yoke muscles being the superior rectus (SR) and inferior oblique (IO) muscles. Middle: straight sidegaze with the yoke muscles being lateral rectus (LR) and medial rectus (MR). Bottom: gaze down and to the side with yoke muscles being the inferior rectus (IR) and superior oblique (SO). 66 chapter 2: anatomy and physiology of eye movements 67 Versions Versions can be classified as follows: dextroversion for rightgaze, levoversion for leftgaze, supraversion for upgaze, and infraversion for downgaze. In contrast to ductions, versions are performed with both eyes open and compare how well the eyes move together in synchrony. Versions will identify a subtle restriction or paresis and muscle overaction that results in asymmetrical eye movements. References 1. Atkinson J. Development of optokinetic nystagmus in the human infant and monkey infant: an analogue to the development in kitten. In: Freeman RD (ed) Developmental neurobiology of vision. New York: Plenum Press, 1979. 2. Bartini C, Horcholle-Bossavit G. Extraocular muscle afferents and visual input interactions in the superior colliculus of the cat. Prog Brain Res 1979;50:335. 3. Beisner DH. Reduction of ocular torque by medial rectus recession. Arch Ophthalmol 1971;85:13. 4. Bloom JN, Graviss ER, Mardelli PG. A magnetic resonance imaging study of the upshoot-downshoot phenomenon of Duane’s retraction syndrome. Am J Ophthalmol 1991;111:548–554. 5. Bremer DL, Rogers GL, Quick LD. Primary-position hypotropia after anterior transposition of the inferior oblique. Arch Ophthalmol 1986;104:229–232. 6. Clark RA, Miller JM, Demer JL. Three-dimensional location of human rectus pulleys by path inflections in secondary gaze positions. Investig Ophthalmol Vis Sci 2000;41:3787–3797. 7. Collins CC. The human oculomotor control system. In: Lennerstrand G, Bach–y-Rita P (eds) Basic mechanism of ocular motility and their clinical implications. New York: Pergamon, 1975:145–180 8. Cynader M, Berman N, Hein A. Recovery of function in cat visual cortex following prolonged deprivation. Exp Brain Res 1975;25:139– 156. 9. Daniel P. Spiral nerve endings in the extrinsic eye muscles of man. J Anat 1946;80:189. 10. Demer JL, Poulkens V, Miller JM, Micevych P. Innervation of extraocular pulley smooth muscle in monkeys and humans. Investig Ophthalmol Vis Sci 1997;38:1774–1785. 11. Demer JL, Oh SY, Poulkens V. Evidence for an active control of rectus extraocular muscle pulleys. Investig Ophthalmol Vis Sci 2000;41: 1280–1290. 12. Fells P, March RJ. Anterior segment ischemia following surgery on two rectus muscles. In: Reinecke RD (ed) Strabismus: proceedings of 68 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. handbook of pediatric strabismus and amblyopia the third meeting of the International Strabismological Association, May 10–12, 1978, Kyoto, Japan. New York: Grune & Stratton, 1978: 375–380. Fink WH. Surgery of the oblique muscles of the eye. St. Louis: Mosby, 1951:92–95. Fishman PH, Repka MX, et al. A primate model of anterior segment ischemia after strabismus surgery. Ophthalmology 1990;97(4):456–461. France TD, Simon JW. Anterior segment ischemia syndrome following muscle surgery. The AAPO&S experience. J Pediatr Ophthalmol Strabismus 1986;23:87–91. Guemes A, Wright KW. Effect of graded anterior transposition of the inferior oblique muscle on versions and vertical deviation in primary position. JAAPOS 1998;201–206. Hawes MJ, Dortzbach RK. The microscopic anatomy of the lower eyelid retractors. Arch Ophthalmol 1982;100(8):1313–1318. Hayreh SS, Scott WE. Fluorescein iris angiography. Arch Ophthalmol 1978;96:1390–1400. Helveston EM, Merriam WW, Ellis FD, et al. The trochlea: a study of the anatomy and physiology. Ophthalmology 1982;89:124–133. Hiatt RL. Production of anterior segment ischemia. Trans Am Ophthalmol Soc 1977;75:87–102. Jampel RS. The fundamental principle of the action of the oblique ocular muscles. Am J Ophthalmol 1970;69:623. Koornneef L. Orbital septa: anatomy and function. Ophthalmology 1979;86:876–880. Linwong M, Herman SJ. Cycloduction of the eyes with head tilt. Arch Ophthalmol 1971;85:570. McKeown CA, Lambert HM, et al. Preservation of the anterior ciliary vessels during extraocular muscle surgery. Ophthalmology 1989;96: 498–507. Mims JL, Wood RC. Bilateral anterior transposition of the inferior obliques. Arch Ophthalmol 1989;107:41–44. Mims JL, Wood RC. Anti-elevation syndrome after bilateral anterior transposition of the inferior oblique muscles: incidence and prevention. J Am Assoc Pediatr Ophthalmol Strabismus 1999;3(6):333–336. Morrison JC, van Buskirk EM. Anterior collateral circulation in the primate eye. Ophthalmology 1983;90:707–715. Oh SY, Poulkens V, Demer J. Quantitative analysis of rectus extraocular muscle layers in the monkey and humans. Investig Ophthalmol Vis Sci 2001;42(1):10–17. Parks MM, Bloom JN. The “slipped muscle.” In: Symposium on strabismus. Transactions of the New Orleans Academy of Ophthalmology. St. Louis: Mosby, 1978:1389–1396. Parks MM. Atlas of strabismus surgery. Philadelphia: Harper & Row, 1983. Parks MM. Causes of the adhesive syndrome. In: Symposium on strabismus. Transactions of the New Orleans Academy of Ophthalmology. St. Louis: Mosby, 1978:269–279. chapter 2: anatomy and physiology of eye movements 69 32. Plager DA, Parks MM. Recognition and repair of the “lost” rectus muscle. Ophthalmology 1990;97:131. 33. Porter JD, Baker RS, Ragusa RJ, Brueckner JK. Extraocular muscles: basic and clinical aspects of structure and functions. Surv Ophthalmol 1995;39:451–484. 34. Saunders RA, Sandall GS. Anterior segment ischemia syndrome following rectus muscle transposition. Am J Ophthalmol 1982;93: 34–38. 35. Saunders RA, Phillips MS. Anterior segment ischemia after three rectus muscle surgery. Ophthalmology 1988;95:533–537. 36. Simon JW, Price EC, et al. Anterior segment ischemia following strabismus surgery. J Pediatr Ophthalmol Strabismus 1984;21:179–184. 37. Spencer RF, Porter J. Structural organization of the extraocular muscles. In: Buttner-Ennever J (ed) Neuroanatomy of the oculomotor system. Amsterdam: Elsevier, 1988:33–79. 38. Stager DR, Weakley DR, Stager D. Anterior transposition of the inferior oblique: anatomic assessment of the neurovascular bundle. Arch Ophthalmol 1992;110:360–362. 39. Stager DR, Porter J, Weakley DR, Stidham DB. A comparative microscopic analysis of the capsule of the nerve to the inferior oblique muscle. Trans Am Ophthalmol Soc 1997;95:453–462; discussion 463–465. 40. Swan KC. Fascia in relation to extraocular muscle surgery. Arch Ophthalmol 1970;83:134–140. 41. Virdi PS, Hayreh SS. Normal fluorescein iris angiographic pattern in subhuman primates. Investig Ophthalmol Vis Sci 1983;24:790–793. 42. von Noorden GK. Anterior segment ischemia following the Jensen procedure. Arch Ophthalmol 1976;94:845–847. 43. von Noorden GK. Letter to the Editor. A magnetic resonance imaging study of the upshoot downshoot phenomenon of Duane’s retraction syndrome. Am J Ophthalmol 1991;112:358–359. 44. Wilcox LM Jr, Keough EM, et al. The contribution of blood flow by the anterior ciliary arteries to the anterior segment in the primate eye. Exp Eye Res 1980;30:167–174. 45. Wright KW, Lanier AB. Effect of a modified rectus tuck on anterior segment circulation in monkeys. J Pediatr Ophthalmol Strabismus 1991;28:77–81. 46. Wright KW, et al. Acquired inflammatory superior oblique tendon sheath syndrome: a clinicopathologic study. Arch Ophthalmol 1982; 100:1752–1754. 47. Wright KW. Color atlas of ophthalmic surgery: strabismus. Philadelphia: Lippincott, 1991. 48. Wright KW. Discussion of paper: Recognition and repair of the lost rectus muscle. Ophthalmology 1990;97:136. 49. Wright KW. The fat adherence syndrome and strabismus after retinal surgery. Ophthalmology 1986;93:411–415.