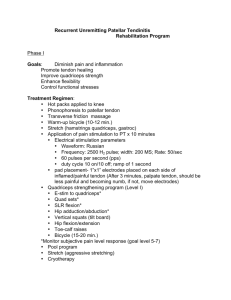
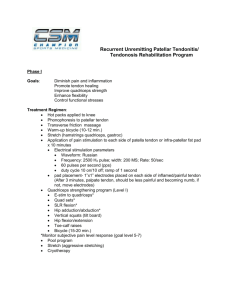
Patellar Tendinopathy / Jumper’s Knee Patellar Tendinopathy Advice: Click Here to View Video We strongly advise seeing a physical therapist for patellar tendonitis pain or any joint pain. Below are the general recommendations from the PJF Performance PT, Jason Pinili. If you would like to set up an online consultation with Jason please email pjfsystem@pjfsystem.com MOST COMMON SIGNS: Pain right below kneecap Pain with quad activation/loading (squats, stairs, jumping, landing, cutting, jogging/running) Pain/stiffness upon getting out of bed, warming up, or after activity • • • • Stage 1: Pain after sports activity Stage 2: Pain at the beginning of sports activity, disappearing with warm-up and sometimes reappearing with fatigue; performance not greatly affected Stage 3: Pain at rest (before and after) and during activity; inability to participate in sports due to performance being affected Stage 4: Rupture of the patellar tendon MOST COMMON CAUSES: 1. 2. Overuse a. Training Volume i. Frequency ii. Duration iii. Intensity b. Too much too soon c. Take a day or two off- when returning to training, decrease load to 50-75% of previous load as long as: d. Pain is not >5/10. Athlete should find alternative methods of retaining tensile strength of patellar tendon- elliptical, biking, swimming, etc. e. Sessions of high intensity should be accompanied with increased rest between sessions Poor Glute Activation/Utilization, Endurance, or Strength a. Decreased hip hinge or glute activation may result in increased knee flexion, demand on quad, force through patellar tendon b. Should implement glute strengthening and improve endurance within program i. Example: prone hip extension-> DL bridge -> SL bridge -> clamshells -> wall sits > theraband sidesteps -> hip hinges -> DL deadlift -> SL RDL -> SL rdl catching weighted ball -> SL step down into SL RDL -> lateral hop to SL RDL ii. Focus on hip hinge with adequate knee flexion (too much hip hinge can place excessive force on low back) 3. 4. 5. Poor Ankle Stability (sprained ankles, decreased proprioception, strained calves, excessive pronation) a. Poor eccentric plantar flexion when landing resulting in force not being absorbed at ankle; knee joint is next joint up to absorb force- can occur with landing, cutting, or balance strategy (if player has poor inversion/eversion/plantar flexion control, he or she will use the quad to eccentrically absorb or concentrically push off b. Focus on eccentric control of plantar flexion as if player was rebounding, slowly controlling heels to the ground c. Add intrinsic foot strengthening/endurance to disperse more force at the level of the ankle/foot d. Ankle strategy/balance in all planes; appropriately use different surfaces to challenge proprioception as well as challenge hand eye coordination while balancing Poor Muscle Length (quad, hamstring, hip flexors, calves), joint mobility a. The main muscles associated with the development of patellar tendon pain are decreased quadriceps and hamstring flexibility i. Poor quad length will result in constant tensile force on patellar tendon (imagine a towel being wrung- the tendon can lose elasticity) ii. Poor hamstring length will predispose the knee into excessive knee flexion, increasing demand on quad b. Dynamic warm-up prior to activity; static OK after activity i. Increase dynamic warm-up time >5-10 min to ensure increased blood flow, lengthening, elasticity if muscle fibers in a functional, sport specific range ii. Ex: quad stretch + calf raise, lunge + rotation, lateral lunges, floor swipes (hamstrings), inch worms, and add in TKE with band to pump the quads and lubricate the tendon Poor Joint Mechanics or Structure (ankle or hip impingement, patellar tracking, tibial rotation, patella alta) a. A stiff landing pattern and a short landing time is associated with patellar tendinopathy b. Excessive external tibial torsion moment during takeoff c. Joint space or structure may require manual therapy for patellar tracking, tibial- femoral mobilization, talocrural mobilization, hip mobilization; superbands may be used for selfmobilization WHAT TO DO / INTERVENTION 1. Reduce Load / Unload Patellar Tendon a. Reduction dependent on intensity/frequency of pain; rest according to intensity of paina day or two off is OK before returning to training or play at ~50-75% intensity or load b. Ideally, an athlete won’t significantly reduce load due to negative effects on the tendon’s tensile strength c. Decrease overall training volume instead (sets x reps) i. Use crosstraining (ex: for basketball players- bike, elliptical, swim, pool running, alter-g treadmill, etc.) instead of just running and playing basketball 2. Reload Patellar Tendon a. Isometrics i. 5x45s holds (70% MVC); pain must settle within 24 hours (if not, load tolerance has been exceeded and program should be modified) ii. Use when pain is >5/10 iii. Manual resistance (open chain knee extension (leg extension machine), Spanish squat, wall sits, TKE) b. Isotonics i. Pain < 3-5 /10 ii. 3 sets 10-15 reps 3x/week (isometrics should be done every day) iii. Sit to stands, TKE (bilateral if using body weight; unilateral if using equipment for resistance), split squats, step downs (forward, lateral), decline squats (gold standard for patellar tendinopathy as it loads the patellar tendon more than regular squats without being excessive) iv. Eccentric exercises 1. Improve tensile strength appropriately (pain ~ 3-5 out of 10 is ok to be monitored; if >5/10 decrease load or increase rest periods between exercises/training sessions v. Heavy Slow Resistance Training 1. 3 exercises: Squats, Leg press, Hack Squat; heavy resistance, slow movement (3s concentric, 3s eccentric); similar results to eccentric training 2. Begin at 15RM progressing to 6RM as appropriate a. If using a decline board, ideal between 15° and 30° decline of the board, and less than or equal to 60° knee flexion to avoid excessive loading of the patellofemoral joint c. Open Chain -> Closed Chain -> Functional and/or Multiplanar Movements i. Once exercises are no longer uncomfortable, athlete may be able to progress ii. When can an athlete be progressed to functional/sport specific, multiplanar movements? 1. When an athlete can perform 4-8 repetitions of a single leg press at 150% BW that they may try stage three exercises; but pain must be <3/10 and symptoms must settle within 24 hours. iii. Hopping, landing, changing directions, cutting, acceleration, deceleration iv. Athlete can return to sport if they can appropriately handle 3 sessions of high load, sport specific movements with no symptoms within 24 hours TIPS - Core, hips, knees, ankles must all be assessed for joint ROM in open chain and closed chain. - Identify mechanical compensations with functional or sport specific movements; are there muscle strength or endurance deficits? You may not see endurance and activation deficits unless player is working out or playing in game. - What is the player’s previous injury history? - Is the player right or left-handed? Which leg is their dominant leg or their take off foot? Is a player a two-foot jumper or one-foot jumper? - With all closed chain exercises, focus should be on preventing excessive anterior displacement of the knees over the toes. Knees will come forward with any squatting, but it must be appropriate to prevent excessive loading of the patellar tendon. - Mechanics can always be corrected in rehab or training, but will it translate to on the court? Highlight the importance of SL activities, and when appropriate, add external forces or challenge player to think and react while maintaining mechanics. - Stretching / muscle lengthening program should be completed throughout rehab and maintenance- hip flexor stretching, quad stretching, calf, glute, piriformis etc. Foam Rolling can be used as tolerated to release soft tissue restrictions throughout the quad, calves, hamstrings. - Current research has shown that anti-inflammatories are not as effective given that most jumper’s knee are chronic degenerative changes, not inflammation (Tendons--time to revisit inflammation. Rees JD, Stride M, Scott A. Br J Sports Med. 2014 Nov; 48(21):1553-7.) - Ice is ok for after activity- 20-30 minutes max - Corticosteroid injections should not be used for any tendon pathology due to long term degradation - Avoid sitting with knees past 90° knee flexion to prevent tensile force on patellar tendon (ex: towel being wrung out); sit with knees straighter when possible - How do I know when it’s time to take time off? o o If you are having significant pain while playing and it is affecting your movement or performance, it is time to step away from the court and focus on rehab, improving strength, mobility, endurance, mechanics. If you are having pain but it doesn’t affect your performance, and it becomes tolerable as you warm up, you may not have to completely step away from playing, but you may need to take the necessary steps to rehab your knee to prevent it from becoming worse. - Recent research has shown that supplementing with 15 g gelatin and 50 mg vitamin C 1 hour before exercise leads to 160% better results in the tendon. This study, from UC Davis, also advises shorter/more frequent sessions for optimal tendon health (Shaw, Barr et al 2017). Two sessions per day or every other day lasting 5-10 minutes is best. These sessions must be separated by at least 6 hours. Essentially one session in the morning and one session in the evening is more effective than one long session. - Below is a recipe for gelatin from the UC Davis study. Gelatin could also be taken in supplement form if preferred. Also, this study showed the gelatin/vitamin C combination to be effective, but it is possible that bone broth may work as well. This recipe adapted from the UC Davis original recipe, and makes eight servings: Ingredients • • • • • • 80 grams of gelatin (½ cup or 10 packets of most brands) 1 cup water 2 cups other liquid (choice of juice/liquid for flavoring, or additional water and use a natural sweetener to taste) 500 mg Vitamin C ½ capsule of Thorne’s NSF Certified forSport® Ascorbic Acid ¼ scoop of Thorne’s Buffered C Powder (for additional calcium, magnesium, and potassium) Directions • • • • • • Bring the two cups of other liquid to a boil Mix the gelatin and vitamin C into one cup of room temperature water Add the boiling liquid to the gelatin/vitamin C mixture Pour into a flat tray or a silicone ice cube tray in eight equal parts Place in the refrigerator If using a flat tray, divide into eight equal pieces