Regulation of Glycolysis
advertisement

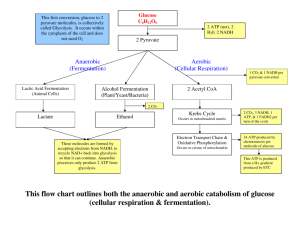
GOALS FOR LECTURE 9: Predict which steps in any metabolic pathway are most likely to be regulated Identify the key regulated steps in glycolysis List the allosteric effectors that regulate key glycolytic enzymes and describe their effects on enzyme activity. Rationalize the roles of these effectors based on cellular energy needs. Recommended reading: TOPIC STRYER, 5th edition DEVLIN, 5th edition Regulation of glycolysis Ch. 16, 443-450 Ch. 14, 614-649 Regulation of Glycolysis: 1. 2. 3. 4. Flux through a metabolic pathway can be regulated in several ways: Availability of substrate Concentration of enzymes responsible for rate-limiting steps Allosteric regulation of enzymes Covalent modification of enzymes (e.g. phosphorylation) Of the 10 steps in the glycolytic pathway, three involve large negative ∆G and are essentially irreversible. These are steps 1 (phosphorylation of glucose), 3 (phosphorylation of fructose-6-phosphate) and 10 (transfer of phosphate from phosphoenolpyruvate to ADP). Net ∆G for glycolysis is about -23 kcal/mol. G o’ (kcal/mol) G (kcal/mol) -4.0 -8.0 +0.4 -0.6 -3.4 -5.3 4. Aldolase +5.7 -0.3 5. Triose phosphate isomerase +1.8 +0.6 6. Glyceraldehyde-3-phosphate dehydrogenase +3.0 -0.8 -9.0 +0.6 8. Phosphoglycerate mutase +2.1 +0.4 9. Enolase +0.8 -1.6 -15.0 -8.0 ENZYME 1. Hexokinase ATP Yield -1 2. Phosphoglucoisomerase 3. Phosphofructokinase 7. Phosphoglycerate kinase 10. Pyruvate kinase -1 +2 +2 9.1 In practice, we generally consider reactions where ∆G is larger than about -2 kcal/mol to be “irreversible”, since at equilibrium the products outnumber the reactants by more than 30:1. If ∆G is larger than -4 kcal/mol, products outnumber reactants by more than 1000:1. The relative magnitude of the energy changes through glycolysis can be best appreciated graphically: The enzymes responsible for catalyzing the three steps with very large negative ∆G, hexokinase (or glucokinase) for step 1, phosphofructokinase for step 3, and pyruvate kinase for step 10, are the primary steps for allosteric enzyme regulation. Generally, enzymes that catalyze essentially irreversible steps in metabolic pathways are potential sites for regulatory control. Usually this is because blocks elsewhere in a pathway may lead to the accumulation of intermediates. Availability of substrate (in this case, glucose), is another general point for regulation. The concentration of these three enzymes in the cell is regulated by hormones that affect their rates of transcription. Insulin is a peptide hormone secreted by pancreatic β cells in response to sudden increases in blood glucose levels, such as after a carbohydrate-rich meal. It is also secreted in response to increases in amino acid levels in the blood, as well as in response to gastrointestinal and other hormones (insulin will be revisited in future discussions of lipid metabolism and diabetes). The general effect of insulin is to promote the storage of energy when food is available in abundance. Glucagon is a different peptide hormone secreted by the pancreatic α cells. Its secretion is stimulated by low blood glucose levels, and its general effect is to oppose the action of insulin. Insulin upregulates the transcription of glucokinase, phosphofructokinase, and pyruvate kinase, while glucagon downregulates their transcription. These effects take place over a period of hours to days, and generally reflect whether a person is well-fed or starving. 9.2 Regulation of glucose uptake The rate of entry of glucose into a cell is limited by the number of glucose transporters on the cell surface and the affinity of the transporters for glucose. The members of the glucose transporter family are expressed at different levels in different tissues. Average blood glucose levels typically hover around 5 mM, but can go as high as 12 mM immediately after a rich meal. The basal glucose transporters present in nearly all cells have a Km for glucose of around 1 mM, much less than the average blood glucose concentration. For most tissues, then, glucose uptake proceeds at a fairly constant rate, regardless of the amount present in the blood. Liver and pancreatic β cells have a distinct glucose transporter with a high Km, around 15-20 mM. In these cells, then, the amount of incoming glucose is pretty much proportional to the amount of glucose in the blood. This allows the β cells to monitor blood glucose levels directly, and thereby regulate insulin secretion. It also insures that glucose is taken up rapidly by the liver only when it is abundant; in the fasting state, more glucose is delivered to other tissues (particularly the brain). Muscle and fat cells express a third type of glucose transporter, with a Km around 5 mM. The level of expression of this transporter on the cell surface is rapidly regulated by insulin. Secretion of insulin causes translocation of these receptors from intracellular stores to the cell surface, allowing more efficient energy storage by these tissues when blood glucose is in excess. 9.3 Hexokinase and glucokinase Hexokinase performs step 1 of glycolysis in most tissues, including muscle and brain. It has a low Km (high affinity) for glucose, so it permits initiation of glycolysis even when blood glucose levels are relatively low. However, its Vmax is relatively low. Hexokinase is inhibited by the product of its reaction, glucose-6-phosphate. This is a very important regulatory step, since it prevents the consumption of too much cellular ATP to form G6P when glucose is not limiting. Glucokinase, found in the liver and pancreatic β cells, requires a much higher glucose concentration for maximal activity. It is thus most active when glucose is very high in the portal vein, immediately after consumption of a carbohydrate-rich meal. It has a high Vmax, allowing the liver to effectively remove excess glucose, and minimize hyperglycemia after eating. Glucokinase is not inhibited by G6P. Tissue distribution: Km V max Inhibition by G6P Hexokinase Most Low (0.1 mM) Low Yes Glucokinase Liver and β cells High (10 mM) High No In the liver, the action of glucokinase is opposed by the action of glucose-6phosphatase, which hydrolytically removes phosphate in a futile cycle. At normal levels of blood glucose (5 mM), the forward and back reactions are balanced. This is wasteful of ATP, but helps the liver to buffer blood glucose concentrations. Glucokinase activity is also affected by an inhibitory binding protein, whose affinity for glucokinase is enhanced by binding fructose-6-phosphate and lessened by binding fructose-1-phosphate. Fructose consumed in the diet (in the form of native fructose or sucrose) is converted to F1P in the liver. This opposes the action of F6P on glucokinase, favoring the forward reaction. The capacity of liver cells to phosphorylate fructose exceeds their capacity to metabolize F1P. Consumption of excess fructose can cause an imbalance in liver metabolism by indirectly depleting liver cells of ATP. 9.4 Phosphofructokinase Phosphofructokinase (PFK) catalyzes the rate-limiting step in glycolysis and is the most important control point. It is also the first irreversible step that is unique to the glycolytic pathway; G6P can be used as an intermediate in other pathways including glycogen synthesis and the pentose phosphate pathway (which will be discussed later). PFK is allosterically inhibited by ATP, so glycolysis is slowed when cellular ATP concentrations are high. ATP binds to a site on PFK distinct from the active site, causing a conformational change resulting in rotation of the positions of Arg162 and Glu161. In the high-affinity state, the positive charge on Arg162 stabilizes the negative charge on the phosphate of F6P, and Km is low. In the low-affinity state, the negative charge on Glu161 repels F6P. PFK in high-affinity state PFK in low-affinity state The conformational transition between these two states is also regulated by cellular pH. Excess H + ions favor the low affinity state. Thus when cellular lactate is high (usually when oxidative phosphorylation is inhibited), the rate of glycolysis is reduced, preventing further accumulation of intracellular acid. This regulation helps to minimize the risk of lactic acidosis when oxygen is scarce. Glycolysis is also a means of preparing carbon-containing backbones for biosynthetic reactions, in the form of acetyl-CoA. Citrate, an intermediate in the TCA cycle, also inhibits PFK, signaling that biosynthetic precursors are abundant. 9.5 When cellular energy is limited, glycolysis should be upregulated. PFK is allosterically activated by high levels of AMP. AMP overcomes the inhibitory effect of ATP. Another allosteric activator of PFK is fructose 2, 6 bisphosphate. F-2,6-BP is not an intermediate in the glycolytic pathway. F-2,6-BP also overcomes the inhibitory effect of ATP. F-2,6-BP is made from F6P by a specific kinase, phosphofructokinase 2 (PFK2). The same polypeptide that encodes this kinase also encodes a phosphatase that catalyzes the reverse reaction, fructose bisphosphatase 2 (FBPase2). Activity of this bifunctional enzyme is controlled by phosphorylation. 9.6 Phosphorylation of the bifunctional enzyme is regulated by blood glucose level, mediated by glucagon and insulin. High glucagon (low blood sugar) causes phosphorylation of the enzyme, which results in conversion of F-2,6-BP back to F6P, removing its stimulatory effect on PFK, and therefore slowing the rate of glycolysis. Conversion of F6P to F-2,6-BP is also stimulated by high levels of F6P. This is an example of feedforward stimulation (the opposite of feedback inhibition). Feedforward regulation ensures that intermediates on metabolic pathways do not accumulate uselessly. F-2,6-BP is also an important regulator of the process of gluconeogenesis, where glucose is synthesized from pyruvate. Pyruvate kinase Pyruvate kinase is the third regulated enzyme of glycolysis. Like PFK, pyruvate kinase is regulated both by allosteric effectors and by covalent modification (phosphorylation). Pyruvate kinase is activated by F-1,6-BP in the liver, a second example of feedforward stimulation. ATP and alanine (a biosynthetic product of pyruvate) act as allosteric inhibitors of pyruvate kinase. Phosphorylation of pyruvate kinase is regulated by blood glucose level, just like PFK. High glucagon (low blood sugar) causes phosphorylation, which in this case renders the enzyme inactive. Pyruvate kinase deficiency causes hemolytic anemia, since red blood cells rely entirely on glycolysis for ATP synthesis. In this inherited disorder, pyruvate and lactate levels are lower than normal, while proximal intermediates such as 1,3 BPG and PEP accumulate. Hormonal regulation of glycolysis ensures coordination among different tissues and organs. As we will see later, the same hormones that regulate the rate of glycolysis also regulate gluconeogenesis and the metabolism of glycogen, a stored form of glucose. 9.7 Summary: Regulation of the glycolytic pathway 9.8