Fundamentals of Care Fundamentals of Care
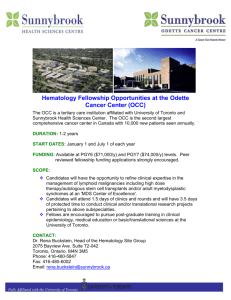
advertisement

Fundamentals of Care Guidance for Health and Social Care Staff Improving the quality of fundamental aspects of health and social care for adults Fundamentals of Care Guidance for Health and Social Care Staff Improving the quality of fundamental aspects of health and social care for adults This version of the Fundamentals of Care is aimed at staff of all grades who provide care and the organisations that employ them. These organisations include all providers of health and social care. Contents Foreword 2 1. Aim of Fundamentals of Care 3 2. Using the Guide 4 3. Introduction to the Practice Indicators 6 4. Practice Indicators 7 1. Communication and information 2. Respecting people 3. Ensuring safety 4. Promoting independence 5. Relationships 6. Rest and sleep 7. Ensuring comfort, alleviating pain 8. Personal hygiene, appearance and foot care 9. Eating and drinking 10. Oral health and hygiene 11. Toilet needs 12. Preventing pressure sores 7 14 19 25 30 35 38 42 46 50 55 59 5. Monitoring the use of the Practice Indicators 63 6. Useful contacts 65 Appendices: 66 A1. Steering Group membership 66 A2. Contributors to redrafting 67 Foreword by Jane Hutt AM, Minister for Health and Social Services The twelve aspects of care described in the document draw together, for the first time, guidance on the quality of care service users may expect from health and social care providers in Wales. I know, from talking with service users, that they are as much affected by the general experience of their care as by its outcome. I also recognise that the experience of care is often variable and dependent on the type of service accessed and geography. These indicators will help ensure that such inequities are addressed across Wales. They relate to a range of settings, from a person’s own home, to care homes and hospitals and to all organisations dedicated to delivering care, in the health, social or independent sectors. Individuals and organisations providing health and social care within Wales, should use these indicators to develop and improve the services they deliver. It is only by constant reference and review that we can raise the quality of care. So much is being achieved already, but more remains to be done, so that the more vulnerable members of our society are helped to enjoy a better, healthier and happier future. I am pleased to commend this document to you. Jane Hutt AM Minister for Health & Social Services 1. Aim of Fundamentals of Care Fundamentals of Care is a Welsh Assembly Government initiative included in the Plan for Wales as part of “Improving Health and Care Services”. The initiative grew out of the following: ● Inconsistency of quality across service settings and areas. ● Emphasis, until recently, on service efficiency and cost, rather than quality of care. ● Common themes in complaints and compliments. ● Increasing expectations of service users. ● Developing partnerships with service users and between organisations. ● Lack of clarity for service users on what they should expect. ● Increasing focus on regulation and performance. ● Awareness of Essence of Care, DOH, 2001. Fundamentals of Care therefore aims to improve the quality of aspects of health and social care for adults. The indicators will be integrated with educational, commissioning and performance management frameworks for the NHS, Social Services and the Care Standards Inspectorate, as appropriate. They therefore reflect an integrated whole systems approach, making them relevant to multi-disciplinary environments across organisational boundaries. 3 2. Using the Guide providers respond to and meet the needs of service-users. Fundamentals of Care is also designed to enable service-users to assess for themselves whether the care they receive is appropriate to their personal circumstances. For example each section suggests an indicator to which care providers should aspire. The indicators are referenced to the relevant Care Standard Regulations. This approach will help both the service provider and the service-user. The service provider can utilise Fundamentals of Care for self audit and quality control purposes and establish how each indicator relates to Care Standard Regulations. In turn service-users in private, voluntary and local authority sector provision are better able to understand how the Care Standards Act shapes the services they may receive. The first reaction to these indicators may be that they are nothing new. This is true. Indeed it would be surprising if material did not already exist on the key subjects addressed, for example, the Essence of Care in England, DOH, 2001. What is different is that these indicators are applicable to the whole of Wales, across the full range of health and social care settings. To achieve this, this document draws together a composite set of indicators from a range of statutory, mandatory and professional requirements and national policies. These include (amongst others): National Minimum Standards, National Service Frameworks, National Institute of Clinical Excellence documents, Occupational Standards and Professional Codes of Conduct. Additional indicators have been included where gaps have been identified from a literature search and extensive consultation. Expectations of service providers in the private and voluntary sector Using the Fundamentals of Care alongside other guidelines and standards Fundamentals of Care does not impose any new requirements, obligations or standards upon domiciliary, care homes or independent healthcare providers. Providers of these services are registered and regulated by the National Assembly through the Care Standards Inspectorate for Wales (CSIW). Fundamentals of Care will supplement but not replace the Regulations and National Minimum Standards issued by the National Assembly and enforced by CSIW. It is anticipated that all care providers, anxious to maintain and develop quality personal care services, will incorporate Fundamentals of Care within training and staff development programmes as a basic foundation for the provision of quality services. Both Health and Social Services may also incorporate these indicators into commissioning, contractual or service-specification requirements. Fundamentals of Care views the service-user as the most significant stakeholder in the development and promotion of best practice and quality services. On a personal basis the relationship between the service-user and care provider is fundamental. The relationship between the person giving care and the person receiving care should be a partnership. Everyone is an individual and should be treated according to their needs and wishes. Service-users should receive the highest quality of care and service providers have a responsibility to provide this. At a wider level, practice and services are governed by legislation and regulations. They are also influenced by standards and guidance. In this broader context Fundamentals of Care seeks to stimulate improvements in quality and the way care 4 Act Regulations. They are therefore supplementary to secondary and primary legislation. It is anticipated, however, that Fundamentals of Care will play a significant role in the development of commissioning, staff training and development programmes. Social Services may wish to use the indicators when commissioning from private sector providers. Expectations of the National Health Service Within the Health Services Fundamentals of Care will be used to drive up and improve the consistency, quality and delivery of care. As a baseline Fundamentals of Care should be used to establish targets for the consistent improvement of services and the provision of care regardless of setting. It is recommended that individual staff and organisations identify those indicators from the cross-references that should already be complied with. For the other indicators there is a responsibility to ensure they are integrated into educational and monitoring systems. All indicators are to be met and compliance systematically monitored, whether this be through clinical supervision, peer review, audit or operational performance mechanisms. Putting the indicators into practice The following need to be considered: ● the service user and their choices and wishes ● the service user’s capacity, capabilities and need of care ● the unpaid carer’s capacity, capabilities and need of training ● staffing levels and skill mix ● use of evidence-based professional assessment tools, practice, and models of care ● the type of environment in which the care is given ● competency, training and education of staff ● supervision of staff ● the maintenance of buildings and equipment ● the provision of suitable facilities and equipment ● operational procedures and policies ● monitoring and evaluation of services ● links to clinical governance systems. The NHS may also wish to use the indicators when commissioning from private sector providers. Expectations of Local Authority Social Service Departments Social Services may use Fundamentals of Care as a nationally recognised framework and where appropriate audit existing domiciliary and residential care services against the relevant indicators. In order to clarify the position fully, Fundamentals of Care may underpin or support Care Standard 5 3. Introduction to the Practice Indicators The document presents a list of indicators that cover twelve Fundamental Aspects of Health and Social Care: ● ● ● ● ● ● ● ● ● ● ● ● Each aspect is described in a separate section. The sections are layed out as follows: Communication and information. Respecting people. Ensuring safety. Promoting independence. Relationships. Rest and sleep. Ensuring comfort, alleviating pain. Personal hygiene, appearance and foot care. Eating and drinking. Oral health and hygiene. Toilet needs. Preventing pressure sores. ● ● ● ● ● The indicators are research and best practice based, having been developed in the light of extensive consultation and a wide range of reference documents. ● The indicators are not in priority order. Most of them relate to the provision of care in any setting, but some will be less relevant in a person’s own home. ● To gain maximum benefit, you will need to read every section. Issues such as respect, independence, communication and choice are important in every situation. an introduction setting the context; a Principle quality statement; Practice Indicators which say in greater detail how the Principle can be put into practice; text in italics under some indicators providing additional guidance for staff; some examples of what the indicators mean in practice to help staff use them. They are not exhaustive and therefore do not cover everything. They are intended to give some clear compass points. Staff will be able to add to the list through their own good and considered practice; cross references which relate the principle and supporting indicators to corresponding existing legal requirements, professional and national standards. Where cross-references are in italics, this indicates that the document referred to is in draft form at the time of writing; selected references. Two other versions are available. The Flyer version contains the Principles and the Booklet has the Principles and Practice Indicators. These two versions are worded with the service user in mind. The documents are also available on the Internet. 6 4. Practice Indicators People have the right under legislation to see the information that has been recorded about them in their medical or care records and, if necessary, to correct any mistakes. The requirement for confidentiality and protection of any information about an individual held in records however remains an important principle (Indicator 1.5). 1. Communication and information This aspect of care includes written, oral and non-verbal communication between staff and service users and their relatives and carers. Many of the failures or complaints about health and social care are due to misunderstandings, inadequate information, or failures in communication. There should be clear and accurate information about the type of service provided. It should be presented in such a way as to take account of special needs. Information must be given in a format and language, which is suitable for the intended use, and reaches the right balance of every day words, technical terms, and explanation. The Patient’s Charter (1990) established that patients have the right to a clear explanation of all proposed treatments, including any risks involved and the alternatives before giving consent. The provision of information is one of the driving forces of NHS philosophy, and communication with users of health and social care services is a key principle of a recent Welsh Assembly Government document The Health and Social Care Guide for Wales (2002). The importance of open and honest communication must be emphasised. People are entitled to know about their condition, especially if they request this information. They should be treated with sensitivity and understanding and account should be taken that people under stress or anxious, may not hear, understand, or remember what has been said. All service users must feel able to raise concerns and know how to make a complaint about a service which has not met their expectation. They must be able to do so without fear of being penalised and have the assistance of independent advice and advocacy if desired. Special care must be taken in communicating with those whose mental capacity may be temporarily or permanently impaired. The more people understand their condition and its treatment, and become involved in decisions about the care they receive, the better they are able to make appropriate choices and manage their own care. Partnership between health and social care providers, patients, clients, service users, their relatives and carers, is the cornerstone of appropriate person centred care. This is important at all stages in the care of an individual, but particularly so during arrangements for transfer of care to alternative care settings, and during the discharge planning process. Effective communication takes time and should be considered to be part of workload, prioritisation and time management. Except in very special circumstances, which are specified in law, informed consent must always be obtained to treatment and care. Intervention without consent may be an assault. On the other hand, non-intervention for people unable to consent may amount to neglect. Principle People must receive full information about their care in a language and manner sensitive to their needs. 7 amongst team members and records may be accessed and used by all. In some circumstances, information may be shared with other staff involved in the care of the individual, if the caring role of the colleague could not be undertaken effectively without knowledge or information relating to the person receiving care. In certain circumstances there is an additional requirement to share information i.e. when information is required by a court order and when it can be justified as being in the interests of protecting the public. Practice Indicators 1.1 Health, personal and social care needs are assessed and set out in a regularly reviewed plan of care. This plan is agreed by the service user and the people caring for them. The plan is only shared with others with the service user’s consent. The plan of care is agreed by the service user and made available to them. The assessment, plan of care and its implementation are recorded and monitored. The plan of care is reviewed to ensure services remain appropriate to the service user’s needs. 1.2 Assistance or specialist aids are provided to those with speaking, sight or hearing difficulties, special needs or learning disabilities, enabling them to receive and respond to information. 1.6 Time is taken to listen and actively respond to any questions and concerns that the service user or their relatives may have. If the person providing care does not have sufficient knowledge to answer questions adequately, they refer them to the appropriate colleague. 1.3 If necessary, people are provided with access to a translator or a member of staff with appropriate language skills. If a translator is needed, they must be thoroughly briefed on the context of the information they convey and on the requirement for confidentiality. 1.7 People are given information explaining how to comment on their care or make a complaint. If requested, information is also given on how to obtain independent advice and support. Some examples of what the indicators mean in practice 1.4 People are consulted about any treatment and care they are to receive. A suitably knowledgeable person explains treatment or care options so that people can make informed choices. Their consent or refusal is clearly and accurately recorded. Some people may have a limited capacity to understand e.g. people with learning disabilities or mental illness. In such cases, every effort is made to help them comprehend what is being said and to involve them in the decision making process with their carer or next of kin. 1.5 People’s personal records are regularly updated and available to them. To ensure confidentiality, they are kept secure and comply with the Data Protection Act 1998. Where care is delivered by a multi-disciplinary team, information needs to be shared 8 ● Always ensure that information you give is accurate. ● Almost never use jargon; if you need to, explain what it means. ● Never assume that your service user is being given information in an appropriate format; always ask them. ● Be clear and unambiguous in what you say or write. ● Always check whether people have any questions. ● Answer questions openly and as simply as you can. ● ● If you are not sure you have correctly understood what your service user is asking or requiring of you, ask them. When you have promised to return to the person using services at a later date with information, always ensure that this is done. ● Make sure that all of your recording is undertaken in a way that can be made accessible to the person using services and will be easily understood by them. ● When a person using services voices dissatisfaction, encourage them to make a complaint if you are not in a position to resolve the issue yourself. ● When you are aware that you have not delivered any aspect of service as well as you might have done, apologise and explain how you will ensure that the problem is resolved. ● through the supervision process, with Fundamentals of Care in mind. ● If you have a job that involves you in preparing information for the benefit of people who use services, check that your local standards are consistent with Fundamentals of Care and always consult service users, carers and other lay people, elected members of the Council for example, before publishing your document. ● If you have reason to think that some one may have an impairment of mental capacity you must consider what information and to whom you should communicate. Where appropriate you should follow the guidance on consent to treatment. N.B. The key thing to remember here is that all people who use health and social care services have a right to be told what is happening to them and why, in a way that is easily intelligible and meets any particular needs they may have. If you are a manager, ensure that communicating and giving information is something you address regularly Cross references Fundamentals Indicator Corresponding Standards Principle Code of Ethics and Professional Conduct for Occupational Therapists Section 2 Creating a Unified and Fair System for Assessing and Managing Care (Unified Assessment Process) NAfW NMS Care Homes for Older People standards 1 NAfW NMS Care Homes for Younger Adults standard 1 Framework for best practice: the production and use of the health information for the public Health and Social Care Guide sections 1,5,7 Improving Health in Wales chapter 3 Level 2 National Occ. Standards in Care Unit 011 Level 3 National Occ. Standards in Care Unit 022 Level 3 National Occ. Standards in Prom. Ind. Unit 023 NMC Code of Professional Conduct section 3 Social Care Induction Framework Core Areas 1.1,1.2,1.3,4.2 Welsh Risk Management Standard 8 9 Fundamentals Indicator Corresponding Standards 1.1 NAfW NMS Care Homes for Older People standard 6 NAfW NMS Care Homes for Younger Adults standard 6,18 CSP Core Standards 8,10 Creating a Unified and Fair System for Assessing and Managing Care Health and Social Care Guide section 1,5,7 Level 3 National Occ. Standards in Care Units SC8,NC11 Level 3 National Occ. Standards in Prom. Ind. Units SC3,SC8 NSF for Diabetes Standard 3 NMC Code of Professional Conduct section 2 Tackling Coronary Heart Disease in Wales standard 2 1.2 NAfW NMS Care Homes for Older People standards 36.6 NAfW NMS Care Homes for Younger Adults standard 40 CSP Core Standard 12 Level 2 National Occ. Standards in Care Unit CL1 Level 3 National Occ. Standards in Care Unit CL1 Level 3 National Occ. Standards in Prom. Ind. Unit CL1 1.3 NAfW NMS Care Homes for Older People standards 1.2 NAfW NMS Care Homes for Younger Adults 1.3 Level 2 National Occ. Standards in Care Unit CL1 Level 3 National Occ. Standards in Care Unit CL1 Level 3 National Occ. Standards in Prom. Ind. Units CL3,CL4 Welsh Health Circular(2002)020 The Health Service and the Welsh Language 1.4 NAfW NMS Care Homes for Older People standard 8 NAfW NMS Care Homes for Younger Adults standard 7,16,18 CSP Core Standard 2 CSP Service Standard 13 Creating a Unified and Fair System for Assessing and Managing Care Good practice in consent Health and Social Care Guide section 1,5,7 Level 3 National Occ. Standards in Care Units X12,X13,X19 Level 3 National Occ. Standards in Prom. Ind. Unit X13 NSF for Diabetes Standard 3 NMC Code of Professional Conduct sections 2,3 Welsh Assembly Government Reference Guide for Consent to Examination or Treatment Welsh Health Circular (2002) 42 Welsh Risk Management Standard 9 10 1 2 3 Fundamentals Indicator Corresponding Standards 1.5 Code of Ethics and Professional Conduct for Occupational Therapists Sections 2.5, 3.4 NAfW NMS Care Homes for Older People standards 7,8,12 NAfW NMS Care Homes for Younger Adults standard 8,10 CSP Core Standard 15 CSP Service Standard 19 Creating a Unified and Fair System for Assessing and Managing Care Health and Social Care Guide section 1 Independent Healthcare D.O.H. Standard m 3 Level 2 National Occ. Standards in Care Unit CU5 Level 3 National Occ. Standards in Care Unit CU5 Level 3 National Occ. Standards in Prom. Ind. Unit CU5 NMC Code of Professional Conduct sections 4,5 Welsh Risk Management Standard 7 1.6 NAfW NMS Care Homes for Older People standard 32 NAfW NMS Care Homes for Younger Adults standard 36 CSP Core Standard 12 Health and Social Care Guide section 8 Level 2 National Occ. Standards in Care Unit CL1 Level 3 National Occ. Standards in Care Unit CL1 Level 3 National Occ. Standards in Prom. Ind. Unit CL1 1.7 NAfW NMS Care Homes for Older People standard 31,32 NAfW NMS Care Homes for Younger Adults standard 35,36 CSP Service Standard 5 Health and Social Care Guide section 8 Improving Health in Wales chapter 3 Level 3 National Occ. Standards in Care Unit NC10 Level 3 National Occ. Standards in Prom. Ind. Units NC10,Z2 Welsh Risk Management Standard 4 All of the references to the National Occupational Standards are guides as to how meeting the standards contained in Fundamentals of Care can contribute evidence to part of the units identified. It is dependent on the nature and complexity of the task undertaken as to how much evidence will be generated. See footnote above See footnote above 11 Selected references Anonymous. (2002) Communication and listening skills, Nursing Times; 98(10) p 7-13. Audit Commission. (1993) What seems to be the matter? Communication between hospitals and patients. HMSO. British Deaf Association. Sign Language Policy. Head Office. Care Council. (2002) Codes of Practice for Social Care Workers. Available from: www.ccwales.org.uk Care Council. (2002) Induction Framework for Social Care. Available from: www.ccwales.org.uk Care Council. (1998) National Occupational Standards in Care Level 2 and 3 and Promoting Independence Level 3. Available from: www.ccwales.org.uk Chartered Society of Physiotherapy. (2000) Core standards. Available from: www.csp.org.uk Chartered Society of Physiotherapy. (2000) Service standards. Available from: www.csp.org.uk College of Occupational Therapists. (2000) Code of Ethics and Professional Conduct for Occupational Therapists. Hallstrom, I. And Elander, G. (2001) Needs during hospitalisation: definitions and descriptions made by patients, Nursing Ethics; 8(5) p409-18. Hemsley B. and Sigafoos J. and Balandin S. and Forbes R. and Taylor C. and Green VA. and Parmenter T. (2001) Nursing the patient with severe communication impairment, Journal of Advanced Nursing; 35(6) p827-35. Henderson A. and Zernike W. (2001) A study of the impact of discharge information for surgical patients, Journal of Advanced Nursing; 35(3) p435-41. Kutner, JS. And Steiner, JF. and Corbett, KK. and Jahnegen, D. and Barton, PL. (1999) Information needs in terminal illness, Social Science and Medicine; 48 (10) p1341-52. Laurent C. and Good Practice Network. (1999) Written for happy endings...how midwives improved patient education, Nursing Times; 95(48), Dec 1-7, p56-7. National Assembly for Wales. (2001) Improving health in Wales. Available at: www.wales.gov.uk/subihealth/content/keypubs/pdf/nhsplan-e.pdf. National Assembly for Wales. (2001) Regulations and national minimum standards for care homes for older people, care homes for younger adults and adult placements. National Assembly for Wales. (2001) Tackling coronary heart disease in Wales: implementing through evidence. Available from: www.wales.gov.uk/subihealth/content/keypubs/pdf/coronary-heart-disease-e.pdf 12 National Assembly for Wales. (2001) Ombudsman for Wales Annual Report. Welsh Administration Ombudsman and Health Service. Nessa J. and Malterud K. (1998) Tell me what’s wrong with me: a discourse analysis approach to the concept of patient autonomy, Journal of Medical Ethics; 24(6) p394-400. Nursing and Midwifery Council. (2002) Code of professional conduct. Available from: www.nmc-uk.org/cms/content/Publications Sowden, A. and Forbes, C. (2001) Patient information, Health Service Journal ; 1 Mar 2001, p.36-7. Welsh Assembly Government. (2002) Creating a unified and fair system for assessing and managing care. Welsh Assembly Government. (2002) Framework for best practice: the production and use of health information for the public. Welsh Assembly Government. (2002) Good practice in consent implementation guide: consent to examination or treatment. Available from: www.wales.gov.uk/subihealth/content/keypubs/pdf/impguide-e.pdf. Welsh Assembly Government. (2002) Health and social care guide for Wales. Welsh Assembly Government. (2002) National service framework for diabetes (Wales). Available from: www.wales.nhs.uk/sites/documents/334/diabetes-standards-wales.pdf. Welsh Assembly Government. (2002) Publication of guidance about consent for examination or treatment for the NHS in Wales. Welsh Assembly Government. (2002) Reference guide to consent for examination or treatment. Available from: www.wales.gov.uk/subihealth/content/keypubs/pdf/refguide-e.pdf. Welsh Assembly Government. (2002) Regulatory and national minimum standards for private and voluntary healthcare services. Welsh Assembly Government. (2002) Welsh Health Circular(2002)020. The Health Service and the Welsh Language. Welsh Assembly Government and Welsh Risk Pool. (2002) Welsh risk management standards. Available from: http://howis.wales.nhs.uk/wrp 13 2. Respecting people This aspect should underpin at all times, the relationship between someone who is receiving a service and the person or people delivering that service. Services should always be provided with compassion and empathy for the person to whom they are being delivered. All human beings – old or young, sick or well, have a right to dignity, privacy and informed choice. People also have a right to expect that these basic human rights will be respected by others, most especially those whose role is to provide a caring service. When people are dependent on others for any aspect of their care, the individual’s ability to ensure these basic human rights for themselves may be compromised. All those who provide care have a responsibility to ensure that whatever care they are providing includes attention to basic human rights. Where people are unable to ensure these rights for themselves, when they are unable to express their needs and wishes as a result of a sensory impairment, a mental health problem, learning disability, communication difficulty or for any other reason, access to independent advocacy services must be provided (see Indicator 2.2). While these rights are common to all human beings, every person is a unique individual with unique needs and wishes. Individual needs and wishes vary with factors such as age, sex, culture, religion and personal circumstances; also, people’s individual needs change over time. These individual needs may increase vulnerability to the loss of basic human rights. It is also important to understand that in exercising individual rights, people exercising those rights take responsibility for the choices they make. Respecting people as individuals is very broad and an integral part of all care. It is particularly important in: ● ● ● Personal care, including maintaining personal hygiene, going to the toilet, and intimate procedures (see Aspects 8 and 11). Communication and examination by health and social care staff (see Aspect 1). Caring for people who are dying or have died. Principle Basic human rights to dignity, privacy and informed choice must be protected at all times, and the care provided must take account of the individual’s needs, abilities and wishes. Practice Indicators 2.1 People are treated with respect, courtesy and politeness. Staff receive training to support this. 2.2 People are able to access free and independent advice so that they can make choices about their care and lifestyle. This may be provided through advocacy services or voluntary agencies such as the Citizen’s Advice Bureau. 2.3 Individuals are addressed by their preferred name. 2.4 Confidentiality and privacy are respected as far as possible, especially in hospital wards, public spaces and reception areas. 2.5 Mail is always given unopened unless otherwise requested. Where a person is unable to open their post, appropriate arrangements are made with their carers. 2.6 People’s feelings, needs and problems are actively listened to, acknowledged and respected. 14 2.7 Information and care are always provided with compassion and sensitivity. ● When a service user has asked you to read their mail, never leave it in a public place or open to view; always place back in an envelope and return to a place of safety, acceptable to the service user. ● Never touch the personal belongings of someone using services, without asking first, and always treat the belongings of others with care and respect. ● Never judge the appropriateness of the emotions that service users may express to you; accept that they are valid for the individual concerned and respond appropriately. ● If people are frightened, offer reassurance. ● If people are angry, listen to them and suggest courses of action that will resolve angry feelings. ● If people express sadness, they will need support in coming to terms with what they have lost or are about to lose. ● Never assume that you know what religious or cultural requirements a service user may have, always ask. ● Never gossip or laugh about people who use services to your colleagues; a service user will almost certainly be in a position of disadvantage when compared with yourself and should never become the butt of jokes and stories. ● If you are a manager of care providers, always model behaviour that reflects respect for others; modelling is a very powerful vehicle by which others can learn. 2.8 Spiritual and cultural needs are acknowledged and respected. Some examples of what the Indicators mean in practice ● Always make clear to your service user that what they have to say is important to you. ● Always demonstrate patience and understanding. ● Always knock the door if you are intending to enter a room occupied by someone using your service. ● Never raise your voice when communicating with your service user, unless this is in order to be heard by someone who has a hearing impairment. ● If a service user questions your actions or views on their care, do not take this personally; be ready to listen and learn from what they have to say. ● Always ask a person using services how they wish to be addressed. Never assume that it is acceptable to address a service user by their first name. ● ● Places such as hospital wards and office reception areas are very public. Always ensure that you are able to maintain confidentiality in such places, before discussing personal matters. Always check that a service user is comfortable discussing issues in busy environments before you start. Never open the personal mail of someone using your services unless they have requested that you do so. 15 Cross references Fundamentals Indicator Corresponding Standards Principle Code of Ethics and Professional Conduct for Occupational Therapists Section 2 NAfW NMS Care Homes for Older People standard 14 NAfW NMS Care Homes for Younger Adults standards 16,18 Health and Social Care Guide section 1 Human Rights Act (1998), Articles 2,3,8,9, 14 Level 2 National Occ. Standards in Care Unit 01 Level 3 National Occ. Standards in Care Unit 02 Level 3 National Occ. Standards in Prom. Ind. Unit 02 NMC Code of Professional Conduct section 2 Race Relations Act (1976) Sex Discrimination Act 1975 (amended 1986) Social Care Induction Framework Core Areas 1.1,1.2 2.1 CSP Core Standard 1 Independent Healthcare D.O.H. Standard c8 m6 Level 2 National Occ. Standards in Care Unit 01 Level 3 National Occ. Standards in Care Unit 02 Level 3 National Occ. Standards in Prom. Ind. Unit 02 2.2 CSP Core Standard 1 Level 3 National Occ. Standards in Care Unit Y2 Level 3 National Occ. Standards in Prom. Ind. Units Z2,Y2,NC10,SNH3U3 2.3 NAfW NMS Care Homes for Older People standard 14 NAfW NMS Care Homes for Younger Adults standards 16,18 CSP Core Standard 1 Level 2 National Occ. Standards in Care Unit CL1 Level 3 National Occ. Standards in Care Unit CL1 Level 3 National Occ. Standards in Prom. Ind. Unit CL1 2.4 NAfW NMS Care Homes for Older People standard 12 NAfW NMS Care Homes for Younger Adults standard 10 CSP Core Standards 1,3 Level 2 National Occ. Standards in Care Unit 01 Level 3 National Occ. Standards in Care Unit 02 Level 3 National Occ. Standards in Prom. Ind. Unit 02 2.5 NAfW NMS Care Homes for Younger Adults standard 16 Level 2 National Occ. Standards in Care Units CU5,W2 Level 3 National Occ. Standards in Care Unit CU5 Level 3 National Occ. Standards in Prom. Ind. Unit CU5 16 Fundamentals Indicator Corresponding Standards 2.6 Independent Healthcare D.O.H.Standard c14 Level 2 National Occ. Standards in Care Unit CL1 Level 3 National Occ. Standards in Care Unit CL1 Level 3 National Occ. Standards in Prom. Ind. Unit CL1 2.7 Level 2 National Occ. Standards in Care Unit CL1 Level 3 National Occ. Standards in Care Unit CL1 Level 3 National Occ. Standards in Prom. Ind. Unit CL1 2.8 CSP Core Standard 1 Level 2 National Occ. Standards in Care Unit 01 Level 3 National Occ. Standards in Care Unit 02 Level 3 National Occ. Standards in Prom. Ind. Unit 02 Selected references Care Council. (2002) Codes of Practice for Social Care Workers. Available from: www.ccwales.org.uk Care Council. (2002) Induction Framework for Social Care. Available from: www.ccwales.org.uk Care Council. (1998) National Occupational Standards in Care Level 2 and 3 and Promoting Independence Level 3. Available from: www.ccwales.org.uk Chartered Society of Physiotherapy. (2000) Core standards. Available from: www.csp.org.uk College of Occupational Therapists. (2000) Code of Ethics and Professional Conduct for Occupational Therapists Coyle, J. and Williams B. (2001) Valuing people as individuals: development of an instrument through a survey of person-centredness in secondary care, Journal of Advanced Nursing; 36(3) p450-9. Davies, S. and Brown, J. and Wilson, F. and Nolan, M. (2000) Dignity on the ward; promoting excellence in care, Nursing Times; 96(33) p 37-9. Department of Health. (2001) Independent Healthcare. Available from: www.doh.gov.uk/ncsc/independenthealthcare.pdf. Department of Health. (2001) National Service Framework for Older People. Available from: www.doh.gov.uk/nsf/pdfs/nsfolderpeople.pdf (PDF format) or www.doh.gov.uk/nsf/frameup/contents_.html (HTML format). Dimond B. (1999) Confidentiality 1: Nurses’ duty to respect patient confidentiality, British Journal of Nursing; 8(9) May 13-26, p 560,562. 17 G.B. Parliament. (1998) Human Rights Act 1998. HMSO. Available from: www.hmso.gov.uk/acts/acts1998/19980042.htm. G.B. Parliament. (1976) Race Relations Act 1976. HMSO. Available from: www.homeoffice.gov.uk/raceact/racerel1.htm. G.B. Parliament. (1975) Sex Discrimination Act 1975. HMSO. Kerish, K. (2000) Individual care: its conceptualisation and practice within a multi-ethnic society, Journal of Advanced Nursing; 31(1) p91. Lothian, K. and Philp, I. (2001) Maintaining the dignity and autonomy of older people in the healthcare setting: care of older people, British Medical Journal; 322(7287) p668-70. National Assembly for Wales. (2001) Regulations and national minimum standards for care homes for older people, care homes for younger adults and adult placements. National Assembly for Wales. (2001) Tackling coronary heart disease in Wales: implementing through evidence. Available from: www.wales.gov.uk/subihealth/content/keypubs/pdf/coronary-heart-disease-e.pdf Nursing and Midwifery Council. (2002) Code of professional conduct. Available from: www.nmc-uk.org/cms/content/Publications The orders of St. John’s Trust, Help the Aged. (1999) Dignity on the Ward Promoting Excellence in Care. University of Sheffield. van Thiel GJM. and van Delden, JJM. (2001) The principle of respect for autonomy in the care of nursing home residents, Nursing Ethics: an International Journal for Health Care Professionals; 8(5) p419-31. Welsh Assembly Government. (2002) Creating a unified and fair system for assessing and managing care. Welsh Assembly Government. (2002) Health and social care guide for Wales. Welsh Assembly Government. (2002) National service framework for diabetes (Wales). Available from: www.wales.nhs.uk/sites/documents/334/diabetes-standards-wales.pdf. Woogara, J. (2001) Human rights and patients’ privacy in UK hospitals, Nursing Ethics: an International Journal for Health Care Professionals; 8(3) p234-46. 18 3. Ensuring safety This aspect of care includes the health, safety and welfare of service users, who have the right to a safe environment, use of appropriate and adequately maintained equipment, and protection against abuse. The safety of people at work and service users who come into contact with the environment in which care is provided, is governed by the Health and Safety at Work Act 1974, and its various safety regulations. Obligations under this legislation include the requirement for appropriate training, documentation and investigation of accidents and untoward incidents. The way in which these requirements are put into practice varies greatly and poses particular challenges for some groups of patients, clients and service users in their own homes. This principle applies to all care settings and all client groups, but the relevance of the individual indicators will vary according to location and client group. Balancing the needs of both staff and service users can be difficult in individual circumstances. For example a heavy immobile person may ask to be moved without the use of lifting equipment which is necessary to protect the carer from back injury. Protection from falls potentially places unacceptable limits on the person’s freedom and autonomy. Sometimes the wishes of the cared-for person conflict with those of his/her family or other carers. At no time should the wishes of the person being cared for put at risk the safety of others. Health and Safety legislation requires that a risk assessment is carried out which involves the careful consideration of what could cause harm, and what precautions need to be taken to prevent accident and injury to either the person receiving care or the care giver. If a person’s safety is put at risk at any time, a record must be made and reviewed by the person or organisation providing care. This relates to all accidents, injuries, falls, medication errors, infections, untoward incidents and near misses. This aspect of care covers: ● Maintenance of a safe physical environment. ● Protection from physical, verbal, sexual and financial abuse. ● Safe working practices. ● Prevention of falls. ● Prevention of infection. ● Prevention from self-harm. ● Prevention of treatment errors. Principle People’s health, safety and welfare must be actively promoted and protected. Risks must be identified, monitored and where possible, reduced or prevented. Practice Indicators 3.1 People receive support free from abuse, neglect and inappropriate care. 3.2 People are protected against verbal, physical, sexual and financial abuse. 3.3 The service user’s environment is clean, properly maintained, safe and secure. Their independence and personal choice are respected. 3.4 Equipment is clean, properly maintained and stored safely. 3.5 People are assessed for risks to their own safety and the safety of others. A plan for managing risk is agreed between the person being cared for and those caring for them. 3.6 Staff receive appropriate information, training and supervision to ensure that people and their carers are safe. 19 This relates to moving skills, use of equipment, abusive and challenging behaviour, medication, first aid, infection control, waste disposal, handling of valuables and general security. 3.7 People are encouraged to develop or maintain the level of independence they wish, striking a responsible balance between risk and safety. 3.8 People are able to summon help easily at all times, using a telephone, bell or other convenient means. If unable to do so their needs will be checked regularly. mentally infirm may become more confused by change. ● If, as a provider of services, you use equipment to do your job, check that it is properly maintained and in good working order before embarking on your day’s tasks. ● Never leave the flex to appliances in places where a service user may trip over it. ● If you are concerned that a service user is making a choice related to their need, which may place them at risk, ensure that you discuss this with them, record both their decision and your view and ensure that your supervisor or manager is aware of your concerns. ● If you believe that you are not adequately trained to undertake specific tasks safely, you should bring this to the attention of your supervisor or manager. ● Make sure that you are fully aware of procedures in your organisation to protect vulnerable adults; if you believe that a service user is being abused or neglected, implement your local procedures immediately. Some examples of what the indicators mean in practice ● Always practise basic personal hygiene, both for yourself, and the person for whom you are caring. ● If you are caring for service users in their own homes, always ensure that appliances have been switched off where appropriate. ● Always ensure that open fires are left safely and guarded, with nothing close to them that may catch alight. ● Never move a service user’s furniture without seeking their agreement; partially sighted people may stumble as a result of the unexpected and the 20 Cross references Fundamentals Indicator Corresponding Standards Principle Code of Ethics and Professional Conduct for Occupational Therapists Section 2 Level 2 National Occ. Standards in Care Units 01,CU1,CU4 Level 3 National Occ. Standards in Care Units 02,CU1 Level 3 National Occ. Standards in Prom. Ind. Units 02,CU1 Social Care Induction Framework Core Areas 1.1,2.1,2.2,2.3,2.4,2.5,2.6,4.2 3.1 NAfW NMS Care Homes for Older People standards 30,32 NAfW NMS Care Homes for Younger Adults standard 36 In Safe Hands Level 2 National Occ. Standards in Care Unit Z1 Level 3 National Occ. Standards in Care Unit Z1 Level 3 National Occ. Standards in Prom. Ind. Units Z1,Z18 NMC Code of Professional Conduct section 8 3.2 NAfW NMS Care Homes for Older People standards 30,32 NAfW NMS Care Homes for Younger Adults standard 36 In Safe Hands Level 2 National Occ. Standards in Care Unit Z1 Level 3 National Occ. Standards in Care Unit Z1 Level 3 National Occ. Standards in Prom. Ind. Units Z1,Z18 NMC Code of Professional Conduct section 8 3.3 NAfW NMS Care Homes for Older People standards 18,33,40 NAfW NMS Care Homes for Younger Adults standard 33,37,41 CSP Core Standard 16 CSP Service Standards 2,16 Level 2 National Occ. Standards in Care Units 01,CU3,CU1 Level 3 National Occ. Standards in Care Units O2,CU1 Level 3 National Occ. Standards in Prom. Ind. Units O2,CU1 NMC Code of Professional Conduct section 8 Patient Safety First Welsh Risk Management Standards 13,22,27,33,35 21 Fundamentals Indicator Corresponding Standards 3.4 NAfW NMS Care Homes for Older People standard 18 NAfW NMS Care Homes for Younger Adults standard 33 Independent Healthcare D.O.H. Standard c20 Level 2 National Occ. Standards in Care Units CU1,CU6 Level 3 National Occ. Standards in Care Unit CU1 Level 3 National Occ. Standards in Prom. Ind. Unit CU1 Welsh Risk Management Standards 14,30 3.5 NAfW NMS Care Homes for Older People standard 32 NAfW NMS Care Homes for Younger Adults standard 36 Creating a Unified and Fair System for Assessing and Managing Care CSP Core Standard 16 CSP (2001) Effectiveness of falls prevention and rehabilitation strategies in older people: implementation for physiotherapy & Falls audit pack CSP Service Standard 2 Level 2 National Occ. Standards in Care Unit CU1 Level 3 National Occ. Standards in Care Unit CU1 Level 3 National Occ. Standards in Prom. Ind. Unit CU1 Welsh Risk Management Standard 13 3.6 NAfW NMS Care Homes for Older People standards 17,18 NAfW NMS Care Homes for Younger Adults standards 20,33 CSP (2002) Guidance in Manual Handling for Chartered Physiotherapists CSP Service Standard 16 Level 3 National Occ. Standards in Care Unit CU7 Level 3 National Occ. Standards in Prom. Ind. Unit CU7 Welsh Risk Management Standard 14 3.7 Independent Healthcare D.O.H. Standard m 12 Creating a Unified and Fair System for Assessing and Managing Care Level 3 National Occ. Standards in Care Unit Y5 Level 3 National Occ. Standards in Prom. Ind. Unit Y5 NSF for Diabetes Standard 3 3.8 NAfW NMS Care Homes for Older People standard 36.8 NAfW NMS Care Homes for Younger Adults standard 40 CSP Core Standard 16 22 Selected references Care Council. (2002) Codes of Practice for Social Care Workers. Available from: www.ccwales.org.uk Care Council. (2002) Induction Framework for Social Care. Available from: www.ccwales.org.uk Care Council. (1998) National Occupational Standards in Care Level 2 and 3 and Promoting Independence Level 3. Available from: www.ccwales.org.uk Chartered Society of Physiotherapy. (2000) Core standards. Available from: www.blindtiger.co.uk/CSP/uploads/-38c9a362-ed71ce5fa5—7696/SOPPcore.pdf. Chartered Society of Physiotherapy. (2001) Effectiveness of falls prevention and rehabilitation strategies in older people: implementation for physiotherapy & Falls audit pack. Available from: www.blindtiger.co.uk/CSP/uploads/-37e5051b-ed0281cb81—7ffa/fallsEBB.doc. Chartered Society of Physiotherapy. (2002) Guidance in Manual Handling for Chartered Physiotherapists. Available from: www.blindtiger.co.uk/CSP/uploads/-38c9a362-ed71ce5fa5—77d7/GIMH4CP.pdf. Chartered Society of Physiotherapy. (2000) Service standards. Available from: www.csp.org.uk College of Occupational Therapists. (2000) Code of Ethics and Professional Conduct for Occupational Therapists. Department of Health. (2001) Independent healthcare. Available from: www.doh.gov.uk/ncsc/independenthealthcare.pdf. Department of Health. (2001) National service framework for older people a digest. Pfizer. H.S.M.E. (2000) Health and safety manual. Health and safety risk assessment policy/procedure. H.S.M.E. (2000) Health and safety manual. Management of manual handling policy. Medical Devices Agency. (2001) Equipped to care: the safe use of medical devices in the 21st century. Available from: www.medical-devices.gov.uk. Mitchell, P. (2002) Nursing essential to improving patient safety, Journal of Advanced Nursing; 38(2) p109-10. National Assembly for Wales. (2001). Regulations and national minimum standards for care home for older people, care homes for younger adults and adult placements. 23 National Institute for Clinical Excellence. (2001) Scope for the development of a clinical guideline on the assessment and prevention of falls in older people. Available from: www.nice.org.uk/article.asp?a=30591. National Patient Safety Agency. (2001) Doing less harm. Available from: www.npsa.org.uk/admin/publications/docs/draft.pdf. National Patient Safety Agency. (Forthcoming) Patient Safety First. Nursing and Midwifery Council. (2002) Code of professional conduct. Available from: www.nmc-uk.org/cms/content/Publications Parker, LJ. (1999) Managing and maintaining a safe environment in the hospital setting, British Journal of Nursing; 8(16) p1053-4, 1056, 1058 passim. Pennels, C. (2001) Practical ways of putting safety first, Professional Nurse; 16(7 Suppl) pS7. Sowden A, Dickson R. (1996) Preventing Falls and further injury in older people, Nursing Standard; vol.10 (47) p32-33. Welsh Assembly Government. (2002) Creating a unified and fair system for assessing and managing care. Welsh Assembly Government. (2000) In safe hands. Welsh Assembly Government. (2002) National service framework for diabetes (Wales). Available from: www.wales.nhs.uk/wrp Welsh Assembly Government and Welsh Risk Pool. (2002) Welsh Risk Management Standards. Available from: http://howis.wales.nhs.uk/wrp Wilson, P. (1998) Safe patient transportation: nurses can make a difference, Nursing Times; 94(26) p66-7. Wilson, T. and Smith, F. and Lakhani, M. (2002) Patient safety in primary healthcare – an overview of current developments in risk mangement and implications for clinical governance, Journal of Clinical Governance; 10(1) p25-30. 24 4. Promoting independence 4.5 Equipment provided for a specific person is kept for their own use. Most people do not want to be dependent on others and want to optimise their independence as quickly as possible. Maintaining independence improves quality of life and maximises physical and emotional well being. 4.6 To promote people’s independence and ability to care for themselves, their environment is as accessible, comfortable and safe as possible, in accordance with their wishes. The expectations of staff, carers and others of what an individual can achieve are often clouded by the assumption that dependency is permanent or inevitable. For example, an individual may not regain their mobility because the expectation of other people may be inappropriately low. This example highlights the need to work with individual strengths and potential. It needs to be recognised, however, that teaching and supporting individuals in this way may take more time and greater skill than simply doing things for them. 4.7 People are encouraged to be active, through work, taking appropriate exercise and/or recreation as far as their condition allows. Some examples of what the Indicators mean in practice ● Always take the time to help individual service users to do things for themselves, or with your support, if they are able. ● Helping someone to do things for themselves will often take longer than if you were to do it for that person; always exercise patience and encouragement. ● If you are aware of aids or equipment that may help your service user maintain their independence, discuss these with them. ● If you believe access to a property or a property itself can be modified in a way that will further promote independence, bring this to the attention of your service user, line manager and the appropriate section of the Local Authority. ● Promoting people’s independence is a national policy; if you believe that the time allocated to you is insufficient, raise this with your supervisor or line manager. Principle The care provided must respect the person’s choices in making the most of their ability and desire to care for themself. Practice Indicators 4.1 Time is available to support and encourage people to care for themselves. 4.2 Ongoing assessment, involving all those relevant to the person’s care, forms the basis of the plan of activities and care. This takes account of the person’s requirements, strengths, abilities and potential. 4.3 Where possible, people are shown different ways of doing things to help them to be independent. Staff refer to physiotherapists or occupational therapists for specialist advice. 4.4 If appropriate, people are offered equipment to help them walk, move, eat, hear and see. This equipment is well maintained. 25 ● ● For some service users, doing things for themselves will challenge their self-confidence; take time to encourage and reassure; encourage small steps forward that are achievable. ● Always see a desire to be active as a positive sign; take appropriate steps to encourage it. ● If you are a commissioner of care services, ensure that the likely cost of working with an individual to maximise independence is included in your calculation when costing packages of care. Family members of the service user may be very worried about the taking of risks. Offer explanation, reassurance and encouragement to the family. Cross references Fundamentals Indicator Corresponding Standards Principle Code of Ethics and Professional Conduct for Occupational Therapists Sections 2,3 Level 2 National Occ. Standards in Care Unit 01 Level 3 National Occ. Standards in Care Unit 02 Level 3 National Occ. Standards in Prom. Ind. Unit 02 Social Care Induction Framework Core Areas 1.1,2.1,4.2 4.1 NAfW NMS Care Homes for Younger Adults standard 18 Level 2 National Occ. Standards in Care Unit Z6 Level 3 National Occ. Standards in Care Unit Y4 Level 3 National Occ. Standards in Prom. Ind. Unit Y4 4.2 NAfW NMS Care Homes for Older People standard 2 NAfW NMS Care Homes for Younger Adults standard 2,7,16,18 CSP Core Standard 8 Independent Healthcare D.O.H. Standard a 11 Level 3 National Occ. Standards in Care Unit SC8 Level 3 National Occ. Standards in Prom. Ind. Unit SC8 NMC Code of Professional Conduct section 3 Creating a Unified and Fair System for Assessing and Managing Care NSF for Diabetes Standard 3 Tackling Coronary Heart Disease in Wales standard 2 26 Fundamentals Indicator Corresponding Standards 4.4 NAfW NMS Care Homes for Older People standards 2,36 NAfW NMS Care Homes for Younger Adults standards 2,18,40 CSP Core Standard 18 Health and Social Care Guide section 5 Level 2 National Occ. Standards in Care Units Z6,Z5 Level 3 National Occ. Standards in Care Unit X10 Welsh Risk Management Standards 13,30 4.5 Health and Social Care Guide section 5 4.6 NAfW NMS Care Homes for Older People standards 13,36 NAfW NMS Care Homes for Younger Adults standards 18,40 Level 2 National Occ. Standards in Care Unit CU1 Level 3 National Occ. Standards in Care Unit CU1 Level 3 National Occ. Standards in Prom. Ind. Unit CU1 4.7 NAfW NMS Care Homes for Older People standards 9,15.8 NAfW NMS Care Homes for Younger Adults standard 14 Level 2 National Occ. Standards in Care Units Z6,Z13 Level 3 National Occ. Standards in Care Units X10,X15 Level 3 National Occ. Standards in Prom. Ind. Unit X15 Tackling Coronary Heart Disease in Wales standard 1 Selected references Care Council. (2002) Codes of Practice for Social Care Workers. Available from: www.ccwales.org.uk Care Council. (2002) Induction Framework for Social Care. Available from: www.ccwales.org.uk Care Council. (1998) National Occupational Standards in Care Level 2 and 3 and Promoting Independence Level 3. Available from: www.ccwales.org.uk Chartered Society of Physiotherapy. (2000) Core standards. Available from: www.csp.org.uk Chesson, R. and Duthie, J. (2000) Staff attitudes to physiotherapy and activities in private nursing homes, Elderly Care; 12(1) p11-3. College of Occupational Therapists. (2000) Code of Ethics and Professional Conduct for Occupational Therapists. 27 Davies, S. and Ellis, L. and Laker, S. (2000) Promoting autonomy and independence for older people within nursing practice: an observational study, Journal of Clinical Nursing; 9(1) p127-36. Dent, V. (2002) Promoting independence in dementia care, Nursing & Residential Care; 2(12) p575-7. Department of Health. (2001) Independent healthcare. Available from: www.doh.gov.uk/ncsc/independenthealthcare.pdf. Eisemann, M. and Richter, J. (1999) Relationships between various attitudes towards selfdetermination in health care with special reference to an advance directive, Journal of Medical Ethics; 25(1) p37-41. Evans, G. (2001) Dealing with advance statements (Living Wills). Pembrokeshire & Derwen NHS Trust. Faulkner, M. (2001) Empowerment in policy and practice, Nursing Times; 97(22) p40-1. Gutteridge, T. (2000) Meeting a special need for confidence and independence, Journal of Dementia Care; 8(5) p24-5. Kennedy, A. and Rogers, A. (2001) Patient empowerment. Improving self-management skills: a whole systems approach, British Journal of Nursing; 10(11) p734-7. Laukkanen, P and Karppi, P and Heikkinen, E and Kauppinen, M. (2001) Coping with activities of daily living in different care settings, Age & Ageing; 30(6) p489-94. Lothian, K. and Philip, I. (2001) Maintaining the dignity and autonomy of older people in the healthcare setting: care of older people, British Medical Journal; 322(7287) p668-70. Mackenzie, A. (2001) Symposium on improving care of the elderly. Training to engage residents with dementia in activities, British Journal of Therapy & Rehabilitation; 8(11) p406-9. National Assembly for Wales. (2002) Consultation on Draft Regulations and Standards for Domiciliary Care Agencies. Available from: www.wales.gov.uk/subisocialpolicy/content/consultations/domiciliary/circular-letter-e.htm National Assembly for Wales. (2001) Regulations and national minimum standards for care homes for older people, care homes for younger adults and adult placements. National Assembly for Wales. (2001) Tackling coronary heart disease in Wales: implementing through evidence. Available from: www.wales.gov.uk/subihealth/content/keypubs/pdf/coronary-heart-disease-e.pdf Nursing and Midwifery Council. (2002) Code of professional conduct. Available from: www.nmc-uk.org/cms/content/Publications 28 Powell, J. and Bray, J. and Roberts, H. and Goddard, A. and Smith, E. (2000) Goal negotiation with older people in three day care settings, Health & Social Care in the Community; 8(6) p380-9. Rasmussen, BH. and Sandman, PO. (1998) How patients spend their time in a hospice and in an oncological unit, Journal of Advanced Nursing; 28(4) p818-28. Ryder, E. and Wiltshire, S. (2001) Understanding empowerment, Nursing Times; 97(32) p39. Welsh Assembly Government. (2002) Creating a unified and fair system for assessing and managing care. Welsh Assembly Government. (2002) Health and social care guide for Wales. Welsh Assembly Government. (2002) National service framework for diabetes (Wales). Available from: www.wales.nhs.uk/sites/documents/334/diabetes-standards-wales.pdf. Welsh Assembly Government and Welsh Risk Pool. (2002) Welsh risk management standards. Available from: http://howis.wales.nhs.uk/gsiteCW/home.cfm?orgid=287 29 5. Relationships Principle This principle applies to all care settings and client groups, but the relevance of the supporting Indicators may vary. People must be encouraged to maintain their involvement with their family and friends and develop relationships with others, according to their wishes. This aspect of care includes arrangements for people in hospital and in residential settings to receive visitors, arrangements for maintaining contacts with families and friends, and meeting the needs of people who are at risk of social isolation. This may be because they are being cared for a long way from their home, have restrictions placed on their freedom and movement (e.g. by the Mental Health Act), or have language/cultural barriers or sensory impairment. People can also be socially isolated in their own homes. The needs and wishes of carers, family, relatives and friends as advocates are very important. Staff should help facilitate these where ever possible. Most carers want to be as closely involved with their relative or friend as possible, and their contribution to care and their role as advocate when the cared-for person is unable or reluctant to express their own needs is very important. Occasionally, however, patients and clients do not want the same level of involvement from their family or friends, and in these circumstances the first responsibility of care staff is to respect the wishes of the cared-for person. Staff also need to respect the boundary around their relationships with those they care for. They must not enter into relationships that exploit people sexually, physically, emotionally, socially or in any other manner. They must not develop relationships which compromise their professional judgement and objectivity and/or give rise to advantageous or disadvantageous treatment of the person concerned.4 Practice Indicators 5.1 People are able to receive visitors within reasonable hours, sensitive to the needs of others. Consideration is given to the condition of the person. Where they are unable to make a decision for themselves regarding visitors, those close to that person should be consulted. Equally if a person wishes to restrict visiting at any time, staff support their decision. 5.2 A comfortable area such as a visitors’ room is available for private telephone calls or for people to spend time with relatives and friends. 5.3 People are encouraged and enabled to be part of the community. 5.4 The person decides how much their family and any informal carers are involved in their care. 5.5 If someone becomes critically ill, arrangements are made to ensure that a relative or friend can stay overnight, either in the same place or in local accommodation.5 5.6 People are offered support with verbal and written communication, particularly if separated from family and friends in their home culture or country of origin.6 5.7 People are put in touch with relevant voluntary organisations if they want them to provide a visiting service. 5.8 People are able to discuss their sexual health needs and are supported in planning to meet those needs. 30 Some examples of what the Indicators mean in practice ● Make sure that your “house rules” are as relaxed and open about receiving guests as they can be, particularly within the context of shared accom modation. Make sure these rules are readily available and easily understood. ● Always encourage service users to maintain their relationships with family and friends. ● Make private space available for private meetings of family and friends. ● Always be welcoming in your approach to visitors, showing courtesy and patience at all times. ● Encourage the use of the telephone for keeping in touch, by making it easily accessible and making any procedure for the payment of calls, easily understood. ● ● Sometimes your service user will want friends or family to help care for him or her by feeding or dressing for example. This sort of help should be encouraged, unless it would compromise the health and safety of your service user. If such help is not appropriate, you should explain why to both your service user and the friend or family member. ● If you are caring for someone from a different culture, take the time to find out from your service user, how links with their family and/or country of origin can be maintained. Your service user may ask you to get in touch with local community or spiritual leaders for example. Such contact should be welcomed and encouraged. ● Most localities have a range of voluntary organisations and community groups who provide befriending, visiting, good neighbour schemes and the like. If your service user asks to be put in touch with such groups, this should be encouraged. Most Social Services Departments have “directories” of such services; alternatively, the nearest Council for Voluntary Service should be able to help. ● If developing or maintaining relationships is a problem for your service user because of communication difficulties, find out what local services are available and get in touch with them. You may have services for people who are blind, deaf, dumb, learning disabled or speech impaired, available locally. ● People have a right to maintain their sexual relationships, or develop new ones so long as behaviour is appropriate in public and open spaces. If your service user wishes to maintain such an existing relationship, or develop a new relationship with a consenting partner, private, comfortable and appropriate space should be made available. This may include sharing a room for example. It may be that your service user expressly says that they do not wish family or friends to be involved in any way in their care; this wish should be respected. The situation will require you to deal tactfully but honestly with friends and family should they raise the matter with you. 31 ● Where such relationships are being maintained, or are developing, always ensure that the privacy and confidentiality of the relationship is maintained – it is nobody’s business apart from the people in the relationship. ● If you suspect that your service user is receiving attention that is upsetting to them because they are perhaps showing signs of distress following a 4 Derived from Code of Ethics and Professional Conduct for Occupational Therapists of the College of Occupational Therapists Arrangements only (and not reimbursement) This does not include the cost of postage and phone calls 5 6 visit, you should report this to your line manager and find gentle and tactful ways of encouraging your service user to talk to you about what is troubling them. Such matters are extremely sensitive: they cannot be ignored, but neither can they be managed in a tactless or aggressive way. It may be that the use of an advocate may be necessary in such circumstances. Cross references Fundamentals Indicator Corresponding Standards Principle Level 2 National Occ. Standards in Care Unit 01 Level 3 National Occ. Standards in Care Unit 02 Level 3 National Occ. Standards in Prom. Ind. Units 02,W5 Social Care Induction Framework Core Areas 1.1,2.1,3.1,4.2 5.1 NAfW NMS Care Homes for Older People standards 10, 34.2 NAfW NMS Care Homes for Younger Adults standards 13,15,39 Independent Healthcare D.O.H. Standard m 21 5.2 NAfW NMS Care Homes for Older People standards 10,14.3 NAfW NMS Care Homes for Younger Adults standards 13,15,18 Level 2 National Occ. Standards in Care Unit W2 5.3 NAfW NMS Care Homes for Younger Adults standard 13,15 Level 3 National Occ. Standards in Care Units Y3,Y5 Level 3 National Occ. Standards in Prom. Ind. Units Y3,Y5 5.4 NAfW NMS Care Homes for Younger Adults standard 15 Level 2 National Occ. Standards in Care Unit W2 5.5 NAfW NMS Care Homes for Older People standard 19.10 NAfW NMS Care Homes for Younger Adults standard 21 32 Fundamentals Indicator Corresponding Standards 5.6 Level 2 National Occ. Standards in Care Units W2,W8 Level 3 National Occ. Standards in Prom. Ind. Units W1,W5,W8 Welsh Risk Management Standards 8 5.7 NAfW NMS Care Homes for Older People standard 10 NAfW NMS Care Homes for Younger Adults standard 13 5.8 NAfW NMS Care Homes for Younger Adults standard 15 Level 3 National Occ. Standards in Prom. Ind. Unit W1 Selected references Bergbom, I. And Askwall, A. (2000) The nearest and dearest: a lifeline for ICU patients, Intensive & Critical Care Nursing; 16(6) p384-95. Care Council. (2002) Codes of Practice for Social Care Workers. Available from: www.ccwales.org.uk Care Council. (2002) Induction Framework for Social Care. Available from: www.ccwales.org.uk Care Council. (1998) National Occupational Standards in Care Level 2 and 3 and Promoting Independence Level 3. Available from: www.ccwales.org.uk Clarke, C. and Harrison, D. (2001) The needs of children visiting on adult intensive care units: a review of the literature and recommendations for practice, Journal of Advanced Nursing; 34(1) p61-8. Department of Health. (1997) A service on the edge: inspection report of social services for deaf and hard of hearing people. HMSO. Available from: www.doh.gov.uk/pdfs/ontheedge.pdf. Department of Health. (2001) Independent healthcare. Available from: www.doh.gov.uk/ncsc/independenthealthcare.pdf. Garnham, P. (2001) Understanding and dealing with anger, aggression and violence, Nursing Standard; 16(6) p37-42. Hupcey, JE. (2001) The meaning of social support for the critically ill patient, Intensive & Critical Care Nursing; 17(4) p206-12. Mayers, CA. (2000) Quality of life: priorities for people with enduring mental health problems, British Journal of Occupational Therapy; 63(12) p591-7. 33 National Assembly for Wales. (2001) Regulations and national minimum standards for care homes for older people, care homes for younger adults and adult placements. NHS Executive. (1999) Doubly disabled: equality for disabled people in the new NHS access to service. NHS Executive. Available from: www.info.doh.gov.uk/doh/point.nsf Priestley, M. (1999) How critical care nurses identify and meet the needs of visitors to intensive care units, Nursing in Critical Care; 4(1) p27-33. Thomas, R. (2001) Patients’ perceptions of visiting: a phenomenological study in a specialist palliative care unit, Palliative Medicine; 15(6) p499-504. Ward, D. (2000) Clinical. Infection control: reducing the psychological effects of isolation, British Journal of Nursing; 9(3) p162, 164-70. Welsh Assembly Government and Welsh Risk Pool. (2002) Welsh risk management standards. Available from: http://howis.wales.nhs.uk/gsiteCW/home.cfm?orgid=287 White, E. and Barnitt, R. (2000) Empowered or discouraged? A study of people with learning disabilities and their experience of engaging in intimate relationships, British Journal of Occupational Therapy; 63(6) p270-6. 34 6. Rest and sleep Sleep is essential for good health and recovery from illness. Most people develop a personal balance between sleep, rest, exercise and activity which meets their individual needs. A change in health or environment can disturb this balance, and service users often complain that they are unable to get enough sleep. People may be embarrassed about sleeping surrounded by strangers, or may be disturbed by the behaviour of others. Inadequate sleep at night may be reflected in sleeping during the day, which may in turn exacerbate the difficulty of sleeping at night. People have altered sleep patterns for many reasons. It is important to note that lack of sleep can cause people to change their behaviour, in turn affecting their quality of life. For people in hospital the most common problem is getting enough sleep as they are disturbed by the ward activities and routines. For people in residential care, the emphasis may be on providing appropriate and stimulating daytime activity. This aspect applies to all settings and all client groups, but the relevance of the Supporting Indicators will vary according to the care setting and the client group. Principle Consideration is given to people’s environment and comfort so that they may rest and sleep. 6.3 Waking, sleeping and resting times are as flexible as possible to meet people’s needs and preferences. 6.4 Where beds and bedding are provided, efforts are made to ensure the person’s comfort. 6.5 If a person’s sleep is disturbed, they are made comfortable and offered the support they need. This could include sleep management and relaxation techniques. Care should be taken to guard against the danger of inappropriate medication. Some examples of what the indicators mean in practice ● Although organisation is important in shared care settings such as hospital wards and care homes, always remember that the service is being provided for the benefit of the people who require the service, not those providing it. ● The balance between sleep, rest and activity will be different for different people and their ability and motivation i.e. recovery will to some extent be dependent upon their individual needs being met. ● Private space for TV, conversation and visits should be made available, radios should all have earphones attached. ● Never assume that you know the conditions that promote sleep; always ask the person who is using your services. Sometimes some people may find shared accommodation preferable. ● Never assume that you know what the “right” balance of sleep, rest and activity is for people who use your services; always ask and take what measures are practical for meeting Practice Indicators 6.1 Noise is minimised and levels of heat, light and ventilation are controlled to help people sleep at night. 6.2 Televisions and radios in shared sleeping areas have earphones to enable individual listening. 35 ● ● individual need. Make sure that beds and bedding are of appropriate quality and always clean. ● If your service user complains of being uncomfortable, investigate the cause thoroughly and take appropriate action to remedy the situation. Sleeplessness is usually distressing. It is important that you respond with patience, tolerance and compassion; look for appropriate solutions to the problem and never voice irritation or annoyance. Cross references Fundamentals Indicator Corresponding Standards Principle Level 2 National Occ. Standards in Care Units 01,Z19 Level 3 National Occ. Standards in Care Unit 02 Level 3 National Occ. Standards in Prom. Ind. Unit 02 Social Care Induction Framework Core Areas 1.1,4.2,5.1 6.1 NAfW NMS Care Homes for Older People standard 39 NAfW NMS Care Homes for Younger Adults standard 37 Level 2 National Occ. Standards in Care Unit Z19 6.2 Level 2 National Occ. Standards in Care Unit Z19 6.3 Level 2 National Occ. Standards in Care Unit Z19 6.4 Level 2 National Occ. Standards in Care Unit Z19 6.5 Level 2 National Occ. Standards in Care Unit Z19 NSF for Older People:Medicines and Older People Selected references Brostrom, A. and Stromberg, A. and Dahlstrom, U. and Fridland, B. (2001) Patients with congestive heart failure and their conceptions of their sleep situation, Journal of Advanced Nursing; 34(4) p520-9. Care Council. (2002) Codes of Practice for Social Care Workers. Available from: www.ccwales.org.uk Care Council. (2002) Induction Framework for Social Care. Available from: www.ccwales.org.uk Care Council. (1998) National Occupational Standards in Care Level 2 and 3 and Promoting Independence Level 3. Available from: www.ccwales.org.uk 36 Church, L. and Davis, P. (1999) Sleep: the gentle healer, Journal of Orthopaedic Nursing; 3(Suppl.1) p53-8. Department of Health. (2001) National Service Framework for Older People: Medicines and Older People. Duxbury, J. (1994) Avoiding disturbing sleep in hospitals, Clinical Night Nursing, Nursing Standard; 9 (10) p31-4. Ersser, S. and Wiles, A. and Taylor, H. and Wade, S. and Walsh, R. and Bentley, T. (1999) The sleep of older people in hospital and nursing homes, Journal of Clinical Nursing; 8(4) p360-8. Hogg, G. (1998) Sleep deprivation in a high-dependency unit, Professional Nurse; 13(10) p693-6. National Assembly for Wales. (2001) Regulations and national minimum standards for care homes for older people, care homes for younger adults and adult placements. National Assembly for Wales. (2001) Tackling coronary heart disease in Wales: implementing through evidence. Available from: www.wales.gov.uk/subihealth/content/keypubs/pdf/coronary-heart-disease-e.pdf. Reid, E. (2001) Clinical. Factors affecting how patients sleep in the hospital environment, British Journal of Nursing; 10(14) p912-5. Southwell, M; Wistow, G. (1995) In-patient sleep disturbance; the views of staff and patients, Nursing Times; 91 (37) p29-31. 37 7. Ensuring comfort, alleviating pain This aspect of care includes basic requirements for being comfortable, such as being cool or warm enough, being in a comfortable position and experiencing appropriate levels of light and noise. Attention is also necessary to specific discomforts such as nausea or pain, which are almost always possible to control to an acceptable level for the individual service user. This aspect of care also includes emotional distress because psychological well-being is so vital to a person’s overall health. A person’s psychological state also affects their perception of pain. It must be remembered that pain and distress are what the person says they are and, to this end, the experience can be made worse by several factors such as: partnership with the person, should always be considered. Helping people to cope with chronic pain, discomfort and distress is a particular challenge and requires support from specialist services. When pain, distress or other specific symptoms are directly related to a physiological cause or a specific treatment process, advice from the appropriate agencies must be sought. This Principle applies to all care settings but the relevance of the supporting indicators will vary according to whether the person is receiving healthcare or social care and whether or not he/she is acutely ill or living with chronic pain or other symptoms caused by a particular disease. This aspect of care and the associated indicators do not include the specification of particular types of medication or other treatment for which specialist standards are available. Principle ● ● ● ● ● ● past experience; fear; anxiety; stress; distress; the environment in which the individual finds themselves i.e. their own home or a care setting. Levels of tolerance of pain and distress are unique and their expression should never be ignored, denied or dismissed by people who are not actually experiencing the feeling or symptom. Consideration must also be given to those persons who are unable to communicate their feelings of pain or distress. Those giving care need to be provided with adequate and appropriate education and training to allow them to recognise indicators of discomfort, pain and distress. People who are unable or unwilling to express themselves verbally, are also entitled to full assessment. Assessment with the family and carers, in People must be helped to be as comfortable and pain-free as their condition and circumstances allow. Practice Indicators 7.1 People are encouraged and given the opportunity to express pain, discomfort or emotional distress with support or assistance offered promptly. People’s personal environments and abilities to effectively communicate are also considered when discussing interventions that make them feel comfortable. 7.2 If a person needs special aids or equipment in order to maintain a comfortable position, these are provided and they are helped to use them correctly. 7.3 The person’s level of discomfort, pain or distress is assessed. A plan for controlling or relieving their pain or distress is agreed, taking into account their preferences. 38 It may be appropriate to use assessment tools to provide effective and appropriate treatment. Results of decisions are recorded for continuity of care. ● Always take the situation of your service user seriously; offer reassurance and prompt action. ● Ensure that you have taken all possible appropriate action to respond to the discomfort or distress of your service user. This may require that you call on specialist expertise e.g. GP, pain clinic or a specialist nurse. ● If a service user requests a review of their treatment regime, do not respond defensively to this, the fact that they have asked, reflects a) their confidence and b) their concern. Ensure that matters are discussed with them. ● Never assume that you know what your service user needs to be comfortable; always ask. 7.4 People have access to a range of appropriate pain relieving therapies and drugs in accordance with an assessment of their needs. 7.5 Specialist advice is sought if their symptoms or emotional distress are not controlled or relieved. Some examples of what the indicators mean in practice ● Make sure that your approach to your service user is always supportive and encouraging; if a person is experiencing pain or distress you need to know and the person needs to have the confidence to tell you. Cross references Fundamentals Indicator Corresponding Standards Principle Level 2 National Occ. Standards in Care Units 01,Z8,Z19 Level 3 National Occ. Standards in Care Unit 02 Level 3 National Occ. Standards in Prom. Ind. Unit 02 Social Care Induction Framework Core Areas 1.1,4.2 7.1 NAfW NMS Care Homes for Older People standard 19.2 NAfW NMS Care Homes for Younger Adults standard 21 Level 2 National Occ. Standards in Care Unit Z19 Welsh Risk Management Standard 7 7.2 NAfW NMS Care Homes for Older People standard 36 NAfW NMS Care Homes for Younger Adults standard 40 Level 2 National Occ. Standards in Care Unit Z19 7.3 Level 2 National Occ. Standards in Care Units Z8,Z19 Level 3 National Occ. Standards in Care Unit Z8 Level 3 National Occ. Standards in Prom. Ind. Unit Z8 39 Fundamentals Indicator Corresponding Standards 7.4 Level 2 National Occ. Standards in Care Unit Z19 7.5 Level 2 National Occ. Standards in Care Units Z8,Z19 Level 3 National Occ. Standards in Care Unit Z8 Level 3 National Occ. Standards in Prom. Ind. Unit Z8 Selected references Care Council. (2002) Codes of Practice for Social Care Workers. Available from: www.ccwales.org.uk Care Council. (2002) Induction Framework for Social Care. Available from: www.ccwales.org.uk Care Council. (1998) National Occupational Standards in Care Level 2 and 3 and Promoting Independence Level 3. Available from: www.ccwales.org.uk Field, L. and Adams, N. (2001) Pain management 2: the use of psychological approaches to pain, British Journal of Nursing; 10(15) p971-4. Hodges, C. (1998) Easing children’s pain, Nursing Times; 94(10) p55-6, 58. Hallström I. and Elander G. (2001) Needs during hospitalization: definitions and descriptions made by patients, Nursing Ethics: an International Journal for Health Care Professionals; 8(5):409-18. Howard, V. (2001) A holistic approach to pain, Nursing Times; 97(34) p34-5. McNair, H. (1999) Let’s put an end to pain, Nursing Times; 95(6) p36-7. McQuay, H. and Moore, A. and Justins, D. (1997) Fortnightly review: treating acute pain in hospital, British Medical Journal; 314(7093) p1531-5. Meeres, C. and McKenna, F. (2001) Dying with dignity, Nursing Times; 97(33) p36-7. Morrissey, T. (2001) Bereavement Policy. Pembrokeshire and Derwen NHS Trust. National Assembly for Wales. (2001) A review of palliative care services in Wales. Welsh Medical Committee. National Assembly for Wales. (2001) Regulations and national minimum standards for care homes for older people, care homes for younger adults and adult placements. Nichols K. (1993) Psychological Care in Physical Illness. Nelson Thornes. 40 O’Neill B. and Fallon M. (1997) ABC of palliative care: principles of palliative care and pain control, British Medical Journal; 315(7111) p801-4. Mann E. and Redwood S. (2000) Clinical. Improving pain management: breaking down the invisible barrier, British Journal of Nursing; 9(19) p2067-72. Regaard, A. (2000) Palliative care. The principles of pain management in advanced cancer, British Journal of Community Nursing; 5(8) p382-6, 388. Welsh Assembly Government. (2002) Adult Mental Health National Service Framework. Welsh Assembly Government and Welsh Risk Pool. (2002) Welsh risk management standards. Available from: http://howis.wales.nhs.uk/wrp Yonwin, H. (2000) Self-directed learning…helping the client to be as comfortable as possible, Nursing & Residential Care; 2(3) p140-3. 41 8. Personal hygiene, appearance and foot care Personal hygiene is important for the maintenance of good physical health e.g. the prevention of infection, for personal comfort (e.g. for feeling clean and cool) and for psychological reasons such as maintaining confidence and self-esteem. “Looking good“ makes an important contribution to “feeling good“ and is, therefore, a fundamental aspect of care and not just a matter of personal vanity. When people are able to care for themselves, personal hygiene habits are largely a matter of personal preference and choice, influenced by the individual’s culture and religion. When people receive this care from others, sensitivity to these same issues is important. The relevance of the supporting indicators will vary according to the location and peoples’ individual needs and preferences. It is important that toiletries are provided for people to meet their short term needs. However, it is also important that people are encouraged to have their own personal clothing, toiletries and equipment. Foot health is essential for maintaining good foot function, which can help to prevent falls (Principle 3) and is also an important part of ensuring comfort and alleviating pain (Principle 7). Neglect of foot health can lead to lack of independence (Principle 4) lack of mobility, (Principle 4) and the occurrence of ulceration and infection (Principle 12). Uncut toe nails alone are a common cause of discomfort. Nail cutting is normally part of personal hygiene. Disabling foot conditions can cause immobility and associated consequences – namely, isolation and its attendant psychological effects and dependence on others. Foot problems can result from a range of medical conditions. People with impaired circulation, who can include Diabetics, require assessment and/or care to the feet by State Registered Podiatrists. Principle People must be supported to be as independent as possible in taking care of their personal hygiene, appearance and feet. Practice Indicators 8.1 People’s personal hygiene, appearance and foot care are discussed with them and any assistance is based on their needs. 8.2 People are helped as necessary to keep their feet comfortable to enable them to be as mobile and independent as possible. 8.3 Facilities and equipment for all aspects of personal hygiene and appearance are accessible, clean and well maintained. This includes washing, shaving, bathing, the use of make-up, care of hair and nails, dressing and undressing. 8.4 Wash bowls and towels are provided for personal use as necessary. Toiletries are provided to meet any short-term needs. After use, bowls are promptly cleaned, dried and inverted for storage. 8.5 Care is discreet and sensitive, ensuring privacy. 8.6 People are referred to a State Registered Podiatrist / Chiropodist for assessment if they have a condition or illness which may require specialist foot care. A plan of care is then agreed with the person and their carer. 8.7 People are encouraged and helped to select, purchase and wear their own clothes and shoes. 8.8 Arrangements can be made for people’s clothes to be laundered and maintained. 42 Some examples of what the indicators mean in practice ● Never fail to recognise the importance of this aspect to most people; its denial can lead to poor morale, motivation and self-confidence. ● Always have available the basic requisites to maintain this aspect. ● Always ensure that items such as brushes, combs, facecloths etc. are kept for personal use, and hygienically maintained. ● ● Make sure that privacy is available for people whose personal needs are being attended to. Never make assumptions about personal preferences, always ask your service user and respect their wishes. ● The individual preferences of people using services e.g. the style in which they wish to wear their hair, or the way in which they wish make-up to be applied, are not subjects for informal chit-chat. Always treat people’s preferences with respect. ● Where purchase of clothes is concerned, wherever possible, your service user should be encouraged to choose his or her own clothes and accessories. ● Make sure that you always know to whom items of clothing belong. ● Your service user wearing someone else’s clothing is not acceptable. ● The clothes, accessories and toiletries of the person using your services should always be treated with the same respect as you would afford your own. Cross references Fundamentals Indicator Corresponding Standards Principle Level 2 National Occ. Standards in Care Units 01,Z9 Level 3 National Occ. Standards in Care Units 02,Y5 Level 3 National Occ. Standards in Prom. Ind. Units 02,Y5 Social Care Induction Framework Core Areas 1.1,4.2 8.1 NAfW NMS Care Homes for Older People standard 15 NAfW NMS Care Homes for Younger Adults standard 19 Level 2 National Occ. Standards in Care Unit Z9 NMC Code of Professional Conduct section 2 8.2 NAfW NMS Care Homes for Older People standard 15 NAfW NMS Care Homes for Younger Adults standard 19 8.3 NAfW NMS Care Homes for Older People standards 35,40 NAfW NMS Care Homes for Younger Adults standard 38 Level 2 National Occ. Standards in Care Unit Z9 Welsh Risk Management Standard 14 43 Fundamentals Standard Corresponding Standards 8.4 Level 2 National Occ. Standards in Care Unit Z9 8.5 NAfW NMS Care Homes for Older People standard 14.2 NAfW NMS Care Homes for Younger Adults standard 18 Level 2 National Occ. Standards in Care Unit Z9 8.6 NAfW NMS Care Homes for Older People standard 15.11 NAfW NMS Care Homes for Younger Adults standard 19.2 8.7 NAfW NMS Care Homes for Older People standard 14.4 NAfW NMS Care Homes for Younger Adults standard 18 Level 2 National Occ. Standards in Care Unit Y1 8.8 NAfW NMS Care Homes for Older People standard 14.4 NAfW NMS Care Homes for Younger Adults standard 18 Level 2 National Occ. Standards in Care Unit Y1 Selected references Care Council. (2002) Codes of Practice for Social Care Workers. Available from: www.ccwales.org.uk Care Council. (2002) Induction Framework for Social Care. Available from: www.ccwales.org.uk Care Council. (1998) National Occupational Standards in Care Level 2 and 3 and Promoting Independence Level 3. Available from: www.ccwales.org.uk Collins, F. (2001) Choosing bathing, showering and toileting equipment, Nursing & Residential Care; 3(10) p488-9. Department of Health. (2000) Care homes for older people, Care Standards Act 2000. Available from: www.doh.gov.uk/ncsc/carehomesforolderpeople.pdf. Ford, P. and McCormack, B. and Wills, T. and Dewing, J. (2000) Defining the boundaries: nursing and personal care, Nursing Standard; 15(3) p43-5. Jevon, P. and Jevon, M. (2001) Practical procedures for nurses: Face shaving, Nursing Times; 97(11) p43-4. National Assembly for Wales. (2001) Regulations and national minimum standards for care homes for older people, care homes for younger adults and adult placements. Nursing and Midwifery Council. (2002) Code of professional conduct. Available from: www.nmc-uk.org/cms/content/Publications 44 Welsh Assembly Government and Welsh Risk Pool. (2002) Welsh risk management standards. Available from: http://howis.wales.nhs.uk/wrp Whiller, J. and Cooper, T. (2000) Clean hands: how to encourage good hygiene by patients, Nursing Times; 96(46) p37-8. Whiting, LS. (1999) Maintaining patients’ personal hygiene, Professional Nurse; 14(5) p338-40. Yonwin, H. (2000) Self-directed learning…enabling clients to maintain their personal hygiene and appearance, Nursing & Residential Care; 2(5) p243-7. 45 9. Eating and drinking This aspect of care includes the choice, presentation, and availability of food, as well as helping those who need assistance to eat and drink. Proper nutrition, that is food and drink, is important for recovery from illness, for the healing of wounds and for good health. Food also plays an important social role. Missing meals, being unable to obtain snacks and drinks, and the lack of help for people who are unable to feed themselves are concerns wherever people are cared for. Some people have problems with chewing and swallowing food. This can sometimes be related to oral health (see Aspect 10) or a stroke. People cannot eat or drink properly if their mouth is sore, or if they have problems with their teeth or dentures. Proper nutrition can depend on food preferences. Choice of food is influenced by people’s cultural practices, religious beliefs and individual tastes. Staff should ensure that people are clear about what is achievable. 9.3 Food and drink are served in an acceptable setting. They are at the right temperature and attractively presented. 9.4 If a meal is missed, alternative food is offered and/or snacks and drinks can be accessed at any time. 9.5 Fresh drinking water is available at all times, except when restrictions are required as part of treatment. 9.6 People are provided with special diets in accordance with their medical needs. This also includes modified food. 9.7 If eating and/or drinking cause people difficulties, they receive prompt assistance, encouragement and appropriate aids or support. People with swallowing difficulties are assessed by a speech and language therapist and where necessary training in assisting people to swallow food or drink safely is given. Some examples of what the indicators mean in practice ● Always provide food of good nutritional quality, hygienically prepared and thoroughly cooked. ● Provide as much variety as is practicable for your service; always provide an alternative menu. ● Allow people time to eat their food without rushing. ● If your service user misses a meal or is not hungry at the mealtime, check regularly whether refreshment is required and offer it appropriately. ● Make sure food looks attractive on the plate and is of the right temperature; ensure that pride is taken in the presentation of the meal. Principle People must be offered a choice of food and drink that meets their nutritional and personal requirements and provided with any assistance that they need to eat and drink. Practice Indicators 9.1 People’s nutritional needs and physical ability to eat and drink are regularly assessed. If necessary, they are provided with specialist advice and support. 9.2 People are encouraged to eat nutritious, varied, balanced meals, hygienically prepared and served at regular times. 46 ● Make sure that fresh drinking water is always available. If you are unsure about how long water has been in a glass or jug, change it. ● Always tell your service user when you have refreshed their glass or mug and tell them where you have placed it. ● Inappropriate levels of nutrition and hydration can lead to rapid deterioration in frail, vulnerable people. If you have any worrying observations about your service user, report these and seek further advice. ● ● Always provide the direct help that people need in order to eat and drink. ● Never leave a drink out of the reach of your service user. As people approach the end of their lives, their willingness to eat and drink often becomes considerably less; very sensitive discussions will need to take place at such times; always report your concerns to your manager; always seek advice and call on specialist expertise whenever necessary; always ensure that concerns are discussed with family and relevant health and care staff in these circumstances. Cross references Fundamentals Indicator Corresponding Standards Principle Level 2 National Occ. Standards in Care Units 01,NC12 Level 3 National Occ. Standards in Care Unit 02 Level 3 National Occ. Standards in Prom. Ind. Unit 02 Social Care Induction Framework Core Areas 2.5,4.2 9.1 NAfW NMS Care Homes for Older People standard 15.9 NAfW NMS Care Homes for Younger Adults standard 19 and supplementary standard 17 Health and Social Care Guide section 5 Level 2 National Occ. Standards in Care Units NC12,NC13 NHS Nutrition and Catering Framework areas 9,10 Nutrition Strategy for Wales action 13 Welsh Risk Management Standard 23 9.2 NAfW NMS Care Homes for Older People standards 16,18.2,34.2 CSIW NMS Care Homes for Younger Adults standards 17,33,39 Health and Social Care Guide section 5 Level 2 National Occ. Standards in Care Unit NC13 NHS Nutrition and Catering Framework areas 3,11,12 Nutrition Strategy for Wales action 24 Tackling Coronary Heart Disease in Wales standard 1 Welsh Risk Management Standard 23 47 Fundamentals Indicator Corresponding Standards 9.3 NAfW NMS Care Homes for Older People standard 16 NAfW NMS Care Homes for Younger Adults standard 17 Level 2 National Occ. Standards in Care Unit NC12 NHS Nutrition and Catering Framework area 12 9.4 Health and Social Care Guide section 5 NHS Nutrition and Catering Framework area 11 Level 2 National Occ. Standards in Care Unit NC13 9.5 Nutrition Strategy for Wales action 24 9.6 NAfW NMS Care Homes for Older People standards 16.5,16.6 NAfW NMS Care Homes for Younger Adults standard 17 Level 2 National Occ. Standards in Care Units NC12,NC13 NHS Nutrition and catering Framework areas 9,10,11 9.7 NAfW NMS Care Homes for Older People standard 16.9 NAfW NMS Care Homes for Younger Adults standard 17 Health and Social Care Guide section 5 Level 2 National Occ. Standards in Care Unit NC12 NHS Nutrition and catering Framework area 12 Selected references Anderson, P. (2000) Tickling patients’ taste buds, Nursing Times; 96(50) p24-6. Barratt, J. (1999) Snacks as nutritional support in dementia care, Nursing Times; 95(32) p46-7. Bond, S. (1998) Eating matters – improving dietary care in hospitals, Nursing Standard; 12(17) p41-2. Brown, J. and Marland, G. (2002) Hydration in older people with mental health problems, Nursing Times; 98(3) p38-9. Care Council. (2002) Codes of Practice for Social Care Workers. Available from: www.ccwales.org.uk Care Council. (2002) Induction Framework for Social Care. Available from: www.ccwales.org.uk 48 Care Council. (1998) National Occupational Standards in Care Level 2 and 3 and Promoting Independence Level 3. Available from: www.ccwales.org.uk Clay M. (2000) Nutritious, enjoyable food in nursing homes, Elderly Care; 12(3) p11-6. Goldhill, MA. (2000) Clinical guideline: 1. Feeding critically ill patients, Care of the Critically Ill; 16(1) p20-1. Hamilton K. and Spalding D. and Steele C. and Waldron S. (2002) An audit of nutritional care delivered to elderly inpatients in community hospitals; Journal of Human Nutrition & Dietetics; 15(1) p49-58. Horan, D. and Coad, J. (2000) Can nurses improve patient feeding?, Nursing Times; 96(50) p33-4. Mitchell H. (1999) Nutrition audit at a community hospital, Journal of Human Nutrition & Dietetics; 12(5) p425-32. National Assembly for Wales. (2001) Regulations and national minimum standards for care homes for older people, care homes for younger adults and adult placements. National Assembly for Wales. (2001) Tackling coronary heart disease in Wales: implementing through evidence. Available from: www.wales.gov.uk/subihealth/content/keypubs/pdf/coronary-heart-disease-e.pdf NHS Estates. (2002) Better hospital food. Part of improving the patient experience. Available from: www.nhsestates.gov.uk/patient environment/content/food.html Steele, C. (1998) The links in the food chain…tailoring a menu to suit all patients’ clinical requirements, Nursing Standard; 12(49) p25-7. Welsh Assembly Government (2002) Diabetes National Service Framework Standards (Wales). Welsh Assembly Government. (2002) Health and social care guide for Wales. Welsh Assembly Government. (2002) Nutrition and catering framework. All-Wales Catering/Nutrition Group. Welsh Assembly Government. (2002) Nutrition Strategy for Wales Consultation Document. Welsh Assembly Government and Welsh Risk Pool. (2002) Welsh risk management standards. Available from: http://howis.wales.nhs.uk/wrp Wood, S. (1998) Full-service…nutritional aspects of nursing, Nursing Times; 94(32) p24-6. 49 10. Oral health and hygiene This aspect of care includes care of the mouth and teeth (including dentures). Although this is normally part of personal hygiene (see Principle 8) it is of particular importance for people who are ill or receiving long-term care and is therefore included separately here. Oral health is necessary for Eating and Drinking (Principle 9), and is also an important part of Ensuring Comfort, Alleviating Pain (Principle 7); neglect of oral health can also lead to infection (Principle 3). People who are unable to eat and drink normally, who are severely debilitated or unconscious, or who are receiving certain therapies e.g. radiotherapy, or certain drugs are especially vulnerable. The care, safety and security of an individual’s dentures are important to retaining dignity and maintaining nutrition; loss of dentures can affect quality of life (Principle 9: Eating and Drinking), Personal Appearance (Principle 8), and personal and social relationships (Principle 5). 10.2 People are encouraged and helped to care for their mouths with all procedures and routines explained in advance and support available when needed. 10.3 A toothbrush and toothpaste or denture brush and bowl are provided to meet shortterm needs. 10.4 If appropriate, people are able to have their dentures identified with their name in case they are lost and they are stored safely when not in use. 10.5 If someone has no teeth or dentures, they still receive support to ensure their mouth is comfortable and healthy. 10.6 If people have any specific problems with their mouth, teeth, dentures or gums, arrangements are made for them to see a dentist, if necessary in their own home. 10.7 People are offered appropriate check-up appoinments with a dentist in accordance with their needs. Some examples of what the indicators This Principle and most of its indicators apply mean in practice to all care settings and all client groups, but some are more relevant for people receiving long term care, others are especially important for people who are ill. Principle People must be supported to maintain healthy, comfortable mouths and pain-free teeth and gums, enabling them to eat well and prevent related problems. ● Oral health and hygiene is often not the most urgent of care needs. Never overlook it. ● Make time available to help support your service user in caring for their own oral hygiene if this is possible for them to do. ● Where this is not possible, ensure a regular routine for oral hygiene e.g. always clean away food from around the mouth when eating is finished. ● If specific procedures have been recommended as part of a treatment plan, always explain what you are going to do and why. Practice Indicators 10.1 Following assessment, a plan of care to keep the person’s mouth healthy and comfortable is agreed with them. For guidance on suitable assessment tools, please see the section Assessment tools below. 50 ● Make sure toothbrushes, toothpaste and bowls are available to people who need them and confined to personal use. ● Never allow your service user’s dentures to get mixed up with those of other people. ● If your service user complains of discomfort in their mouth, seek the advice of a dentist. Cross references Fundamentals Indicator Corresponding Standards Principle Level 2 National Occ. Standards in Care Units 01,Z9 Level 3 National Occ. Standards in Care Units 02,Y5 Level 3 National Occ. Standards in Prom. Ind. Units 02,Y5 Social Care Induction Framework Core Areas 1.1,4.2 10.1 NAfW NMS Care Homes for Older People standard 2 NAfW NMS Care Homes for Younger Adults standard 2 Level 2 National Occ. Standards in Care Unit Z9 10.2 NAfW NMS Care Homes for Older People standard 15.2 NAfW NMS Care Homes for Younger Adults standard 19 Level 2 National Occ. Standards in Care Unit Z9 10.3 Level 2 National Occ. Standards in Care Unit Z9 10.5 Level 2 National Occ. Standards in Care Unit Z9 10.6 NAfW NMS Care Homes for Older People standard 15.11 NAfW NMS Care Homes for Younger Adults standard 19.2 Level 2 National Occ. Standards in Care Unit Z9 10.7 NAfW NMS Care Homes for Older People standard 15.11 NAfW NMS Care Homes for Younger Adults standard 19.2 Level 2 National Occ. Standards in Care Unit Z9 51 Assessment tools Eilers J, Berger A, Peterson M. (1988). Development, testing and application of the oral assessment guide. Oncology Nursing Forum; 15(3) p325-330. Fiske J, Lewis D. (2001) BSDH Guidelines for the oral management of oncology patients requiring radiotherapy, chemotherapy and bone marrow transplantation. Journal of Disability and Oral Health; 2(1) p3-14. This contains an oral assessment tool and practical nursing oral care guidelines at the different stages of treatment. Griffiths J. (2002) Guidelines for oral health care for people with physical disability. Journal of Disability and Oral Health; 3(2) p51-58. This contains a simple assessment tool to identify clients who have oral and/or dental problems, are not receiving regular dental care and/or are at risk of poor oral health. Subjective indicators include the ability to speak, smile or eat without pain or discomfort. This example of an Oral Health Assessment may be adapted to suit any client group or used for self assessment. Griffiths J, Lewis D. (2002) Guidelines for the oral care of patients who are dependent, dysphagic or critically ill. Journal of Disability and Oral Health; 3(1) p30-33. This contains an oral assessment guide designed as a flow chart with practical guidance on techniques and materials. Rattenbury N, Mooney G, Bowen J. (1999) Oral assessment and care for inpatients. Nursing Times; 95(49) p52-53. Griffiths JE. (1996) Working with nurses who care for clients with cognitive impairment. International Dental Journal; Abstract A96 46(4) Supplement 2 p440. Griffiths JE, Williams J. (1998) Risk factors for oral health in neuro-psychiatric patients in a rehabilitation unit. Japanese Society of Dentistry for the Handicapped; Abstracts / Proceedings. Vol 19; Supplement. September p347. Selected references Age Concern. Dental Care and Older People. Factsheet 5. Available from: www.ageconcern.org.uk Alzheimer’s Society. (2001) Dental care and dementia. Arnold, C. and Brookes, V. and Griffiths, J. and Maddock, S. and Theophilou, S. (2000) Guidelines for oral health care for people with a physical disability. British Society for Disability and Oral Health. Available from: www.bsdh.org.uk/home/guidelines/physical.pdf. Blinkhorn, AS. (2002) The scientific basis of dental health education (4th ed). Health Development Agency. 52 Bowsher, J. and Boyle, S. and Griffiths, JA. (1999) A clinical effectiveness systematic review of oral care, Nursing Standard; 13(37) p31. Budtz-Jorgensen E, Mojon P, Rentsch A, Deslauriers N. Effects of an oral health programme on the occurrence of oral candidosis in a long-term care facility. Community Dental Oral Epidemiology 2000; 28(2) p141-149. Care Council. (2002) Codes of Practice for Social Care Workers. Available from: www.ccwales.org.uk Care Council. (2002) Induction Framework for Social Care. Available from: www.ccwales.org.uk Care Council. (1998) National Occupational Standards in Care Level 2 and 3 and Promoting Independence Level 3. Available from: www.ccwales.org.uk Davies, R. and Bedi, R. and Scully, C. (2000) ABC of oral health: oral health care for patients with special needs, British Medical Journal; 321(7259) p495-8. Department of Health. (2001) The essence of care. Available from: www.doh.gov.uk/essenceofcare/index.htm. Field, D. (1998) Practical procedures for nurses. Mouth care, Nursing Times; 94(7) insert 2p Fiske, J. and Griffiths, J. and Jamieson, R. and Manger, D. (2000) Guidelines for oral health care for long-stay patients and residents. British Society for Disability and Oral Health. Available from: www.bsdh.org.uk/home/guidelines/longstay.pdf. Fiske K, Lloyd HA. Dental needs of residents and carers in elderly people’s homes and carers’ attitudes to oral health. European Journal of Prosthodontic Restorative Dentistry 1992; 1 p91-95. Frenkel HF. Behind the screens: care staff observations on delivery of oral health care in nursing homes. Gerodontology 1999; 16(2) p75-80 Frenkel H, Harvey I, Newcombe RG. Oral health care among nursing home residents in Avon. Gerodontology 2000; 17(1) p33-38. Griffiths, J. and Jones, V. and Leeman, I. and Lewis, D. and Patel, K. and Wilson, K. (2000) Guidelines for the development of local standards of oral health care for dependent, dysphagic, critically and terminally ill patients. British Society for Disability and Oral Health. www.bsdh.org.uk/home/guidelines/depend.pdf. Griffiths, J. and Jones, V. and Leeman, I. and Lewis, D. and Patel, K. and Wilson, K. and Blankenstein, R. (2000) Oral health care for people with mental health problems guidelines and recommendations. British Society for Disability and Oral Health. Available from: www.bsdh.org.uk/home/guidelines/mental.pdf. 53 Heath R, Muller F, Lewis D, McKerlie R. Standards of dental care in residential homes: a Web Way Forward. Gerodontology 1999; 16(2) p123-125. Help the Aged. (2002) Oral health and older people. Imsand M, J-P Janssens, Auckenthaler R, Mojon P, Budtz-Jorgensen E. Bronchopneumonia and oral health in hospitalised older patients. Gerodontology 2002; 19(2) p66-72. Levine, RS. And Stillman, C. (2001) The scientific basis of dental health education: a policy document. NHS Health Development Agency. National Assembly for Wales. (2001) Regulations and national minimum standards for care homes for older people, care homes for younger adults and adult placements. Royal College of Surgeons of England and British Society for Disability and Oral Health. (2001) Clinical guidelines and integrated care pathways for the oral health care of people with learning disabilities. Available from: www.rcseng.ac.uk/dental/fds/pdf/icppld.pdf Royal College of Surgeons England, Dental Faculty. (2000) Guidelines on the management of oncology patients. Sumi Y, Miura H, Sunakawa M, Michiwaki Y, Sakagami N. Colonization of denture plaque by respiratory pathogens in dependent elderly people. Gerodontology 2002; 19(1) p25-29. Taylor GW, Loesche WJ, Terpenning MS. Impact of oral disease on systemic health in the elderly: diabetes mellitus and aspiration pneumonia. Journal of Public Health Dentistry 2000; 60(4) p313-320. Terpenning MS, Bradley SF, Wan JY, Chenoweth CE, Jorgensen KA, Kauffman CA. Colonozation and infection with antibiotic resistant bacteria in a long term care facility. Journal American Geriatric Society 1994; 42(10) p1062-1069. 54 11. Toilet needs This aspect of care is about bladder and bowel functions, which are a private and intimate part of people’s lives. Being dependent on the help of others for managing them often embarrasses people. This places a special responsibility on those providing care to acknowledge and respect these feelings, and to pay special attention to maintaining the person’s privacy and dignity (see Aspect 2). This Aspect of care includes taking people to the toilet, helping people to use bedpans, commodes, urinals and other special devices, helping them to manage their clothing, and clean and dry their skin. It focuses on the promotion and maintenance of continence. Specific procedures such as the management of catheters, stomas, administering suppositories, and the management of incontinence are outside the scope of these indicators. This principle and most of the indicators apply to all care settings and to all client groups, but the way in which they are put into practice will vary. For example in old buildings or in an individual’s own home some indicators (e.g. 11.1) may be difficult to achieve. For some people, for example those who are unable to walk, the problem is not managing their bladder and bowel functions but getting to and from the toilet; for others the problem is communicating or recognising their need. Principle Appropriate, discreet and prompt assistance must be provided when necessary, taking into account any specific needs and privacy. 11.2 A person who has difficulty in controlling their bladder or bowel functions is offered an assessment by a professional health worker and a plan of care is agreed. 11.3 Toilet facilities are clean and appropriately equipped with toilet paper, soap and fresh hand towels. 11.4 Toilet facilities shared by others have clear signs and provide privacy. 11.5 If required, people are helped to manage their bladder and bowel functions with privacy and dignity, maintaining their continence and giving them as much independence as possible. 11.6 If necessary, people are aware of and have easy access to methods for calling assistance. 11.7 Body waste is hygienically disposed of promptly, appropriately and with sensitivity. 11.8 People have access to hand washing facilities after using the toilet or equivalent equipment e.g. a commode. Particular attention is given to infection control. Some examples of what the indicators mean in practice ● Always respond to people’s need to toilet promptly. ● Never show irritation or annoyance whatever the circumstances. ● Always approach problems of incontinence with compassion and sensitivity; it is often the most demoralising aspect of frailty. ● Always ensure that dignity and privacy is maintained. ● Always ensure that toilets, commodes, Practice Indicators 11.1 People’s need of assistance to get to or use the toilet are assessed and if appropriate they are enabled to use the toilet (or commode) independently. 55 towels and the like, are as attractive as possible to use and never dirty or poorly maintained. ● Make sure that your service user has easy access to a means by which they can notify you of their needs. ● Never enter a room e.g. bathroom or toilet without knocking. ● ● Always ask your service user how they wish to be helped in dealing with their toileting needs – never make assumptions. Never leave commodes and the like either unemptied or on view – such practices compromise your service user’s dignity and right to privacy. ● Never leave bedpans or bottles on beds, lockers or floors. ● Always offer assessment where incontinence is an issue. ● Always ensure that your service user is clean and as comfortable as possible following toileting. Cross references Fundamentals Indicator Corresponding Standards Principle Level 2 National Occ. Standards in Care Units 01,Z11 Level 3 National Occ. Standards in Care Units 02,Z12 Level 3 National Occ. Standards in Prom. Ind. Units 02,Z12 Social Care Induction Framework Core Areas 1.1,4.2 11.1 NAfW NMS Care Homes for Older People standard 36 NAfW NMS Care Homes for Younger Adults standard 40 Level 2 National Occ. Standards in Care Unit Z11 Level 3 National Occ. Standards in Care Unit Z12 Level 3 National Occ. Standards in Prom. Ind. Unit Z12 11.2 NAfW NMS Care Homes for Older People standard 15.6 NAfW NMS Care Homes for Younger Adults standard 19 Level 3 National Occ. Standards in Care Unit Z12 Level 3 National Occ. Standards in Prom. Ind. Unit Z12 11.3 NAfW NMS Care Homes for Older People standards 35,36,40.1 NAfW NMS Care Homes for Younger Adults standards 38,40,41 Health and Social Care Guide section 5 Level 2 National Occ. Standards in Care Unit Z11 56 Fundamentals Indicator Corresponding Standards 11.4 Health and Social Care Guide section 5 Level 2 National Occ. Standards in Care Unit Z11 Level 3 National Occ. Standards in Care Unit Z12 Level 3 National Occ. Standards in Prom. Ind. Unit Z12 11.5 NAfW NMS Care Homes for Older People standard 14.2 NAfW NMS Care Homes for Younger Adults standard 18 Level 2 National Occ. Standards in Care Unit Z11 Level 3 National Occ. Standards in Care Unit Z12 Level 3 National Occ. Standards in Prom. Ind. Unit Z12 11.6 NAfW NMS Care Homes for Older People standard 36.8 NAfW NMS Care Homes for Younger Adults standard 40 Level 2 National Occ. Standards in Care Unit Z11 11.7 Level 2 National Occ. Standards in Care Unit Z11 Level 3 National Occ. Standards in Care Unit Z12 Level 3 National Occ. Standards in Prom. Ind. Unit Z12 Welsh Risk Management Standard 35 11.8 Level 2 National Occ. Standards in Care Unit Z11 Selected references Anonymous. (2000) Self-directed learning…access and use the appropriate toilet facilities, Nursing & Residential Care; 2(5) p243-7. Beresford SA. (1997) Combined toilets and bidets for use by people with a disability, British Journal of Therapy & Rehabilitation; 4(9) p481-2, 484-6. Cadd, A. and Keatinge, D. and Henssen, M. and O’Brien, L. and Parker, D. and Rohr, Y. and Schneider, J. and Thompson, J. (2000) Assessment and documentation of bowel care management in palliative care: incorporating patient preferences into the care regimen, Journal of Clinical Nursing; 9(2) p228-35. Care Council. (2002) Codes of Practice for Social Care Workers. Available from: www.ccwales.org.uk Care Council. (2002) Induction Framework for Social Care. Available from: www.ccwales.org.uk Care Council. (1998) National Occupational Standards in Care Level 2 and 3 and Promoting Independence Level 3. Available from: www.ccwales.org.uk 57 Collins, F. (2001) Choosing bathing, showering and toileting equipment, Nursing & Residential Care; 3(10) p488-9. Dean R. (1999) Considerations for bathroom equipment and adaptations, Nursing & Residential Care; 1(3) p164-6, 190-1. Department of Health. (1999) Guidance of continence services. Dowse, J. and Mackender, J. (2000) Back to basics: continence, Nursing Times; 96(30) p7-9. National Assembly for Wales. (2001) Regulations and national minimum standards for care homes for older people, care homes for younger adults and adult placements. Roe, B. and Whattam, M. and Young, H. and Dimond, M. (2001) Elders’ needs and experiences of receiving formal and informal care for their activities of daily living, Journal of Clinical Nursing; 10(3) p389-97. Royal College of Nursing. (1999) Commissioning continence advisory service RCN guide. Available from: www.rcn.org.uk/rcn_extranet/media/continence1410.pdf. Taylor-Cookson, J. and Mitchell, J. (2001) Toileting equipment for children with special needs, British Journal of Therapy & Rehabilitation; 8(9) p352-6. Welsh Assembly Government. (2002) Health and social care guide for Wales. Welsh Assembly Government. (2002) Nutrition and catering framework. All-Wales Catering/Nutrition Group. Welsh Assembly Government and Welsh Risk Pool. (2002) Welsh risk management standards. Available from: http://howis.wales.nhs.uk/wrp Willis, J. (2000) Bowel management and consent, Nursing Times; 96(6 Ntplus) p7-8. 58 12. Preventing pressure sores Current literature refers to pressure “ulcers”. However for the purpose of this document the term “sore” has been used, following extensive public consultation. A pressure sore is a breakdown of the skin and underlying tissue, which occurs, usually over bony areas such as the sacrum, buttocks, heels, shoulders, and elbows, as a result of unrelieved pressure, shear or friction. Anyone whose mobility is limited by being confined to a bed or chair because of injury, illness or frailty, including those with mental health needs or a learning disability, is vulnerable. There is even a risk to those who spend a relatively short time on an operating theatre table or patient trolley. This risk increases with prolonged immobility, poor nutrition, obesity, excessive thinness, debilitating illness, lowered mental awareness, (or loss of consciousness), moist skin due to sweating or incontinence, over-hydration, or dehydration. Pressure sores are serious, and may become a life-threatening problem for individuals receiving care in any setting. If individuals at risk are identified and the appropriate skin care and attention is received, giving all due regard to all the specific factors which may increase the risk, the likelihood of pressure sores can be limited. It is therefore a fundamental aspect of care, and, part of the responsibility of the care team. This aspect of care does not include the treatment of established pressure sores, for which specialist clinical guidelines are available. Where any of the risk factors mentioned above are present, people receiving care in their own homes or residential settings should be assessed by a district nurse. of the indicators will vary with the location and the client group. Principle People must be helped to look after their skin and every effort made to prevent them developing pressure sores. Practice Indicators 12.1 People are assessed for risk of pressure sores and if considered at risk, they receive further assessment by a registered nurse and a plan of care is drawn up. 12.2 People are made aware of the risks of pressure sores and shown ways of preventing them. They and those caring for them are encouraged and advised on appropriate care procedures. 12.3 Appropriate beds, chairs and other equipment are made available to reduce the risks of pressure sores. More specialist preventative equipment such as special mattresses and cushions are also available if necessary. All equipment is clean and properly maintained. 12.4 Correct moving techniques are encouraged, including regular turning and appropriate self-care, helping people to avoid pressure sores, increasing their well-being, independence and dignity. 12.5 If a person is at risk, their skin is checked at least once daily, preferably when their personal hygiene is attended to. 12.6 A person who is at risk or who has a pressure sore has access to advice from a registered nurse. This includes assessment and a plan of care based on recognised best practice. This Principle is relevant to all care settings and client groups, but the relevance of some 59 Some examples of what the indicators mean in practice ● Prevention is better than cure. Nearly all pressure sores can be prevented. ● Listen carefully to what the person says about how their skin feels e.g. itching, burning. Teach them what they can do for themselves to keep their skin in good condition. ● Teach the person to change their position frequently. ● Check every day for any changes in condition or colour of the skin e.g. redness, dryness or soreness. ● If you are in any doubt, get advice. ● If you are a commissioner of services, make sure that you have a clear policy about the responsibility for provision of appropriate equipment to prevent or relieve pressure sores. Cross references Fundamentals Indicator Corresponding Standards Principle Level 2 National Occ. Standards in Care Unit 01 Level 3 National Occ. Standards in Care Unit 02 Level 3 National Occ. Standards in Prom. Ind. Unit 02 Social Care Induction Framework Core Areas 1.1,4.2 12.1 NAfW NMS Care Homes for Older People standard 15.3 NAfW NMS Care Homes for Younger Adults standard 19 Level 2 National Occ. Standards in Care Unit Z7 Level 3 National Occ. Standards in Care Unit Z7 Level 3 National Occ. Standards in Prom. Ind. Unit Z7 NICE Pressure ulcer risk assessment and prevention 12.2 Level 2 National Occ. Standards in Care Unit Z7 Level 3 National Occ. Standards in Care Unit Z7 Level 3 National Occ. Standards in Prom. Ind. Unit Z7 NICE Pressure ulcer risk assessment and prevention 12.3 Level 2 National Occ. Standards in Care Unit Z7 Level 3 National Occ. Standards in Care Unit Z7 Level 3 National Occ. Standards in Prom. Ind. Unit Z7 NICE Pressure ulcer risk assessment and prevention 12.4 Level 2 National Occ. Standards in Care Unit Z7 Level 3 National Occ. Standards in Care Unit Z7 Level 3 National Occ. Standards in Prom. Ind. Unit Z7 NICE Pressure ulcer risk assessment and prevention 60 Fundamentals Indicator Corresponding Standards 12.5 Level 2 National Occ. Standards in Care Units Z7,Z9 Level 3 National Occ. Standards in Care Unit Z7 Level 3 National Occ. Standards in Prom. Ind. Unit Z7 NICE Pressure ulcer risk assessment and prevention 12.6 Level 2 National Occ. Standards in Care Unit Z7 Level 3 National Occ. Standards in Care Unit Z7 Level 3 National Occ. Standards in Prom. Ind. Unit Z7 NICE Pressure ulcer risk assessment and prevention Selected references Adcock, L. (2001) Preventing pressure ulcers: the work of the residential homes nursing team, Nursing Older People; 13(1) p14-6. Care Council. (2002) Codes of Practice for Social Care Workers. Available from: www.ccwales.org.uk Care Council. (2002) Induction Framework for Social Care. Available from: www.ccwales.org.uk Care Council. (1998) National Occupational Standards in Care Level 2 and 3 and Promoting Independence Level 3. Available from: www.ccwales.org.uk Clay, M. (2000) Pressure sore prevention in nursing homes, Nursing Standard; 14(44) p45-50, 52, 54, Available from: www.nursing-standard.co.uk/archives/vol14-44/pdfs/4550w44.pdf. Gebhardt, K. (2002) Pressure ulcer prevention: part 1. Causes of pressure ulcers, Nursing Times; 98(11) p41-4. Gould, D. and James, T. and Tarpey, A. and Kelly, D. and Pattison, D. and Fox, C. (2000) Intervention studies to reduce the prevalence and incidence of pressure sores: a literature review, Journal of Clinical Nursing; 9(2) p163-77. McCafferty, E. and Watret, L. and Brown, C. (2000) A multidisciplinary audit of patients’ seating needs, Professional Nurse; 15(11) p715-8. National Assembly for Wales. (2001) Regulations and national minimum standards for care homes for older people, care homes for younger adults and adult placements. NHS. (2001) Policy for the prevention and treatment of pressure ulcers. National Institute for Clinical Excellence. (2001) Working together to prevent pressure ulcers. Available from: www.nice.org.uk/pdf/clinicalguidelinepressuresorespatleafletenglish.pdf. 61 North West Wales NHS Trust. (2001) Pressure ulcer policy and guidelines. Ogonovsky, M. (2001) Draft policy for pressure ulcer prevention and management. North Glamorgan NHS Trust. RCN Guidelines. (1999) Pressure ulcer risk assessment and prevention. Department of Health. Available from: www.nice.org.uk/Docref.asp?d=16423. Reed, S. and Hambridge, K. and Land, L. (2001) Ntplus. Implementing best practice in pressure ulcer prevention, Nursing Times; 97(24) p69-71. Russell, L. (1998) Wound care management. Physiology of the skin and prevention of pressure sores, British Journal of Nursing; 7(18) p1084, 1088, 1090-2 passim. Shipperley, T. (2000) Guidelines for pressure ulcer prevention and management, Nursing Times; 96(14 Ntplus) p11-2. Stanton, J. (2001) Literature review. A nurse’s aid to clinical selection of pressure-reducing equipment, British Journal of Nursing; 10(15) pS16, S18, S21-4 passim. The Tissue Viability Society webpage. Available from: www.tvs.org.uk. 62 5. Monitoring the use of the indicators Performance monitoring will take place at all levels, as illustrated below. Service Users and Carers Service Providers Community Health Councils Local Health Boards Commissioners Social Services Local Authorities Regional Offices NHSD CSIW Welsh Assembly Government 63 SSIW NHS Social Services Within the NHS, monitoring of the standards is included within the Service and Financial Frameworks process. Organisations will need to provide evidence that they are implementing the standards. Social Services Inspectorate Wales (SSIW) inspects how local authorities carry out their social services responsibilities. In doing so, SSIW checks how authorities meet the requirements of legislation and guidance, including good practice guidelines, and how local authorities themselves ensure quality through their management and monitoring arrangements. These will include the Fundamentals of Care. As NHS performance management develops, it will increasingly focus on continuous improvement. Organisations’ performance will be assessed against a set of criteria within a balanced scorecard, which brings together a number of different elements. These might include existing capacity and organisation and processes, as well as outcomes. Within this context, application of the Fundamentals of Care standards will need to be assessed along with other elements of performance, such as meeting financial requirements and implementation of National Service Frameworks. The aim will be to support organisations in making a single and joined up assessment of their performance, as the basis for consolidation of good practice and improvement where necessary, rather than working through piecemeal and partial audits. Care Standards Inspectorate Wales The National Assembly for Wales has a range of regulations and national minimum standards that cover services that people receive at home, in care homes or in private and voluntary health care settings. CSIW is responsible for ensuring that providers in the independent, voluntary and local authority sectors deliver services in accordance with these regulations and national minimum standards. The Fundamentals of Care will be referred to by CSIW in addition to other national guidance, where it is helpful to provide guidance on practice. As the new continuous improvement approach is introduced, application of these standards will be absorbed into a national process of setting requirements, assessing performance, creating action plans for improvement, putting these into action and monitoring change. It is also envisaged that Community Health Councils will be able to use the standards during their visits to healthcare settings. In terms of planning, the new Health and Wellbeing Strategies will take account of these standards. 64 6. Useful Contacts For an electronic version of this document, access the Welsh Assembly Government website at: www.wales.gov.uk/subihealth/content/booklet-e.pdf Association of Welsh Community Health Councils Park House Greyfriars Road Cardiff CF10 3AF Tel. 029 2023 5558 Care Standards Inspectorate Wales National Assembly for Wales 4-5 Charnwood Court Heol Billingsley Nantgarw CF15 7QZ Tel. 01443 848451 NHS Wales Clinical Governance Support and Development NHS Quality Division Welsh Assembly Goverment Cathays Park Cardiff CF10 3NQ Tel. 029 2082 3319 Maggie Parker (Chair of Steering Group) Office of the Chief Nursing Officer Welsh Assembly Goverment Cathays Park Cardiff CF10 3NQ Tel. 029 2082 3915 NHS Direct Wales Tel. 0845 46 47 www.nhsdirect.wales.nhs.uk Patients Association PO Box 935 Harrow Middlesex HA1 3YJ Tel. 020 8423 9111 Care Council of Wales Tel. 029 2022 6257 Welsh Risk Pool (01745) 589799 Carers National Association Tel. 029 2081 1370 Crossroads Wales Tel. 029 2022 2282 Contact-a-Family Wales Tel. 029 2049 8001 Princess Royal Trust for Carers Tel. 020 7480 7788 Carer’s Assessment Leaflet available from: www.wales.gov.uk/subisocialcarers/ 65 Appendices Appendix 1 Steering Group membership A steering group consisting of the following individuals guided the project. Name Representing Mandy Arthur Vanessa Bourne David Boyland Professor Dame June Clark Natalie Cooper Maggie Crawford Vernesta Cyril Dr Brynley Davies Margaret Ellis Sue Gregory Janet Griffiths Florinda Hall Judith Hill Linda Hopkins(Researcher) Gillian Hughes Yvonne Hurcombe Jonathan Isaac PMD, Welsh Assembly Government Patients Association PMD, Welsh Assembly Government (Researcher) University of Wales Swansea and CYNGOR SSIW, Welsh Assembly Government Independent Healthcare Sector Southeast Wales Racial Equality Council Independent Medical Advisors Directors of Social Services Nurse Executives Wales Chair All Wales Special Interest Group (Dental) Southeast Wales Racial Equality Council Iechyd Morgannwg Health Association of Welsh Community Health Councils CSIW, Welsh Assembly Government Campaign for Care (Service Users) Project Manager, Office of the Chief Nursing Officer, Welsh Assembly Government Association of Welsh Community Health Councils (Researcher) University of Wales Swansea (Chair) Office of the Chief Nursing Officer, Welsh Assembly Government All Wales Committee for Health Care Professions Office of the Chief Medical Officer, Welsh Assembly Government Welsh Council for Voluntary Action Health Professional Group, Welsh Assembly Government SSIW, Welsh Assembly Government CSIW, Welsh Assembly Government CSIW, Welsh Assembly Government PMD, Welsh Assembly Government Care Forum Wales Jane Jeffs Janet Jones Maggie Parker Sue Rees Dr David Salter Daisy Seabourne Jan Smith Howard Teague Sue Whitson Angela Williams Gaynor Williams Cheryl Wilsom-Carter 66 Appendix 2 Contributors to redrafting The Steering Group acknowledges the contribution of the following people who helped to redraft the documents: Sue Acreman, Therapy Services Manager, Velindre NHS Trust Mair Allinson, Senior Nurse, North Glamorgan NHS Trust Victoria Deakins, Occupational Therapist, Powys Healthcare NHS Trust Ruth Derrick, Team Manager, Torfaen Social Services Iolo Eilian, Planning and Development Officer, Wrexham Social Services Cerri Evans and Andrew Critten, Plas Penmon Nursing Home John Greer, Chief Podiatrist, Pembrokeshire and Derwen NHS Trust Helen Jones, Social Worker, Wrexham Social Services Tracy Livingstone, Assistant Matron, Nightingale Home Hospices and Cancer Support Centre Dr Charles Twining, Clinical Psychology Advisory Subcommittee, Welsh Medical Committee Jackie Wilding, Parkinsons Disease Specialist, Powys Healthcare NHS Trust 67 ISBN: 0 7504 3102 4 © Crown copyright 2003 Welsh Assembly Government, Cathays Park, Cardiff CF10 3NQ 03/03