ENGAGING PRIMARY AND SECONDARY STAKEHOLDERS IN CME:
advertisement

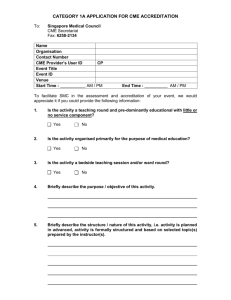
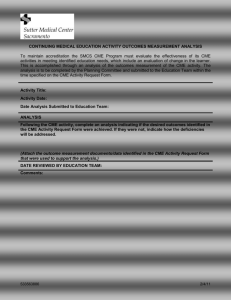
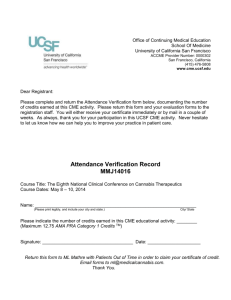
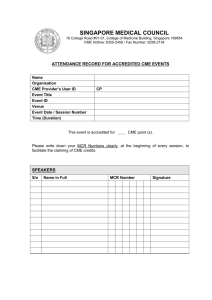
ENGAGING PRIMARY AND SECONDARY STAKEHOLDERS IN CME: A Model for Continuous Improvement in Healthcare Outcomes Lisa Keckich, MS As the CME industry looks to emerge as a driver of improved quality of care and patient outcomes, comprehensive educational strategies reflective of the multifaceted healthcare environment are essential to realize these goals. Such strategies actively engage diverse stakeholders in healthcare and foster broad participation and collaboration to transform the reach and redefine the value of CME. While alliances are not new to the world of CME, limited financial and human resources, coupled with short-term profitability targets and the demand for more immediate outcomes data has often resulted in partnerships forged for convenience rather than value. The resulting environment is one where collaborations are: 1) sought largely for endorsement purposes and fail to define the strategic and mission-driven value for each organization beyond financial remuneration; 2) fail to navigate the administrative and political barriers of each organization to make truly impactful improvements; or 3) fail to leverage human or financial resources outside of the organization to broaden the scope of delivery. In order for CME to serve as a catalyst for improving patient health, providers must not only redefine collaboration, but operationalize an approach for successful engagement of collaborators and management of outcomes. The proposed framework creates a methodology to consider the broader health implications of the planned CME; identify prospective partners and define value for each stakeholder; assess the viability of the partnership relative to the goals and scope of the educational initiative; and develop an implementation plan that optimizes resources and mitigates risk. OBJECTIVE To create a roadmap to identify prospective partners who can enhance the delivery and outcomes of CME. METHODOLOGY To broaden the impact of CME in healthcare delivery and patient health, improve the efficiency and effectiveness of education delivery, and create educational platforms responsive to the larger healthcare marketplace, CME providers must engage stakeholders who are in a position to influence successful outcomes. The value of these relationships includes both strategic and operational benefits, with implications for not only clinicians and patients, but the opportunity to further public health interests. Stakeholder Analysis In order to assess the relevance and value a potential collaborator may contribute in furthering the goals, objectives and impact of a CME initiative, a systematic evaluation of those stakeholders must be undertaken. Such an examination will optimize the CME providers’ time and financial investment and ensure the right fit between partner and deliverables. Timeline Generate list of all possible stakeholders Y GROUP A Existing Relationship? Y N History of Partnerships? GROUP N GROUP B C Group A offers the most immediate opportunity and possibility for collaboration with the least amount of startup investment. Group B offers the second most direct opportunity, but providers should anticipate additional time and resources to create a dialogue and establish a relationship. Providers who wish to engage in any potential collaboration with organizations in Group C should anticipate a significant investment in time and resources to secure. In order to direct resources towards those collaborations which offer the greatest benefit to the success of the education, compare the level of influence each partner holds relative to their effectiveness as an organization. Assessment of Influence Rate each organization on your list based on the following criteria: - Ability to engage internal stakeholders - Ability to engage external stakeholders - Ability to maintain political or public support - Ability to influence healthcare policy Planning & Implementation Once all collaborators have agreed to partner conceptually, the greatest roadblock to success is failure to adequately plan and implement the proposed initiative. To align with ACCME criteria, CME providers will use their planning document to drive decision making and operationalize the project; however, these steps alone may not be considerate of the required processes/rules within each stakeholder’s system. Therefore, it is recommended that as part of the planning process, the CME provider profile each stakeholder based on similar sets of criteria. Organizational barriers imposed by rigid cultures, employee beliefs, complicated decision making hierarchies and resource limitations can affect performance and influence the success of the planned initiative. Overcoming these barriers is a matter of interpreting these organizational conditions and intervening in a way that is responsive and respectful.1 CME Provider Medical Specialty Society Patient Advocacy Group Hospital Expected Outcomes CME program delivering L5 outcomes and meeting MOC requirements MOC compliant education for members Published and measurable strategies to improve QOL for patients with XYZ Improved hospital compliance around accreditation standards and delivery of QI Goals & Strategies To improve the perfor- To improve reimbursemance of physicians in ment of members who the treatment of XYZ treat XYZ and deliver better outcomes To create an iPhone app where patients can collect daily data around XYZ and transmit to their physician To meet standards for Joint Commission accreditation and improve state funding Resources • • • • • Education Manager (staff) • Education Committee (volunteers) • Communications Committee (volunteers) • Lobbyist • Membership Email Blasts • Membership Newsletter • Membership Facebook and Twitter • Project Manager • Director of Development • Facebook and Twitter • Celebrity relationships • • • • Decision Making Processes • Task DecisionsProgram Manager • Content DecisionsMedical Director and Faculty • Policy DecisionsCompliance Officer • Task Decisions – Staff • Design Decisions – Committee • Policy DecisionsBoard of Directors • Task Decisions – Project Manager • Financial DecisionsDirector of Development • Policy DecisionsBoard of Trustees • Task Decisions – QI Officer and CME Manager • Policy DecisionsCompliance Officer • Content DecisionsDepartment Head and CME Manager Technology Document Sharing Web Portal PI CME Portal Membership Intranet Website Intranet Satellite TV Live Case Recording Equipment Culture Fast paced Flat hierarchy Long workdays Volunteer driven Several competing political factions Consensus driven in decision making Self-described “family” Informal decision making structure All materials must be “green” Unknown Assessment of Organizational Effectiveness Rate the effectiveness of each organization on your list based on the following criteria 1: - Life-cycle stage (e.g., start-up v. established organization) - Availability and skill of resources (e.g., volunteer v.paid staff) - Organizational size and complexity - Degree of bureaucracy/assessment of power alignments and decision making processes - Purpose: for profit v. non profit - Technology capabilities - Organizational Culture High Prioritize who is critical to the success of the initiative, based on a high level of influence and high assessment of organizational effectiveness. The results should be plotted on a chart for easy identification 2: High Priority Collaborations Influence INTRODUCTION Low High Low Step 1 Scan the environment and compile a listing of all possible stakeholders who may have an interesting the outcomes of the education Step 2 Divide the list into two groups—those with whom you have an existing or prior relationship and those where no relationship exists Step 3 For those prospective partners where no relationship exists, determine whether there is a history of them partnering with other CME providers The result is 3 groups: Group A: Stakeholders with whom you have partnered with in the past Group B: Stakeholders who have demonstrated a commitment to working with other CME providers on external education/collaborations Group C: Organizations with no prior experience in external collaborations with CME providers REFERENCES: 1. Harrison, Michael I. Diagnosing organizations: methods, models and processes. 1994. Sage Publications. 2. Ruhe, Mary C. Stakeholder analysis in health services management. Accessed on 2/12/11. http://www.case.edu/med/epidbio/mphp439/Stakeholder_Analysis.htm Acknowledgements: Caryn Lobel, MD, Mindi Daiga, MBA Medical Director Program Team Digital Strategist Compliance Officer Organizational Effectiveness Approaching Stakeholders Once a list of high-impact collaborators are identified, the value for those stakeholders and the objectives and expected outcomes of the education must be clearly defined: 1. Identify decision-makers within organization and gauge level of access to those individuals 2. Create a rationale for engagement a. Demonstrate how proposed education aligns to stakeholders’ organizational priorities and mission b. Define value for the stakeholder at the organizational and constituent level; Examples: i. Organizational Level: revenue, ability to influence policy, ability to improve levels of care, ability to control healthcare delivery costs ii. Constituent level: enhanced education, improved reimbursement practices, improved access to care c. Describe expected outcomes and measures of success d. Provide examples of how similar collaborations have been successful 3. Describe proposed relationship a. Roles and responsibilities b. Access to information c. Resource allocations/requirements for each organization and proposed timing d. Levels of ownership and control/oversight e. Mechanisms for systems integration (technology, shared staffing) f. Financial commitments and/or revenue projections Disclosures: Lisa Keckich, MS has no relationships to disclose QI Officer Compliance Officer CME Manager Department Head By conducting this type of analysis prior to commencing the project, the CME provider can improve the ongoing efficiency of the implementation, appropriately manage the expectations of each stakeholder, and ensure individual goals are being met. Once completed, the analysis is considered when mapping out ongoing steps which include: 1. Establish an internal communications plan and mechanism for reviews and approvals that is considerate of the profile completed for each stakeholder 2. Create a project roadmap and outline collaborator’s tasks at each milestone 3. Recognize a process for contingency planning 4. Design an outcomes methodology and define measures of success 5. Create an external communications/awareness plan CONCLUSION Financial and capacity limitations restrict the number of collaborations that can be pursued each fiscal year; however, by earmarking resources to engage in 1-2 large scale initiatives annually, providers have the opportunity to diversify funding streams, improve the efficiency and effectiveness of the education being developed, deliver more sophisticated outcomes considerate of both CME criteria and public health variables, and influence healthcare practice and policy. ©2011 The Academy of Continued Healthcare Learning