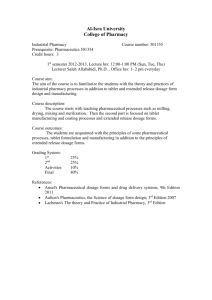
cGMP in the USA - Pharmaceutical Manufacturing
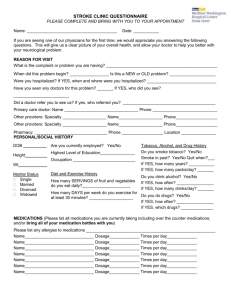
advertisement

FDA FDA cGMP cGMP China China Training Training Program Program December -7, 2005 December 55-7, 2005 Ying Ying Jie Jie Convention Convention Center Center Beijing Beijing University University Beijing Beijing cGMP in the USA Nicholas Buhay Deputy Director Division of Manufacturing & Product Quality Office of Compliance, CDER, FDA Introduction to Drug Current Good Manufacturing Practice Of US FDA An An Outline Outline • Legal bases for cGMP • cGMP legal principles • cGMP Implementation Tools • cGMP Resources • Overview of cGMP Requirements • Integrity of Records and Data FD&C FD&C Act; Act; 501(a)(2)(B) 501(a)(2)(B) “A drug shall be deemed adulterated if: ... the methods used in, or the facilities or controls used for, its manufacture, processing, packing, or holding do not conform to or are not operated or administered in conformity with current good manufacturing practice ...” more... FD&C FD&C Act; Act; 501(a)(2)(B) 501(a)(2)(B) “to assure that such drug meets the requirements of this Act as to safety and has the identity and strength, and meets the quality and purity characteristics, which it purports or is represented to possess.” cGMP cGMP legal legal principles principles • Quality built into product – By “taking care” in making medicine – Can’t ‘test’ into product the quality • Without/Inadequate cGMP – Product(s) adulterated(defects need not be shown) – Firm and its management are responsible cGMP cGMP legal legal principles principles • Non-compliance = eventual problems – Superpotency/subpotency – Contamination – Misbranding – Bioavailability – Safety and efficacy cGMP cGMP Legal Legal Principles Principles • Scope – Ingredients (APIs + excipients) – Finished dosage forms administered to humans/animals »OTC, Rx products »Biologics, veterinary drugs »Drugs undergoing study(IND, etc) – Manufacturers, test laboratories, packagers(including pharmacies) cGMP cGMP legal legal principles principles • Excluded from the cGMP requirement – Positron emission tomography, per FDAMA (own cGMP to be developed) – Drug products compounded per Section 503 Pharmacy Compounding (FDAMA) cGMP cGMP Legal Legal Principles Principles • Current = dynamic – Standards evolve over time • Good practices – Minimal standards – Not “best practices” » Unless “best” is, in fact, current minimal cGMP cGMP Legal Legal Principles Principles • Feasible and valuable – No threshold for “percentage” in practice »Doesn’t have to be “predominant” – Enforceable even if nobody is doing it »Stronger case if someone is doing it The The cGMP cGMP Regulation Regulation • cGMP for Finished Pharmaceuticals 21 CFR 210, 211 – First issued: June 1963 – Today’s version: September 1978 – Scope »Dosage forms for human/vet/biologics »OTC, Rx, IND, NDA, Medical Gases »Not: pharmacies, ingredients, nonclinical research, etc The The cGMP cGMP Regulation Regulation • cGMP for Finished Pharmaceuticals 21 CFR 210, 211 – Substantive » Force and effect of law – Constitute major part of (not entire) cGMP more... The The cGMP cGMP Regulation Regulation • cGMP for Finished Pharmaceuticals 21 CFR 210, 211 – Establish “what to” do, not “how to” do »Minimal standards »Maximum flexibility »Specific enough to address problems • e.g., Penicillin contamination control »Technology neutral »Scalable cGMP cGMP Implementation Implementation Tools Tools • Compliance Policy Guides – Specific actions we do related to cGMP – Examples: » Sub Chapter 410 Bulk Drugs • The regulations for finished pharmaceuticals will be applied as guidelines for bulk drugs » Sub Chapter 420 Compendial (USP)/Test Requirements Ex:USP not required for release test » Other Sub Chapters • Labeling and Repackaging • Stability/Expiration • Process Validation • Etc cGMP cGMP Implementation Implementation Tools Tools • cGMP Guidance Documents – Principles: »Not requirements »Agency “current thinking” »Detailed, technical »Expression of “How to” meet “what to” do (requirements) – Shape industry behavior »offers routes to efficiency in meeting cGMP requirement, evaluation of compliance cGMP cGMP Implementation Implementation Tools Tools • cGMP Guidance Documents (Examples) – General Principles of Process Validation – Compressed Medical Gases – Sterile Drug Products Produced by Aseptic Processing – Guideline on the Preparation of Investigational New Drug Products more... cGMP cGMP Implementation Implementation Tools Tools • cGMP Guidance Documents – Investigating Out of Specification Test Results for Pharmaceutical Production – Manufacturing, Processing or Holding of Active Pharmaceutical Ingredients cGMP cGMP Implementation Implementation Tools Tools • cGMP Compliance Programs –Instructions to FDA inspectors – Drug Manufacturing Inspections Program » Systems-based assessment of site – Preapproval Inspection Program » Points to inspect » Laboratory support » Regulatory approaches cGMP cGMP Implementation Implementation Tools Tools • cGMP Guides to Inspection of…. – Help field investigators apply cGMP »Uncover need for cGMP changes »Specific to topics (e.g., cleaning validation) cGMP cGMP Resources Resources • Internet WWW site by DMPQ – http://www.fda.gov/cder/dmpq »cGMP regulations and ongoing changes »Preamble to the cGMP regulation »Division subject contacts »Medical gases »Active pharmaceutical ingredients »Human Drug cGMP Notes/Policy »etc. Overview Overview of of cGMP cGMP requirements requirements in in the the regulation regulation • cGMP Regulations – 21 CFR 210 » Status of the regulations » Applicability of the regulations » Definitions • Batch • Lot • In-process material • Quality control unit • Representative sample • etc Overview Overview of of cGMP cGMP requirements requirements in in the the regulation regulation • cGMP Regulations – 21 CFR 211 » Subpart A General Provisions » Subpart B Organization an Personnel » Subpart C Buildings and Facilities » Subpart D Equipment » Subpart E Control of Cmpnts/Cntr/Closures » Subpart F Production and Process Controls » Subpart G Packaging and Labeling Controls more... Overview Overview of of cGMP cGMP requirements requirements in in the the regulation regulation • cGMP Regulations – 21 CFR 211 »Subpart A General Provisions • this is minimum cGMP Overview Overview of of cGMP cGMP requirements requirements in in the the regulation regulation • cGMP Regulations – 21 CFR 211 »Subpart B Organization and Personnel • There shall be a quality control unit • quality control unit responsibility to approve/reject Overview Overview of of cGMP cGMP requirements requirements • cGMP Regulations – 21 CFR 211 » Subpart C Buildings and Facilities • buildings shall be….suitable • operations to be in specifically defined areas….separate…. Or such other control systems for ….operations as are necessary to prevent contamination or mix-ups…. (see list, includes aseptic processing) • “separate” facilities for penicillin • building….shall be….clean and sanitary Overview Overview of of cGMP cGMP requirements requirements • cGMP Regulations – 21 CFR 211 »Subpart D Equipment • surfaces ….shall not be reactive, additive, or absorptive • Equipment….shall be cleaned, maintained and sanitized…. Overview Overview of of cGMP cGMP requirements requirements • cGMP Regulations – 21 CFR 211 » Subpart E Control of Components, Containers and Closures • containers and closures ….handled in a manner to prevent contamination. • Testing or examination of c/c/c’s • test to identify each component • tests on components for conformance with specs • test c/c/c’s microscopically, for adulterants, microscopically Overview Overview of of cGMP cGMP requirements requirements • cGMP Regulations – 21 CFR 211 » Subpart F Production and Process Controls • written procedures for production and process control • formulated not less than 100 % • portions of components identified, examined by a 2nd person before dispensed for use in manufacture • sampling and testing of in-process materials and products, some specified • time limits • reprocessing allowed, but controlled Overview Overview of of cGMP cGMP requirements requirements • cGMP Regulations – 21 CFR 211 » Subpart G Packaging and Labeling Controls • examination, approval of labels, labeling • strict control over labeling issue, and return to stock • written procedures, physical separation of labeling operations • examination of materials before use • inspection of facilities immediately before • tamper resistant packaging (for OTC products) • expiration dating Overview Overview of of cGMP cGMP requirements requirements • cGMP Regulations – 21 CFR 211 » Subpart H Holding and Distribution » Subpart I Laboratory Controls » Subpart J Records and Reports » Subpart K Returned and Salvaged Drug Products Overview Overview of of cGMP cGMP requirements requirements • cGMP Regulations – 21 CFR 211 »Subpart H Holding and Distribution • quarantine before release • store under appropriate conditions Overview Overview of of cGMP cGMP requirements requirements • cGMP Regulations – 21 CFR 211 »Subpart I Laboratory Controls • establish specs, standards, sampling plans, test procedures • calibration, of laboratory equipment • test each batch of drug product • adequate acceptance criteria • validate test methods • conduct stability program more.... Overview Overview of of cGMP cGMP requirements requirements • cGMP Regulations – 21 CFR 211 » Subpart I Laboratory Controls • Special tests – sterility and pyrogenicity – ophthalmic ointments for foreign/abrasive particles – controlled release products for rate of release • keep reserve samples • test non-penicillin products for penicillin when reasonable possibility of exposure to presence of penicillin Overview Overview of of cGMP cGMP requirements requirements • cGMP Regulations – 21 CFR 211 »Subpart J Records and Reports • keep records, make available for inspection • conduct annual review of each drug product for changes to specs, control procedures • keep equipment cleaning and use log • keep component, container, closure and labeling records more.... Overview Overview of of cGMP cGMP requirements requirements • cGMP Regulations – 21 CFR 211 » Subpart J Records and Reports • have SOP for master production and control record, maintain record • use batch production and control records for manufacture, keep records • records to be reviewed/approved by qual control unit • complete data derived from all tests necessary to assure compliance more.... Overview Overview of of cGMP cGMP requirements requirements • cGMP Regulations – 21 CFR 211 »Subpart J Records and Reports • distribution records, with lot numbers(except medical gases) • complaint files Problem – Drug Regulatory Program depends heavily on the reliability (i.e. truthfulness, completeness and accuracy) of data & information in records – Applications for approval [AIP] – Manufacturing Controls documentation [non-AIP] – Historical experience with broad scale unreliability of data in records or in conduct related to records Data Data and and records records that that are are not not acceptable acceptable or or are are misleading misleading What are some characteristics of data that lack integrity? » Untrue, made up, false, no source in an event » Omission of significant data from the submission that is determined to be material to the review process. Data that is not submitted, but should have been » Inaccurate (e.g. First data failed specs, retest data passes specs, no lab investigation, but retest data is submitted to the application.) Records Records Must Must be be True True • All data and information in records submitted to FDA & supporting documents in the possession of the applicant are accurate & true representations of – – Actual tests performed & the test results – Actual manufacturing & quality control steps & procedures associated with the development and manufacture of the submission batch (clinical/pilot or biobatch) – any other actions and conditions associated with the application Wrongful Acts ÎAny act or conduct that subverts the integrity of the review process, including, but not limited to the following: – submitting fraudulent applications – offering or promising a bribe or illegal gratuities – – making an untrue statement of a material fact (e.g. false statement, a misstatement or an omission of a fact) submitting unreliable data which results from system-wide or firm-wide behavior Wrongful Acts (continued) ÎAn untrue statement of material fact is a false statement, a misstatement or an omission of a fact that is important in the review process. ÎSystem-wide incompetence is also a wrongful act ÎWhen an untrue statement of material fact or system- wide incompetence is found, several steps are required to the invoke the AIP including: – – Documentation of a pattern or practice of wrongful acts. Ensuring that the untrue statements are material facts. Pattern or Practice ÎPattern- More than one instance of errors or acts involving the subject matter important to the evaluation of an application ÎPractice- An act or process of doing something affecting subject matter important to the evaluation of an application ÎA practice can be one or more acts or processes. A pattern or practice can occur in one or more applications. If submitted to an Application ÎThe AIP procedures broadly define the term, “application” to include, but not be limited to, any application, amendment, supplement or other submission made by an applicant. ΓSubmitted” is an understandable term and includes documents received by the review branch. ÎWrongful acts also include omissions of data and/or information that should have been submitted to an application. Food, Drug, and Cosmetic Act Section 505(e) (excerpt below) Numbered Part 5 – The Secretary shall, after due notice and opportunity for hearing to the applicant,withdraw approval of an application with respect to any drug under this section, if the Secretary finds…. – (5) that the application contains any untrue statement of a material fact TO INVOKE AIP ÎDocumentation of a pattern or practice of wrongful conduct that raises significant questions about the reliability of data submitted to an application - wrongful acts - pattern or practice - unreliable data Restore FDA’s Confidence in Data??? ÎCooperation with investigators ÎIdentification of involved individuals ÎCredible internal review & actions ÎProblem analysis/identify all instances of wrongful acts ÎUse of impartial auditor/Outside consultant ÎAudit Plan, audits, audit reports ÎOther measures as FDA deems appropriate Restore FDA’s Confidence in Data ÎCorrective Action Operating Plan: ÎAnalysis of audit findings ÎImplementation of auditor recommendations ÎActions taken to correct fraud/wrongful acts, e.g. ÎWithdraw applications & recall products ÎTimetable ÎIdentification of persons assigned to complete and verify corrective actions ÎComprehensive ethics program ÎProcedures for monitoring effectiveness of the plan ÎTraining in the requirements of the Act and 18 USC 1001 Corrective Actions Plan Evaluation Monitor applicant’s actions/inquiries during internal review ÎInspection to assess actions taken by applicant to determine if ÎInternal Review performed adequately ÎCorrective Action Operating Plan implemented adequately ÎSubmit recommendation to CDER to remove site from the policy ÎExpect a long time to pass before restoration Overview Overview of of cGMP cGMP requirements requirements • cGMP Regulations – 21 CFR 211 »Subpart K Returned and Salvaged Drug Products • if conditions cast doubt returned product shall be destroyed unless proved ok by test, examination, investigation • salvage only if evidence from tests and inspection show all standards met Input Input for for cGMP cGMP Changes Changes • Establishment inspections – Industry changes/problems • Defect reports/complaints/recalls • Litigation • Agency application reviews • Trade/scientific literature • Citizen petitions Management Management of of cGMP cGMP Regulatory Regulatory Program Program • FDA/CDER – OC/Division of Manufacturing and Product Quality – – – – maintenance of the regulation definitive interpretation manage guidance development develop, operate, evaluate programs – train FDA/outreach to industry We We Have Have Discussed Discussed • Legal bases for cGMP • cGMP legal principles • cGMP Implementation Tools • cGMP Resources • Overview of cGMP requirements • Integrity of Records and Data Nicholas Buhay Deputy Director Division of Manufacturing and Product Quality, HFD-320 Center for Drug Evaluation and Research Phone: 301-827-8940 Fax: 301-827-8907 E-mail: buhay@cder.fda.gov Montrose Metro Centre II Room 438 11919 Rockville Pike Rockville, MD 20852 FDA CGMP China Training Program December 5-7, 2005 Ying Jie Convention Center Beijing University Beijing Counterfeit Drugs Nicholas Buhay Deputy Director Division of Manufacturing & Product Quality Office of Compliance, CDER, FDA Counterfeit Drugs • Not permitted: – Doing any act to cause a drug to be a counterfeit – Sale or dispensing a counterfeit – Holding for sale or for dispensing a counterfeit 2 Counterfeit Drugs • A drug, or container or labeling of it, that falsely represents the drug to be – To be the product of another manufacturer, processor, packer, or distributor – To have been packed or distributed by another manufacturer, processor, packer, or distributor 3 Counterfeit Drug • Not permitted: Why???? – Product lacks assurance of safety and efficacy 4 Counterfeit Drug • Assurance of Safety and Efficacy results from – Knowledge of the pedigree (heritage) of the shipment – Opportunity for regulatory attention to confirm • Inspection of conditions and practices in manufacture • Samples and tests • Review of information 5 Unapproved Drugs • In USA, components (API + non-active ingredients) are specified by source factory in the approval of a new drug application (NDA or ANDA) • Sometimes, also precursor chemicals are specified by source factory 6 Unapproved Drugs • The use of other materials different from materials from the specified source factory may be counterfeiting, but • Definitely the product made is an ‘unapproved new drug’ 7 Example: • Tablets look like ‘Viagra’ but • Tablets not manufactured, processed or distributed by manufacturer approved by FDA 8 Example • Acetaminophen API made by factory in Milan but, • Label says product made by factory in Beijing 9 Example • Buspirone API made by factory in India and, • Tablet manufacturer in USA uses the buspirone API to make buspirone tablets but, • Manufacturer’s FDA approved Abbreviated New Drug Application (ANDA) specifies tablet manufacturer must use only buspirone made by factory in Canada 10 Example • Importer in New York buys methylphenidate made in factory in Guangdong and, • Puts it into different drum labeled with name of factory in South Africa – Also, puts C of A data onto South Africa factory letterhead document 11 Example • The government of Russia orders Captopril Tablets to be made in a factory in Ireland and, • A multinational company operated factories in Ireland and in Puerto Rico and, • Captopril Tablets made in Puerto Rico factory of the company are shipped to Russia to fill the order 12 Example • A company in China operates two factories, one in Shanghai and one in Tianjin, and, • The factory in Tianjin is approved in an ANDA by FDA as source factory for cefuroxime but, • The company sells cefuroxime made in the Shanghai factory for use in making the approved drug tablets – The company writes batch records showing manufacture of this cefuroxime in the Tianjin factory 13 Example • A multinational company operates factories in France and Italy; an FDA approved ANDA approves total synthesis of cefaclor in the Italy factory, but • The company orders the factory in France to make a specified precursor and sends it to the Italy factory and, • The Italy factory uses the precursor to complete the synthesis of cefaclor • Italy factory sends cefaclor to USA – Italy factory makes batch records showing complete synthesis 14 ??Problem: Complex distributiona • • • • API source factory to Trader (s) to Importer to Finished Pharmaceutical Manufacturer • Carriers 15 ??Solution • Limit distribution system? • Markers? • Characterization/Identification? • Maintain ‘pedigree’? 16 Pedigree • Process specific • Lot specific • Shipment specific 17 Pedigree • Documentation – – – – – – – – – Batch records Labels Certificate of Analysis Sales Shipping Declaration (Gates) Receipt Storage Use 18 Pedigree • Modern Technology – Packaging – Shipping – Electronics 19 Summary • Counterfeiting of products are – Manufactured under unknown conditions and practices – Manufactured with unknown process – Undesirable product event (adverse reaction, product defect, etc) cannot be resolved • Regulatory oversight process is undermined • Loss of assurance 20 Concern validated • Actual event: – Haiti 1996 – Contaminated “Acetaminophen Syrup” product • 3% Glycerin • Water, sugars • 14% Ethylene glycol (engine antifreeze) • 80 children died 21 Concern validated • Source of contamination – “Synthetic Glycerin” component material – Used by Haiti manufacturer factory – Importer in Haiti – Trader in Netherlands (applied label to read ‘Glycerin USP’ – Trader in China – Manufactured in China (factory unknown) 22 ??Cause • • • • Manufacturer? Trader (s) Importer? Terror?? 23 FDA Approach to Thwarting Counterfeiting Multi-Pronged Approach • Technology • State and Federal Regulatory Action • Secure Business Practices • Education and Reporting • International Collaboration 24 Technology • Authentication Technologies • Track and Trace Technologies • No magic bullet – must use layered approach • Technology alone probably insufficient without secure business practices 25 Authentication Technology • Inks, Holograms, Taggants etc. • FDA recommends use of one or more on products/packaging, particularly those likely to be counterfeited • Manufacturers to use on a product specific basis after doing a cost/benefit analysis • No requirements for any particular technology 26 Track and Trace Technology Requires: • Mass Serialization • Infrastructure – hardware and software Can be accomplished with: • Radiofrequency Identification (RFID) Technology • 2D Bar Codes 27 Conclusion Counterfeit Drugs will be an ongoing problem • Sophistication FDA’s multi-pronged approach will make deterring and detecting counterfeits more feasible • Layered approach 28 Conclusion • • • • Don’t counterfeit It is a social threat It is a business threat Participate in development of distribution integrity 29 Conclusion • We must protect our children, our sick, our revered elders • We will be watching • We will appreciate your help 30 FDA cGMP Inspections Peking University 2005 Robert C. Horan, PhD FDA Pharmaceutical Inspectorate New York District FDA Inspections Periodic (biennial) comprehensive cGMP Pre-Approval Inspection(PAI) “For cause” Inspection may involve more than one assignment and will verify corrections to previous inspections. All inspections cover GMPs Foreign Inspections by Country in FY 2004 India 14% Others 19% Germany 14% Ireland 4% Spain 4% Switzerland 4% Italy 10% Japan 5% France 5% China 7% Canada 7% United Kingdom 7% Foreign Inspection in FY 2004 by Firm Type Both API and Dosage 9% Control Lab 2% Micronizer 1% Intermediates 10% API 51% Dosage 27% FDA cGMPs for 21st Century Initiative Announced 8/2002; objectives include: Encourage adoption of new technologies Promote industry use of modern quality system approaches Encourage risk-based approaches which focus on critical elements Ensure FDA review, compliance and inspection policies based on state-of-art pharmaceutical science FDA cGMPs for 21st Century Initiative Systems Based Inspections Risk-Based Approach to Manufacturing and Regulation Pharmaceutical Inspectorate PAT Guidance document/ PAT Team Quality Systems Guidance document Process Validation (Compliance Policy Guide revised; Guidance being revised) 21 CFR Part 11 Electronic Records Guidance (riskbased; geared toward GMP documents) Pharmaceutical Inspectorate Cadre of most experienced investigators who are dedicated to drug inspections Intensively trained along with quality reviewers and compliance staff in FDA headquarters (HQ) Overall goal is to have PI work closely with HQ personnel – more efficiently integrate review and inspection functions Pharmaceutical Inspectorate FDA Review staff, Compliance Officers and PI candidates attended training modules which focused on: ¾ Current Regulatory Programs ¾ Advanced Quality Systems ¾ PAT and Modern Pharmaceutical Technology ¾ Risk Management Pharmaceutical Inspectorate Field Investigators (18) from across U.S. make up the Pharmaceutical Inspectorate Screening process with certification board ¾ Completed training with HQ personnel ¾ One month detail working with HQ staff ¾ Level III certification (highest level) ¾ Conduct PAIs, complex drug inspections ¾ Process Analytical Technology PAT is a system for designing, analyzing and controlling manufacturing through “real time” measurements of critical quality attributes of raw and in-process materials and processes, with the goal of ensuring final product quality. See FDA Guidance document on PAT Process Analytical Technology Examples of PAT applications: Continuous real time measurements of content uniformity of tablets during production (using near Infra-Red) Near IR measurement of moisture level during API drying process to determine actual end of operation for each batch Process Analytical Technology A process is generally considered well understood when: ¾ ¾ All critical sources of variability are identified and explained Variability is managed by the process “Quality cannot be tested into products; it should be built-in or should be by design.” Process Validation Life Cycle Approach Process validation begins with process development and continues beyond the initial “validation” batches for as long as product is manufactured/marketed Sources of critical variability identified and controlled Quality System role in maintaining validated state (quality built in; not tested into product) Process Validation FDA Compliance Policy Guide “Process Validation Requirements for Drug Products and Active Pharmaceutical Ingredients CPG 7132c.08”; revision date 12 March 2004 FDA Industry Guideline on Process Validation – currently being revised System Inspections Quality Facilities and Equipment Materials Production Packaging/Labeling Laboratory Controls Most Common GMP Deficiencies by System – API/ Dosage Inspections for 2004/5 Materials 6% Packaging and Labeling 1% Laboratory 19% Facilities & Equipment 17% Production 11% Quality 46% “State of Control” Detailed inspection of a system so that the findings reflect the state of control in that system for every product (profile) class If one of the six systems is out of control, the firm is considered out of control A system is considered out of control based on GMP deficiencies which suggest lack of assurance of quality Quality System Quality must be built into the process Quality is not tested into the product Assurance of Quality comes from - Design of robust process based on thorough knowledge of that process and the sources of variability - Effective Quality System in place Role of Management in QS Management is responsible for: ¾ Organizational structure ¾ All Processes ¾ All Procedures ¾ Facilities & Resources In short, everything to insure product quality, customer satisfaction and continuous improvement Quality System Responsibilities Assures overall compliance with cGMPs Review and approval duties for: 1) Product Quality Reviews (at least annually) 2) Complaint reviews 3) Discrepancy/ failure investigations 4) Change Control 5) CAPA (Corrective And Preventive Action) Quality system (continued) 6) 7) 8) 9) 10) 11) Reprocess/ Rework Validation/ Revalidation Rejects Stability Failures/ Out of trend data Quarantine products Documented GMP & Job Related Training Laboratory Control System Adequate lab facilities under the Quality Unit which is independent from Production Adequately staffed laboratories (supervisory and bench personnel) Written specifications for raw materials, intermediates, APIs, labels & packaging Written procedures for sampling, testing, approval or rejection of materials and for the recording and storage of data Change control for written procedures Method validation/ revalidation Laboratory Control System Reference Standards (primary; secondary) Equipment Qualification Calibration: written procedures, schedule, documentation Validation and Security for computerized handling of test results and related data; system for assuring integrity of all lab data Laboratory controls followed and documented Laboratory Control System Written procedure (SOP) covering out of specification “oos” results Investigation of “oos” results conducted in a timely manner as per SOP and documented (complete records maintained). Conclusions from “oos” investigations documented and corrective actions/ need for addition investigation identified and implemented. “oos” review included in Product Quality Reviews Laboratory Control Records Description of samples Identification of method used Raw data for sample/ standard preparation, reagents Complete record of all data from testing Record of all calculations Statement of the test results; how compare with established acceptance criteria Signature of the person who performed each test; dates tests performed Date/ signature of second qualified person who reviewed original test records for accuracy, completeness and compliance with established standards Production System Training (documented; job-related) Master production and control records Batch production and control records Change control procedure Contemporaneous, accurate and complete batch production documentation Implementation and documentation of inprocess controls, tests, and examinations Production system (continued) Adequate written procedures & practice for charge-in of materials Identification of equipment with contents, stage of manufacturing, status Equipment cleaning records Established time limits for completion of production steps/stages Production system (continued) Deviations investigated and documented contemporaneously with investigation Process validation based on knowledge of process (scientific basis for identifying critical steps/critical process parameters/control points) Justification and consistency of in-process specifications and final product specifications Data/information documented and available to Quality Unit for review (trending, investigations etc.) Facilities & Equipment System FACILITIES Location, design, construction appropriate to facilitate cleaning, maintenance, operations Layout and air handling designed and constructed to prevent cross-contamination Flow of materials & personnel designed to prevent mix-ups or contamination Facilities & Equipment System Defined areas or other control systems to prevent mix-ups or contamination ¾ Incoming materials (id, quarantine) ¾ Sampling area (prevent contamination) ¾ Quarantine (intermediates, APIs) ¾ Released materials ¾ Rejection Facilities & Equipment System EQUIPMENT Appropriate design, size, location, non-reactive product contact surfaces Identification clearly marked Qualification (DQ, IQ,OQ, PQ) Calibration Preventive Maintenance schedule and procedures Cleaning procedures and validation Records of use, cleaning, maintenance Facilities & Equipment System Lubricants, heating fluids or coolants (not contact/alter product quality) Closed or contained equipment Inspection prior to use ***************************************** Separate facilities or containment where needed (penicillins, highly potent compounds etc.) Utilities Qualified and appropriately monitored; drawings should be available Designed and constructed to prevent contamination or cross-contamination Recirculated air to production (same concern) Permanently installed pipework should be appropriately identified Drains of adequate size with air break Water Process water at minimum meeting WHO guidelines for potable water Justify quality of water used to achieve stated API quality and establish specifications Water treatment facilities validated API to be used for incorporation into sterile dosage form – water used in later stages should be monitored and controlled for total microbial counts, objectionable organisms and endotoxins Materials System Written procedures for receipt, identification, quarantine, storage, handling, sampling, testing and approval or rejection of materials System to evaluate suppliers (critical materials) Purchased against agreed specification Change control process for changing suppliers Upon receipt check for correct labeling, seals Before co-mingling bulk material, id/test Assurances obtained from non-dedicated tankers Materials System Identification on large storage containers and associated manifolds, filling and discharge lines Code given to received batches; status identity At minimum, a specific identity test on incoming batches; COA Supplier evaluation should include three fully tested batches; one fully tested batch/year Written sampling plan with justification Prevent contamination of sampled containers Materials System Stored in manner to prevent degradation, contamination, no adverse effect on quality Drums, bags, boxes off the floor First in, first out Rejected materials identified and controlled under a quarantine system Established re-test/ re-evaluation periods Packaging & Labeling System Written procedures for receipt, identification, quarantine, sampling, examination and/or testing P&L P&L should conform to specifications Records maintained for each shipment (showing receipt, examination & result) Containers protective, clean, not alter product quality; if re-used, cleaned & labeling defaced Labeling Access to label storage area limited Written procedures for reconciliation; investigation if discrepancy All excess labels with batch #, destroyed Obsolete labels destroyed Printing devices controlled to insure accuracy of label (against batch record) Print labels checked against master and a copy placed into the batch record Packaging/Labeling Operations Documented procedures to assure correct packaging materials/ labels used Operations designed to prevent mix-ups Labels: API name, batch #, storage conditions Shipped API: Name/ address manufacturer; special transport conditions; expiry/ retest date Documented clearance before operations Packaged/ labeled intermediates or APIs examined as part of packaging (documented) Seal employed to assure package integrity APIs are Drug Substances FDA Food, Drug and Cosmetic Act definition of drug includes “articles intended for use in the diagnosis, cure, mitigation, treatment or prevention of disease in man or other animals” (no distinction between APIs & dosage forms) Before ICH Q7A, FDA used dosage drug regulations as guidance for API inspection Still true (see next slide) , however, ICH Q7A provides guidance on the application of those cGMPs to APIs) From current FDA Compliance Program 56002 for Drug Manufacturing Inspections: (This is the compliance program for FDA Investigators; this revision introduced Systems Inspections) “The cGMP regulations are not direct requirements for manufacture of APIs…….but they are guidance for cGMP in API manufacture.” Current FDA Compliance Guide on Process validation From FDA Compliance Policy Guide “Process Validation Requirements for Drug Products and Active Pharmaceutical Ingredients CPG 7132c.08”; revision date 12 March 2004: Validation of manufacturing processes is a requirement of the Current Good Manufacturing Practice (cGMP) regulations for finished pharmaceuticals, and is considered an enforceable element of current good manufacturing practice for active pharmaceutical ingredients (APIs) under the broader statutory cGMP provisions of the Federal Food, Drug, and Cosmetic Act”. Differences API/ Dosage Form APIs involve purification steps GMP controls tighter for later API steps API impurity profile is critical focus and steps which produce or remove impurities require greater control and validation Dosage forms do not involve purification Similarities APIs/Dosage Forms Require demonstrated knowledge of process and application of appropriate GMP controls to assure safety, identity, strength, quality and purity. Systems in control to be in compliance Life Cycle Approach to Validation (beyond the initial “conformance batches”) Similarities include…. Processes for specific products vary in complexity (either API or dosage can involve complex or simple processes) In-process controls Finished product controls Critical steps/ critical process parameters Process validation Quality assurance for consumer is based on understanding & control of sources of process/ product variability More Similarities….. Science based approach for the establishment of processes Knowledge of process based on Process Development work ¾ Design Of Experiments (DOE) ¾ Quality System (review/ trending) Continuous Improvement possible within well characterized process FDA CGMP China Training Program December 5-7, 2005 Ying Jie Convention Center Beijing University Beijing Solid Oral Dosage Forms Nicholas Buhay Deputy Director Division of Manufacturing & Product Quality Office of Compliance, CDER, FDA Oral Solid Dosage Forms/Michael O'Meara/ 2004 Solid Oral Dosage Forms Discussion of Manufacturing Considerations and Current Good Manufacturing Practice Oral Solid Dosage Forms/Michael O'Meara/ 2004 FORMS • • • • • Powders Pills Troche Capsules Tablets Oral Solid Dosage Forms/Michael O'Meara/ 2004 Most Common Dosage Forms • • • • • Convenient Relatively Stable Easily Administered Palatable Flexible Oral Solid Dosage Forms/Michael O'Meara/ 2004 Capsules • Hard Gelatin • Soft Gelatin Oral Solid Dosage Forms/Michael O'Meara/ 2004 Hard Gelatin Capsules • Empty Capsule Storage – Controlled temperature and humidity • Too moist - capsules become tacky • Too dry - capsules become brittle and change dimensions • 30 to 45% R.M. ideal Oral Solid Dosage Forms/Michael O'Meara/ 2004 Operations • • • • Rectify the capsule Separate body from cap Fill the body Replace the cap Oral Solid Dosage Forms/Michael O'Meara/ 2004 Capsule Filling Machine • Hand Operated • Semi-automatic • Fully automatic Oral Solid Dosage Forms/Michael O'Meara/ 2004 Oral Solid Dosage Forms/Michael O'Meara/ 2004 Oral Solid Dosage Forms/Michael O'Meara/ 2004 Process Variables • • • • • Speed Humidity Bulk Powder Level Weight Variation Gelatin Moisture Content Oral Solid Dosage Forms/Michael O'Meara/ 2004 Compressed Tablet • Un-coated • Immediate Release Oral Solid Dosage Forms/Michael O'Meara/ 2004 Multiple Compressed • Layered • Compression Coated – Tablet Within a Tablet – Two Part – Three Layer – Function as Film/Sugar Coated Oral Solid Dosage Forms/Michael O'Meara/ 2004 Repeat-Action Active ingredient in the tablet core and in the coating. Oral Solid Dosage Forms/Michael O'Meara/ 2004 Delayed-Action/Enteric Coated • Coating protects core in the stomach • Drug released in the upper GI tract after the stomach Oral Solid Dosage Forms/Michael O'Meara/ 2004 Film Coated • Solvent Based • Aqueous Based • Alternative to Sugar Coated Oral Solid Dosage Forms/Michael O'Meara/ 2004 INGREDIENTS • Active • Non-Active – Drug Substance – – – – – – – – Diluents Binders Lubricants Disintegrants Coloring Flavoring Antiadherents Glidants Oral Solid Dosage Forms/Michael O'Meara/ 2004 Drug Substance • Fully Characterized – Physical Specifications (Including Particle size distribution, density, isomerism and Morphology) – Chemical Specifications (Including Impurity and Degradation Profile) Oral Solid Dosage Forms/Michael O'Meara/ 2004 DILUENTS • • • • • Lactose Starch Mannitol Calcium Sulfate Sorbitol • • • • • Dicalcium Phosphate Kaolin Sodium Chloride Powdered Sugar Microcrystalline Cellulose Oral Solid Dosage Forms/Michael O'Meara/ 2004 DISINTEGRANTS • • • • • Starch Microcrystaline Cellulose Alginic Acid Gums Crospovidone Oral Solid Dosage Forms/Michael O'Meara/ 2004 Binders • • • • • • Starch Paste Glucose Gelatin Solution Acacia Sucrose Sodium Alginate Oral Solid Dosage Forms/Michael O'Meara/ 2004 LUBRICANTS • • • • • • Magnesium Stearate Calcium Stearate Talc Stearic Acid Sodium Lauryl Sulfate Sodium Acetate Oral Solid Dosage Forms/Michael O'Meara/ 2004 Observations Oral Solid Dosage Forms/Michael O'Meara/ 2004 -) Testing standards for raw materials used in the manufacture of ***** 40 mg tablets do not include specifications for physical characteristics. Oral Solid Dosage Forms/Michael O'Meara/ 2004 -) ***** raw material is not sufficiently characterized to determine its suitability for the manufacturing process. Various lots have passed all acceptance criteria, but have been identified as the causative factor in granulation and tableting deviations. Oral Solid Dosage Forms/Michael O'Meara/ 2004 -) …..The affect of particle size distribution, surface area and the particle morphology of the bulk drug substance, on the granulation process were not fully evaluated….. Oral Solid Dosage Forms/Michael O'Meara/ 2004 There was a failure by QA to identify two separate lots of diluted Isosorbide Dinitrate bulk drug substance, received from the supplier in the same shipment... Oral Solid Dosage Forms/Michael O'Meara/ 2004 -) The investigation into the acquisition and release of aluminum stearate of the wrong grade obtained from an unapproved source failed to identify that the wrong grade of material was ordered from the vendor. Oral Solid Dosage Forms/Michael O'Meara/ 2004 GRANULATING • Wet Granulation • Direct Compression • Dry Granulation – Slugging – Roll Compaction Oral Solid Dosage Forms/Michael O'Meara/ 2004 Wet Granulation • Advantages • Disadvantages – Improved Compressibility – Improved uniformity – Decreased segregation – Flexibility – Process complexity – Cost – Possible affect on drug substance Oral Solid Dosage Forms/Michael O'Meara/ 2004 Wet Granulation Manufacturing Steps W eighing Mixing Granulation Screening Drying Screening Lubrication Compression Oral Solid Dosage Forms/Michael O'Meara/ 2004 Wet Granulation • Specific Manufacturing Instructions • Amounts, Rates and Timing of Granulating Fluid Additions • Mixer Speeds and Configuration • Specified End Points - Motor Load, Appearance, Texture Oral Solid Dosage Forms/Michael O'Meara/ 2004 FDA 483 Observation ...some granulation batches have required on the spot changes in established procedures for water addition and/or mix time to compensate for over and under granulation problems, the addition of a wet milling step or hand processing to break up lumps in over granulated batches, an additional drying step... Oral Solid Dosage Forms/Michael O'Meara/ 2004 Dry Granulation • sensitive to • Useful when ingredients are moisture or heat • Blended ingredients are either compressed into “slugs” or roll compacted into “sticks” or sheets • Slugs or sticks are screened/milled • Granulation is blended with lubricant and disintegrants then compressed Oral Solid Dosage Forms/Michael O'Meara/ 2004 Roller Compactor Oral Solid Dosage Forms/Michael O'Meara/ 2004 Direct Compression • Ingredients are milled and/or screened, then mixed, then compressed into tablets. • Few Manufacturing steps • Greater potential for segregation Oral Solid Dosage Forms/Michael O'Meara/ 2004 Mixers & Blenders • • • • • Pony/Planetary Mixer High Shear Mixer Ribbon Blender Screw Blender Tumble Blenders – – – – Twin Shell Double Cone Drums Other Oral Solid Dosage Forms/Michael O'Meara/ 2004 Mixing Process Validation • Validation of the reliability of mixing operations is a very significant control expected • Sample from the blender (if possible) • 10 individual assays • Sample size – Approximate unit dose Oral Solid Dosage Forms/Michael O'Meara/ 2004 Planetary Mixer • Good horizontal mixing • Cross contamination risk • Poor vertical mixing Oral Solid Dosage Forms/Michael O'Meara/ 2004 Oral Solid Dosage Forms/Michael O'Meara/ 2004 Oral Solid Dosage Forms/Michael O'Meara/ 2004 Ribbon Blender • Horizontal and vertical mixing • Dead zones • Cleaning issues Oral Solid Dosage Forms/Michael O'Meara/ 2004 Oral Solid Dosage Forms/Michael O'Meara/ 2004 Oral Solid Dosage Forms/Michael O'Meara/ 2004 Oral Solid Dosage Forms/Michael O'Meara/ 2004 Screw Blenders • Three Distinct Intermixing Action – Screw produces lifting action – Orbiting screw moves material from the walls of the blender into the center of the vessel – Material lifted by the screw gravitates downward – No picture Oral Solid Dosage Forms/Michael O'Meara/ 2004 Tumble Blenders • Shell blenders • Twin Shell and Double Cone – Low energy mixing • clumping and segregation – Working capacity – Cleaning – Liquid Dispersion Granulation Oral Solid Dosage Forms/Michael O'Meara/ 2004 Oral Solid Dosage Forms/Michael O'Meara/ 2004 Oral Solid Dosage Forms/Michael O'Meara/ 2004 Oral Solid Dosage Forms/Michael O'Meara/ 2004 Oral Solid Dosage Forms/Michael O'Meara/ 2004 High Shear Mixers • Very efficient • Ideal for wet granulation • Amount and addition rate of granulating fluid must be strictly controlled • End points can be measured • Single pot production • Heat • Cleaning Oral Solid Dosage Forms/Michael O'Meara/ 2004 Oral Solid Dosage Forms/Michael O'Meara/ 2004 Oral Solid Dosage Forms/Michael O'Meara/ 2004 OTHER BLENDERS • Drum • Bags Oral Solid Dosage Forms/Michael O'Meara/ 2004 Inspection Observations Oral Solid Dosage Forms/Michael O'Meara/ 2004 there were no blend time studies conducted to assure uniformity of granulation for the pre-blend or final blend steps…In addition, production batch records do not specify a finite time for blend steps. Oral Solid Dosage Forms/Michael O'Meara/ 2004 one of six granulation samples obtained from the blender, at final blend step, assayed below specification. Oral Solid Dosage Forms/Michael O'Meara/ 2004 - Content uniformity of the preservative was not included in the validation study for ***. Oral Solid Dosage Forms/Michael O'Meara/ 2004 - During the processing of *** 500mg tablet batch ***, an operator was observed inverting a drum of granulation several times prior to placing it above the tablet press granulation hopper. This step is not part of the established process, but is reportedly common practice. Oral Solid Dosage Forms/Michael O'Meara/ 2004 - ******* 40 mg tablets are not manufactured in accordance with the approved filed process. The current manufacturing process includes an additional 5 minutes of blending with intensifier bar prior to the granulation step, an additional 3 minute blending step (drum mix) during the tableting operation, and pre-compression and dissolution evaluation steps, none of which are represented in the filed process. Oral Solid Dosage Forms/Michael O'Meara/ 2004 DRYING • Fluid Bed • Tray • Vacuum Oral Solid Dosage Forms/Michael O'Meara/ 2004 Fluid Bed Drying • Efficient • Uniform drying • Process Variables – Temperature – Air velocity – Filter pore size Oral Solid Dosage Forms/Michael O'Meara/ 2004 Fluid Bed Granulating • Process Variables – Droplet size and spray rate – Inlet air temperature, humidity and velocity – Location of spay nozzle Oral Solid Dosage Forms/Michael O'Meara/ 2004 Oven/Tray Drying • Drying is less uniform than with fluid bed • End point determination • Cross contamination issues • Cleaning Oral Solid Dosage Forms/Michael O'Meara/ 2004 Vacuum Drying • Jacketed tumble dryer • Heat applied to vessel walls • Vacuum draws off moisture/solvent Oral Solid Dosage Forms/Michael O'Meara/ 2004 Oral Solid Dosage Forms/Michael O'Meara/ 2004 Oral Solid Dosage Forms/Michael O'Meara/ 2004 Milling • Process Variables – – – – – – Feed rate Inlet feed throat design Blade type Rotor speed Screen type (Overhead) Oral Solid Dosage Forms/Michael O'Meara/ 2004 Transfer & Storage • • • • • Post blending segregation Floor vibration Chutes and collars Equipment Vibration Segregation ???? Oral Solid Dosage Forms/Michael O'Meara/ 2004 Compression • Start up tablets • In process testing – – – – – – hardness friability size shape disintegration thickness Oral Solid Dosage Forms/Michael O'Meara/ 2004 Tablet Presses • • • • Single Punch Rotary Press High Speed Rotary Press Multi-layer Rotary Press Oral Solid Dosage Forms/Michael O'Meara/ 2004 Oral Solid Dosage Forms/Michael O'Meara/ 2004 Tooling • Quality Control • Accountability – unique identifier – security Oral Solid Dosage Forms/Michael O'Meara/ 2004 Oral Solid Dosage Forms/Michael O'Meara/ 2004 Oral Solid Dosage Forms/Michael O'Meara/ 2004 Problems • Sticking and Picking – granulation moisture – lubricant – punch face • Capping – Fines – Air – punch-die clearance Oral Solid Dosage Forms/Michael O'Meara/ 2004 Problems • Lamination • Chipping & Cracking – Tooling – granulation procedure – formulation • increase binder • lubricant – tooling – granulation • fines • granule size Oral Solid Dosage Forms/Michael O'Meara/ 2004 Common controls • Hardness • Friability – Force required to break a tablet – Ability to withstand abrasion and trauma without crumbling Oral Solid Dosage Forms/Michael O'Meara/ 2004 Common controls • Disintegration • Dissolution – The time it takes for a tablet to disintegrate in an aqueous medium – How the formulation releases the drug Oral Solid Dosage Forms/Michael O'Meara/ 2004 Inspection Observations Oral Solid Dosage Forms/Michael O'Meara/ 2004 The investigations into a capping problem associated with seven production batches of XXX Tablets identified by MDIR's for one year are incomplete, in that; there was no evaluation of the granulation nor of the raw materials used. Oral Solid Dosage Forms/Michael O'Meara/ 2004 The manufacturing process for XXX Extended Release Tablets is not validated in that : a) the 45 station Stokes BB2 rotary tablet press (firm's ID # xxx ) was not qualified to assure the capability and controls for this piece of equipment were suitable to meet requirements established for manufacture of this product. Oral Solid Dosage Forms/Michael O'Meara/ 2004 MDIR's were not generated, nor investigations conducted to determine cause, identity of content, and quantity of "chunks" of granulation which had to be occasionally removed from the tablet press screen during compression of xxx, batch xxx, nor of "lumpy" granulation observed in the hopper of the press during granulation of xxx, batch xxx. Oral Solid Dosage Forms/Michael O'Meara/ 2004 - Development history supports an in-process disintegration limit lower than the current value of < 15 min. An unusual dissolution profile in a development batch was associated with in-process disintegration times > 9min. Oral Solid Dosage Forms/Michael O'Meara/ 2004 - The ***** 40mg tablet manufacturing process is not validated in that: a) Tableting parameters are set batch to batch based on precompression dissolution test results. Oral Solid Dosage Forms/Michael O'Meara/ 2004 b) Critical physical characteristics of raw materials have not been identified. c) Validation lots did not include specifications for the physical characteristics of blends and granulations. Oral Solid Dosage Forms/Michael O'Meara/ 2004 d) Final blend samples taken for physical characteristics analysis were composite. Oral Solid Dosage Forms/Michael O'Meara/ 2004 - The agency was not notified, in accordance with NDA Field Alert reporting requirements, when it was determined that lot **** failed dissolution testing at the 1 month stability station. Oral Solid Dosage Forms/Michael O'Meara/ 2004 - The operating speed for the Perry Powder Filler when filling XXX is listed as 95 bottles per minute (BPM) in the Line Set-up Standard Sheet, which is outside the 80 to 90 BPM range used in the validation batches. Oral Solid Dosage Forms/Michael O'Meara/ 2004 COATING • • • • • Protect drug from the environment Mask taste Improve appearance Separate ingredients Provide multiple release profiles Oral Solid Dosage Forms/Michael O'Meara/ 2004 Equipment • Standard coating pan • Perforated coating pan • Fluidized bed Oral Solid Dosage Forms/Michael O'Meara/ 2004 Standard Pans Oral Solid Dosage Forms/Michael O'Meara/ 2004 Oral Solid Dosage Forms/Michael O'Meara/ 2004 Perforated Pans Oral Solid Dosage Forms/Michael O'Meara/ 2004 Fluid Bed Oral Solid Dosage Forms/Michael O'Meara/ 2004 Types • Film • Enteric • Sugar Oral Solid Dosage Forms/Michael O'Meara/ 2004 Film Coating Materials • Polymers - Hydroxypropyl methylcellulos Povidone Polyethyleneglycol • Enteric Materials Cellulose acetate phthalate Oral Solid Dosage Forms/Michael O'Meara/ 2004 Sugar Coating Materials • Sealant - Shellac • Sugar - Syrup and color Oral Solid Dosage Forms/Michael O'Meara/ 2004 Process Variables • • • • Pan design Pan speed & load Air quality Temperature • • • • Airflow rate Spray rate Spray pattern Nozzle to bed distance Oral Solid Dosage Forms/Michael O'Meara/ 2004 There are no written SOP's for conducting batch record reviews to assure consistency and completeness of those reviews... Oral Solid Dosage Forms/Michael O'Meara/ 2004 A sticky note, attached to the official lab report, both dated with the same day, contained unacceptable test results of an individual tablet relative to a dissolution profile test conducted during the initial validation batch xxx, for product XXX. The values for this tablet were not included on the final lab report. Oral Solid Dosage Forms/Michael O'Meara/ 2004 - 80% of the Aluminum Stearate used in the formula for ***** lot ***** was an unapproved grade obtained from an unapproved source. This lot has been distributed. The following two lots, ***** & *****, which were manufactured using 100% of the unapproved material were rejected for failing to meet specification. Oral Solid Dosage Forms/Michael O'Meara/ 2004 - There was no investigation conducted following the rejection of 86 kg of XXX 40mg tablets from lot ***** (a post validation lot) when the 2 hour compression trial sample failed dissolution testing; there was also no QA Management evaluation of the incident or its impact on the validation status of the process. Oral Solid Dosage Forms/Michael O'Meara/ 2004 The local Quality Unit review has failed to assure the accuracy and completeness of validation reports, manufacturing documents, and analytical reports. For example:... Oral Solid Dosage Forms/Michael O'Meara/ 2004 The local QA unit failed to follow the procedure (***.*) to notify senior corporate officials of significant quality issues so that resources could be allocated to resolve problems... Oral Solid Dosage Forms/Michael O'Meara/ 2004 Laboratory procedures do not provide for the expeditious analysis of stability samples that require multi stage testing. For example, stage one dissolution testing for stability sample *** was initiated on August 9, but stage three testing, indicating a stability failure, was not completed until October 5. Oral Solid Dosage Forms/Michael O'Meara/ 2004 Specifically, the manufacturing process for lots of *** mg tablets manufactured between *** and *** was not validated in that approximately 9 of 39 lots were rejected due to dissolution failures. Changes made to the manufacturing process during this time did not resolve the dissolution failures. Approximately 21 lots manufactured during this time were released for commercial distribution. Oral Solid Dosage Forms/Michael O'Meara/ 2004 Summary • Process Analysis • Process Variables • Process Controls Oral Solid Dosage Forms/Michael O'Meara/ 2004 Summary • • • • • • • Evaluate material Evaluation of site for cross-contamination Consider operations (steps) in process Consider equipment for operations Determine process controls Demonstrate process reliability (validation) Commit to continuous monitoring of manufacturing experience Oral Solid Dosage Forms/Michael O'Meara/ 2004 Inspection References Oral Solid Dosage Forms/Michael O'Meara/ 2004 GUIDE TO INSPECTIONS OF DOSAGE FORM DRUG MANUFACTURER'S - CGMP'S October, 1993 Oral Solid Dosage Forms/Michael O'Meara/ 2004 GUIDE TO INSPECTIONS OF ORAL SOLID DOSAGE FORMS PRE/POST APPROVAL ISSUES FOR DEVELOPMENT AND VALIDATION January, 1994 Oral Solid Dosage Forms/Michael O'Meara/ 2004 GUIDE TO INSPECTIONS VALIDATION OF CLEANING PROCESSES May 1987 Oral Solid Dosage Forms/Michael O'Meara/ 2004 GUIDE TO INSPECTIONS OF PHARMACEUTICAL QUALITY CONTROL LABORATORIES July, 1993 Oral Solid Dosage Forms/Michael O'Meara/ 2004 EXPIRATION DATING AND STABILITY TESTING FOR HUMAN DRUG PRODUCTS Inspection Technical guide 41 (http://www.fda.gov/ora/inspect_ref/itg/itg4 1.html) Oral Solid Dosage Forms/Michael O'Meara/ 2004 CGMP Guidance: Answers to Frequently Asked Questions Notes Human Drug CGMP Notes (3/1995-7/2000) • Human Drug CGMP Notes (1/1993-12/1994) – – – – – – – – [CNOTES vol. 1 no. 1 Feb 1993] [CNOTES vol. 1 no. 2 May 1993] [CNOTES vol.1 no. 3 Sept 1993] [CNOTES vol.1 no. 4 Dec 1993] [CNOTES vol. 2 no. 1 Mar 1994] [CNOTES vol. 2 no. 2 Jun 1994] [CNOTES vol. 2 no. 3 Sep 1994] [CNOTES vol. 2 no. 4 Dec 1994] ►TO FIND, GO TO WEBSITE: http://www.fda.gov/cder/dmpq/index.htm Other Resources • Guidance for Industry: CGMPs (Pharmaceutical CGMPs for the 21st Century) – Questions and Answers on Current Good Manufacturing Practices (cGMP) for Drugs (Posted 8/4/2004) ►TO FIND, GO TO WEBSITE: http://www.fda.gov/cder/guidance/cGMPs/default.htm Oral Solid Dosage Forms/Michael O'Meara/ 2004 Good Luck!! • Think soundly • Operate under control Oral Solid Dosage Forms/Michael O'Meara/ 2004 FDA API Inspections Robert C. Horan, PhD FDA Pharmaceutical Inspectorate New York District Quality System observations FDA 483 Observations for Product Quality Reviews range from: No SOP for Product Quality Reviews No Product Quality Reviews conducted to: various components of the reviews not done inadequate investigations no corrective actions or other conclusions Quality System observations Regarding the annual product reviews: The reports do not identify the specific batches which were covered by the review period and there is no evaluation of specific data from the batches covered. The annual report from 200X was found to contain some conclusions regarding out of specification data and corrective actions without providing specific information such as batch numbers, actual events, specific data, conclusions and any specific corrections made. Quality System observations An example is on page 3 which states: “The main unqualified item in 200X is the XXX content out of the specific range. We take relative measures to strengthen the control of manufacturing process, training the workers, strengthening the workers’ quality sense”. Quality System observations Many of the firm’s written procedures (SOPs) have not been periodically reviewed and revised where needed to ensure that they accurately describe current procedures at the firm and are in compliance with cGMPs. Some of the SOPs were found to have approval dates as far back as 1994. Examples include but not limited to: a) **********, revision 1, approved 10 Jan 1994 b) XXXXXXXXX, revision 1, approved 23 March 1998 Further, review of SOP XX found that it describes equipment which had been removed two years ago and the attachments “C” and “D” are no longer used for documentation and were replaced by other forms which were not attached to the SOP. Quality System observations From a Warning Letter: “Failure to establish corrective and preventive actions (CAPA) procedures for investigating the cause of non-conformities relating to product, processes and the quality system. Specifically, the firm received – complaints related to……. You failed to follow SOP # -- in that investigations were inadequate and no CAPAs were implemented. Quality System observations Change control forms for changes in Master Batch Production records fail to identify specific changes made. Further, there is no written evaluation of the significance of the change, need for re-validation etc. Quality System observations Software change control reports were found to have multiple text changes made by means of “white-out” rather than by following the firm’s written procedure of crossing out the original text and initialing (stamp) the correction. Further, there were no written explanations given for the specific changes made. Quality System observations There is no control over the use of signature stamps by production and quality control personnel used in the signing of documents. Quality System observations Process validation reports for API *** did not have criteria for acceptable reduction of the two specified impurities “eimp” and “fimp”. Batch record review (20 consecutive batches) found that post-validation batches showed typical levels of both impurities were much higher than in the validation batches. A number of batches exhibited “eimp” values that were more than double that in validation batches and approached the limit of 1.0%. Quality System observations SOP “QA Inspector in the Workshop” describes a twice daily check of equipment readings versus data recorded in batch records. Examination of several entries in the QA inspector’s log and corresponding batch records from those same dates/times found discrepancies between the QA inspector’s record and batch record data. Quality System observations Further, on (date), the QA inspector recorded a temperature of 0 C for the critical **** reaction step ------ for batch ***, however, my examination of the batch record found that for that step which lasts 5 hours, the temperature never reached 0 C. In fact, the critical temperature range is 12 to 20 C and examination of 25 batch records close to dates for batch *** found 1) Examples of temperature exceed upper limit 2) No batches recorded a temperature of 0C. Cited on warning letter The firm’s procedures for identifying and documenting problems that occur in manufacturing are deficient. For example, 235 “minor” deviations were logged year-to-date, of which only one was fully documented as a deviation investigation. Minor deviations that were not fully investigated and documented included: Quality System observations 1) API ^^^ production lot *** failed to form final product crystals. The cause was attributed to an operator error and the charging of excess solvent. Non-validated measures were used to attempt to force the formation of crystals. The in-process lot was subsequently divided into thirds and blended into three other production lots that became finished API ^^^ lots ***, *** and ***. This was listed as a minor deviation and a full investigation was not performed. continued 2) API ^^^ production lot *** yielded only 57%. The yield was approximately 30% below average. The cause was attributed to an initial high processing temperature caused by the computer system. No additional information or justification was provided; this was listed as a minor deviation and a full investigation was not performed. Quality System observations Review of a number of “oos” for potency in API ***, it was found that this was attributed to failure of temperature sensors on manufacturing equipment XXX and that the temperature had been out of the critical control range. In reviewing other deviation reports, it was found that following earlier episodes of “oos” potency values, there were corrective actions recommended including one to increase the frequency of calibrations of the sensing devices. Examination of the applicable SOPs found these recommended had not been implemented and no other corrective action taken. Quality System observations Action limits for testing of Purified Water have been exceeded several times without any investigations or completion of non-conformance reports. The test results were included in the Purified Water System Qualification report dated (date). For example, Use Point XX sampled on (date), results were “Unsatisfactory” for absence of clinically significant organisms (pathogens), User Point YY sampled on (date, three months earlier) had Total Viable Counts which were more than 10 times the action limit of X cfu/mL. This data was recorded in the final report signed by quality management. Quality System observations The written procedure (SOP XX-Y) for training of employees does not address the conduct of job specific, performance based training and there is no documented record of such training for quality control laboratory and production personnel. Inspection found many production deviations where the cause was reported to be operator error and retraining was conducted. SOP XX-Y does not address the retraining of personnel and there is no documentation of retraining. There are no individual training records for personnel. Laboratory observations Calibration of pH meter #__ is done using buffers at pH 4.0, 7.0 and 9.0, however, it is used to measure the pH of *** which has an expected pH around 12. Balance # ___ used in the testing of *** is calibrated at ___ intervals using weights in the range *-*, however, sample weights as per the method for testing of *** are considerably below the lower end of the calibration. Laboratory observations The identification test used for XX@-Na by FTIR compared the spectrum of XX@-Na against the spectrum for USP XX@. These spectra are not equivalent and are in fact quite different. Identification testing of API *** batches …,…,…,…,… using IR was not actually done. The analyst simply used a previous spectrum and changed the batch number each time. Laboratory observations Regarding the computerized and paper systems used in the recording of quality control testing data for chemistry, microbiology and in-process production testing the following was observed: a) The computerized (LIMS) system is not secure in that it is possible for data to be changed. This was observed following a request during inspection for a challenge to be performed. In performing the requested challenge, the analyst was able to change previously recorded input including sample gross and net weights resulting in changed assay results. Laboratory observations b) There is no system such as the use of pre-coded sheets, signed and distributed by a responsible quality employee for assuring the integrity of loose paper data sheets used in the recording of test results Laboratory observations Inspection of the QC and Microbiology laboratories found that analysts use loose printed sheets for recording raw data, there were stacks or pads of blank pages readily available. In the microbiology laboratory, in response to a question about how the name of the product is stamped on the data page, an analyst took out a stamp and ink pad and demonstrated how it would be done. There is no procedure in place to insure the integrity of data sheets used in the QC laboratory. Laboratory observations Examination of the HPLC systems in the API testing laboratory found that for the *** systems, the audit trail function was not enabled. For the *** HPLCs, the audit trail function was enabled, however, the laboratory management has never conducted an examination of the audit trail on any of these instruments. No training of analysts regarding audit trail. Laboratory observations Generic Statement – details withheld FDA inspections sometimes find evidence of data in computer files which is not recorded in laboratory notebooks, lab worksheets or final written reports. Laboratory observations The firm’s QC chemistry laboratory has three HPLC systems and reportedly tests about 2000 samples per year, however, the calibration is done only once every two years (by government agency). There is no established basis for not conducting more frequent full equipment calibration related to the high equipment usage. Laboratory observations Note: At least several FDA 483s have cited observations regarding incomplete information provided on certificates following their calibrations. It has also been cited several times that the factories receive no other information and that it is not possible for an adequate review to be done of the instrument calibration – either by the factory or outside auditor - such as FDA). Laboratory observations Calibration of HPLC is inadequate in that the lamp energy was not determined to assure that it is capable of detecting low concentration of impurities during impurity determination. Laboratory observations System suitability is not performed each time the HPLC assay method is run. The firm has conducted system suitability only once in the history of testing API***. The firm does no conduct system suitability each time testing is done as per USP. Laboratory observations The firm has not demonstrated that the assay method used for stability testing of API *** is stability indicating. Laboratory observations There is no data available from the forced degradation studies which serve as the basis for demonstrating that the stability test method for testing of API stability samples is stabilityindicating. The management stated that at the time the studies were conducted in 200X, the factory was not retaining raw data. (continued) Laboratory observations Further, there is no record of preparation of samples, sample stress treatments or the actual testing. Finally, there is no record of the subdividing of stressed samples to prepare a sub-sample to be sent to a contract laboratory for the peak purity studies. Laboratory observations For the related compounds methods for *** API, the procedure states to run the chromatogram for NLT 2.5 times the retention time of the API. Review of earlier test data shows that a significant recurring impurity elutes at approximately five times the retention time of the API, which could go undetected when following the instructions for chromatographic run time. Laboratory observations For several tests from the USP monograph for API ^^^, USP, the firm either did not perform the test or did not conduct it as per USP. For example, the UV identity test was not done and the IR identity scan in the batch records was simply a copy of a “representative” batch run previously; “the test for the specified impurity 4XXXXX was not conducted for any of the batches examined (batches ***, *** and ***) and the “Crystallinity” test was not done. Laboratory observations The firm’s “out of trend” (“OOT”) investigation for stability testing on three consecutive validation batches ****1, ****2 and ****3 concluded that the “OOT” result was due to analyses being conducted by different analysts on different instruments. The following is noted: The analysts were also reportedly trained and the instruments calibrated and deemed acceptable for the testing There is no documented basis for the investigation conclusion The conclusion suggests the method is not robust, however, the investigation did not address the significance for all other previous testing Laboratory observations For the related compounds method for ***, several errors exist in the procedure that were not detected during the review process. These include the incorrect concentration listed for the stock standard and the incorrect dilution for the low level standard preparation. Laboratory observations Following an out of specification result for *** in the 6 month stability sample of ***, lot ***, the analyst reported that the "Test FAILED" on the report sheet and forwarded this to the group leader, however, no action was taken. According to the laboratory manager, the sheet must have been missed and was not discovered for more than two months. Laboratory observations There is no written procedure which requires the investigation, review and trending of laboratory deviations not covered by “oos” investigations. Inspection of product *** found that there were HPLC assays discontinued when an outdated reference standard solution introduced unknown peaks. The firm has stability data for 15 days use of *** reference standard solution and supervisor stated “We would not normally use such an old solution. It was done because standard is expensive”. “oos” The firm’s investigation of “oos’ test results for assay,, related substances and residual solvents for the two consecutive batches *** and *** of API ^^^ was limited to verifying that there was no laboratory error and the results were valid. There was no evaluation to determine the root cause of the multiple critical specification failure, no extension of the investigation to consider the potential significance for other batches. The only further action taken was to reprocess the batches and sell them to the local market instead of U.S. “oos” The firm received complaint of batches **** and *** of the API product ^^^ failing the related substances test for the single largest related substance. The API manufacturer investigated the original test records from (date) and found that the analyst had selected the wrong peak as the largest related substance peak. The investigation was not extended to other batches. Review during the current inspection of test results from other batches found that the same analyst made the same mistake for several other batches. This had not been discovered by the API manufactuer’s investigation. “oos” Inspection found that an “oos” for potency of API ^^^, lot *** was invalidated based solely on the testing of a new sample. Examination of the firm’s SOP PP-T, found the following regarding the procedure for “oos” investigations: a) If an identified cause for the “oos” is not determined or not confirmed, then a second analyst will test a new sample. b) If the second sample meets specification, the conclusion is made that the original sampling was flawed. (continued next slide) “oos” c) d) If the new sample failed, only then would the lab supervisor prepare an “oos” reporting form which would be copied to production, QC and QA. The SOP does not address retesting the original sample. “oos” Regarding the firm’s procedure for investigation of “oos” test results: a) There is no log, file or other cumulative record of the firm’s “oos” investigations. b) The annual product reviews do not include review of these investigations. c) There is no time frame identified in the SOP for completion of “oos” investigations. “oos” (From an FDA letter sent to factory to indicate inadequate written response to FDA 483): Specifically, we remain concerned regarding the consistency of the manufacturing process and/or analytical procedures. The inspection revealed numerous “oos” assay results in different samples from batch *** as well as “oos” for two other batches within the same campaign. Some of the “oos” values were attributed to analytical error but the cause of others remain undetermined. (continued next slide) “oos” Your written response indicates that the “oos” investigations will be closed out within 30 days and that new laboratory SOPs have been written, training has been provided to laboratory personnel, and additional laboratory personnel have been recruited. Please provide the documentation that the “oos” investigations have been completed and that the cause of the “oos” assay results have been identified as either process related or analysis related. (continued next slide) “oos” Please address any process or analytical changes which may have been necessary to address this issue. Facilites & Equipment The firm’s written procedures for preventive maintenance (PM) do not include examination and evaluation of all equipment components or schedule for replacement of parts. In this regard, there were three batches (***, *** and ***) which were reported in the annual product review to be contaminated with particles from a shredded Teflon gasket associated with the --mixer. Inspection found: (continued…..) Facilites & Equipment a) b) There was no extension of the investigation to determine if previous batches may have been contaminated. In addition, the investigation does not document the identification of the contamination being consistent with Teflon particles. The engineering management stated that while they are responsible for equipment maintenance, they have no PM procedures and stated PM should be the responsibility of production. Facilites & Equipment c) d) There are no PM SOPs in the production department. The production department has a machine log for each piece of equipment, however, review of the machine log for the mixer found no record of the Teflon gasket replacement in the period following the reported contamination. Facilites & Equipment The investigation into lots of API ^^^ returned due to the presence of metallic particles does not include a measure to prevent future recurrence. Please note: The following two slides list other observations on that same FDA 483. Facilites & Equipment Facilities & equipment in which crude APIs are exposed during processing are not maintained in a clean and sanitary manner and are not designed to prevent contamination of the crude APIs from foreign particles like dirt, rust, dust, paint chips and metal. Facilites & Equipment Then 483 lists a number of examples…..transfer of crude API from ----- reactor to centrifuge is performed underneath a metal platform in a building which is open to the outside; transfer to the multimill is performed in a room with peeling and flaking paint on walls/ ceiling; inside of the multimill granulator is corroded toward the bottom of the chute and was missing knives; interior of the vacuum dryer for crude API is rusted; transfer room of API to drums has peeling/ flaking paint on wall/ceilings. Facilites & Equipment In the warehouse for storage of replacement parts such as valves for the process water system and reverse osmosis membranes, there were numerous pigeons observed flying above the equipment parts and evidence of bird droppings. This included in the locked cage which contained the stored reverse osmosis membranes. Facilites & Equipment There are no piping or instrument drawings of the incoming source water, deionized water or Ultrafiltration Water systems to show current “as-built” components, treatment or distribution systems of water, for the purpose of system maintenance, monitoring and operation. Facilites & Equipment Welds used in the initial installation or replacement of critical equipment components are not examined, not electropolished or in any other manner evaluated against acceptance criteria. Several investigations of microbial contamination implicated residual weld material as a principal contributing factor. Facilites & Equipment There is a dead leg of at least 1 foot in length between the crystallization vessel XX (for purified API) and the centrifuge. (Note: This was from a previously used connection to another piece of equipment – no longer is use – now capped) Facilites & Equipment The firm recently introduced and qualified a new delivery system for nitrogen blanketing of a critical step in the *** process. The system including new valves and flow meters was qualified as reported in IQ, OQ reports. Facilites & Equipment Inspection on (date) found that although the replacement valves associated with lines X and Y were closed, the nitrogen flow meter display indicated a significant nitrogen flow to line X. (NOTE: The initial change was made to deal with intermittent flow problem. Following the inspection, the firm determined that the new valve design was faulty/ not appropriate for the intended use and replaced all of the valves). Facilites & Equipment Equipment cleaning deficiencies include: a) Product residues were visible in numerous pieces of equipment labeled as clean (including fluid bed dryers, centrifuges; one vessel which was stated to have not been used in several weeks had yellow-brown residue, no status label) Facilites & Equipment b) c) Tape on discharge chutes of centrifuges and other surfaces with potential for product contact. There were rough welds on the product contact surface of the hopper used to charge purified product to the dryer. (Risk for next batch ? Degradants ?) Facilites & Equipment According to the firm’s written procedure (SOP XX-Y), the cleaning of Sparkler filters requires that at the completion of a campaign, the equipment is dismantled and all components thoroughly cleaned. Examination of Sparkler filters #s *** and *** found the bolts to be worn/ stripped. Facilites & Equipment The firm’s maintenance employees in the presence of the plant manager and the FDA investigator were unable to remove the bolts using dedicated tools. The firm has no individual equipment cleaning record and the batch documentation records only that all equipment in the “train” was cleaned. Facilites & Equipment The Ultra-Filtered (UF) Water system which produces water used in the critical steps of API production was observed to have ball-type valves at numerous locations including in the finishing area for the final API ******. These valves are potential “dead-legs” in the UF Water system. (API ****** is intended to further processing to manufacture sterile products for injection.) Facilites & Equipment The piping throughout the purified/UF water system is ABS plastic pipe and elbows and the line leading to the stainless steel holding tank (ABS) attaches to a stainless steel line by means of a flange. It was stated that the water in the line before the storage tank is drained at times when the system is not producing water, however, it was noted that the ABS line to the flange slopes in a manner which would not promote adequate drainage and, therefore, could promote biofilm production. Production observations The firm’s SOP XX states that batch production records for use in production are photocopied from the master record, however, examination of executed batches found that: • Batch production records are not an accurate reproduction of the master. • The following steps lacked instruction details given in the master records: (6 examples listed on FDA 483) Production observations This observation was on FDA 483 and then cited in a letter from FDQ CDER to firm: “The master production and batch production records for APIs ***, ^^^ and +++ are deficient in that they do not require documentation of all significant steps and in many cases are unclear. (Ten examples given on FDA 483).” Production observations From an FDA 483: Stage IV master production record does not specify the mill speed nor the screen to be used during milling and this information is not recorded in the batch record. Additionally, the master record does not specify the screen to be used during seiving. Production observations From Regulatory Letter: We also have concerns regarding particle size specifications in which all four prospective validation batches failed to meet the release specification. Note: The letter then reports the fact that inspection found that firm actually used different equipment from that described in manufacturing instructions and validation protocol. Production observations In the crystallization step to obtain crude ***, the manufacturing instructions state to add 100 Liters of xxx dropwise within 5 to 10 minutes. When it was pointed out that this would be more than 3000 drops per second (in 10 minutes) and that the same instruction is given in the (original language version), the firm’s (management title) stated that discussion with the production personnel found that this is accomplished “roughly” in the time period mentioned in the batch record by means of a valve. Production observations It was noted that, in contrast to other manufacturing steps which provide details, there is no instruction regarding use of valves or other means of controlling the flow. (Note: There was suggestion at one point that the word “dropwise” came from pilot scale batches but no documented evaluation of the criticality of the rate of addition and how “dropwise” should have been converted to an accurate instruction for the scaled-up batches). Production observations Inspection of first batches of new product *** found that the first batch failed specification for --- and this was related to a critical step. Batch rejected. Corrective action, change critical process step time from 20 minutes to 30 minutes. (see next slide) Production observations Examination of batch records for product +++ which has similar critical step states in the manufacturing instruction: “ Perform operation --- for twenty (30) minutes”. There is no record of the actual time it took for the operation, yet every batch record has two signatures verifying step done as described. Production observations From Warning Letter (“***” from FDA not by RCH) Several batches of API are *** in a *** to produce one large batch. The individual batches are not tested for residual solvents and found to meet appropriate specifications prior to ***. This process has not been validated for *** of the combined batch. The *** is tested for residual solvents, but the sampling method, one composite sample, does not provide evidence of ***. Production observations Inspection of the manufacturing facility on (date) at (time) found that while the two batches of ***, lots ----- and ----- had just begun the XXXXX step, the BPRs were signed by two operators verifying that the 9 step process had been completed. Further, the production QA employee signed the sheet stating that the above was reviewed and approved. Production observations Examination of reactor GLR # XXX in use for the ****** step (critical step) for batch $$$$$ of the API ***** found that the thermometer which extends into the reaction mass could not be read. The QA Manager who was accompanying the inspection examined the batch record for that batch, then leaned forward, examined the thermometer and stated that the temperature was XX C which she stated was “right on target”. (continued) Production observations I asked for the production manager to examine the thermometer and it was determined that not only could it not be read, the thermometer bulb was broken and the fluid had emptied. It could not be determined when the thermometer had broken nor where the contents of the thermometer had gone. Production observations Inspection found that the initial production deviation report # D-XX stated that batches ##### and +++++ of the product *** from a campaign in (time period) were rejected due to failing potency results. An amended deviation report prepared just the week before the current inspection reported that operators admitted to not adequately monitoring the critical step X.00Y and simply recorded results typical of previous batches. (continued) Production observations The amended deviation report: a) Failed to explain how the workshop supervisor was able to sign the batch record stating that he had observed the monitoring of the batches and that it had been done as per written instructions b) Failed to document an extension of the investigation to determine if there were other batches for which the operators had not properly monitored and documented the reaction progress. Production observations Related to the previous observation, a production employee from that shift who was reprimanded reported that for a previous batch ***, there was a spill of the final product blend from the blender onto the floor of production room XX and the employees swept the batch with broom and with scoops and reloaded the material back into the blender. According to the investigation report written five months after the event, the team leader was confronted and acknowledged this had happened. This incident had not been documented or reported at the time it occurred. Production observations Note: A deviation report examined at another factory stated that certain deviations and batch rejections were related to “More experienced workers know what to do but take short cuts and do not follow procedures.” Materials observations From a Warning Letter Sampling and Testing of incoming xxx used in the manufacture of API *** were inadequate: At least one specific identity test to verify the identity of the incoming material was not conducted. The reliability of the supplier’s certificate of analysis (COA) was not established in that a complete analysis was not performed and compared with the COA at appropriate intervals. Materials observations From a Warning Letter Procedures for the recovery of solvents were inadequate: Procedures for solvent recovery had not been established to ensure that solvents are controlled and monitored to assure they meet appropriate standards before reuse or commingling with other approved materials. (FDA 483 observation concerned co-mingling recovered solvent with fresh solvent before testing of the recovered solvent). Materials observations Recovered solvents were not adequately controlled in that a drum of recovered chloroform was observed stored in the area identified for storage of recovered ethyl acetate. (From a Warning Letter; the actual FDA 483 observation also pointed out that the recovered chloroform was in the middle of several drums of the other solvent). Materials observations Raw material sampling was not performed in an appropriately controlled area and foreign material was noted on the surface of bags of approved materials. Materials observations Sterile PE film used during production to form sterile bags for the finished product is gamma irradiated in a validated sterilization at another firm, however, the integrity of this film may potentially be compromised prior to use due to the practice employed in sampling for release for production. The PE film is transferred to the production area (class 100), sampled, resealed and transferred back to the warehouse with “Release” stickers place of the original cardboard boxes in which the rolls of PE film are stored. Materials observations The firm has out-sourced the testing of API ^^^ for residual solvents and does not request testing of residual solvent for every batch of product manufactured. In addition, review of two test reports from the contract laboratory, selected at random, found that despite the fact that the firm’s batch records and the DMF show ethanol to be the only solvent used in the process, the test results showed benzene to be present at levels more than 20 PPM. (continued) Materials observations Finally, the firm reportedly sends recovered solvent to a contract firm which performs further purification, however, there were no records present to support this arrangement and in response to my inquiry, it was stated the factory has never audited the contract firm which purifies the solvents. Materials observations The computer software designed by the firm’s IT department for raw material inventory control has not been validated and has no user controls. Materials observations There is no password security for the two computer terminals (Materials Section and Synthesis Section) which are used for entering and monitoring information regarding the receipt, use and inventory records for raw materials and intermediates. Packaging & Labeling observations Failure to have a written procedure for receipt, identification, quarantine, sampling, release and handling of labels Incoming labels are not proofed against a master label. There is no specimen labels placed in the executed batch records. Packaging & Labeling observations There is no procedure to reconcile the quantities of labels issued and returned or destroyed. Final product labeling for API *** lacks retest date and storage temperature. Labels on drums of finished API not sticking. (Note: Inspection found solution employed was use two labels – hope one sticks). Packaging & Labeling observations The written procedure (SOP) covering labeling of finished product, i.e., printed bags stamped with lot number does not address the details of label issuance or reconciliation following the labeling operation. (Inspection found printed bags with two API batch numbers in packaging staged for use in packaging of those batches. The accompanying paperwork recorded numbers of bags issued and returned even though operation not yet started.)