Autosomal Dominant Inheritance
advertisement

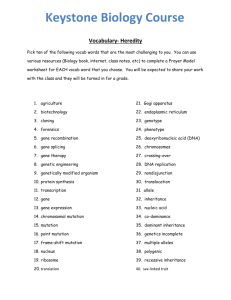
Overview Autosomal Dominant Inheritance Review of some basic concepts of mendelian inheritance Characteristics of autosomal dominant inheritance in man Mohammad Keramatipour MD, PhD Examples of human autosomal dominant disorders Keramatipour@tums.ac.ir M Keramatipour 1 M Keramatipour Review of Basics 2 Mendel’s Work Mendel’s experiments: ¾ Genes come in p pairs ((Mendel: factors)) ¾ Genes can have different alleles, some (dominant traits), ), exert their effects over others (recessive ( traits)) ¾ At meiosis alleles segregate from each other (each gamete receives one allele) ¾ The segregation of different pairs of alleles is independent Unifactorial inheritance: ¾ First described by Mendel in 1865 “Versuche uber Pflanzen Hybriden” – Experiment on Plant Hybrids ¾ Republished in 1901 by Bateson: Mendelain inheritance became synonymous with unifactorial inheritance ¾ Refers R f to those h trait/ i / di disorders d that h are d due to the h inheritance of a single gene M Keramatipour Mendel’s own words: ¾ Dominant, recessive 3 M Keramatipour 4 Dominant vs. Recessive Definitions Dominant Dominant:: a phenotype expressed in the same way in both Distinction is not absolute, specially in medical terms?? h homozygote t and dh heterozygote t t Many dominant traits have different phenotype in heterozygous and homozygous states Recessive Recessive:: a phenotype expressed only in homozygote ¾ True dominant human disorders 8 Huntington disease 8 Multiple endocrine adenomatosis I Incomplete dominant or semi semi--dominant dominant:: phenotype of heterozygous state, AB, is intermediate between the phenotypes p yp of AA and BB Many recessive traits have heterozygous manifestation at Co Co--dominant dominant:: phenotype of AB displays the phenotypic cellular biochemical cellular, biochemical, or molecular level features of both the homozygotic states M Keramatipour ¾ Sickle cell disease 5 M Keramatipour Continue to next page 6 Dominant vs. Recessive Monogenic Inheritance Sickle cell disease: ¾ Properties: Clinical level: patients are homozygous for a defective allele at the Beta globin locus and produce Hb S instead of normal Hb A: clinically, a recessive disease ¾ Different phenotype result from alternative genotypes att a single i l llocus ¾ Number of genotypes & phenotypes are small ¾ Biochemical level: heterozygotes produce Hb S and Hb A, so at the level of hemoglobin synthesis synthesis, co co--dominant ¾ Physiologic level: the normal allele is incompletely dominant and defective allele is incompletely recessive because a proportion of red blood cells in heterozygotes show the sickling phenomenon and they have mild anemia M Keramatipour 7 ¾ Relationship between genotype and phenotype is simple i l ¾ Well Well--suited for analysis using crosses and pedigree M Keramatipour Mechanisms of Dominance 8 Haploinsufficiency Default mechanism: mechanism: mutations produce recessive alleles to Haploinsufficiency Haploinsufficiency:: arise when 50 50% % reduction in amount or activity of the gene product result in abnormal phenotypic h t i ffeatures t Commonly occurs with mutation in genes encoding transcription factor (or other regulatory proteins) proteins), structural proteins, and cell surface receptors the wildwild-type allele because they produce inactive alleles ¾ Most recessive disorders in human are enzyme defects ¾ Most dominant conditions shows aberrant structural or developmental problems Why Wh some mutant t t alleles ll l show h d dominance: i Example: ¾ Waardenburg syndrome ¾ Angioneurotic A i ti edema: d mutation t ti iin Cl esterase t inhibitor i hibit gene 8 Due to rapid removal of the protein from circulation (independent of its concentration) production of large quantities of protein is needed ¾ Haploinsufficiency ¾ Gain G i -ofGainoff-function f ti mutations t ti ¾ New (sometimes toxic) protein function ¾ Dominant negative mutation ¾ Recessive mutations with dominant effects M Keramatipour 9 M Keramatipour Waardenburg Syndrome - Type I 10 Waardenburg Syndrome AD condition caused by point mutation in PAX3 gene that codes for a DNA binding protein (2q35) PAX3: expressed in developing neural crest & dermatomyotomal components of somites somites,, that give rise to skeletal muscles and dermis Loss of function mutation in PAX3: deficiency of neural crest derivatives such as melanocytes in hair hair, eyes eyes, inner ear, causing white forelock, white eyelashes, pachy depigmentation, depigmentation dep g e tat o , se sensorineural so eu a dea deafness, ess, a and d… M Keramatipour 11 M Keramatipour 12 GainGain -of of-Function Mutations Achondroplasia May happens by: Increased gene dosage: ¾ Hereditary sensory and motor neuropathy type 1: duplication of PMP22 PMP 22 gene, codes for peripheral myelin protein 22 AD condition, mutation in FGFR FGFR3 3 on 4p16 16..3 ¾ 98 98% % point mutation, GG-to to--A transition ¾ 1% GG-t0-C transversion at N N1138 1138 Ectopic or temporally altered mRNA expression: ¾ Mutation affects the time or place of gene expression ¾ Usually involves the regulatory part of the gene ¾ Hereditary persistence of fetal hemoglobin: caused by mutation in globin promoter region and prevent the normal switch between γglobin to δ and β-globin ¾ Both cause substitution of an arginine for a glycine at position 380 (G (G380 380A) A) ¾ 80 80% % of cases de novo mutation ¾ Paternal age effect ¾ Defect: 8 Zone of chondroblast proliferation in the physeal h l growth th plates l t Increased protein activity: due to increased halfhalf-life or activity ¾ Achondroplasia A h d l i M Keramatipour 13 New Protein Function 14 Dominant Negative Mutation New protein function: If a mutant allele interferes with the wildwild-type allele this is termed a dominant negative mutation ¾ A missence mutation in the alpha1 antitripsin gene convert the protein to an inhibitor of thrombin, resulting in a severe bleeding disorder This could occur in multimeric proteins Various types of collagen proteins Toxic protein alteration ¾ Hereditary amyloidoses: amyloidoses: mutation in trans trans--thyretin gene Osteogenesis imperfecta: mutation in the central portion leads to resistance of protein to proteolysis and increases th stability the t bilit off th the protein. t i P Protein t i th then accumulates l t and d undergoes multimerization in the cell as fibrils causing disruption of the cell M Keramatipour M Keramatipour of the collagen subunit genes Marfan Syndrome 15 Recessive Mutation with Dominant Effects M Keramatipour 16 Autosomal Dominant Inheritance Mutations clinically show dominant pattern of inheritance in the family More than half of known mendelian traits are dominant At the cellular or molecular level are recessive It happens in most of the dominantly inherited familial Autosomal dominant disorders have high incidence: ¾ ~ 1/500 for familial hypercholesterolemia ¾ ~ 1/500 in hypertrophic yp p cardiomyopathy y p y ¾ ~ 1/1000 for myotonic dystrophy ¾ ~ 1/ 2500 - 3000 for several other conditions such as neurofibromatosis fib t i and d Huntington H ti t disease di cancer syndromes (a germline mutation in a tumor suppressive gene + a “second hit”) RBRB-1 (retinoblastoma gene) is a classic example ¾ Heterozygous cells for the mutation are normal, so mutation itselff is recessive ¾ Disease results through transmission of a first mutation with a second somatic mutation in the normal allele of a retinal cell (two (two--hit hypothesis) M Keramatipour 17 M Keramatipour 18 Monogenic AD CVDs Pedigree Pattern In general term: Long QT syndrome: AD, ( also AR) Hypertrophic cardiomyopathy (HCM): AD ¾ Phenotype usually appears in every generation, each Familial hypercholesterolemia: AD affected person has an affected parent ¾ 50 50% % risk of inheriting the trait for any child ¾ Normal family members do not transmit the phenotype to their children ¾ Males and females are equally likely to transmit the phenotype ¾ Male to male transmission Familial defective apolipoprotein B ((apo apo B): AD Brugada syndrome: AD (SCN (SCN5 5A) Marfan syndrome: AD (FBN (FBN1 1, TGFBR TGFBR2 2) Restrictive cardiomyopathy cardiomyopathy: y p y: AD ((Desmin Desmin,..) ,..)) ….. M Keramatipour 19 M Keramatipour 20 Pedigree Example Autosomal Dominance Inheritance M Keramatipour 21 Counseling: Autosomal Dominant M Keramatipour 22 Reduced Penetrance, Variable Expressivity Important issues: ¾ New mutation 8 Isolated cases 8 Advanced parental age 8 Low reproductive fitness Mechanism of reduced penetrance and variable expressivity: ¾ Environmental factors ¾ Somatic mutations ¾ Unstable DNA triplet repeat sequences ¾ Age of onset ¾ Germ Germ--line mosaicism ¾ Clinical heterogeneity due to 8 Reduced penetrance 8 Variable expression p 8 Pleiotropy 8 Anticipation M Keramatipour ¾ Genetic background g ¾ New dominant mutations ¾ Somatic mosaicism ¾ Gonadal (germline) mosaicism 8 Osteogenesis imperfecta: 15 15% % of cases 23 M Keramatipour 24 Familial Hypercholesterolemia LDL Metabolism Low Density Lipoprotein Receptor (LDLR) mutation 5% of patients with hypercholesterolemia High incidence: 1/200 to 1/1000 Pathogenesis: ¾ Muatation in LDLR ¾ Plays a key role in cholesterol homeostasis ¾ LDLR is responsible for clearance of cholesterol from circulation i l ti ¾ Mutation disrupt the clearing process of cholesterol and the disease caused due to high level of cholesterol in circulation M Keramatipour 25 M Keramatipour 26 Phenotype of the Disease LDLR Pathway & Cholesterol Metabolism Age of onset ¾ Heterozygotes: Early ro middle adulthood ¾ Homozygotes: Childhood High cholesterol level (the earliest finding finding, usually at birth) Atherosclerosis, Coronary Artery Diseases (main cause of death) S Skin (tendon) (te do ) xanthomas a t o as Recurrent polyarthritis and tenosynovitis Arcus cornea M Keramatipour 27 M Keramatipour FH, More Sever in Males M Keramatipour 28 Xanthomas in FH 29 M Keramatipour 30 Xanthomas in FH Genetics of FH Mutation in LDLR 2-10 10% % are large insertions, deletions, or rearrangements mediated by recombination between Alu repeats within LDLR gene Some mutations are dominant negative Most mutation are private mutations (allelic heterogeneity) In some population there are founder effects (high prevalence of one mutation) Homozygotes have a sever form of the disease Mutation may y disrupt p different stages g of LDLR synthesis, y , transport and …. M Keramatipour 31 M Keramatipour 32 33 M Keramatipour 34 LDLR Mutations M Keramatipour Diagnosis and Management Long QT Syndrome Characterized by prolonged ventricular depolarization Diagnosis ¾ Clinical findings ¾ Increased QQ-T interval ¾ Family history ¾ Deformation of T wave & presence of U wave ¾ Laboratory findings ¾ Genetic testing 8 Prenatal diagnosis g is p possible in suitable families Management ¾ Lowering gp plasma level of cholesterol is the key y target g ¾ Diet: low low--fat, high high--carbohydrate diet ¾ Drug g therapy py M Keramatipour 35 M Keramatipour 36 Facts About LQT Types of LQT Syndrome Birth incidence: 1/5000 – 1/7000 Genetics of LQT: ¾ Mainly Autosomal dominant 8 Romano Romano--Ward syndrome ¾ Sometimes recessive 8 Jervell and Lange Langeg -Nielsen syndrome y ¾ Genetic heterogeneity ¾ Mutation effects: 8 Loss of function: Potassium channels genes 8 Gain of function: Sodium channels genes M Keramatipour 37 LQTS Type Chromosomal Locus Mutated Gene Ion Current Affected LQT1 11p15.5 KVLQT1 IKs LQT2 7q35--36 7q35 HERG IKr LQT3 3p21--24 3p21 SCN5A INa LQT4 4q25--27 4q25 ? ? LQT5 21q22.1--22.2 21q22.1 KCNE1 (heterozygotes) IKs LQT6 21q22.1--22.2 21q22.1 MiRP1 IKr M Keramatipour Cardiac Arrhythmias 38 Management/ Treatment Ventricular tachycardia Genetic: ¾ Torsades de Pointes ¾ Genetic testing available 8 80 80% % mutation detection rate 8 PND and PGD is possible p ¾ Ventricular fibrillation Syncope Cardiac arrest ¾ Gene therapy Sudden death Others: ¾ Beta Beta--blockers ¾ Pacemaker M Keramatipour 39 M Keramatipour Hypertrophic Cardiomyopathy Dilated Cardiomyopathy Dilated cardiomyopathy Hypertrophic cardiomyopathy (HCM) ¾ Asymmetric y left ventricular hypertrophy yp p y ¾ Usually autosomal dominant ¾ Prevalence: ~ 1:500 ¾ Traditionally an idiopathic disorders ¾ Today is a sarcomere disorder ¾ Mutation M t ti in i around d 11 genes that th t encode d different diff t element l t of sarcomere ¾ Genetic testing available in many center in US for majority of genes (MYH7 (MYH7, TPM1 TPM1, MYBPC MYBPC3 3, ….) ¾ Detection rate: 50 50--60% 60% in patients M Keramatipour 40 ¾ Dilatation and impaired p contraction of left ventricle ((or both)) ¾ Alcohol abuse, viral myocarditis, metabolic disorders, .. ¾ 30 – 50 50% % of DCM have g genetic cause ¾ Mainly autosomal dominant (Troponin T, Beta Mysin Heavy Chain, …) ¾ X-linked form also (dystrophin) ¾ Genetic testing available at least for 4 genes causing disease di ¾ First degree relatives are being screened 41 M Keramatipour 42 Marfan Syndrome Thank you for listening, any comments? Autosomal dominant Prevalence 1/3000 – 1/5000 Genes: ¾ Type I: FBN1 FBN1 ¾ Type II: TGFBR TGFBR2 2 M Keramatipour 43 M Keramatipour 44