Rapid Fire Anterior Segment
advertisement

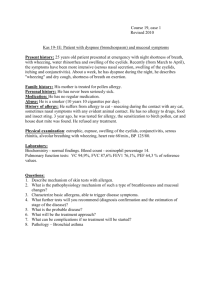
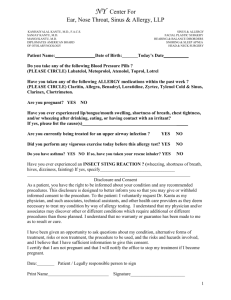
2014 Fall CE@SCO COURSE 4 Adventures of the Anterior Segment COPE Course 42589-AS CEE Approved SCO HOMECOMING / FALL CE WEEKEND • OCTOBER 9-12, 2014 8/25/2014 Disclosures Adventures in the Anterior Segment Walter O. Whitley, OD, MBA, FAAO Director of Optometric Services Virginia Eye Consultants Walter O. Whitley, OD, MBA, FAAO has received consulting fees, honorarium or research funding from: – Alcon • Santen – Allergan • Science Based Health – Bausch and Lomb • TearLab Corporation – Biotissue • Tearscience – Beaver-Visitec • Valeant Ophthalmics – Nicox Clinical Considerations • Urgency vs. Emergency • Acute vs. Chronic Case Study • 62 yo female presents for recent onset redness, discharge, swelling, and irritation. OU for the last 3 days • Current Drops: – Restasis BID OU – Genteal PRN OU • Mild vs. Severe • Ocular History • Progressive vs. Stable • Proparacaine to the rescue? – Cataract Extraction with PCIOL Dec 2012 OU – Blepharospasm treated with Botox injections • Health - unremarkable • Teaches 1st Grade Examination Assessment and Plan • Acute Conjunctivitis – Bacterial?? Viral?? Allergic?? • Considerations – – – – Associated symptoms? Are they contagious? Impact on treatment? Any other testing considerations? 1 8/25/2014 Acute Conjunctivitis Viral or Bacterial?? • Common condition – affects approximately 2% of the population annually1 • Can be caused by virus, bacteria, allergy, or other less frequent causes • 1-2% of all office visits2 • 20-70% of acute conjunctivitis is viral 3 • 65-90% caused by Adenovirus4 The Red Eye Protocol Conjunctivitis Management History Signs Symptoms Pink eye exposure, spread from one eye to the other, recent upper respiratory symptoms Itching, burning, foreign body sensation, tearing, discharge, eyelash matting Pre-auricular adenopathy, chemosis AdenoPlus POSITIVE Education: hygiene and hand washing Supportive care: artificial tears, cool compresses and antihistamines Consider antiviral medication No antibiotics THE RED EYE PROTOCOL FOR CONJUNCTIVITIS NEGATIVE Consider topical antibiotics or antihistamines Viral Conjunctivitis Treatment Supportive therapies Decontamination at home and hand washing Isolation Anti-viral therapy – No FDA-approved drugs specific for the treatment of Adenoviral conjunctivitis – Off-label applications for some currently available drug therapies: Povidone Iodide and Ganciclovir NO ANTIBIOTICS REQUIRED! 2 8/25/2014 Off-Label Adenoviral Treatments Off-Label Adenoviral Treatments Povidone Iodide (PVI)1 PVI (0.8%) extinguishes infectivity of free Adenovirus after 10 minutes of exposure but is less effective against intracellular Adenovirus Ganciclovir .15% Gel vs Preservative Free Tears (N=18) Ganciclovir .15% gel N=9 Preservative free tears N=9 Recovery time [mean (range)] 7.7 (7-12) days 18.5 (7-30) days SEIs 2 patients 7 patients Isenberg et al found Povidone Iodide (1.25%) ineffective Povidone Iodide (0.4%) – Dexamethasone (0.1%)2 9 eyes of 6 patients with confirmed Adenovirus enrolled 8/9 enrolled showed clinical resolution by day 4 6/6 patients with significant reduced DNA copies by day 5 5/6 culture positives with no infectivity by day 5 [1] Monnerat N, Bossart W, Thiel MA. Klin MonblAugenheilkd. 2006. 223(5): 349-352. [2] Pelletier JS, Stewart K, Trattler W, et al. Adv Ther, 2009. 26(8): 776-783. Problems with Steroid Treatment Although it may make the patient feel better… Risk of HSV (~3-21% of pink eye)1,2 Increase infectivity and viral replication of Adenovirus 3-6 Prolongation of Adenoviral positive cultures 3-6 Result: increase potential spread of Adenovirus 3-6 Medical-legal issues [1] Colin J. Ganciclovir ophthalmic gel, 0.15%: a valuable tool for treating ocular herpes. Clin Ophthalmol. 2007;1:441-53. Bacterial Conjunctivitis Treatment • Fluoroquinolones – Besifloxacin – Levofloxacin – Moxifloxacin – Gatifloxacin – Ciprofloxacin • Macrolides – Azithromycin [1] Marangon F.B., et al. American Journal of Ophthalmology, 2004. 137(3): 453-458. [2] Prost M, Semczuk K. KlinOczna, 2005. 107(7-9): 418-420. [3] Gaynor BD, Chidambaram JD, Cevallos V, et al. Br J Ophthalmol. 2005 Sep;89(9):1097-9. [4] Iihara H, Suzuki T, Kawamura Y, et al. Diagn Microbiol Infect Dis. 2006 Nov;56(3):297-303. [5]Uchio E, Takeuchi S, Itoh N, et al. Br Ophthalmol. 2000 Sep; 84(9):968-72. [6] Silverman M, Bressman B. Conjunctivitis. Available at: http://www.emdicine.com/emerg/topic110.htm. Prevalence of Allergy • A nationwide survey found that more than half (54.6%) of all U.S. citizens test positive to one or more allergens.1 • Allergic diseases affect as many as 40 to 50 million Americans.2 Conjunctivitis Treatment • Allergic – – – – – – OTC agents Antihistamines Mast cell stabilizers Combination antihistamine/mast cell stabilizers Non-steroidal anti-inflammatory agents Corticosteroids • Greater than 70% of patients with systemic allergy may manifest ocular symptoms.3 1 Arbes SJ et al. Preval ences of positive skin test responses to 10 common allergens in the U.S. population: Results from the Third National Health and Nutrition Examination Survey. J Allergy Clin Immunol. 2005; 116:377-383. . 2 Airborne allergens: Something in the air. National Institute of Allergy and Infectious Diseases. NIH Publication No. 03-7045. 2003. 3 Katelaris CH, Bielory L. Evidence-based study design in ocular allergy trials. Curr Opin Allergy Clin Immunol. 2008;8(5):484-8. 17 | PAT12500SK 3 8/25/2014 Most Prescription Treatment Options Have a Limited Effect on the Inflammatory Cascade Early-Phase Mediators Ocular Allergy Complications • Unpredictable Refractive Results • Diffuse Lamellar Keratitis • Chronic Cystoid Macular Edema • Conjunctival Scarring • Corneal Opacity & Ectasia • Trichiasis Entropion • Corneal Ulceration Late-Phase Mediators Mast Cell Membrane Phospholipids Mast Cell Stabilizers (MCS)1 Work Here Phospholipase A2 Activity Arachidonic Acid Combination Antihistamines/MCS1 Work Here Histamine Heparin Proteases (tryptase, chymase) Antihistamines 1 PAF Cyclooxygenase Pathway NSAIDs Work Here Cyclic Endoperoxides Lipoxygenase Pathway Hydroperoxides (5-HPETE) Work Here Prostaglandins Prostacyclin Thromboxane A2 HHT, MDA (PGF2α, PGD2, PGE2) (PGI2) (TXA2) Leukotrienes (LTC4, LTD4, LTE4, LTB4) 1. Adapted with permission from Donnenfeld ED. Refract Eyecare. 2005;9(suppl):12-16. 2. Slonim CB. Rev Ophthalmol. 2000:101-112. Point of Service Allergy Testing Allergy Antigen Testing • Cutaneous Skin Prick Test • Tear IgE – – – – – Advanced Tear Diagnostics (Birmingham, AL) – Rapid Pathogen Screening (Sarasota, FL) – TearLab (San Diego, CA) Must stop anti-histamine Rx Dermatitis or eczema may preclude testing Risk of severe specific allergic reaction Less suitable for infants and children • RAST (Radioallergosorbent Test) Pharmacia patent • ImmunoCap Specific IgE Test • Skin Testing – – – – – Allergy Corp Group (Charleston, SC) – Doctors Allergy Formula (Norcross, GA) New Gold Standard in 2010 Not as sensitive as Skin Testing More costly than Skin Testing Delayed results 21 Who Should Be Tested? • Recurrent or chronic URD, i.e., rhinitis, sinusitis, allergic-rhinitis • Unseasonal allergy-like symptoms • Seasonal or perennial allergy-like symptoms • Recurrent otitis media • Exogenous asthma and other conditions in which IgE mediation is suspected 22 Serum and Skin Prick Test Comparison Key Allergy Test Differences Blood Test Skin Prick Ordered in PCP or ECP office Yes Yes OK to stay on allergy medication Yes No Only one needle stick Yes (blood draw) No (60) No risk of severe allergic reaction Yes No OK with skin rash present Yes No Children as young as 3 months Yes No Same day results in the office No Yes 24 4 8/25/2014 ANTIGEN SKIN TESTING Specific Allergy Therapy CPT 95004 • • • • • Preventive Palliative Alternative Immunotherapy Pharmacologic – Topical, Nasal, Inhaled – Dermatologic – Systemic 26 Graded Pharmacotherapy Stepwise Treatment Strategies for Allergic Conjunctivitis Avoidance, cold compresses, tears, over-the-counter medications Mild Topical antihistamines/mast cell stabilizers Oral antiallergics (allergists may already have patients on orals; may exacerbate the ocular condition while improving the nasal condition) Montelukast Moderate + Mast cell stabilizers (treats allergy before mediator is released) + Combination antihistamine/mast cell stabilizers + Topical corticosteroids (most beneficial for severe outbreaks) Severe Topical corticosteroids (short course; fluorometholone/dexamethasone/loteprednol/prednisolone) Topical immunomodulating agents (tacrolimus, cyclosporine) Oral steroids • • • • • • • • • • • • 12 Patient Allergy Tips Never rub your eyes Wash your hands Use allergy free pillows Stay indoors Use drops for eyes, sprays for nose Avoid “get the red” out vasoconstrictors Chill your drops Use cool compresses Apply allergy drops proactively Pets out of the house or bedroom Know and avoid your personal antigens Try Montelukast: no sedation, no drying 28 Case Study • 2/13 ROV: 52 YO Asian Female / Follow up 4 month dry eye check. Intermittent foreign body sensation and fogged vision over 1 year • Ocular Hx: DES, LASIK 12.08.11 – Ocular Medications: Restasis BID OU • Medical Hx: Allergies, Borderline Diabetes, Acid Reflux – Systemic Medications: Multivitamin, Iron Slit Lamp Examination • BCVA – OD 20/25– OS 20/20- • MR – OD pl – 0.75 x 005 – OS -0.50 DS • External: normal OU • Conjunctiva: 2+ injection • Cornea: 1+ Diffuse SPK OU • Tear Eval: – 4 sec NIBUT – Schirmer 8/9 • Iris: flat OU • A/C: deep & quiet OU • Lens: clear OU 5 8/25/2014 Diagnostic Testing • Definition • • • • Clinical history Symptom questionnaire Tear film break up time Ocular surface staining • • • • • Schirmer / Red Thread Test Lid and meibomian morphology MG Expression Tear meniscus Tear film osmolarity – Nafl / Lissamine Green SLK and Treatment • • • • • • • • Lubrication Acetylcysteine Mast cell stabilizers Steroids Cyclosporin A Soft contact lens Silver nitrate Autologous serum Superior Limbic Keratitis • Botulinum toxin • Supratarsal steroid injection • Resection • Conjunctival ablation • Consider thyroid evaluation Example of Culture Report • Pathogenesis – Uncommon chronic disease – Superior bulbar and tarsal conjunctiva and limbus – Bilateral – Middle aged women – Abnormal thyroid function – Symptoms worse than signs – Remission occurs spontaneously – Blink-related trauma – Tear film insufficiency – Excess of lax conjunctival tissue – Inflammatory process – Self-perpetuating cycle Eyelid / Conjunctival Cultures • Eyelid – Moisten swab, rub along the lid margins • Conjunctiva – Inferior palpebral conjuntiva • Inoculate solid media plates • Culture – Calcium alginate swab – Cotton-tipped applicator – Transport medium Demodex Mite • Hold for: – Bacteria 1 week – Viral 2 weeks – Fungal 1 month • Test for all sensitivities 6 8/25/2014 Demodex • Life Cycle 14 ½ Days • .1mm to .4mm • Demodex Brevis – Live in Sebaceous Glands Connected to Hair Follicles (Zeis) • Demodex Folliculorum Increases of Demodex with Age • • • • • 13% of subjects 3 to 15 years 34% of subjects 19 to 25 years 69% of subjects 31 to 50 years 87% of subjects 51 to 70 years 95% of subjects 71 to 96 years – Live in the Eyelash Follicles and Meibomian Glands • Move at 1cm Hour • Avoid Light and Migrate at Night Czepita D, Kuzna-Grygiel et al. Investigations of the occurrence as well as the role of Demodex Folliculorum and Demodex brevis in the pathogensis of blepharitis 2005. Demodicosis • • • • • • Dry Eyes Itching Scaling of Lids Decreased Vision Madarosis As a result of blockage of follicles and hyperkeratinization and epithelial hyperplasia Demodex • Linked to Some Forms of Rosacea • Mating at Night in Hair Follicle • Eggs are Laid Deep Inside Sebaceous and Meibomian Glands • Larvae Hatch in Glands 3-4 Days • Develop Into Adults 7 Days Demodex Diagnosis • Observation Under Light Microscope of Lash Follicle • Small and Translucent • Often Diagnosis of Exclusion • Need Reliable Clinical Tests Case Study • • • • • • • 54 Year Old Female History of Pernicious Anemia Hypo Thyroid (Synthroid) HRT B-12 Prozac 2 year hx of Severe Dry Eye Syndrome 7 8/25/2014 Case Study • Full Scope Treatment of OSD Case Study • Full Scope Treatment of OSD – Plugs Lower and Upper (Upper removed) – Lid Hygiene – Progressing over 4 years in therapy – Various Artificial Tears – Currently with HA – Restasis – Lotemax – AzaSite • Sterilid (marked improvement that gradually diminished) – Doxycycline – Thera Tears Nutrition Conventional Treatment Methods Are Not Effective in Managing Demodex Blepharitis Case Study • Full Scope Treatment of OSD – Autologous Serum (Got worse after 1 week) – Worse at Night (no Nocturnal Lagophthalmos) – Itching – Discussion of Demodex • • • • Cannot be killed by Baby shampoo (common lid hygiene) Cannot be killed by 10% Propidone iodine (surgical scrub) Cannot be killed by 75% alcohol Cannot be killed by Macrolides such as erythromycin (antibiotic) • Cannot be killed by Metronidazole (for Rosacea treatment) • Cannot be killed by 4% Pilocarpine (for lice treatment) • Killed dose-dependently by Tea Tree Oil (TTO), derived from Melaleuca alternifolia Tea Tree Oil • • • • • • Compounding Pharmacy 50% Solution of Tea Tree Oil 20% Solution of Tea Tree Ointment Tea Tree Shampoo Tea Tree Soap Cliradex Tea Tree Oil • Begin Application of Tea Tree Lotion at Night on Face/Lids/Lashes • Office Visit – 4% Lidocaine Applied to Base of Lashes – 50% Tea Tree Oil Applied to Base of Lashes – Repeat X 2 in 10 Minute Intervals – Lotemax qid 8 8/25/2014 Demodex Case Study • Began Resolution Within 2 Days • Tapered Steroid over 3 days • “First time in over 2 years that I haven’t felt my eyes” • Linens • Treat Husband Case Study • 3/27/12 Increased light sensitivity / pain OU – Dx: Rebound Iritis OU – Tx: Restart difluprednate and nepafenac TID OU • 5/14/12 F/u chronic iritis OU, FBS OS – Dx: Improved Chronic Iritis OU, Dry eye disease OS>OD – Tx: Decrease steroid and NSAID to BID OU, ATs BID OU Understanding Tear Film Instability in Dry Eye • 72 YOAAF – Referred by OD for Cataract Eval OU. Blurred VA. Occasionally uses ATs prn. • Med Hx of allergies, acid reflux and HTN • SLE: 3+ NS OU • Uneventful cataract sx OU – OD 1/4/12 OS 2/1/12 Case Study • 9/7/12 – F/u chronic iritis, FBS OS>OD, Tearing – Dx: Resolved iritis OU, Dry eye disease OU – Tx: Start on cyclosporine 0.05% OU, F/u 4-6 mos • 2/25/13 – F/U dry eye disease OU, OS always has a FBS, Chronic tearing – Dx: DED OU / See photo – TearLab: 298 / 301 Osmolarity & Tear Film Instability in DED • Normal subjects exhibit low and stable osmolarity – Normal tear osmolarity = 280 - 300 mOsms/L – Equivalent to blood osmolarity = 285-300 mOsms/L – Indicative of the tears being held in proper homeostasis • Dry Eye subjects exhibit elevated and unstable osmolarity – Osmolarity changes between eyes and over time – Variability is the hallmark of DED ( > 8 mOsms/L between eyes) • Osmolarity was found to be the least variable of all common signs1 – Osmolarity: 8.7% – Corneal Staining: 12.2% – Conjunctival Staining: 14.8% – Meibomian Grading: 14.3% – TBUT: 11.7% – Schirmer’s Test: 10.7% 1Sullivan BD, Crews LA, Sönmez B, de la Paz MF, et al. Cornea 2012 9 8/25/2014 InflammaDry Advanced Tear Diagnostics Tearscan Referred to Conjunctival Resection • Dx: Conjunctivalchalasis OS>OD • Tx: Schedule for conjunctivoplasty OS – Disc R/B/A to surgery including 50% chance that symptoms will not improve even after a successful operation. – Pt elected to proceed with conjunctivoplasty OS only, as that is the more symptomatic eye. Case Example • 39 year old female • Presents for a frequent burning sensation OU – Most often in the morning with complaints of dryness that blinking helps – Also notes redness with blisters around eyelids • Ocular Medications – Systane Q1H OU – Elidel applied to eyelids BID Medical History • Review of Systems – Sinus problems • Systemic Medications – Spironolactone, Singulair, Flonase, Baby Aspirin • Family Health – Hypertension – Mother • Social History – Never smoked, 1 glass of wine daily, 1 cup of caffeine daily Exam • VA cc – OD: 20/20-1 OS: 20/20-1 • Pupils, EOMs and Confrontation fields all normal • Adnexa – 2+ Erythema of the lids – Vascularization of the lid margins 10 8/25/2014 Slit Lamp Exam • • • • • • • Conjunctiva: 2+ inferior limbal injection TBUT of 3 seconds Schirmers 30/17 Cornea: 2+ SPK OU, Few limbal infiltrates Anterior Chamber is deep and quiet Iris normal Lens is clear Impression and Plan Case Example - PB • 3 Weeks Later – mild improvement • SLE – Improved Lids / Conj / Cornea • Plan: • Blepharitis and Staph Hypersensitivity • Ocular Rosacea – – – – – – – Continue Systane PRN Start Doxycycline 50mg BID PO Warm compresses BID OU Loteprednol 0.5% / tobramycin 0.3% TID OU Loteprednol 0.5% ung PRN OU Fish Oil 2000mg PO Consider cyclosporine 0.05% at next visit – D/c loteprednol / tobramycin – Start cyclosporine BID – Cont systane – Cont doxycycline 50 mg po – Fish oils 2g per day – Warm compress qhs – Consider Lipiflow treatment • RTC 3-4 weeks for follow up appointment LipiFlow® Thermal Pulsation System Don’t Have $100,000 for a LipiFlow? LipiFlow safely and effectively treats Meibomian gland obstruction in both upper and lower eyelids simultaneously, in an in-office procedure, taking only 12 minutes per eye 65 11 8/25/2014 MiBoFlo ThermoFlo® Meibomian Duct Therapy Meibomian Gland Treatments Nocturnal Lagophthalmos • Typical Patient – Has progressed as a dry eye patient – Has little response to traditional treatment – Often doesn’t realize lagophthalmos – Sandy gritty feeling in the morning – Feels the need for artificial tears upon waking – Slight photophobia – Feels better after a shower Noctural Lagophthalmos Noctural Lagopthalmos • Ask Every Dry Eye Patient “how do your eyes feel first thing in the morning when you wake up?” • Ceiling Fans at night? • Look for lid closure • Children • Solutions: – Ointments, gels, weights, tape – Tranquileyes, Lacriserts 12 8/25/2014 Case Study - CH • • • • • • 07/06/09 54 YOMW / Referred from OD for K Ulcer Started on levofloxacin 0.5% Q1h OS Pain and Redness started 5 days prior SCLW / Denies sleeping in lenses VAcc OD 20/60 OS 20/200 Infectious versus Sterile • Infiltrate • Ulcers – – – – – – – – Rare Painful AC reaction Usually single lesion Discharge Epithelial staining Corneal edema > 2.0 mm in size – – – – – – – – Common Mild pain No AC reaction Multiple lesions Minimal discharge Epithelium intact No corneal edema < 2.0mm in size Fungal Keratitis Case Study • • • • • 3 + injection 3.5 mm ulcer 2+cells Cultures taken Added tobramycin Q2h Bacterial Keratitis Symptoms • Pain • Photophobia • Redness • Decreased vision • Discharge Signs • Focal infiltrate • Stromal loss • Epithelial defect • Lid swelling • Hyperemia • Mucopurulent discharge • K edema • AC reaction • Poss. hypopyon Acanthamoeba Keratitis 13 8/25/2014 HSV Keratitis Staph Hypersensitivity 7/7/09 7/9/09 • Cloudy since yesterday • Labs – No growth • SLE – Conj - 4+ Injection – Cornea - 3.5 mm ulcer / Haze / 1+edema / WBC – A/C - Rare cell • Plan – Continue present meds – Add sub-conjuctival injection of gentamycin – Add loteprednol 0.5% tid OS • More photophobic • SLE – Conj - 2+ Injection – Cornea – 3.0 mm ulcer / 1+edema / WBC surrounding ulcer – A/C – D/Q • See lab results Steroids for Corneal Ulcer Trial • Objective: To determine whether there is a benefit in clinical outcomes with the use of topical corticosteroids as adjunctive therapy in the treatment of bacterial corneal ulcers • Results: No significant difference was observed – – – – 3-month BSCVA (P =.82) Infiltrate/scar size (P = .40) Time to reepithelialization (P = .44) Corneal perforation (P > .99) Srinivasan M, Mascarenhas J, Rajaraman R, Ravindran M, Lalitha P, Glidden DV, Ray KJ, Hong KC, Oldenburg CE, Lee SM, Zegans ME, McLeod SD, Lietman TM, Acharya NR; Steroids for Corneal Ulcers Trial Group. 14 8/25/2014 Treatment • • • • • • Primary goal – eliminate the pathogens Secondary goal – prevent host destruction Treated as bacterial initially Small infiltrates – empirically (<1.0mm) Discontinue CL wear Cycloplegics – Homatropine 5% tid – Scopolamine 0.25% tid – Atropine 1.0% tid if hypopyon present Treatment • Fluoroquinolones – standard – Broad spectrum – Bioavailability – Biocompatibility • Peripheral infiltrates – q1-2h • Medium size – q1h w/ loading dose • Vision threatening – Fortified antibiotics – Tobramycin/gentamycin (15mg/mL) q1h – Cefazolin (50mg/mL) or vancomycin (25mg/mL) q1h – Fluoroquinolone Antimicrobial Susceptibility Surveillance: Ocular TRUST Antibiotic Resistance Monitoring in Ocular Microorganisms Study (ARMOR) • 200 S. aureus and 144 CNS ocular isolates were collected from 34 centers across the US. • Of the S. aureus isolates: – 39 percent were fluoroquinolone-resistant – 39 percent methicillin-resistant – 31 percent resistant to both • Of the CNS isolates: • Nationwide surveillance specific to isolates from ocular infections • Longitudinal data • Ocular TRUST 2006-2008 – Fluoroquinolones most consistently active agents across common ocular pathogens – Gatifloxacin = Levofloxacin = Moxifloxacin – 43 percent were fluoroquinolone resistant – 53 percent methicillin-resistant – 36 percent resistant to both Asbell, PA. Sahm DF. AAO Poster PO066. Atlanta. November 8-9, 2008 Ocular TRUST Results Ocular TRUST Results Staphylococcus aureus In Vitro Susceptibility Coagulase-Negative Staphylococci (CNS) In Vitro Susceptibility Methicillin-Susceptible S. aureus Methicillin-Resistant S. aureus Methicillin-Susceptible CNS Key Key CIP, ciprofloxacin; GAT, gatifloxacin; LEV, levofloxacin; MOX, moxifloxacin; AZTH, azithromycin; PEN, penicillin; PLX, polymyxin B; TOB, tobramycin; TMP, trimethoprim CIP, ciprofloxacin; GAT, gatifloxacin; LEV, levofloxacin; MOX, moxifloxacin; AZTH, azithromycin; PEN, penicillin; PLX, polymyxin B; TOB, tobramycin; TMP, trimethoprim Asbell, PA. Sahm DF. AAO Poster PO066. Atlanta. November 8-9, 2008 Methicillin-Resistant CNS Asbell, PA. Sahm DF. AAO Poster PO066. Atlanta. November 8-9, 2008 15 8/25/2014 Treatment • Subconjunctival injections • Oral fluoroquinolones – – – – – 0.3mg/dl lidocaine – 0.3mg/dl gentamycin • Topical steroid Impending perforation N. gonorrrhea Ciprofloxacin 500 mg bid Moxifloxacin 400 mg qd • Admission to hospital may be necessary – Use w/ caution • Oral pain meds – Sight threatening – Non-compliance – If IV needed – PRN Case Example - BL • 63YOWM Referred by PCP for sudden decrease VA OD and swelling of eyelids OD>OS for 1 week – – – – Pressure from forehead to cheek Worse in evenings Mild seasonal allergies Some tearing and redness OD • Bitten 3 weeks ago on top of the head while working in the yard which become swollen that evening • Went to PCP and given oral ABX which finished yesterday Diagnosis??? • Considerations: – PCP told him he had an infection not shingles – Episode started 3 weeks prior • Treatment – – – – Valacyclovir 1000mg TID po Diflurprednate QID OD Timolol 0.5% QAM OD F/u 1 week Follow-up • • • • • • Daily evaluation Taper with improvement Modify treatment based on results of culture If non-responsive, culture Corneal biopsy may be needed If impending / complete K perforation: – Cyanoacrylate tissue glue – K transplant, patch graft Examination • Non-healing scab on R forehead • Conjunctiva: 2+ injection OD • Cornea: 2+SPK, 2+ MCE, 1+ KPs, No dendrites OD • AC: 2+ Cells OD • Lens: 2+ NS OD / 1+NS OS • IOP: 31/13 Herpes Varicella-Zoster Virus • Primary infections: Chicken pox – Remains latent in dorsal root or other sensory ganglia after primary infection – May lie dormant for years to decades • Later infections: Shingles – Virus specific cell-mediated immune responses decline – Localized cutaneous rash erupting in a single dermatome – HZO accounts for 10-25% of all cases of shingles 16 8/25/2014 Herpes Zoster Ophthalmicus • 90% of U.S. population infected with VZV by adolescence • 100% of U.S. population by 60 years of age • 1.5-3.4 cases per 1,000 individuals Herpes Zoster Ophthalmicus • • • • • • • • • • • Conjunctivitis Scleritis Pseudodendrites Keratic precipitates Iritis Synechiae Neurotrophic keratitis Elevated IOP Potential vascular occlusion Nerve palsies Glaucoma (longer-term) http://emedicine.medscape.com/article/783223-overview#aw2aab6b4 HZO: Signs and Symptoms • Prodromal phase: fatigue, malaise, low-grade fever • Unilateral rash over the forehead, upper eyelid, and nose – 60% of patient have dermatomal pain prior to rash – Erythematous macules to papules to vesicles to pustules to crusts – Other symptoms: eye pain, conjunctivitis, tearing, decrease VA, eyelid rash – Hutchinson’s sign HZO: Treatment • Local wound care • Analgesia • Antivirals – Valtrex 1g TID • Post-herpetic neuralgia – Tricyclic antidepressants – Topical capsaicin ung – Gabapentin • Antibiotics?? • Oral corticosteroids • Post-herpetic neuralgia: >12 months for 50% Vaccines for HZO - Zostavax • Zostavax is live attenuated herpes zoster (HZ) virus – >50% reduction in the incidence of HZ – >60% reduction in symptom severity in patients who developed HZ – 66.5% reduction in postherpetic neuralgia. Case Example - AM • 44yo Asian American c/o blurred VA, redness, tearing, peri-orbital edema starting 2-3 days prior • Med Hx: Uncontrolled DM (Dx in 1998) • Must have chicken pox as a child • Vasc: OD 20/60 PH 20/30 OS 20/80 PH 20/40 • May help patients who've had HZO already • IOP: 21 / 18 1. Oxman MN, Levin MJ, Johnson GR, et al. A vaccine to prevent herpes zoster and postherpetic neuralgia in older adults. N Engl J Med. 2005 Jun 2;352(22):2271-84. 17 8/25/2014 What is Your Treatment? • Prednisolone acetate 1% vs. diflurprednate 0.05% vs. loteprednol etabonate .5% • Homatropine 5% vs. Scopolamine 0.25% vs. Atropine 1% Case Example • Acute, non-granulomatous, anterior uveitis OS • Cause??? • Treatment – Ordered labs – CBC w/diff, ESR, SMA-12, HLA-B27, Urinalysis, FTA-ABS, RPR, Lyme Western Blot – Diflurprednate q2h OS – Homatropine 0.5% TID OS – Doxycyline 100 mg BID po • Would you prescribe an oral medication? • Would you consider lab testing? When Should Lab Tests Be Ordered? Uveitis: Common Systemic Associations • Bilateral cases • Hyperacute cases • Most common cause • Atypical age group • Worsens with tapering • Other systemic causes – Idiopathic : 38-70% – HLA-B27 related disease • Recurrent uveitis • VA worsens • Recalcitrant cases • Immunosuppressed • • • • – – – – Ankylosing spondylitis Reactive arthritis Psoriatic arthritis Inflammatory bowel disease Sarcoidosis Systemic Lupus Erythematosus Rheumatoid Arthritis Behcets Disease Photo accessed from http://www.aao.org/theeyeshaveit/red-eye/images/anterior-uveitis.jpg Lab Testing • Minimum lab testing – – – – – – – – – – – CBC with differential Erythrocyte sedimentation rate (ESR) Angiotensin converting enzyme (ACE) Venereal disease research laboratory (VDRL) Fluorescent treponemal antibody absorption (FTA-ABS) Lyme titers in endemic areas HLA-B27 Antinuclear antibody (ANA) test Urinalysis Chest X-ray PPD Pulse Therapy • • • • • QID to Q 1 Hour for 7 to 10 Days Zero Tolerance for AC Cells Avoids Surface Toxicity Quick & Dirty Hit It Hard and Fast: Aggressive 18 8/25/2014 Uveitis Take Home Pearls Conclusions • Be a detective and find the cause • Practice to the fullest extent of our profession • Be aggressive with treatment • Be a detective • Don’t taper too soon • Think horses, not zebras • Treat and follow Thank You! Walter O. Whitley, OD, MBA, FAAO wwhitley@vec2020.com 19