How Can Population Based Care Models Be Applied to Improve
advertisement

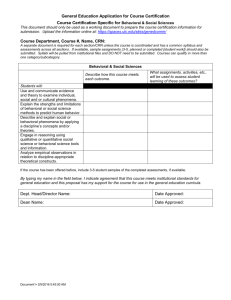
11/4/2014 How Can Population Based Care Models Be Applied to Improve Health Outcomes for Persons with Serious Mental Illness October, 15, 2014 Marc Avery, MD Clinical Associate Professor of Psychiatry Associate Director for Clinical Services, Department of Psychiatry and Behavioral Sciences University of Washington School of Medicine, Outline Population-Based Care and SMI Marc Avery 1. Definition 2. Importance 3. Supporting evidence Jennifer Clancy 1. Organizational Considerations 2. The Convening Organization 3. Barriers 4. Examples Jennifer Clancy, MSW Associate Director, California Institute for Behavioral Health Solutions Director, CIBHS Coordinated Care Collaborative Marc Avery, MD DISCLOSURES Employment: Associate Director for Clinical Services, Division of Integrated Care and Public Health and AIMS Center (Advancing Integrated Mental Health Solutions) Clinical Associate Professor of Psychiatry, School of Medicine; Dept. of Psychiatry and Behavioral Sciences, University of Washington School of Medicine Contracts (current & recent) California Institute of Behavioral Health Solutions Wyoming Health Care Authority Telehealth Corporation Psychiatric Advisor Magazine NO FINANCIAL RELATIONSHIPS THAT PRESENT A CONFLICT OF INTEREST FOR TODAY’s PRESENTATION I WILL NOT DISCUSS OFF LABEL OR INVESTIGATIONAL USE OF MEDICATIONS OR OTHER TREATMENTS Building on 25 years of Research and Practice in Integrated Mental Health Care © University of Washington 1 11/4/2014 Definition 1: Population based care means Ensuring outcomes for all patients in a group with a targeted condition Definition 2: Population Based Care Means – Not allowing our patients to fall between the cracks. 1. 2. Tufts Managed Care Institute Newsletter, November 2000 http://www.tmci.org/downloads/topic11_00.PDF Jurgen Unutzer, AIMS Center, University of Washington Where does population based care “fit in”? Patient Centered / Team Based Care Population-Based Measurement-Based Treatment to Target Evidence-Based Accountable © University of Washington Mental Disorders • Are common, disabling, expensive, and with high mortalities. • Are mostly chronic conditions that require deliberate / persistent follow up. • A small percentage of persons in need of mental health get any services. Why Population Based Care for SMI Persons? • System and Payment Reform -Expanded Coverage -Accountable Care Organizations -Health Home • Control of Escalating Costs • Clinical Effectiveness *Multiple investigators, references available by request. 2 11/4/2014 Why are Persons with Severe Mental Illness more Vulnerable to “Falling Through the Cracks”? Systems Issues 1. Payment system that discourages recovery 2. Episodic treatment authorizations 3. Services that often favor crisis intervention over disease management. 4. Fragmented service network Patient and Provider Issues 1. Stigma 2. Patient Health Behaviors 3. Clinical Inertia Washington State Senate Ways and Means January 31, 2011 Effects are Bidirectional 10 Mental Illness Results in Increased MEDICAL COSTS 50% higher Annual Health Care Costs regardless of # medical illnesses Annual Cost ($) Chronic disease score DDD Unutzer J, et al. JAMA. 1997;277:1618-1623. © University of Washington 3 11/4/2014 Sometimes the patients who need us most are the ones we forget.. Group 1 Punctual Articulate Polite Engaging Compliant / Adherent Responsive Has transportation Good support system Clinically straightforward Culturally Similar Group 2 Misses Appointments Disorganized Angry, agitated Reserved Isolative, Avoidant Rejecting Lacks transportation Lacks social supports Complex and Confusing Culturally Dissimilar Good News! We have evidence and increasing experience with models of care that work better! Primary Care Locus • IMPACT / Collaborative Care • TEAMcare • Behavioral Health Consultant / Cherokee Model Community Behavioral Health Locus • P-Care • Health Promotion Activities • SAMSHA-PBHCI “At baseline”? “Stable”? From: O’Conner, Patrick, et. Al, Clinical Inertia and Outpatient Medical Errors, 2005 AHRQ, Advances in Patient Safety IMPACT Team Care Model (Patient Centered Healthcare Home for Behavioral Health) Primary Care Practice with Mental Health Care Manager Outcome Measures Treatment Protocols Population Registry Psychiatric Consultation 4 11/4/2014 An Integrated Team-Based Approach – with a new Twist IMPACT doubles effectiveness of care for depression 50 % or greater improvement in depression at 12 months % Usual Care 70 IMPACT 60 PCP Core Program 40 New Roles Psychiatric Consultant BH Care Manager Patient 50 30 20 10 0 1 2 3 4 5 6 7 Participating Organizations 8 Unützer et al., JAMA 2002; Psych Clin NA 2004 IMPACT reduces health care costs MHIP: P4P-based quality improvement ROI: $ 6.5 saved / $ 1 invested cuts median time to depression treatment response in half. 1.00 Cost Category 4-year costs in $ 0 522 558 767 -210 7,284 6,942 7,636 -694 Other outpatient costs 14,306 14,160 14,456 -296 Inpatient medical costs 8,452 7,179 9,757 -2578 Inpatient mental health / substance abuse costs 114 61 169 -108 31,082 29,422 32,785 -$3363 0.75 0.00 0.25 0.50 Pharmacy costs 16 24 32 40 48 56 64 72 80 88 96 104 112 120 128 136 Difference in $ 522 Outpatient mental health costs 8 Usual care group cost in $ 661 IMPACT program cost 0 Intervention group cost in $ Total health care cost Savings Weeks Before P4P Unutzer et al, AJPH, 2012. After P4P Unützer et al., Am J Managed Care 2008. © University of Washington 5 11/4/2014 Primary Care Access, Referral and Evaluation PCARE (Druss, et. Al 2010) What about SMI patients who: 1. Get the majority of their services in a CMHC? 2. Have much more complicated service teams? Integrated Primary Care Team VS. RN Care Manager Community Mental Health (n = 142) Integrated Community BH Care Team • • • • Primary Care / Medical Increased Preventive Care (58% versus 21%) Treatment for CV illness (34% versus 28) Primary Care Linkage (71% versus 52%) Increase in self-rated health Health Promotion: Improving Fitness and Reducing Obesity: What Works Stephen J. Bartels, M.D., M.S. & John A. Naslund, M.P.H. HEALTH PROMOTION RESOURCE GUIDE: Choosing Evidence-Based Practices for Reducing Obesity and Improving Fitness for People with Serious Mental Illness. 2014 SAMSHA Publication. www.integration.samsha.gov From: World Psychiatry. 2011 June; 10(2): 138–151. 6 11/4/2014 Create a Table to follow… Topic Tool Frequency Target Goal Blood Pressure SBP/DBP Monthly SBP<140 and 45%, 50% DBP<90 Tobacco/Nicotine Smoking status Monthly 0 5% Depression PHQ Monthly 5 point reduction or score <10 10% Anxiety GAD Monthly 5 point reduction or score <10 10% Obesity BMI Quarterly >25 45% Diabetes HBA1c Annually <7.5 25% Cholesterol / Lipids LDL-C Annually HDL-C>40 LCL-C<130 50% Alcohol AUDIT (modified) Quarterly Drug Use DAST (modified) Quarterly SAMSHA Primary and Behavioral Health Care Integration (PBHCI) Program Study Questions: 1.Is PCBHCI Possible? 2.Does it improve outcomes? 3.What components work best? SAMSHA-HSA Primary and Behavioral Health Care Integration (PBHCI) Program SAMSHA Training and T.A. Grantees I II III IV V VI 13 9 34 8 30 9 National Council Evaluation RAND Deborah M. Scharf, Nicole K. Eberhart, et. Al., December 2013. EVALUATION OF THE SAMHSA PRIMARY AND BEHAVIORAL HEALTH CARE INTEGRATION (PBHCI) GRANT PROGRAM: FINAL REPORT, U.S. Department of Health and Human Services Assistant Secretary for Planning and Evaluation Office of Disability, Aging and Long-Term Care Policy. SAMSHA Primary and Behavioral Health Care Integration (PBHCI) Program Core Elements: Required: • Screening and Referral for Primary Care Prevention • Use of Clinical Registry or Tracking System • Person-Centered Care Management • Prevention and Wellness Support Services Optional: • Co-Location • Population Consultation • Embedded RN care managers • Preventive EBPs 7 11/4/2014 SAMSHA-HAS Primary and Behavioral Health Care Integration (PBHCI) Program Models: 1.Coordinated Care 2.Co-located Care 3.Integrated Care • Partner with primary care organization • Hire primary care team Deborah M. Scharf, Nicole K. Eberhart, et. Al., December 2013. EVALUATION OF THE SAMHSA PRIMARY AND BEHAVIORAL HEALTH CARE INTEGRATION (PBHCI) GRANT PROGRAM: FINAL REPORT, U.S. Department of Health and Human Services Assistant Secretary for Planning and Evaluation Office of Disability, Aging and Long-Term Care Policy. THANK YOU! Practical Experience with Facilitating Population Based Care Jennifer Clancy, MSW Associate Director CA Institute for Behavioral Health Solutions Marc Avery, MD mavery@uw.edu http://uwaims.org/index.html © University of Washington 8 11/4/2014 Jennifer Clancy, MSW Topics 1. Overview Of The Organizations That Are Vital for the SMI Population DISCLOSURES Employment: Associate Director, California Behavioral Health Solutions 1. The Role of Convening Organizations in SMI Population Health Grant funding (current & recent) None Contracts (current & recent) CA Department of Health Care Services 2. Historical Barriers to Creating Coordinated Care Systems for SMI Population NO FINANCIAL RELATIONSHIPS THAT PRESENT A CONFLICT OF INTEREST FOR TODAY’s PRESENTATION I WILL NOT DISCUSS OFF LABEL OR INVESTIGATIONAL USE OF 3. Solutions: Examples of Convening Organizations Coordinated Care to Address Population Health Needs MEDICATIONS OR OTHER TREATMENTS. 33 The Organizations Shaping the SMI Population Health- As Is FUNDERS RECIPIENT/ INTERMEDIARY PAYORS/ CONTRACTORS PROVIDER NETWORK CMS HRSA DHCS FQHC FQHC CBOs (MH, SUD, SS, Peers) SAMHSA County BH HEALTH Managed Care Plan County Behavioral Health Tax Payers (Millionaires) CBO: SUD 34 Where Are We Going? Coordinated System Offering Integrated Care Foundations CBO: MH CBO: Social Service, Peers…. Etc., etc. County Behavioral Health FQHCs/Health Clinics UNCOORDINATED SYSTEM 35 Various Funding Sources Organized by Population Health and Triple Aim Principles Social Service Agencies, i.e. Housing Wellness Agencies: i.e. Gym Convening Organization/Integrator Accountable for Population Health Peer Providers Behavioral Health Provider: SUD and MH Primary Care Provider 36 9 11/4/2014 Convening Organizations 1. Convening Organizations What Can The “Convening Organization” Do? 1. Assumes accountability for a population Convenes all provider organizations necessary to support the whole health of the population Builds a vision and shared understanding of the potential benefits of a coordinated system Supports the development of the organizational relationships and agreements/MOUs 2. What Are The Barriers each Faces in serving as the “Convening Organization” for SMI population? Medi-Cal Managed Care Plans (MCPs): Historically not responsible for mental health care Subcontracts to Managed Behavioral Health Organizations MCPs need to develop knowledge- build a provider network and a delivery system SMI population County Mental Health Plans (MHPs): Which Organizations Can Serve as “Convening Organizations” for SMI population? Medi-Cal Managed Care Plans County Mental Health Plan Historically isolated from agencies they must partner with Organizational isolation consequence of : stigma; carved out funding; traditional split of mind/body care Limited experience using health information technology 37 38 Solutions for Coordinated Care Partnerships for Population Health Fresno County Care Coordination Partnership: Fresno County Dept. of Behavioral Health Clinica Sierra Vista: (County Mental Health Plan as Convener) FQHC, integrated mental health & primary care clinic serving Medi-Cal, Medi-Care & uninsured individuals County MHP, convening organization and client care coordinator Ambulatory Care Center High-fidelity IMPACT model of integrating mental health services into primary care clinic. Serves clients with mild/moderate mental illness A local Public Health Plan created by the Regional Health Authority to serve Medi-Cal members in the counties of Fresno, Kings & Madera. 39 40 10 11/4/2014 Clinica Sierra Vista (FQHC) Fresno County Dept. of Behavioral Health (MHP) *12% *18% 4% Ambulatory Care Center (PCP) Behavioral Health and physical health care’s coordination has, thus far, been driven by individual providers rather than system change. Longterm change must be driven by the systems rather than pushed forward by a few practitioners. 1% *38% CalViva Health (MCP) *Percentages may include duplicated clients Ambulatory Care Ctr 12% Clinica Other PCP 36% Sierra Vista 21% The Fresno County Care Coordination Partnership Team will make changes to improve the whole health status of adult individuals by coordinating services for the clients with the most serious mental illness and substance use disorders. PCP Unknown 31% 41 42 Key changes the Team has been working on Overall Theme Across All Agency Partners • Multidisciplinary Clinical Care Conferences (routine & ad hoc) • Develop routine SUD screening • Support of client self-management • Ensuring and monitoring routine medication reconciliation • Ensuring and monitoring authorizations for sharing client PHI • Referral process between MHP and PCP • Sharing of patient physical exams, test & lab results • Recognize the importance of physical and mental health care to overall well-being of an individual • Shared goal and all agency partners benefit! Agency Catalysts for Care Coordination/Population Health: – Mental Health (Medical Director) – CalViva Heath Plan – Primary Care 43 44 11 11/4/2014 CC measures data collection process • Excel spreadsheet (tracks key health indicators, ROIs, etc.) • MHP’s EHR system (Avatar) - Data reports created specifically for CCC & embedded into EHR for ease of generating data CSV (FQHC) CalViva (MCP) NextGen Who is responsible for collection? • PCPs and MCPs collect data for their respective measures. • MHP data analyst responsible for MH data collection, synthesis of data from MCP & PCPs, and reporting out to CiBHS Maintain key personnel from partner agencies Buy-in from executive leadership Right People at the Table with the Right Personalities: ACC (PCP) EPIC Agency-Specific CCC Data Measures & Client List • Client centered and dedicated providers • Providers who follow through and are accountable • Providers who are real learners. “Care coordination and population health is so different from what has been done before- given the learning curve, the team members must be learners”. • Providers who are honest, transparent, and “leave their egos at the door” DBH (MHP) Avatar CiBHS CCC 45 Solutions for Coordinated Care Partnerships for Autism Population Health 46 48 The Problem: Late Diagnosis = Late Intervention = Diminished Quality of Life & Higher Life-Long Care Cost Autism Assessment Center of Excellence (Medi-Cal Managed Care Health Plan as Convener) National Ave Age of diagnosis Average age of ASD diagnosis of Latino Children Average age of ASD diagnosis in the Inland Empire in the Inland Empire Age diagnosis can be reliable & valid 47 12 11/4/2014 Kids with Autism Deserve an Answer! 49 The Solution: Formation of the Inland Empire ASD Collaborative 50 Autism Society Inland Empire Scarce Resources Concept Dept Children’s Network Lack of clinical criteria Lack of essential medical personnel Fragmented System First 5 Riverside & First 5 San Bernardino Counties Desert Mountain Special Education LPA Inland Empire Health Plan (IEHP) Quality of Life Treatment is not well understood or coordinated Delay in diagnosis = Decisions based on cost rather than clinical criteria Diminished life-long functioning Inland Regional Center Lost early intervention = Vision: Riverside County Mental Health Department Riverside County Office of Education San Bernardino Department of Behavioral Health AACE Center: Integrated & Child-Centric Inland Empire (IE) ASD Collaborative 51 of Pediatrics Loma Linda University 52 “Every child in the Inland Empire will have access to a collaborative, organized, integrated and TransDisciplinary Assessment/treatment resource for Autism.” Mission: “To meet the autism community’s needs through shared responsibility for a comprehensive and TransDisciplinary assessment, Treatment Recommendations, Referrals and Resources in order to maximize the quality of life for children in the Inland Empire with Autism and their families.” Inter-agency collaboration Comprehensive assessment Improves referrals and aligns providers and educators Eliminates wasted time & duplicative assessments “One Stop Shop” Early Intervention Reduces parent’s burden of having to advocate and coordinate across multiple agencies Access to treatment at an earlier age leads to a higher Quality of Life & functioning 13 11/4/2014 53 The AACE Center Opens 2014 and Promises to: Creating Population Health 54 Be recognized by medical treatment providers, school districts and social service programs as a trusted and credible assessment provider Provide families and providers with useful, appropriate and actionable treatment recommendations, referrals and resources Be financially self-sustaining 2 years after start-up Create a model that can be replicated in other communities. When a Solution Depends on Shared Responsibility, there Must Still Be a “Convening Organization” Collaboration takes Longer to Implement Bringing Everyone Along takes Shared Vision and Mission which must be centered on the Target Population - not any single Agency When Commitment and Perseverance Prevail a Collaborative Strategy often yields The Best Result for Population Health as it is a: “Community Solution” 14