INTPSY-10667; No of Pages 8
International Journal of Psychophysiology xxx (2013) xxx–xxx
Contents lists available at SciVerse ScienceDirect
International Journal of Psychophysiology
journal homepage: www.elsevier.com/locate/ijpsycho
Is blunted cardiovascular reactivity in depression mood-state dependent? A comparison
of major depressive disorder remitted depression and healthy controls
Kristen Salomon ⁎, Lauren M. Bylsma, Kristi E. White, Vanessa Panaite, Jonathan Rottenberg
University of South Florida, United States
a r t i c l e
i n f o
Article history:
Received 4 December 2012
Received in revised form 21 May 2013
Accepted 31 May 2013
Available online xxxx
Keywords:
Cardiovascular
Depression
Reactivity
Blood pressure
Heart rate
Impedance cardiography
a b s t r a c t
Prior work has repeatedly demonstrated that people who have current major depression exhibit blunted
cardiovascular reactivity to acute stressors (e.g., Salomon et al., 2009). A key question regards the psychobiological basis for these deficits, including whether such deficits are depressed mood-state dependent or whether
these effects are trait-like and are observed outside of depression episodes in vulnerable individuals. To examine
this issue, we assessed cardiovascular reactivity to a speech stressor task and a forehead cold pressor in 50 individuals with current major depressive disorder (MDD), 25 with remitted major depression (RMD), and 45
healthy controls. Heart rate (HR), blood pressure and impedance cardiography were assessed and analyses controlled for BMI and sex. Significant group effects were found for SBP, HR, and PEP for the speech preparation period and HR, CO, and PEP during the speech. For each of these parameters, only the MDD group exhibited
attenuated reactivity as well as impaired SBP recovery. Reactivity and recovery in the RMD group more closely
resembled the healthy controls. Speeches given by the MDD group were rated as less persuasive than the
RMD or healthy controls' speeches. No significant differences were found for the cold pressor. Blunted cardiovascular reactivity and impaired recovery in current major depression may be mood-state dependent phenomena
and may be more reflective of motivational deficits than deficits in the physiological integrity of the cardiovascular system.
© 2013 Elsevier B.V. All rights reserved.
1. Introduction
Depression has emerged as an important psychological predictor of
risk for cardiovascular disease. Prospective evidence links depression
among otherwise healthy individuals with future incidence of cardiovascular disease (Kuper et al., 2002; Penninx et al., 2001; Rugulies, 2002;
Wuslin and Singal, 2003). Recently, evidence has pointed to a relationship between depression and blunted cardiovascular reactivity. For example, our research group reported that individuals meeting DSM-IV
criteria for major depressive disorder (MDD) demonstrated less reactivity but impaired recovery relative to a healthy control group (Rottenberg
et al., 2007; Salomon et al., 2009). Similarly, self-reported depressive
symptomatology has also been linked to blunted reactivity in nonclinical samples (Schwerdtfeger and Rosenkaimer, 2011), coronary artery disease patients (York et al., 2007), and large-scale community
cohorts (Carroll et al., 2007; de Rooij et al., 2010). The traditional
reactivity hypothesis links exaggerated reactivity to CVD risk; however, recent theorizing regarding allostatic load suggests that
blunted reactivity and impaired recovery are also markers of poor
health (McEwen, 1998). Specifically, McEwen argued that allostatic
Abbreviations: MDD, major depressive disorder; RMD, remitted major depression.
⁎ Corresponding author at: Department of Psychology, PCD 4118G, University of South
Florida, Tampa, FL 3360, United States. Tel.: +1 813 974 4922.
E-mail address: ksalomon@usf.edu (K. Salomon).
load may be indicated by inadequate mobilization of a stress–response
system. Some degree of cardiovascular response to stress is functional
in that it mobilizes energy toward coping efforts to manage the stressor.
Thus, blunted reactivity, or inadequate responding, can be seen as maladaptive in some contexts. Further, blunted reactivity may be associated
with unique and deleterious health consequences. As Carroll and colleagues have noted, reactivity is often positively associated with an
up-regulation of immunity associated with host defense; thus by consequence, blunted reactivity may be associated with down-regulated
immunity and compromised ability to fight infectious disease (Carroll
et al., 2009).
While considerable evidence suggests that relatively robust reactivity
is associated prospectively with increased risk for CVD (Chida and
Steptoe, 2010), it has recently been argued that the relationship between
reactivity and pathological states may be curvilinear (Lovallo, 2011). In
other words, reactivity above or below the average range may indicate
poor health. This argument is based on emerging evidence that comparably low levels of reactivity in both the cardiovascular and HPA systems are
related to a number of unhealthy states including obesity (Carroll et al.,
2008), addiction (al'Absi et al., 2003; Panknin et al., 2002), disordered eating behavior (Ginty et al., 2012), exercise dependence (Heaney et al.,
2011), fibromyalgia (Reyes del Paso et al., 2010) and fatigue among
Veterans with Gulf War Illness (Peckerman et al., 2000), as well as states
that confer risk for poor health such as racial/ethnic discrimination
(Salomon and Jagusztyn, 2008) and low cognitive ability (Ginty et al.,
0167-8760/$ – see front matter © 2013 Elsevier B.V. All rights reserved.
http://dx.doi.org/10.1016/j.ijpsycho.2013.05.018
Please cite this article as: Salomon, K., et al., Is blunted cardiovascular reactivity in depression mood-state dependent? A comparison of major
depressive..., International Journal of Psychophysiology (2013), http://dx.doi.org/10.1016/j.ijpsycho.2013.05.018
2
K. Salomon et al. / International Journal of Psychophysiology xxx (2013) xxx–xxx
2011). Further, curvilinear relationships between physiological and
psychological phenomenon is not without precedent. The classic
Yerkes–Dodson law suggests that, when a task is difficult, performance exhibits a curvilinear relationship with arousal (Yerkes and
Dodson, 1908). More recently, this relationship has been applied to
the action of the locus coreleus–norepinephrine (LC–NE) system in
the brain and its effects on memory and attention (Aston-Jones and
Cohen, 2005). These models support the idea that flexibility and balance of physiological symptoms are also hallmarks of health. Rigidity
of response in over or under responding reflects inflexibility and an inability to adapt. Thus, the idea that blunted reactivity may be related to
pathology is reasonable.
Given that blunted reactivity may be seen as pathological, one key
question is whether blunted reactivity in depression is a stable biomarker
of risk for depression or is a marker of the depressed state. If blunted reactivity is a stable biomarker, then we would expect that those at risk for
depression to exhibit it even when they are not depressed; i.e., prior to
becoming depressed or after remitting from depression. Alternatively, if
it is a phenomenon that marks the depressed state, we would expect
those at risk to exhibit normative levels of reactivity. Prior data on this
issue are scarce and inconclusive. In the same large-scale community cohort discussed above, blunted reactivity was positively associated with
future depressive symptomatology, controlling for current symptomatology (Phillips et al., 2011). Elevations on depressive symptom measures
may or may not indicate the presence of diagnosable depression. Fortunately, blunted cardiovascular reactivity has also been shown to predict
a future depression, when depression is defined with structured clinical
interviews (Rottenberg et al., 2005). These findings suggest that blunted
reactivity may indicate a future risk for depression and not necessarily
current depression.
Relatedly, it is unclear what constitutes the psychobiological basis of
blunted reactivity in depression. Is blunted reactivity an indicator of
physiological deficits in the integrity of the cardiovascular system or is
it mediated by psychological processes? Lovallo (2011) has argued that
what the pathological states associated with blunted reactivity may
share, are dysregulated emotion and motivation systems. Depression,
addiction, obesity, and disordered eating, among others, signal difficulties with mood regulation, behavior regulation, and, perhaps, impulsivity
(Lovallo, 2011). In the context of acute laboratory task reactivity, emotional and motivational dysregulation may refer to a broad inability to respond appropriately to the emotional or motivational context, or may
simply be reflective of a lack of behavioral mobilization during the task.
Effort exerted during a task is related to the degree of reactivity during
the task (Wright et al., 1992). As long as a task is not seen as impossible
to perform, reactivity increases linearly with the difficulty of the task. On
the other hand, if a task is seen as impossible, or difficulty exceeds what a
person feels they can accomplish, very little reactivity occurs, indicating
that effort is reduced (Wright and Dill, 1993). Further, mood may affect
perceptions of task difficulty, such that those in a negative mood perceive
difficulty as too high for their abilities and thus fail to mobilize effort on a
task (Gendolla and Krusken, 2001, 2002). In our prior study (Salomon et
al., 2009), we found that an MDD group appraised a challenging speech
task as more stressful than the control group, suggesting an increased
perception of difficulty. However, the differences in appraisal did not explain differences in reactivity. Unfortunately, while task appraisals relate
to effort (i.e., a task perceived as too difficult or stressful may lead to
withheld effort), they are indirect. A better proxy for effort would be performance on the task. Unfortunately, we did not record the speech task in
the prior study, so we could not examine performance. Certain objective
aspects of performance, such as number of words spoken, provide a data
concerning behavioral mobilization during the task. Other aspects of performance, such as the persuasiveness of the speech, are arguably related
to more psychological aspects of motivation and task engagement. In the
present study, we sought to remedy this limitation. If blunted reactivity
is related to decreased behavioral effort as a consequence of depressed
mood, then those with depression should speak less and give less fluent
speeches. If blunted reactivity is related to less motivational investment
in the task, those with depression should give less persuasive speeches.
Further, if negative mood leads to decreased effort in general, those
with remitted depression, and thus, improved mood, should not exhibit
blunted reactivity.
For our primary task we used a psychological stressor; preparing
and giving a speech. This task is an active coping task and requires
motivated performance that can be directly evaluated by others.
Our secondary task was a forehead cold pressor. Individual differences in response to forehead cold pressor are well documented
(Ruiz, Uchino and Smith, 2006). The cold pressor is a passive task,
requiring endurance, and reactivity to forehead cold is driven primarily by stimulating the “dive reflex,” characterized by a reduction in
heart rate in response to cold temperature to the forehead region
(e.g., Heath and Downey, 1990: Reyners et al., 2000). We included
the cold pressor task because a pattern of blunted reactivity in a passive, physiologically-driven task might suggest a physiological basis
for blunted in reactivity in depression.
The present study sought to extend previous findings by comparing
reactivity among a group with fully remitted depression (RMD) to those
currently depressed (MDD) and healthy controls. We hypothesized
that, as in our prior data, individuals with MDD would exhibit blunted
reactivity to a speech stressor relative to healthy controls. In regard to
the RMD group, our hypothesis was open. If blunted reactivity was a
marker of risk for depression, we expected that the RMD group would
also exhibit blunted reactivity relative to healthy controls similar to
the MDD group. If blunted reactivity was indicative of the depressed
state, we expected that the blunted effects would be restricted to the
MDD group, and the RMD group would not differ from the healthy control group. We also sought to examine whether effort would explain reactivity differences by examining several aspects of performance during
the speech task.
2. Method
2.1. Participants
2.1.1. Recruitment and clinical assessment
Participants were recruited from fliers and online forum postings in
and around the Tampa Bay community. Individuals responding to research ads via email and phone were initially screened over the phone
to determine eligibility. Screening items were based on diagnostic questions from the Structured Clinical Interview based on the Diagnostic and
Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV-TR) Axis
I Disorders, Research Version, Patient Edition with Psychotic Screen
(SCID-I/P W/PSY SCREEN; First et al., 2002). A total of 820 potential participants were initially screened by telephone. Of those individuals, 271
were scheduled to complete the diagnostic interviews. Clinical psychology doctoral students completed the interviews and final diagnoses for
study inclusion were based on responses to the SCID administration. Of
those who completed the initial telephone screening, 31 individuals
failed to attend their appointment and were unable to be rescheduled
or decided they were no longer interested in participating. A total of
240 participants were consented and completed the SCID. Participants
were excluded from further study if they reported diagnosed cardiovascular disease, use of medications with known strong effects on cardiovascular measures (e.g., antipsychotics, beta blockers, etc.), history of a
major head injury, hearing impairment, diagnosis of bipolar disorder,
substance abuse occurring within 6 months prior to entry into the
study, or any history of primary psychotic symptoms. Participants were
not excluded for regular antidepressant use; however antidepressant
use was relatively uncommon in the sample. Less than 20% (n = 13)
of the MDD/RMD participants (MDD n = 9, RMD n = 4) and none of
the healthy controls reported taking antidepressants in the last month.
Of those participants who completed a SCID, 97 were excluded for failing
to meet inclusion or exclusion criteria, leaving 143 eligible participants
Please cite this article as: Salomon, K., et al., Is blunted cardiovascular reactivity in depression mood-state dependent? A comparison of major
depressive..., International Journal of Psychophysiology (2013), http://dx.doi.org/10.1016/j.ijpsycho.2013.05.018
K. Salomon et al. / International Journal of Psychophysiology xxx (2013) xxx–xxx
who were invited to participate in the psychophysiology assessment.
Twenty-three individuals failed to complete the psychophysiological
assessment at time 1, primarily due to scheduling difficulties. Participants who completed time 1 psychophysiology assessment fell into
one of three categories, those who met criteria for MDD with a current
episode (n = 50), those who met criteria for a history of MDD, but without a current episode (RMD, n = 25), and those who had no history of
any Axis I disorder as assessed by the SCID (Healthy Controls, n = 45).
We used strict criteria for remission requiring that individuals with
RMD exhibited no more than one sub-threshold symptom and no
sub-threshold depressed mood or anhedonia for at least 4 weeks.
Current anxiety disorder was also assessed by the SCID. Comorbid anxiety disorders were common in the MDD (n = 37) and the RMD (n = 7)
groups, and included panic (n = 4), social phobia (n = 11), obsessive–
compulsive disorder (n = 2), post-traumatic stress disorder (n = 3),
generalized anxiety disorder (n = 23) and not otherwise specified
(n = 11). The demographic and clinical characteristics of the eligible
sample are provided in Table 1.
2.1.2. Clinical symptom severity measures
At the time of the SCID interview, participants were also administered the 17-item Hamilton Rating Scale for Depression (HRSD;
Hamilton, 1960), a well-validated clinician-rated measure designed
to assess the presence and severity of depression symptomatology.
Each item is scored on a 0–2 or 0–4 scale during a structured interview with the patient and the sum of these ratings is used as a
score of global severity of depressive symptoms. The Beck Depression
Inventory (BDI-II; Beck et al., 1996) and the Beck Anxiety Inventory
(BAI; Beck et al., 1988) were also administered to measure depression
and anxiety symptom severity. The BDI-II and the BAI are both
21-item well-validated self-report measures of depression and anxiety
symptom severity.
2.1.3. Diagnostic reliability
Diagnostic reliability was monitored on an ongoing basis. We
conducted a formal reliability analysis of 15 cases that included
both eligible and ineligible participants. Diagnostic agreement was
assessed by having a second rater code SCID responses by listening
to the audiotape records. The second rater was blind to the diagnostic
decision of the original rater. For the classification of current MDD, and
healthy control subjects the decision of the two raters agreed in all 15
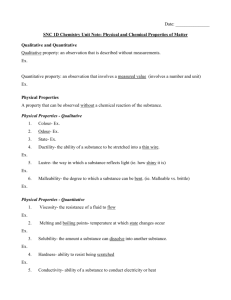
Table 1
Demographic, physical, and clinical characteristics of the eligible recruited sample.
Group
Variable
Age (years), M (SD)
Age, range
Caucasian ethnicity, N (%)
Female gender, N (%)
BMI, M (SD)
Waist circumference, M (SD)
Income, M (SD)⁎
BDI, M (SD)
BDI, range
BAI, M (SD)
BAI, range
Comorbid anxiety disorder
Antidepressant use past month
MDD
n = 50
RMD
n = 25
Control
n = 45
31.93 (11.77)
19–56
32 (59.30%)
45 (83.30%)
28.50a (8.99)
91.14a (19.57)
4.95 (2.87)
31.11a (9.49)
15–49
19.22a (8.86)
3–39
74.0%
16.7%
30.03 (10.26)
19–57
19 (52.80%)
20 (55.60%)
27.13a,b (8.05)
91.94a (17.86)
5.91 (3.04)
6.75b (5.30)
0–19
6.97b (7.87)
0–41
28.0%
19.4%
29.41 (12.07)
18–59
34 (66.70%)
37 (72.50%)
24.18b (5.74)
83.60b (12.69)
6.10 (3.43)
2.58c (4.16)
0–25
1.79c (2.99)
0–15
0%
0%
Note. BDI = Beck Depression Inventory, 2nd Edition, BAI = Beck Anxiety Inventory,
BMI = Body Mass Index. Means not sharing the same subscript differ at p b .05.
⁎Income was assessed on a 6-point scale with higher numbers representing higher
income — a score of 5–6 represents an income range of $25,000 and $34,999.
3
cases, k = 1.00. For the classification of RMD, the raters agreed in 14
of 15 cases (k = .81). We also assessed inter-rater reliability on key
clinician-rated scales for the same 15 cases. We found excellent
inter-rater reliability for the Global Assessment of Functioning (GAF;
α = .96) Scale and Hamilton Rating Scale for Depression (HAM-D;
α = .98)
2.2. Procedure for cardiovascular assessment
Cardiovascular assessments were conducted within 3 weeks of the
clinical assessment sessions. If more time had passed due to scheduling
difficulties, some participants were again administered the mood modules of the SCID to ensure diagnostic status had not changed. One
person was deemed no longer eligible because of a change in diagnostic
status.
After obtaining informed consent, participants completed a packet of
questionnaires. Each participant then was assessed for height and weight
with a fixed steel tape and a beam scale. Waist circumference was measured in cm at the level of the umbilicus. Next, the experimenter attached
the measurement sensors. Participants were seated comfortably in a
small recording room. The experimenter noted the presence of a video
camera and informed the participants that they would be monitored
throughout the protocol. Participants then viewed a neutral travelogue
film for a 10-min acclimation and baseline assessment. The two cardiovascular reactivity tasks were then administered in counterbalanced
order. The speech task required participants to prepare a speech on a specific topic (i.e., defending themselves against a traffic ticket), and to deliver the speech. The preparation and delivery phases of the speech task
were each 3 min. To increase evaluation apprehension during the speech
task, a research-assistant was present in the room and silently observed
and took notes and participants were made aware of the camera recording their speech. The second task consisted of a forehead cold pressor. A
cold ice pack was placed on participants' foreheads for 2 min. Each task
was separated by a 5-minute recovery where participants rested and a
5-minute buffer period where participants watched more of the travelogue film. After the second task, sensors were removed, and participants
were paid, debriefed, and thanked.
2.3. Data recording, reduction, and processing
A digital camera was used to record behavior throughout the experiment. ECG and impedance cardiography was recorded continuously.
Impedance and ECG data were collected continuously during baseline,
task, and recovery phases. We collected systolic (SBP) and diastolic
(DBP) blood pressure according to published guidelines (Shapiro et al.,
1996) using an Accutorr Plus blood pressure monitor (Datascope Corp.,
Mahwah, NJ). Participants' electrocardiograms (ECG) were obtained
according to published guidelines (Jennings et al., 1981). Cleartrace LT
disposable Ag/AgCl electrodes (Conmed Andover Medical, Haverhill,
MA) were placed in a modified Lead II configuration on the chest, and
ECG was amplified using a Biopac MP150 system with an ECG100 amplifier (Biopac Instruments Inc., Goleta, CA). We collected impedance cardiography according to the guidelines outlined by Sherwood et al. (1990)
using four mylar-band electrodes fully encircling the neck and torso
with the Biopac NICO100C monitor and Z0 & dZ/dt signals were digitized,
acquired, and stored using a PC and Biopac AcqKnowledge software.
BP recordings were taken at two-minute intervals during study
phases. During the 10-minute resting baseline, BP was recorded at the
fifth, seventh and ninth minutes because ECG and impedance cardiography signals were obtained during the last 5 min of baseline only. During
the three-minute speech preparation and speech delivery phases, BP recordings were obtained at the first and third minute of each phase. For
the three-minute cold pressor task, BP was measured during the first
and third minutes. During both recovery phases, BP recordings were
obtained during the first, third and fifth minutes.
Please cite this article as: Salomon, K., et al., Is blunted cardiovascular reactivity in depression mood-state dependent? A comparison of major
depressive..., International Journal of Psychophysiology (2013), http://dx.doi.org/10.1016/j.ijpsycho.2013.05.018
4
K. Salomon et al. / International Journal of Psychophysiology xxx (2013) xxx–xxx
HR and the impedance-derived measures of stroke volume (SV),
pre-ejection period (PEP), and cardiac output (CO) were obtained
using MindWare IMP 2.56 software (MindWare Technologies, Ltd.,
Gahanna, OH). The ECG and dZ/dt signals were ensemble-averaged
over 60-s epochs. The data were screened for artifact by visual inspection. Total peripheral resistance (TPR) was estimated using the
formula TPR = (MAP/CO) ∗ 80 in dyne-s/cm5 with mean arterial
pressure (MAP) calculated as (SBP + (2 ∗ DBP)) / 3. Baseline, task,
and recovery values for each measure were computed by averaging
the available values for each phase. Reactivity scores were calculated
as the arithmetic difference between task and baseline averages. Recovery scores were calculated as the arithmetic difference between
recovery and baseline values, such that smaller values indicate greater recovery.
2.4. Behavioral measures
Speech behavior was coded for 97 participants; 15 participants (13%)
had missing videos due to technical difficulties, such as the research assistant forgetting to record the video or partial recordings of speeches.
The recording was transcribed by two research assistants. The text was
used to compute objective indicators of task engagement such as the
number of words spoken, number of prompts from the experimenter
for the participant to continue the speech for the allotted time, and number of words indicating dysfluency (i.e., “um”). The transcriptions were
also analyzed with the Linguistic Inquiry and Word Count (LIWC2007)
program to identify words signaling positive and negative emotionality
used during the speech. Video recording of the participants delivering
the speech was used to code persuasiveness of the speech. Persuasiveness of the speech was determined using a global measure based upon
the entirety of the 3-minute speech. In making decisions about the degree of persuasiveness, the coder was instructed to attend to the level
of detail presented, logical flow of the story, whether the participant
spoke with conviction, and whether the speaker made a compelling
and believable argument. The speeches were coded on a 0 to 10 scale,
where 10 is the most persuasive. Persuasiveness was double coded for
20% (n = 20) of the cases and reliability was computed (α = .75).
2.5. Data analysis
First, a series of analyses of covariance (ANCOVAs) was conducted to
examine group differences in baseline SPB, DBP, and HR levels including
BMI and sex as covariates. To examine group differences in speech responses, a series of repeated measures ANCOVAs was conducted with
group (MDD, RMD, healthy control) as the between-subjects factor, and
phase (baseline, speech preparation, speech delivery, recovery) as the
within subjects factor with SBP, DBP, HR, SV, CO, PEP, and TPR as the dependent measures and BMI and sex included as covariates. Parallel repeated measures ANCOVAs were conducted for the cold pressor task
with three phases (baseline, cold, cold recovery).
Additional analyses were conducted to examine group differences in
reactivity and recovery separately. We conducted a series of ANCOVAs
with group (MDD, RMD, healthy control) as the between-subjects factor
and reactivity change scores as the dependent measures, again with BMI
and gender entered as covariates. To examine group differences in recovery, we conducted a series of ANCOVAs with group as the betweensubjects factor and recovery change scores as the dependent measures,
with BMI, sex, and reactivity score entered as covariates. For ANOVAs
that revealed significant differences among the groups, a Tukey's LSD
post-hoc analysis was conducted to determine which groups differed significantly. Analyses were conducted using IBM SPSS 19.0, and effect sizes
are reported as partial eta-squared (η2p). All covariates were chosen a
priori based on a wealth of evidence linking them to cardiovascular reactivity and recovery.
To examine group differences in speech behavior, we conducted a
series of ANOVAs with group as the between-subjects factor, and speech
behavior (persuasiveness, number of words produced, number of words
indicating dysfluency, and number of prompts needed to continue the
speech) as the dependent measures. For ANOVAs that revealed significant differences among the groups, a Tukey's LSD post-hoc analysis
was conducted to determine which groups differed significantly.
3. Results
3.1. Demographic, physical, and clinical variables
Demographic, physical, and clinical characteristics of the sample are
presented in Table 1. There were no significant differences among the
three groups on any of the demographic variables. The healthy control
group had significantly lower BMI and smaller waist circumferences relative to the current and remitted depressed groups, but the depressed
and remitted depressed groups did not differ on these variables. As
expected, current and remitted depressed participants reported more
depressive and anxiety symptoms than healthy controls, and currently
depressed participants reported more depressive and anxiety symptoms relative to the remitted group.
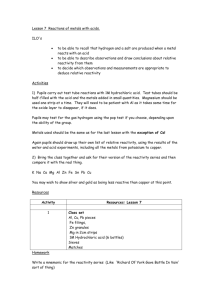
3.2. Resting baseline levels
As displayed in Table 2, the groups did not significantly differ on
resting levels of any of the cardiovascular measures (all ps > .05).
3.3. Speech task responses
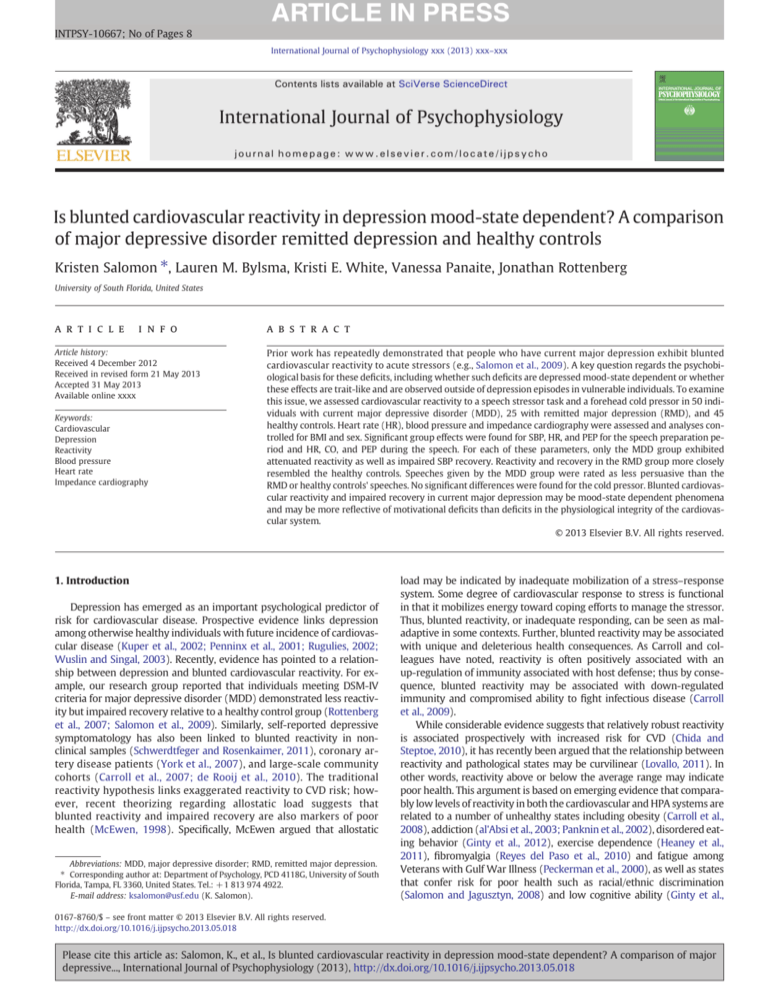
For the repeated measures ANCOVAs on speech task responses, significant group by phase interactions occurred for HR, F(4.2, 217.6) = 6.36,
p b .001, η2p = .108, PEP, F(4.5, 230.7) = 5.53, p b .001, η2p = .098,
and CO, F(4.2, 224.9) = 3.14, p b .005, η2p = .058. The interaction for
TPR approached significance, F(5.0, 237.4) = 2.19, p b .06, η2p = .044.
No other group by phase interactions were significant (all ps > .18).
Significant main effects of phase were found for SBP, F(2.39, 253.01) =
20.45, p b .001, η2p = .162, DBP, F(2.04, 215.78) = 20.47, p b .001,
η2p = .162, HR, F(2.11, 217.76) = 28.43, p b .001, η2p = .215, PEP,
F(2.26, 230.69) = 17.06, p b .001, η2p = .143, SV, F(2.29, 233.33) =
10.51, p b .001, η2p = .093, and TPR, F(2.50, 237.36) = 3.08, p b .05,
η2p = .031, but not CO, F(2.12, 216.06) = 2.08, p > .12, η2p = .020. A
significant main effect of group emerged for SBP, F(2, 106) = 5.21,
p b .01, η2p = .089. Post-hoc tests indicated that the MDD group had
lower overall SBP levels (M = 117.23, SE = 1.50) than the control
group (M = 123.27, SE = 1.51) and the RMD group (M = 123.94,
SE = 2.08), whereas the latter two did not significantly differ. Table 2
presents the mean cardiovascular levels for each speech phase by group.
As described earlier, to distinguish between reactivity and recovery, ancillary analyses were conducted on change scores. For the
speech preparation period, significant effects on reactivity for group
were found for SBP, F(2, 108) = 3.74, p b .05; η2p = .065, HR, F(2,
103) = 5.61, p b .01, η2p = .098; and PEP, F(2, 103) = 4.32,
p b .05, η2p = .077, with the MDD group exhibiting significantly
less HR, PEP, and SBP reactivity than the healthy controls. The MDD
group significantly differed from the RMD group for preparation HR
and PEP. Reactivity in the RMD group did not significantly differ
from that of healthy controls on any of the measures. No significant
group differences were found for DBP, SV, CO, or TPR reactivity during
the speech preparation period (all ps > .05).
For the speech delivery period, significant group differences in reactivity were found for HR, F(2, 102) = 8.14, p = .001, η2p = .138,
PEP, F(2, 102) = 9.33, p b .001, η2p = .155, CO, F(2, 102) = 4.68,
p b .05, η2p = .084, and TPR, F(2, 97) = 3.15, p b .05, η2p = 061.
Post-hoc tests indicated that the MDD group again exhibited significantly less reactivity than the healthy controls for delivery HR, CO,
PEP and TPR. The MDD group significantly differed from the RMD
group for delivery HR, CO and PEP. Reactivity in the RMD group did
Please cite this article as: Salomon, K., et al., Is blunted cardiovascular reactivity in depression mood-state dependent? A comparison of major
depressive..., International Journal of Psychophysiology (2013), http://dx.doi.org/10.1016/j.ijpsycho.2013.05.018
K. Salomon et al. / International Journal of Psychophysiology xxx (2013) xxx–xxx
5
Table 2
Mean cardiovascular levels by group, task, and phase.
Phase
SBP
a,b
(mm Hg)
DBPa,c (mm Hg)
HRa,c,d (bpm)
PEPa,d (ms)
SVa (ml)
COc (l/min)
TPRa (dyne-s/cm5)
MDD
RMD
Control
MDD
RMD
Control
MDD
RMD
Control
MDD
RMD
Control
MDD
RMD
Control
MDD
RMD
Control
MDD
RMD
Control
Baseline
Prep
111.28
116.33
112.94
69.22
69.13
68.43
73.90
71.94
68.42
109.54
112.61
108.77
112.91
128.95
120.07
8.15
9.11
8.49
942.72
850.81
888.96
117.66
126.67
123.92
74.68
77.59
75.65
78.66
82.18
77.25
105.28
102.89
99.90
111.87
123.20
117.76
8.59
9.96
8.95
988.26
887.91
949.82
(1.91)
(2.11)
(1.88)
(1.20)
(1.27)
(1.36)
(1.71)
(2.32)
(1.36)
(1.61)
(3.23)
(2.25)
(5.80)
(9.05)
(6.84)
(0.35)
(0.68)
(0.42)
(71.30)
(81.97)
(62.37)
Speech
(2.47)
(2.17)
(2.01)
(1.65)
(1.35)
(1.37)
(1.81)
(2.65)
(1.86)
(1.77)
(3.36)
(2.41)
(5.67)
(9.59)
(6.19)
(0.37)
(0.81)
(0.45)
(86.90)
(92.73)
(78.11)
129.20
136.11
133.00
82.41
85.02
84.00
83.98
90.85
86.77
101.27
94.55
90.92
110.65
124.71
116.62
9.11
11.18
10.01
998.09
783.93
924.20
(2.10)
(2.54)
(2.11)
(1.77)
(1.93)
(1.69)
(1.82)
(3.11)
(2.46)
(1.83)
(3.40)
(3.09)
(5.63)
(7.04)
(5.70)
(0.40)
(0.70)
(0.53)
(83.06)
(41.12)
(72.68)
Speech recovery
Cold
114.98
123.96
118.71
70.93
73.81
70.96
74.98
74.27
69.00
105.77
104.94
101.24
116.62
136.16
130.66
8.52
10.01
8.90
937.00
811.87
906.38
114.44
121.72
115.98
71.20
73.35
72.47
69.77
69.77
65.28
108.29
109.76
107.82
120.80
131.24
125.50
8.18
9.08
8.07
999.33
874.67
997.83
(1.87)
(2.20)
(1.73)
(1.27)
(1.18)
(1.25)
(1.73)
(2.39)
(1.43)
(1.66)
(2.89)
(2.46)
(6.05)
(9.48)
(6.78)
(0.37)
(0.77)
(0.45)
(78.41)
(58.75)
(82.78)
Cold recovery
(2.35)
(2.31)
(1.84)
(1.52)
(1.46)
(1.36)
(1.77)
(2.53)
(1.48)
(1.55)
(3.33)
(2.16)
(6.88)
(9.28)
(7.05)
(0.40)
(0.74)
(0.43)
(90.76)
(68.62)
(86.68)
112.71
118.93
114.08
70.11
72.65
70.29
73.33
72.66
68.41
108.06
109.49
106.77
114.20
127.76
122.88
8.15
9.24
8.27
952.08
855.62
940.43
(2.00)
(2.21)
(1.52)
(1.14)
(1.47)
(1.19)
(1.66)
(2.25)
(1.38)
(1.59)
(2.88)
(2.12)
(5.92)
(8.91)
(6.62)
(0.34)
(0.73)
(0.41)
(78.92)
(63.37)
(75.49)
Note. Numbers in parentheses are standard errors.
a
Significant speech task phase main effect.
b
Significant speech task group main effect.
c
Significant cold pressor phase main effect.
d
Significant speech task group by phase interaction.
not significantly differ from that of healthy controls on any of the
measures. No significant group differences were found for SBP, DBP,
SV, or CO, reactivity during the speech delivery period.
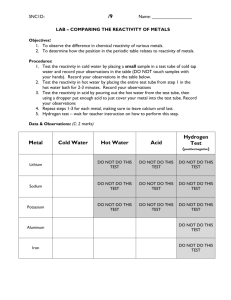
For the speech recovery period, significant group differences were
found for SBP, F(2, 107) = 3.45, p b .05, η2p = .060. The MDD group
exhibited less recovery than the RMD group and healthy controls. No significant group differences were found for the other cardiovascular measures (all ps > .11). Fig. 1 presents the means for speech reactivity and
recovery change by group and phase.
3.4. Cold pressor responses
For the cold pressor task, no significant group by phase interactions
were found (all ps > .29). Significant main effects of phase were found
for DBP, F(1.85, 201.80) = 3.62, p b .05, η2p = .032, HR, F(1.83,
191.68) = 4.69, p b .05, η2p = .043, and CO, F(1.35, 141.86) = 3.61,
p b .05, η2p = .033. No significant main effects of group were found,
although the effect for SBP approached significance, F(2, 109) =
2.91, p b .06, η2p = .051. Similarly, no significant group differences
Fig. 1. Mean reactivity and recovery change scores by group and phase. Note. *p b .05; **p b .01. Means for speech preparation, speech delivery, and speech recovery are adjusted
for gender and BMI. HR = heart rate, SBP = systolic blood pressure, CO = cardiac output, and PEP = pre-ejection period.
Please cite this article as: Salomon, K., et al., Is blunted cardiovascular reactivity in depression mood-state dependent? A comparison of major
depressive..., International Journal of Psychophysiology (2013), http://dx.doi.org/10.1016/j.ijpsycho.2013.05.018
6
K. Salomon et al. / International Journal of Psychophysiology xxx (2013) xxx–xxx
in reactivity or recovery were found for any of the cardiovascular
measures (all ps > .14). Table 2 presents the means for cold task
levels by group.
3.5. Speech behavior
A series of ANOVAs revealed that there were no significant differences
among the three groups for any of the indices of behavioral engagement,
including number of words produced, number of words indicating
dysfluency, and number of prompts needed to continue the speech, and
words signaling positive and negative emotionality (all ps > .12).
However, group differences were observed for speech persuasiveness,
F(2, 94) = 4.50, p b .05. A post-hoc analysis revealed that the effect
was driven by the fact that the MDD participants produced less persuasive speeches than healthy controls (p b .05). To ensure that differences
in coders' ratings were not influenced by the sex or BMI of the participant,
we repeated analyses on persuasiveness controlling for these two factors.
The results were nearly identical to those reported above. Means and
standard deviations for speech behavior are provided in Table 3.
3.6. Covariate analyses
Because the groups significantly differed on ratings of speech persuasiveness, we examined whether persuasiveness, as a proxy for behavioral
mobilization, explained the differences in reactivity and recovery. When
persuasiveness was entered as a covariate into all significant ANCOVAs,
results were unchanged. Therefore, speech persuasiveness did not account for the differences in reactivity and recovery among MDD, RMD,
and healthy controls.
We repeated all analyses including antidepressant medication use as a
covariate to examine if medications explained differences in reactivity.
Antidepressant use was dummy-coded (1 = used antidepressants regularly in past month, 0 = did not use antidepressants regularly in past
month). Similarly, we repeated all analyses including dummy-coded
comorbid anxiety disorder as a covariate (1 = present, 2 = absent).
The results were virtually identical to those reported above and neither
medication use nor comorbid anxiety disorder was a significant covariate.
4. Discussion
Depression has been repeatedly associated with blunted cardiovascular reactivity, but the psychobiological basis of this effect is unclear.
The present study was designed to determine if the blunted reactivity
associated with MDD fluctuates with the depressed state or if it is a stable biomarker of risk for depression. The present findings suggest the
former. In this sample, those diagnosed with MDD exhibited a pattern
of attenuated reactivity relative to healthy controls, replicating prior
findings in MDD (Salomon et al., 2009), but those who had previously
Table 3
Descriptive statistics for speech behavior.
Measure
Group
MDD
Persuasiveness, M (SD)⁎
# of words, M (SD)
Dysfluency, M (SD)
# of prompts required to
continue, M (SD)
# of positive emotionality
words, M (SD)
# of negative emotionality
words, M (SD)
4.67
423.26
7.00
1.16
(2.07)
(74.50)
(6.20)
(1.34)
RMD
Control
5.14 (1.81)
465.45 (82.50)
9.05 (8.76)
1.09 (1.27)
6.13
446.16
6.47
1.25
(2.27)
(84.56)
(3.93)
(1.70)
1.98 (1.01)
2.19 (0.97)
2.23 (1.04)
1.01 (0.60)
1.09 (0.98)
1.10 (0.54)
Note. # = number.
⁎ Significant difference between MDD and healthy controls (p b .05).
suffered a major depressive episode, but were currently no longer depressed exhibited a similar pattern of reactivity to the healthy controls.
If blunted reactivity was a biomarker of risk for depression, we would
expect that the remitted-depression group would look similar to the depressed group in terms of reactivity. While these findings suggest that
the blunted reactivity seen during a major depressive episode remits
along with depression, returning to normative levels of cardiovascular
reactivity, the cross-sectional nature of the current study prevents
strong conclusions on this score. To better test this idea, a longitudinal
design would be optimal.
Relatedly, we sought to isolate the psychobiological basis of blunted
reactivity in depression. If blunted reactivity reflects a fundamental compromise in the capacity for physiological response, then we would expect
that the MDD group would show also blunted reactivity to a cold pressor
relative to healthy controls. This was not the case. Our findings are in
agreement with others finding depression-related blunted reactivity to
active coping, beta-adrenergic stressors (Carroll et al., 2007; Phillips et
al., 2011; York et al., 2007) but not passive coping, alpha-adrenergic
stressors (Salomon et al., 2009). However, Schwerdtfeger and
Rosenkaimer (2011) suggest that task self-relevance, not hemodynamic
profile, may be critical for finding blunted reactivity associated with depression. They used three tasks: a beta-adrenergic speech task (giving a
speech) and two alpha-adrenergic tasks (watching the video of their
speech and a cold pressor). They found an association between depressive symptomatology and blunted reactivity during both speech stressors
— one active/beta-adrenergic and one passive/alpha-adrenergic. Thus,
their findings suggest that the self-relevance of the task is of greater importance than the specific adrenergic response that the task elicits
(Schwerdtfeger and Rosenkaimer, 2011). Neither our present nor prior
studies include an alpha-adrenergic self-relevant task so we cannot
make this comparison, but we agree with Schwerdtfeger & Rosenkaimer,
and feel that our data supports their views regarding task self-relevance
and blunted reactivity in depression. Finally, one further consideration
with the present findings is that the cold pressor task did not elicit the
same degree of reactivity as the speech task. Thus the lack of group differences in cold pressor reactivity may be due to an overall lower level of
reactivity.
Differences were only observed on a self-relevant speech task that required active coping. We reasoned that if blunted reactivity during the
speech task reflects motivational deficits, that we would be able to see
signs that depressed participants were withholding effort during the
task. We examined effort by coding participants' speeches for indices of
emotional content, behavioral mobilization and motivational investment.
No differences in the number of positive or negative emotional words
used during the speech emerged between groups. Although evidence
suggests that depressed individuals use more negative and fewer positive
words in their speech (Pennebaker et al., 2003; Rude et al., 2004), our
study suggests that these differences do not occur in the context of a laboratory reactivity speech task. The groups also did not differ on indices of
behavioral mobilization. Those with MDD spoke as many words, spoke
them with similar fluency, and required a similar number of prompts to
continue as participants in the other groups. The only difference was
that the speeches given by the MDD group were rated as less persuasive
than the speeches given by the other two groups. While persuasiveness
does imply effort, it suggests a lack of motivational investment in
performing well, not necessarily a lack of behavioral effort to engage in
the task. However, the differences in persuasiveness did not explain the
differences in cardiovascular reactivity.
While we believe that persuasiveness captures a key aspect of motivational investment in the present study, we also think it is possible that
more subtle motivational deficits in depression may explain blunted reactivity during active coping tasks like a speech stressor. For example,
less persuasive speeches may have been a downstream result of reduced motivational investment during the speech preparation phase,
which we did not assess. Future work could address this issue through
a thought sampling technique which might determine the number of
Please cite this article as: Salomon, K., et al., Is blunted cardiovascular reactivity in depression mood-state dependent? A comparison of major
depressive..., International Journal of Psychophysiology (2013), http://dx.doi.org/10.1016/j.ijpsycho.2013.05.018
K. Salomon et al. / International Journal of Psychophysiology xxx (2013) xxx–xxx
speech-related versus unrelated thoughts. Thus our measure of investment may have been too limited or specific to fully capture the spectrum of motivational deficits explaining differences in blunted
reactivity.
Blunted reactivity recently has been proposed as a marker of emotion
and motivation dysregulation (Carroll et al., 2009; Lovallo, 2011).
According to these authors, reactivity outside the normative range, either
blunted or exaggerated, may have implications for poor health. Blunted
reactivity has been linked to a number of disorders and psychological
states associated with deficits in emotional and motivational regulation
such as depressive symptomatology (Carroll et al., 2007), disordered
eating (Ginty et al., 2012), obesity (Carroll et al., 2008), and risk for addiction (Lovallo, 2007; Panknin et al., 2002). Further, blunted reactivity has
been associated with a number of conditions that are associated with
poor health including fibromyalgia (Reyes del Paso et al., 2010), fatigue
(Peckerman et al., 2000), racial/ethnic discrimination (Salomon and
Jagusztyn, 2008) and low cognitive ability (Ginty et al., 2011). Our findings provide some tentative support for motivational dysregulation in
depression. While seemingly putting forth as much behavioral effort during the speech, depressed participants were unable to be as persuasive as
the remitted and healthy control participants. Similar to obese individuals
who try to lose weight or alcoholics who try not to drink, perhaps depressed individuals best efforts to successfully perform the speech task
are ultimately unsuccessful. Similarly, our findings support the contention that blunted reactivity is an indicator of risk for poor psychological
and physical health.
Our findings also demonstrated group differences in SBP recovery
such that the MDD group evidenced impaired recovery relative to the
RMD and control groups. Although differences during the recovery period
were modest, this finding also replicates and extends our previous work.
In addition, a lack of recovery has been identified as one pattern of
allostatic load (McEwen, 1998). Impaired recovery is specifically significant because of its link to increased risk for cardiovascular disease
(Chida and Steptoe, 2010; Hocking Schuler and O'Brien, 1997; Steptoe
et al., 2006; Steptoe and Marmot, 2006), indicating one potential pathway
placing those with depression at greater risk for disease. Impaired cardiovascular recovery has been linked to a number of processes likely to operate in depression, such as perseverative cognition (Nolen-Hoeksema,
2000; Spasojevic and Alloy, 2001), including anxiety, worry, and rumination (Brosschot et al., 2006; Glynn et al., 2002). Thus it is possible that
depression leads to increased perseveration after the task, and thus, impaired recovery.
Most published research showing blunted cardiovascular reactivity
examined only heart rate and blood pressure responses. The present
study adds to this literature by demonstrating the autonomic and hemodynamic underpinnings of blunted reactivity. Namely, the PEP and CO
responses seen in the MDD group suggest that the blunted HR and SBP
responses are driven by sympathetic cardiac influences. Additionally,
findings from our prior sample, as well as the current sample show
that respiratory sinus arrhythmia reactivity is also blunted in MDD
(Salomon et al, 2009; Bylsma et al., under review) suggesting that
blunted HR reactivity is concurrently driven by a lack of withdrawal of
parasympathetic control during stress.
The present study utilized a sample of currently and formerly depressed people that was reasonably representative and thus contained
individuals who had other conditions and were taking medication. Additional covariate analyses including comorbid anxiety disorder and
medication use suggested that these were not confounds but with our
design, we cannot entirely rule out the possibility of confounding with
comorbid anxiety and medication use. The generalizability of the
present findings is also limited by the relatively small sample size.
Requiring MDD as determined by clinical interviews is resource
intensive and often result in smaller samples than those utilizing
normative levels of self-reported depressive symptomatology. For
this reason, it is reassuring that the present findings converge with
evidence showing that symptoms of depression are associated with
7
blunted reactivity in a large prospective cohort (Carroll et al., 2007;
Phillips et al., 2011).
In sum, individuals with MDD exhibited less reactivity relative to
never-depressed healthy controls and asymptomatic formerly depressed
individuals. Future research should involve longitudinal methods to better address whether blunted reactivity tracks episodic depression within
the same individuals. Also, a better understanding of the specific emotional and motivational deficits associated with blunted reactivity is
warranted, given that blunted reactivity seems to be associated with
not only depression, but a number of maladaptive psychological profiles.
Acknowledgments
The authors would like to acknowledge April Taylor-Clift, Bethany
Morris and Kristina Przystawik for their assistance in conducting this
study. This study was funded by NIH/NIMH R21MH077669-01A1.
References
al'Absi, M., Wittmers, L.E., Erickson, J., Hatsukami, D., Crouse, B., 2003. Attenuated adrenocortical and blood pressure responses to psychological stress in ad libitum and abstinent
smokers. Pharmacology, biochemistry, and behavior 74, 401–410.
Aston-Jones, G., Cohen, J.D., 2005. An integrative theory of locus coeruleus–norepinephrine
function: adaptive gain and optimal performance. Annual Review of Neuroscience vol.
28, vol. 28, pp. 403–450.
Beck, A.T., Brown, G., Epstein, N., Steer, R.A., 1988. An inventory for measuring clinical
anxiety — psychometric properties. Journal of Consulting and Clinical Psychology
56 (6), 893–897.
Beck, A.T., Steer, R.A., Brown, G.K., 1996. Manual for the BDI-II. Psychological Corporation,
San Antonio, TX.
Brosschot, J.F., Gerin, W., Thayer, J.F., 2006. The perseverative cognition hypothesis: a
review of worry, prolonged stress-related physiological activation, and health.
Journal of Psychosomatic Research 60 (2), 113–124.
Bylsma, L.M., Salomon, K., Taylor-Clift, A., Morris, B., Rottenberg, J., 2013. Blunted respiratory sinus arrhythmia reactivity in major depressive disorder marks the depressed state.
(under review).
Carroll, D., Phillips, A.C., Hunt, K., Der, G., 2007. Symptoms of depression and cardiovascular
reactions to acute psychological stress: evidence from a population study. Biological
Psychology 75, 68–74.
Carroll, D., Phillips, A.C., Der, G., 2008. Body mass index, abdominal adiposity, obesity,
and cardiovascular reactions to psychological stress in a large community sample.
Psychosomatic Medicine 70 (6), 653–660.
Carroll, D., Phillips, A.C., Lovallo, W.R., 2009. Are large physiological reactions to acute
psychological stress always bad for health? Social and Personality Compass
(Health Section) 3, 725–743. http://dx.doi.org/10.1111/j.1751-9004.2009.00205.x.
Chida, Y., Steptoe, A., 2010. Greater cardiovascular responses to laboratory mental stress
are associated with poor subsequent cardiovascular risk status: a meta-analysis of
prospective evidence. Hypertension 55 (4), 1026–U1368.
de Rooij, S.R., Schene, A.H., Phillips, D.I., Roseboom, T.J., 2010. Depression and anxiety:
associations with biological and perceived stress reactivity to a psychological stress
protocol in a middle-aged population. Psychoneuroendocrinology 35 (6), 866–877.
First, M.B., Spitzer, R.L., Gibbon, M., Williams, J.B.W., First, M.B., Spitzer, R.L., Gibbon, M.,
Williams, J.B.W., 2002. Structured Clinical Interview for DSM-IV-TR Axis I Disorders,
Research Version, Patient Edition with Psychotic Screen (SCID-I/P W/PSY SCREEN).
Biometrics Research, New York State Psychiatric Institute, New York (November).
Gendolla, G.H.E., Krusken, J., 2001. The joint impact of mood state and task difficulty on
cardiovascular and electrodermal reactivity in active coping. Psychophysiology 38
(3), 548–556.
Gendolla, G.H.E., Krusken, J., 2002. The joint effect of informational mood impact and
performance-contingent consequences on effort-related cardiovascular response.
Journal of Personality and Social Psychology 83 (2), 271–283.
Ginty, A.T., Phillips, A.C., Der, G., Deary, I.J., Carroll, D., 2011. Heart rate reactivity is associated
with future cognitive ability and cognitive change in a large community sample. International Journal of Psychophysiology 82 (2), 167–174.
Ginty, A.T., Phillips, A.C., Higgs, S., Heaney, J.L.J., Carroll, D., 2012. Disordered eating behaviour
is associated with blunted cortisol and cardiovascular reactions to acute psychological
stress. Psychoneuroendocrinology 37 (5), 715–724.
Glynn, L.M., Christenfeld, N., Gerin, W., 2002. The role of rumination in recovery from
reactivity: cardiovascular consequences of emotional states. Psychosomatic
Medicine 64 (5), 714–726.
Hamilton, M., 1960. A rating scale for depression. Journal of Neurology, Neurosurgery,
and Psychiatry 23 (1), 56–62.
Heaney, J.L.J., Ginty, A.T., Carroll, D., Phillips, A.C., 2011. Preliminary evidence that exercise
dependence is associated with blunted cardiac and cortisol reactions to acute psychological stress. International Journal of Psychophysiology 79 (2), 323–329.
Heath, M.E., Downey, J.A., 1990. The cold face test (diving reflex) in clinical autonomic
assessment: methodological considerations and repeatability responses. Clinical
Science 78 (2), 139–147.
Hocking Schuler, J.L., O'Brien, W., 1997. Cardiovascular recovery from stress and hypertension risk factors: a meta-analytic review. Psychophysiology 34, 649–659.
Please cite this article as: Salomon, K., et al., Is blunted cardiovascular reactivity in depression mood-state dependent? A comparison of major
depressive..., International Journal of Psychophysiology (2013), http://dx.doi.org/10.1016/j.ijpsycho.2013.05.018
8
K. Salomon et al. / International Journal of Psychophysiology xxx (2013) xxx–xxx
Jennings, J.R., Berg, W.K., Hutcheson, J.S., Obrist, P., Porges, S., Turpin, G., 1981. Publication
guidelines for heart rate studies in man. Psychophysiology 18 (3), 226–231.
Kuper, H., Marmot, M., Hemingway, H., 2002. Systematic review of prospective cohort
studies of psychosocial factors in the etiology and prognosis of coronary heart
disease. Seminars in Vascular Medicine 2, 267–314.
Lovallo, W.R., 2007. Individual differences in response to stress and risk for addiction. In:
al' Absi, M. (Ed.), Stress and Addiction: Biological and Psychological Mechanisms.
Academic Press, MA, USA, pp. 227–248.
Lovallo, W.R., 2011. Do low levels of stress reactivity signal poor states of health? Biological
Psychology 86 (2), 121–128.
McEwen, B.S., 1998. Stress, adaptation, and disease — allostasis and allostatic load. In:
McCann, S.M., Lipton, J.M., Sternberg, E.M., Chrousos, G.P., Gold, P.W., Smith, C.C.
(Eds.), Neuroimmunomodulation: Molecular Aspects, Integrative Systems, and
Clinical Advances: , vol. 840, pp. 33–44.
Nolen-Hoeksema, S., 2000. The role of rumination in depressive disorders and mixed
anxiety/depressive symptoms. Journal of Abnormal Psychology 109, 504–511.
Panknin, T.L., Dickensheets, S.L., Nixon, S.J., Lovallo, W.R., 2002. Attenuated heart rate
responses to public speaking in individuals with alcohol dependence. Alcoholism,
Clinical and Experimental Research 26 (6), 841–847.
Peckerman, A., LaManca, J.J., Smith, S.L., Taylor, A., Tiersky, L., Pollet, C., et al., 2000.
Cardiovascular stress responses and their relation to symptoms in Gulf War
veterans with fatiguing illness. Psychosomatic Medicine 62 (4), 509–516.
Pennebaker, J.W., Mehl, M.R., Niederhoffer, K.G., 2003. Psychological aspects of natural
language use: our words, our selves. Annual Review of Psychology 54, 547–577.
Penninx, B., Beekman, A.T.F., Honig, A., Deeg, D.J.H., Schoevers, R.A., van Eijk, J.T.M., et al.,
2001. Depression and cardiac mortality — results from a community-based longitudinal
study. Archives of General Psychiatry 58, 221–227.
Phillips, A.C., Hunt, K., Der, G., Carroll, D., 2011. Blunted cardiac reactions to acute psychological stress predict symptoms of depression five years later: evidence from a large community study. Psychophysiology 48 (1), 142–148.
Reyes del Paso, G.A.R., Garrido, S., Pulgar, A., Martin-Vazquez, M., Duschek, S., 2010.
Aberrances in autonomic cardiovascular regulation in fibromyalgia syndrome and
their relevance for clinical pain reports. Psychosomatic Medicine 72 (5), 462–470.
Reyners, A.K.L., Tio, R.A., Vlutters, F.G., van der Woude, G.F., Reitsma, W.D., Smit, A.J.,
2000. Re-evaluation of the cold face test in humans. European Journal of Applied
Physiology 82 (5–6), 487–492.
Rottenberg, J., Salomon, K., Gross, J.J., Gotlib, I.H., 2005. Vagal withdrawal to sad film
predicts subsequent recovery from depression. Psychophysiology 42, 277–281.
Rottenberg, J., Clift, A., Bolden, S., Salomon, K., 2007. RSA fluctuation in major depressive
disorder. Psychophysiology 44, 450–458.
Rude, S.S., Gortner, E.M., Pennebaker, J.W., 2004. Language use of depressed and
depression-vulnerable college students. Cognition & Emotion 18 (8), 1121–1133.
Rugulies, R., 2002. Depression as a predictor for coronary heart disease: a review and
meta-analysis. American Journal of Preventative Medicine 23, 51–61.
Ruiz, J.M., Uchino, B.N., Smith, T.W., 2006. Hostility and sex differences in the magnitude,
duration, and determinants of heart rate response to forehead cold pressor:
parasympathetic aspects of risk. International Journal of Psychophysiology 60
(3), 274–283.
Salomon, K., Jagusztyn, N.E., 2008. Resting cardiovascular levels and reactivity to interpersonal incivility among Black, Latina/o, and White individuals: the moderating
role of ethnic discrimination. Health Psychology 27 (4), 473–481.
Salomon, K., Clift, A., Karlsdottír, M., Rottenberg, J., 2009. Major depressive disorder is
associated with attenuated cardiovascular reactivity and impaired recovery
among those free of cardiovascular disease. Health Psychology 28, 157–165.
Schwerdtfeger, A., Rosenkaimer, A.-K., 2011. Depressive symptoms and attenuated physiological reactivity to laboratory stressors. Biological Psychology 87 (3), 430–438.
Shapiro, D., Jamner, L.D., Lane, J.D., Light, K.C., Myrtek, M., Sawada, Y., et al., 1996. Blood
pressure publication guidelines. Psychophysiology 33, 1–12.
Sherwood, A., Allen, M.T., Fahrenberg, J., Kelsey, R.M., Lovallo, W.R., Van Dooren, L.J.P.,
1990. Methodological guidelines for impedance cardiography. Psychophysiology
27, 1–23.
Spasojevic, J., Alloy, L.B., 2001. Rumination as a common mechanism relating depressive
risk factors to depression. Emotion 1, 25–37.
Steptoe, A., Marmot, M., 2006. Psychosocial, hemostatic, and inflammatory correlates
of delayed poststress blood pressure recovery. Psychosomatic Medicine 68 (4),
531–537.
Steptoe, A., Donald, A.E., O'Donnell, K., Marmot, M., Deanfield, J.E., 2006. Delayed
blood pressure recovery after psychological stress is associated with carotid
intima–media thickness — Whitehall Psychobiology Study. Arteriosclerosis,
Thrombosis, and Vascular Biology 26 (11), 2547–2551.
Wright, R.A., Dill, J.C., 1993. Blood-pressure responses and incentive appraisals as a
function of perceived ability and objective task demand. Psychophysiology 30
(2), 152–160.
Wright, R.A., Williams, B.J., Dill, J.C., 1992. Interactive effects of difficulty and instrumentality
of avoidant behavior on cardiovascular reactivity. Psychophysiology 29 (6), 677–686.
Wuslin, L.R., Singal, B.M., 2003. Do depressive symptoms increase the risk for the onset
of coronary disease? A systematic quantitative review. Psychosomatic Medicine
65, 201–210.
Yerkes, R.M., Dodson, J.D., 1908. The relation of strength of stimulus to rapidity of habitformation. Journal of Comparative Neurology and Psychology 18 (5), 459–482.
York, K.M., Hassan, M., Li, Q., Li, H., Fillingim, R.B., Sheps, D.S., 2007. Coronary artery disease
and depression: patients with more depressive symptoms have lower cardiovascular
reactivity during laboratory-induced mental stress. Psychosomatic Medicine 69 (6),
521–528.
Please cite this article as: Salomon, K., et al., Is blunted cardiovascular reactivity in depression mood-state dependent? A comparison of major
depressive..., International Journal of Psychophysiology (2013), http://dx.doi.org/10.1016/j.ijpsycho.2013.05.018