Student Athletic Trainer Manual
advertisement

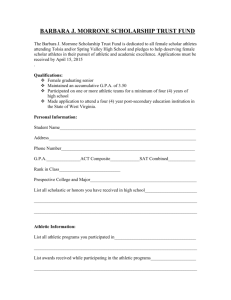
I. INTRODUCTION Introduction to the Manual The Athletic Training Education Program is designed to teach undergraduate students the knowledge, skills, and attitudes necessary to be a Certified Athletic Trainer. This program is a weave of classroom lecture, discussion, demonstration, and practice with clinical observation, learning, application, and experience. An effective educational process requires the collaborative effort of faculty, students, and clinical instructors. The information in this manual details the educational, clinical and professional standards of the program. These standards should guide students, faculty, and clinical instructors in the effective presentation, understanding, and application of educational competencies and clinical proficiencies over time. Students enrolled in the Athletic Training Education Program must be familiar with the guidelines set forth in this manual. They are expected to take initiative in their learning by being prepared for class, asking questions, taking advantage of learning opportunities, and making their education a high priority. During classroom and clinical experiences, students should display professional behavior consistent with the Code of Ethics. Finally, students, faculty, and clinical instructors should be respectful of each other, their patients, the facilities and equipment, and the profession of athletic training. Any questions regarding this manual or the Athletic Training Education Program should be directed to the Program Director for Athletic Training, 815-836-5921. To ensure effective communication of policies and procedures, I acknowledge that I have read, understand, and agree to follow the policies and procedures listed in the ATHLETIC TRAINING EDUCATION PROGRAM MANUAL. Any questions regarding policies or procedures mentioned in this manual should be directed to the Athletic Training Program Director. Athletic Training Student ____________________________________ Signature _____________________________________ Date ________________ 2 ATHLETIC TRAINING, AN ALLIED HEALTHCARE PROFESSION A Certified Athletic Trainer is an allied health care professional who collaborates with physicians to optimize activity and participation of patients and clients. The Certified Athletic Trainer functions as an integral member of the athletic health care team in secondary schools, colleges and universities, professional sports programs, sports medicine clinics, and other health care settings. The roles of the Athletic Trainer has been defined by the ROLE DELINEATION STUDY in the following manner: 1. Prevention of Athletic Injuries 2. Recognition, Evaluation, and Immediate Care of Athletic Injuries 3. Rehabilitation and Reconditioning of Athletic Injuries 4. Health Care Administration 5. Professional Development and Responsibility THE NATIONAL ATHLETIC TRAINERS’ ASSOCIATION The NATA is a member-based trade association that strives to enhance the quality of health care delivered by certified athletic trainers. The National Athletic Trainers' Association (NATA) was founded in 1950 in Kansas City. It’s mission is to enhance the quality of health care provided by certified athletic trainers and to advance the athletic training profession. An annual meeting and clinical symposia is held each year in June. The NATA has more than 30,000 members worldwide from a variety of health care professions. Students are encouraged to become a member of the NATA. For an application, benefits of membership and additional information about the NATA please visit their website: http://www.nata.org/. -Taken from NATA Website ACCREDITING AGENCIES The Joint Review Committee on Educational Programs in Athletic Training (JRC-AT) was incorporated in Texas in October 1991. The JRC-AT was a Committee on Accreditation under the Commission on Accreditation of Allied Health Educational Programs (CAAHEP); effective June 30, 2006, the JRC-AT became independent from CAAHEP and changed its name to the Commission on Accreditation of Athletic Training Education (CAATE). The CAATE is the agency responsible for the accreditation of professional (entry-level) Athletic Training educational programs. The CAATE has defined policies and procedures which can be found on the Commission’s website (www.caate.net). -Taken from the CAATE Website 3 BOARD OF CERTIFICATION, Inc. The National Athletic Trainers' Association Board of Certification Inc. (BOC) has been responsible for the certification of athletic trainers since 1969. Upon its' inception, the BOC was an entity of the professional membership organization the National Athletic Trainers' Association (NATA). However, in 1989, the BOC became an independent non-profit corporation. The Mission of the Board of Certification is to certify athletic trainers and to identify for the public, quality healthcare professionals through a system of certification, adjudication, standards of practice and continuing competency programs. Accordingly the BOC provides a certification program for the entry-level athletic trainer and establishes requirements for maintaining status as a Certified Athletic Trainer (ATC). The BOC is the only accredited certification program for athletic trainers in the United States. For additional information please see their website: www.bocatc.org ILLINOIS ATHLETIC TRAINERS ASSOCIATION The Illinois Athletic Trainers' Association (IATA) works to: 1. Improve the quality of athletic health care in the State of Illinois through the advancement, promotion, and improvement of the Athletic Training Profession at all levels 2. Promote a better working relationship among those persons interested in Athletic Training by providing a means for a free exchange of ideas within the profession. For more information on becoming a member of the IATA or to learn what your state organization is doing for you visit: http://www.illinoisathletictrainers.org/ Athletic training in Illinois is governed by the Illinois Athletic Training Practice Act. This piece of legislation applies to certified athletic trainers and students studying athletic training. To see a copy of the act go to the Department of Financial and Professional Regulations website: http://www.idfpr.com/DPR/default.asp 4 II. THE ATHLETIC TRAINING EDUCATION PROGRAM 5 THE MISSION STATEMENT OF THE ATHLETIC TRAINING EDUCATION PROGRAM The mission of the Lewis University Athletic Training Education Program is to provide a comprehensive, entry-level educational and clinical foundation for undergraduate students wishing to pursue BOC certification and a career as a Certified Athletic Trainer. The educational program presents current, scientifically-based instruction and application of anatomy, exercise physiology, physical assessment, nutrition, rehabilitation, and administration. The diverse clinical program encourages professional behavior, the application of knowledge, and the development of critical thinking. PROGRAM GOALS 1. Maintain CAATE accreditation 2. Provide students with quality education 3. Attract and retain exemplary faculty 4. Secure superlative clinical experiences 5. Identify and collaborate with conscientious clinical instructors (CI) 6. Prepare students to be health care professionals and Certified Athletic Trainers ACCREDITATION STATUS Beginning January 1, 2004, only students who graduate from a CAATE Accredited Athletic Training Education Program are eligible to apply for the BOC Certification Examination. The Lewis University Athletic Training Education Program was granted full initial accreditation in October, 2003. Graduates of this program are eligible to apply for the BOC Certification Examination and apply for Illinois State licensure. For additional information regarding CAATE accreditation, please see the Program Director for Athletic Training. 6 FACULTY AND ADMINISTRATION INTERIM DEAN, COLLEGE OF ARTS & SCIENCES Dr. Cathy Ayers 815-836-5242 MEDICAL DIRECTOR/TEAM PHYSICIAN Dr. Pietro Tonino 708-216-8730 CHAIRPERSON, SPORT & EXERCISE SCIENCE DEPT. Karen Lockyer 815-836-5454 PROGRAM DIRECTOR Cathy Bohlin 815-836-5921 ASSISTANT PROFESSOR Lark Welch 815-836-5823 ASSISTANT PROFESSOR Dr. Ralph Miller 815-836-5934 ASSOCIATE PROFESSOR Dr. Pat Vidmar-Scubic 815-836-5930 CLINICAL SITES ATHLETIC & THERAPEUTIC INSTITUTE-JOLIET ATHLETIC & THERAPEUTIC INSTITUTE–AURORA DOWNERS GROVE SOUTH HIGH SCHOOL HINSDALE CENTRAL HIGH SCHOOL HINSDALE SOUTH HIGH SCHOOL JOLIET CATHOLIC ACEDEMY JOLIET JUNIOR COLLEGE LEWIS UNIVERSITY LOCKPORT HIGH SCHOOL NEWSOME PHYSICAL THERAPY NEWSOME PHYSICAL & HAND THERAPY PLAINFIELD NORTH HIGH SCHOOL PLAINFIELD CENTRAL HIGH SCHOOL PLAINFIELD SOUTH HIGH SCHOOL UNIVERSITY OF ST. FRANCIS 815-577-9936 630-236-7544 630-795-8905 630-570-8236 630-468-4236 ADVENTIST BOLINGBROOK HOSPITAL ROMEOVILLE FIRE DEPARTMENT 630-226-8100 815-886-7227 Ext. 356 815-741-2499 815-836-5614/815-836-5446 815-588-8416 815-744-4660 630-357-4253 815-609-8506 Ext. 2603 815-439-3265 Ext. 3033 815-439-5555 Ext. 5727 815-740-3845 7 REQUIRED COURSEWORK 16-171 First Aid and CPR (1) 16-196 Human Anatomy (3) 16-197 Human Physiology (3) 16-211 Weight Training (3) 16-250 Introduction to Athletic Training (3) 16-251 Athletic Taping Lab (1) 16-256 Sport Psychology (3) 16-263 Physical Assessment of the Lower Extremity (3) 16-264 Physical Assessment of the Lower Extremity Lab (1) 16-265 Physical Assessment of the Upper Extremity (3) 16-266 Physical Assessment of the Upper Extremity Lab (1) 16-271 Nutrition and Exercise (3) 16-275 Health (3) 16-300 Disease Processes and Exercise (3) 16-304 Clinical I (1) 16-305 Clinical II (1) 16-306 Emergency Care (1) 16-307 Pharmacology for Sport and Exercise Science (1) 16-340 Kinesiology (3) 16-345 Exercise Physiology (3) 16-361 Athletic Training Management (3) 16-370 Legal Aspects of Sport (3) 16-405 Clinical III (1) 16-406 Professional Development for Athletic Trainers (1) 16-440 Therapeutic Exercise (3) 16-441 Therapeutic Modalities (3) 16-481 Internship (4) =========================== 62 Total Hours Minimum of “C” grade in all Athletic Training required Courses Minimum of "B" grade in all Athletic Training Lab/Clinical Courses Students must maintain an overall GPA of 2.5 or above Students who receive a failing grade in a clinical or lab will be dismissed from the ATEP University Requirements for Graduation Students must meet the following requirements to earn a Bachelor of Arts Degree, in addition to the requirement for the Athletic Training major: Successfully complete 128 hours Complete the last 32 hours of course work at Lewis University Complete General Education Requirements listed in the University Catalog specific to the year you entered the University 8 Sample Schedule for Student Entering as a Freshman FALL 1 Weight Training (3) Human Anatomy (3) First Aid and CPR (1) SPRING 1 Introduction to Athletic Training (3) Human Physiology (3) Athletic Taping Lab (1) FALL 2 Physical Exam of the Upper Extremity (3) Physical Exam of the Upper Ext. Lab (1) Kinesiology (3) Nutrition & Exercise (3) Emergency Care (1) SPRING 2 Physical Exam of the Lower Extremity (3) Physical Exam of the Lower Extremity Lab (1) Therapeutic Modalities (3) Disease Processes and Exercise (3) Health (3) Pharmacology for Sport & Exercise Science (1) FALL 3 Clinical I (1) Sport Psychology (3) Therapeutic Exercise (3) SPRING 3 Athletic Training Management (3) Exercise Physiology (3) Clinical II (1) FALL 4 SPRING 4 Clinical III (1) Internship (4) Legal Aspects of Sport (3) Professional Development for Athletic Trainers (1) Sample Schedule for Transfer Students FALL 1 Weight Training (3) Human Anatomy (3) First Aid and CPR (1) Athletic Taping Lab (1) Introduction to Athletic Training (3) SPRING 1 Physical Exam of the Lower Extremity (3) Human Physiology (3) Health (3) Physical Exam of the Lower Extremity Lab (1) Pharmacology for Sport & Exercise Science (1) FALL 2 Physical Exam of the Upper Extremity (3) Physical Exam of the Upper Ext. Lab (1) Kinesiology (3) Nutrition & Exercise (3) Emergency Care (1) SPRING 2 Athletic Training Management (3) Clinical I (1) Therapeutic Modalities (3) Exercise Physiology (3) Disease Processes and Exercise (3) FALL 3 SPRING 3 Legal Aspects of Sport (3) Clinical III (1) Therapeutic Exercise (3) Sport Psychology (3) Clinical II (1) Professional Development for Athletic Trainers (1) SUMMER 3 Internship (4) 9 ACADEMIC ADVISEMENT Faculty Academic Advisor Students planning to study Athletic Training should declare Athletic Training as their major as soon as possible. This form is available in the Dean of the College of Art's and Sciences office. Students should meet with the Athletic Training Program Director or faculty advisor in the Department of Sport and Exercise Science prior to registering for each semester. Student Responsibility It is the responsibility of each student to know and to meet graduation requirements and to make a reasonable effort to obtain adequate academic advisement. Students should schedule regular appointments with their academic advisor to discuss progress towards graduation requirements, academic difficulties, and career goals. University and Major requirements for Graduation are published in the University Catalog. Transfer Credit Upon admission to Lewis University, the Office of Admissions and the Athletic Training Program Director evaluate transcripts from previously attended academic institutions. The decision to accept a required course from another institution is based on course content and whether required competencies have been met. Once students have been admitted to Lewis University, NO required Athletic Training courses may be taken at other colleges or universities for transfer to Lewis University without PRIOR approval from the Athletic Training Program Director and Dean of the College of Arts and Sciences. 10 APPLICATION PROCESS The Athletic Training Education Program (ATEP) is a rigorous and time intensive major with a strong academic emphasis. It is necessary for students to have a strong understanding of anatomy and it’s relationship to exercise and injury prior to beginning the clinical portion of the major. There is a 3 phase application process to the ATEP. Application packets are available in the Program Director’s office and students are encouraged to pick up an application packet as soon as possible. The packet includes an explanation of Application procedures, the ATEP manual, and application form, a physical exam form with heath history questionnaire, technical standards information, confidentiality agreement and criteria for acceptance. The application process is the same for ALL students ie: 1st year students, transfer students, and student athletes. Transfer students are advised that the clinical program is a minimum of 7 semesters. PHASE 1 Students must submit documentation of the following requirements by November 15th for enrollment in Physical Assessment of the Lower Extremity Lab during the Spring Semester or April 15th for enrollment in Physical Assessment of the Upper Extremity Lab during the Fall Semester. 1. Copy of current First Aid Card 2. Copy of current CPR Card 3. Passing score (>500) on the TOEFL Written Exam. (International Students Only) 4. Current enrollment in, completion of, or eligibility for College Writing I 5. Completed Health History Form and demonstrate good health and up to date immunizations documented by a Physician on the Physical Exam Form (form provided) 6. Complete, legible Athletic Training Education Program Application (form provided) 7. Two typed, professional letters of recommendation 8. A signed confidentiality agreement (form provided) Students who do not meet the following requirements may not continue with Phase 2 of the application process. 11 PHASE 2 Students who successfully demonstrate each requirement of Phase 1 will be further evaluated using the criteria listed below. The physical test and interview will take place during the first week of December for enrollment in Physical Assessment of the Lower Extremity Lab during the Spring Semester or the last week of April for enrollment in Physical Assessment of the Upper Extremity Lab during the Fall Semester. 1. Successfully (80%) demonstrate the following skills during a physical test. -Lower body stretching -Splint an upper extremity injury -Demonstrate a functional taping based on injury -Perform a 2-person seated carry -Demonstrate appropriate rescue breathing and CPR techniques as indicated -Apply and Explain the RICE technique to a mock patient 2. Successfully (80%) demonstrate the ability to engage in professional communication during an interview. Specifically students will be evaluated on their ability to: -understand and speak the English language at a level consistent with professional practice -maintain composure during a stressful situation -display appropriate demeanor and rapport that relate to professional education and quality patient care PHASE 3 It will be verified that students who have successfully completed Phase I and Phase II have also: 1. passed (>70%) the Introduction to Athletic Training Final Exam 2. passed (>70%) the Athletic Taping Lab Written Final Exam 3. passed (>70%) the Athletic Taping Lab Practical Final Exam 4. Successfully (>90%) completed the Athletic Taping Lab worksheets 5. A cumulative grade point average of 2.5 or above 6. Successfully (C or better) completed: Introduction to Athletic Training Athletic Taping Lab Human Anatomy (or equivalent) First Aid and CPR The number of students accepted is based on the number of clinical sites available. When the number of students qualifying for admittance into the program exceeds the number of openings, acceptance will be based on the student’s GPA in the core courses (Introduction to Athletic Training, Athletic Taping Lab, Human Anatomy, & First Aid and CPR), and their cumulative GPA. Notification of acceptance or rejection into the clinical program will be by U.S. Mail approximately 2 weeks after grades from the fall semester have been completed for enrollment in Physical Assessment of the Lower Extremity Lab during the Spring Semester or after summer grades have been completed for enrollment in Physical Assessment of the Upper Extremity Lab during the Fall Semester. Students who do not meet the criteria may reapply for the clinical program. 12 General Health Requirements Prior to admittance into the Athletic Training Education Program, students will be expected to show good physical and mental health, and current immunizations documented by a physician as part of the General Medical Requirements Document. Additionally, students must meet University immunization requirements and provide documentation of a negative TB test. If at any time during a clinical experience the Clinical Instructor or Program Director has reason to believe the student is not in appropriate physical or mental health the student will be asked to leave the clinical site until proof of appropriate health can be demonstrated. Inappropriate physical and mental health is considered any physical condition that puts the student, other students, the athletic training staff, or patients at risk for disease or illness, or interferes with the student's ability to perform the expected duties. Technical Standards Students in the Athletic Training Education Program must demonstrate: 1. The mental capacity to assimilate, analyze, synthesize, integrate concepts and problem solve to formulate assessment and therapeutic judgments and to be able to distinguish deviations from the norm; 2. Sufficient postural and neuromuscular control, sensory function, and coordination to perform appropriate physical examinations using accepted techniques; and accurately, safely and efficiently use equipment and materials during the assessment and treatment of patients; 3. The ability to communicate effectively and sensitively with patients and colleagues, including individuals from different cultural and social backgrounds; this includes, but is not limited to, the ability to establish rapport with patients and communicate judgements and treatment information effectively. Students must be able to understand and speak the English language at a level consistent with competent professional practice; 4. The ability to record the physical examination results and a treatment plan clearly and accurately; 5. The capacity to maintain composure and continue to function well during periods of high stress; 6. The perseverance, diligence and commitment to complete the athletic training education program as outlined and sequenced; 7. Flexibility and the ability to adjust to changing situations and uncertainty in clinical situations; 8. Affective skills and appropriate demeanor and rapport that relate to professional education and quality patient care. Candidates for selection to the Athletic Training Education Program will be required to verify they understand and meet these technical standards or that they believe, with certain accommodations, they can meet the standards. Each candidate must demonstrate meeting each technical standard during the application process. The LARC Center, in consultation with the BOC, will evaluate a student's request for accommodations and confirm that the stated condition qualifies as a disability under applicable laws. This includes a review of whether the accommodations requested are reasonable, taking into account whether accommodation would jeopardize clinician/patient safety, or the educational process of the student or the institution, including all coursework, clinical experiences and internships deemed essential to graduate. 13 Confidentiality Agreement As a student in the Lewis University Athletic Training Education Program I acknowledge having access to patient/athlete medical records as part of clinical experiences. I also understand that medical records are considered confidential information and disclosing any information regarding the health or health care of an individual including but not limited to: general health, injuries, rehabilitation, treatment, or prognosis without written consent from the individual is illegal. By signing this statement I agree to keep private any patient/athlete medical information that would violate state confidentiality laws. I also agree to accept the consequences for violating this agreement including a written reprimand to be placed in my academic file and possible dismissal from the Lewis University Athletic Training Education Program. Student (Please print) _________________________________ Student Signature ____________________________________ Date __________________ Witness ____________________________________________ **All students admitted to the program will sign and follow this agreement. 14 TERMINOLOGY Direct Supervision Direct supervision is defined as constant visual and auditory interaction between the student and the Clinical Instructor. The Clinical Instructor shall be physically present for proficiency instruction and evaluation. Each student enrolled in an athletic training clinical experience should receive direct supervision from his or her Approved Clinical Instructor (ACI). Supervision This applies to the Internship experiences under the direction of a supervisor. Daily personal/verbal contact at the site of supervision between the athletic training student and the supervisor who plans, directs, advises, and evaluates the students' athletic training field experience. Clinical Education and Field Experience Exposure Requirements Upper Extremity: High-risk sport to the upper extremity based upon injury statistics. Traditionally this would include throwing sports, swimming, gymnastics, etc. that require extensive stresses of the upper extremity of both genders. Lower Extremity: High-risk sport to the lower extremity based upon injury statistics. Traditionally this would include soccer, cross-country running, track, basketball, etc. that require extensive stresses of the lower extremity of both genders. Equipment Intensive: High-risk sports where all participants are required to wear protective equipment for the head and the shoulders. Traditionally this would include football, ice hockey, and men's lacrosse. General Medical: General medical experiences of both genders are those associated with physicians, physician assistants, or nurse practitioners. Clinical Setting The clinical setting shall include the Athletic Training Room, athletic practices, and competitive events. Additional clinical settings may be utilized and may include sports medicine clinics, physical therapy sites, and/or rehabilitation clinics, college or university health centers, hospital emergency rooms, physician's offices, or other appropriate health care settings. The student must be supervised by an appropriate clinical instructor in these settings. Educational Competencies The educational content required of entry-level Athletic Training Education Programs. Clinical Proficiencies The practical skills required of entry-level Certified Athletic Trainers. First Responder Student First Responder has been defined as an individual who uses their skills in first aid and CPR to care for acute injuries/illnesses. Preventative techniques may be applied as taught in the Athletic Taping Lab and Weight Training class including prophylactic taping and bracing, and stretching. 15 ROLES AND RESPONSIBILITIES Team Physician/Medical Director The Team Physician is an essential member of the Sports Medicine Team. The role of the Team Physician is to oversee all activities that occur in the Athletic Training Room. This includes providing medical services to the student-athletes and providing direction to the Certified and Student Athletic Trainers. Specifically, the Team Physician conducts pre-season physicals, assesses and oversees the rehabilitation of illness and injuries, and makes return to play decisions. Interaction with the staff and students is both supervisory and educational in nature. The Medical Director is an interactive part of the Athletic Training Education Program, providing instruction and clinical experiences to students. The responsibilities of the Medical Director is to present lectures on current topics related to Athletic Training, demonstrate examination techniques on a variety of patients, explain and expose students to various diagnostic procedures, facilitate surgical observations, and serve as a resource for students enrolled in the Athletic Training Education Program. Athletic Training Program Director This faculty member is responsible for the development, execution, and modification of all curricular matters that affect the Athletic Training Education Program. Specifically the Program Director verifies instruction on the competencies and clinical proficiencies, discovers, implements, and monitors clinical experiences that meet CAATE standards, and selects, educates, and supervises Clinical Instructors. Good communication between the Athletic Training Program Director, Clinical Instructors, Students, Team Physician/Medical Director, and Staff at clinical sites is essential to provide quality clinical experiences. Finally, the Program Director should seek out opportunities to practice and maintain athletic training skills. Approved Clinical Instructor An Approved Clinical Instructor (ACI) is a BOC Certified Athletic Trainer with a minimum of one year of work experience as an athletic trainer, and who has completed the Approved Clinical Instructor Training Session. Initially, the ACI will provide the student with a brief orientation to the facility, facility policies, and their expectations. Throughout the clinical experience, the ACI provides formal instruction and evaluation of clinical proficiencies in classroom, and/or in clinical education experiences through direct supervision of athletic training students. The ACI has a responsibility to provide students with appropriate, professional experiences and to provide guidance and assistance as needed. A student's clinical instructor should be able to intervene on behalf of the athlete/patient at all times. If necessary, the ACI will file an Incident Report for any violation of the ATEP policies or clinical site policies. It is always the ACI’s perogative to dismiss a student from their site. Finally, a student’s ACI will evaluate the student’s performance at the midpoint and conclusion of the experience. 16 Clinical Instructor A clinical instructor (CI) is a BOC Certified Athletic Trainer or other qualified health care professional with a minimum of one year of work experience in their respective academic or clinical area. Clinical instructors supervise athletic training students in the field experiences. A clinical instructor assumes the same role and responsibilities as an ACI but is not charged with the final formal evaluation of athletic training students' integration of clinical proficiencies. Student The student at a clinical site has the role of a professional in training, and is expected to be professional, responsible, reliable, and prompt. Additionally, the student must abide by state and federal laws regarding sexual harassment and appropriate behavior with a minor. The student should receive direction, instruction, and feedback from their clinical instructor on a daily basis. The student’s experiences should include observation, skill practice, and skill application. The objectives of the course should coordinate with clinical experiences. Application of a skill or technique can only occur once the student has demonstrated competence in the skill during class. If at any time the student does not feel comfortable performing a certain skill the student should inform their supervisor immediately. It is the responsibility of the student to establish and follow a schedule set-up with their clinical instructor. A copy of this schedule should be given to the clinical instructor and the course instructor and a copy retained by the student. The clinical instructor and course instructor should be notified prior to any absences or changes in the schedule. First Responder A student who is not under the direct supervision of a Certified Athletic Trainer or other allied health care professional assumes the role of a First Responder. A First Responder cares for a patient/athlete who has been injured or who is suffering from illness or serious medical problems. The following tasks are considered within the scope of a First Responder: Control of airway, breathing and circulation Control of external bleeding Treatment of shock Treatment of wounds Splinting of broken bones or dislocations Care for victims of a heart attack, stroke, seizure, diabetes, bite, sting, and heat or cold illness. Additionally, preventative techniques may be applied as taught in the Athletic Taping Lab and Weight Training class including prophylactic taping and bracing, and stretching 17 III. PROGRAM POLICIES & PROCEDURES 18 Retention Policy Throughout their academic career, students must: 1. maintain a minimum overall GPA of 2.5 2. achieve a “C” grade in all required courses 3. achieve a "B" grade in all clinical/lab courses 4. show proof of current first aid and CPR certification Students who receive a failing grade in a clinical or lab will be dismissed from the ATEP If the above standards are not met, the student will be considered on probation and ineligible for enrollment in any clinical/lab courses until the standards are achieved. Academic Integrity Policy Scholastic integrity lies at the heart of Lewis University and the Department of Sport and Exercise Science. Students enrolled in classes within the Department of Sport and Exercise Science should expect to be evaluated on their own work. Plagiarism, collusion and other forms of cheating and scholastic dishonesty are incompatible with the principles of Lewis University. Students engaging in such activities are subject to loss of credit and expulsion from the University. Cases involving academic dishonesty are initially considered and determined by the instructor and the Department in which the course is offered. In the Department of Sport and Exercise Science this would include the instructor, Program Director for Athletic Training and the Department Chair. Appeal of the Department of Sport and Exercise Sciences decision is to the Dean of the College of Arts and Sciences, who shall review the decision and make a recommendation to the Vice President for Academic Affairs, whose decision is final. Student Grievance Policy Student grievances with regard to didactic or clinical experiences will be handled using the College of Arts and Sciences Grade Appeal Process published in the University Catalog. Classroom Attendance It is the philosophy of the Athletic Training Education Program that class attendance enhances learning and therefore students are encouraged to attend all classes. The attendance policy for each class is at the discretion of the instructor and is included in the syllabus distributed at the beginning of the semester. 19 Clinical Packets At the beginning of each clinical/lab course students will be given a clinical packet containing: a course syllabus, worksheets, supervisor evaluations, BOC hour verification form(s), and Clinical Hour Record Sheets. This packet should be brought to every class meeting and to all clinical experiences. DO NOT LOSE THE PACKET. Clinical Progressions Appendix A describes a student's progression through their Athletic Training Clinical Education. A logical and purposeful list of proficiencies has been assigned to each clinical experience in the athletic training education program. Each proficiency must be successfully demonstrated and evaluated in a mock situation by an Approved Clinical Instructor (ACI) prior to the skill being utilized in a "live scenario". ACIs should record successful demonstrate of a proficiency in a student's clinical packet. Clinical Hours Each clinical course will have a minimum amount of hours the instructor believes is necessary for a student to learn and practice the skills related to the course objectives. These hours should be recorded daily on a Clinical Hour Record Sheet found in the Clinical Packet. Students should have their clinical instructor sign the Record Sheet at the end of each month. Students can summarize each clinical experience using the Clinical Experience Record found in Appendix C. Clinical Experience Attendance Attendance during each clinical experience is explained in the syllabus for the course. Students are expected to set-up a schedule with their clinical instructor during the first week of class. Once this schedule is established, the student must adhere to the schedule. Missing a scheduled day of clinical partially or in its entirety will affect the student's final grade. If a situation arises and the student is not able to attend clinical their ACI should be notified PRIOR to the student’s scheduled time. Students are allowed 4 absences (regardless of excuse). These will be marked on the hour record accordingly (1, 2, 3, 4). Additional absences will result in a lowering of the student’s final grade. (1 letter grade/absence beyond 4) Clinical Supervision A Certified Athletic Trainer or other appropriate allied health care professional must supervise ALL clinical experiences. In the event where a student is unsupervised they are to act as a First Responder. Student First Responder has been defined as an individual who uses their skills in first aid and CPR to care for acute injuries/illnesses. Preventative techniques may be applied as taught in the Athletic Taping Lab and Weight Training class including prophylactic taping and bracing, and stretching. Athletes/patients who require additional skills beyond those described above must be referred to an appropriate health care provider. 20 Student Travel Policy Students are not required to experience traveling with a team during any clinical experience. A small amount of work-study money is available for students who volunteer for travel with a Lewis University team. Students who apply for work-study positions must be certified in First Aid and CPR, and successfully completed the Athletic Taping Lab and Weight Training Theory and Practice course. The Athletic Training Education Program considers this type of travel as unsupervised. Students who participate in this type of activity are legally responsibility to follow applicable state legislation (ie: state practice act). When traveling, students are to function as a First Responder. (See Roles and Responsibilities on page 16.) Because this travel is for a work-study position, class absences that may result may be considered unexcused. It is the student's responsibility to make arrangements with instructors for any classes they may miss. Transportation Students are responsible for their own transportation to and from on and off-campus clinical sites. 21 OSHA Requirements Students will be not be admitted to the Athletic Training Education Program until a signed Blood Borne Pathogen Risk Statement is on file in the Program Director’s office. Furthermore, each student must successfully complete OSHA Training during the first week of each clinical course. Initial OSHA Training is conducted at the first meeting of the Physical Assessment of the Upper/Lower Extremity Labs. Refresher sessions will occur in all classes containing a clinical component. Students may not begin clinical experiences until a written test, given the 1st week of class is passed with an 80% or better. Students who do not achieve a passing score will be required to complete a self study course and achieve an 80% on a written test prior to beginning any clinical experience. Students who fail to successfully complete this training will be asked to drop the clinical/lab course. Each student is also evaluated on proper OSHA techniques during an oral practical exam during the first 2 weeks of the semester. Students will be expected to follow the OSHA procedures in place at the clinical site they have been assigned. Health Policy Statement All students must meet the following requirements at all times while in the Athletic Training Education Program: 1. Completed physical examination form and medical history attesting to their good health 2. Proper immunization records at University Health & Counseling Services 3. A signed Informed Consent statement acknowledging the health risks inherent in Athletic Training 4. A signed Technical Standards Statement acknowledging the physical and mental demands of Athletic Training. 5. Successfully complete a physical test and interview. (See Application Process on page 11-12) Students absent from clinical experiences due to accident or illness are required to submit a release statement from a physician prior to returning to their clinical site. A copy should be given to the Program Director and their clinical instructor. Available Accommodations A student may request accommodations due to disability, handicap, or other reason. A specific form, available from the Program Director, must be completed and returned. The Lekrone Center for Academic and Career Services (LARC) will review the student's request in collaboration with the BOC. Accommodations will be based on their recommendations. The request must be specific as to the nature of the problem. Medical documentation of specific needs must accompany the request. The student is responsible for demonstrating that the request should be granted. 22 Appearance Standards An individual’s appearance affects a person’s first impression of that individual. From an Athletic Training Student’s first clinical experience to their last, their dress/appearance should always be professional. As a member of the health care industry, Athletic Training Students are expected to present themselves in a clean, well groomed, and professional manner. This type of dress combined with skills and knowledge in the field of Athletic Training will help gain the respect of colleagues, patients, doctors, parents, coaches, and other allied health care professionals. The Department of Sport and Exercise Science has developed the following expectations for Lewis University Athletic Training Students during clinical experiences. This dress code is a minimum requirement and may vary slightly at off-campus facilities. When assigned to an off-campus facility the dress code for that facility must be followed. Students should not expect to see much deviation from this dress code in an off-campus site. Students should expect to be dismissed for the day if they are in violation of the dress code. Repeated violation will result in the student's withdrawal from the clinical. Pants/Shorts: Students should wear "docker-type" pants or shorts or wind/warm-up pants. The pants or shorts should be clean, not torn, and enhance the student's professional appearance. Jeans are not allowed at any time. Shorts should be a minimum of mid thigh length. Shirts: A Lewis University Athletic Training shirt or a solid-colored t-shirt, collared shirt, or sweatshirt should be worn at all clinical experiences. A collared shirt should be worn for events. Lewis University shirts and sweatshirts are preferred. Shoes: Closed toe shoes with socks must be worn in all clinical environments. Jewelry: Jewelry should not be excessive or detract from the student's professionalism. A watch should be worn at all times during clinical experiences. Tattoos: Tattoos should not be visible at any time during a clinical experience. Hair and Makeup: Should be neat and clean. Outdoor events: Certain aspects of your clinical experience will require you to be outside and endure a variety of weather conditions. When discussing clinical experiences and scheduling with the clinical instructor, students should be aware of possible out-door clinical experiences and be prepared for those experiences including rain, snow, and temperature extremes. In any situation your clothing should not restrict you from being able to perform the expected duties. 23 Liability Insurance A liability insurance policy is in place for students enrolled in a clinical or lab course. For further policy information please see the Vice President for Business and Finance. Additionally, students may purchase individual liability insurance policies. See the Program Director for further information. Criminal Background Check Students must be aware that some clinical sites may require drug testing and/or criminal background checks prior to placement at the site. Substance Abuse Policy The use of alcohol, tobacco, and illegal substances is not allowed during a student’s clinical experience. If there is reason to believe a student is under the influence of an illegal substance or a legal substance that might impede their judgement or ability to function during a clinical, the student will be asked to leave the clinical site, and an incident report will be placed in the student’s department academic file. Prior to resuming clinical activities the student must meet with the Program Director and have their consent to resume such activities. Code of Ethics The Code of Ethics of the National Athletic Trainers' Association has been written to make the membership aware of the principles of ethical behavior that should be followed in the practice of Athletic Training. The primary goal of the Code is the assurance of high quality health care. The principles cannot be expected to cover all specific situations that may be encountered by the practicing Athletic Trainer, but should be considered representative of the spirit with which Athletic Trainers should make decisions. Whenever there is a conflict between the Code and legality, the laws prevail. The NATA Code of Ethics is a minimal standard for students enrolled in the Lewis University Athletic Training Education Program. Violations will result in department disciplinary action ranging from short-term suspension to Program expulsion. A copy of the NATA Code of Ethics can be found in Appendix C. Incident Reports Incident reports will be filed for any violation of the policies in this manual or policies of the clinical site to which the student has been assigned. Once the Program Director receives the Incident Report it is the students responsibility to meet with the Program Director prior to returning to the clinical site. Incident reports filed against a student will result in department disciplinary action ranging from short-term suspension to program expulsion. Incident forms can be found in Appendix D. 24 APPENDIX A CLINICAL PROGRESSIONS 25 APPENDIX A PHYSICAL ASSESSMENT OF THE UPPER EXTREMITY LAB NEW PROFICIENCIES TO BE ASSESSED 1. 2. 3. 4. 5. 6. 7. 8. Tape and wrap shoulder, elbow, wrist, hand and fingers OSHA: Control bleeding Clean and protect wound Steristrips Assess vital signs: blood pressure, pulse, respirations, temperature Select and instruct client on ROM exercises Assess weather: Sling psychrometer lightening air quality Check activity setting for hazards: Physicalenvironmental Assess: Weight, Body composition, Weight charts Evaluate and manage heat and cold illnesses Access and recommend nutritional guidelines for fluid replacement 9. Correctly triage emergency situations 10. Take a complete medical history 11. Administer sensory and neurological and circulatory tests 12. Use an otoscope to examine the nose, outer and middle ear 13. Snellen eye chart 14. Select & fit protective equipment: helmet/head gear, shoulder pads, mouth guard, rib brace 15. Construct, apply and remove: padding, donut pad, checkrein, soft cast 16. Exercise to improve neuromuscular control and coordination: 17. Observe and identify clinical signs and symptoms of common injuries 18. Classify body types 19. Recognize postural deviations in the upper extremity, head and neck 20. Clinical signs and symptoms with common injuries 21. Palpate to assess integrity of bony landmarks and soft tissue 22. Use appropriate and professional Communication 26 APPENDIX A PHYSICAL ASSESSMENT OF THE LOWER EXTREMITY LAB NEW PROFICIENCIES TO BE ASSESSED 1. Tape and wrap hip, pelvis, knee, leg, ankle, foot, toes 2. OSHA: Control bleeding Clean and protect wound Steristrips RICE 3. Assess vital signs: blood pressure, pulse, respirations 4. Select and instruct client on ROM exercises 5. Exercise to Improve cardiorespiratory endurance for the lower body: Bike, treadmill, stairclimber 6. Correctly triage emergency situations 7. Take a complete medical history 8. Administer sensory and neurological and circulatory tests 9. Assess: height, limb girth, limb length 10. Exercise to improve neuromuscular control & coordination for the lower body: PNF patterns, incline board, balance activities 11. Select and fit prophylactic protective equipment: footwear, ankle, knee brace 12. Construct, apply and remove: pading, donut pad, checkrein, soft cast 13. Observe and identify clinical signs and symptoms of common injuries 14. Classify body types 15. Recognize postural deviations 16. Palpate to assess integrity of bony landmarks and soft tissue in the lower extremity 17. Use appropriate professional communication. 27 APPENDIX A CLINICAL I CONTINUEING EVALUATION OF LEARNED SKILLS 1. Assess body composition 2. Select and fit protective equipment 3. Tape, wrap, pad and brace 4. Correctly triage emergency situations 5. Evaluate and manage heat and cold illnesses 6. Perform neurologic assessment 7. Obtain a complete medical history 8. Recognize clinical signs and symptoms with common injuries 9. Administer sensory and neurological and circulatory tests 10. Palpate to assess integrity of bony landmarks and soft tissue NEW PROFICIENCIES TO BE ASSESSED 1. Demonstrate proper lifting and spotting techniques 2. Establish a repetition max test 3. Perform and evaluate results of Flexibility tests Strength tests Agility tests Speed tests Upper/lower body strength test Upper/lower body power test Upper/lower body muscular endurance test 4. Perform isometric tests 5. Exercise to improve muscular strength 6. Exercise to improve agility 7. Instruct the following Upper body a. throwing b. catching Lower Body a. Carioca b. cross-over c. figure eight (8) 8. Instruct and perform exercises to improve activity-specific skills. 9. Palpate the four abdominal quadrants. 10. Use commonly used special test to make a differential diagnosis 11. Administer active and passive ROM tests using goniometry 12. Use manual muscle testing techniques 13. Implement an emergency action plan 14. Splint various body segments. 15. Stabilize, spine board and transport an adult or child with a spinal injury 16. Select, fit and instruct : Crutch use Cane Manual conveyance 17. Manage an airway with and without headgear on 18. Perform 1 and 2 person CPR on an adult or child using a bag valve mask 19. Assist a drowning victim 20. Locate the phone # and address of the nearest poison control center 21. Replicate reporting a drug overdose or poisoning situation 22. Replicate using an emergency inhaler to prevent an asthma attack 23. Ability to access and recommend nutritional guidelines for the following: a. weight loss b. weight gain 28 24. 25. 26. 27. 28. 29. 30. 31. 32. Ability to use the nutritional food pyramid. Ability to access and assess the following nutritional intake values: Ability to determine energy expenditure and caloric intake. Ability to calculate the basal metabolic rate of energy expenditure. Explain a potentially catastrophic injury to an injured adult or child, athletic personnel, family Effectively communicate with physicians, EMTS Perform record keeping with sensitivity to confidentiality Develop facility design plans, evacuation, rehab and treatment areas Replicate using an emergency epinephrine injection 29 APPENDIX A CLINICAL II CLINIC SETTING CONTINUING EVALUATION OF LEARNED SKILLS 1. Perform and evaluate the results of the following tests Flexibility tests strength testing Agility tests 2. Select, fit, and instruct patient to use crutches, cane 3. Perform goniometry measurements 4. Exercise to improve agility and cardiorespiratory endurance 5. Demonstrate appropriate communication skills speed tests NEW PROFICIENCIES TO BE ASSESSED 1. Interpret isokinetic test results and determine appropriate follow-up care 2. Use standardized record keeping Insurance documentation Progress notes 3. Determine current inflammatory stage of patient 4. Determine indications, contraindications and precautions to treatment protocols 5. Select the appropriate parameters, prepare and apply Modalities intermittent compression Massage myofascial release techniques traction 6. Exercise to improve ROM 7. Exercise to improve Muscular strength, endurance, speed, power Neuromuscular control 8. Assess joint end point and select and perform appropriate Joint mob techniques 30 APPENDIX A CLINICAL II (cont’d) GENERAL MEDICINE SETTING CONTINUEING EVALUATION OF LEARNED SKILLS 1. 2. 3. 4. Assess vision using Snellen eye chart Assess body temperature: oral tympanic axillary Use an otoscope to examine nose, outer and middle ear Demonstrate appropriate communication skills NEW PROFICIENCIES TO BE ASSESSED 1. Observe and identify clinical signs and symptoms of ear injury and illness jaw, mouth, tooth 2. Use a stethescope to identify normal sounds: breath heart bowel 3. Differential assessments Respiratory conditions Skin Eyes, ears, Nose and Throat Cardiovascular Endocrine Gastrointestinal Eating disorders STDs Genitourinary tract and organs Gynecological Viral 4. Simulate intervention for a person with a substance abuse problem and recommend referral 5. Simulate a confidential conversation with a health care professional regarding suspected abuse 6. Locate available community based resources for psychosocial intervention 7. Use PDR or other drug reference 8. Document/track medications 9. Replicate procedure for administering OTC meds 31 APPENDIX A CLINICAL III CONTINUEING EVALUATION OF LEARNED SKILLS 1. 2. 3. 4. 5. Use PDR or other drug reference Recognize postural deviations and predisposing conditions Assess weather and physical hazards Interpret weight charts Access and assess RDA or equivalency Nutrient intake Energy expenditure & caloric intake 6. Assess limb length 7. Perform isometric tests 8. Perform neurological assessment 9. Use manual muscle testing techniques 10. Differential assessment 11. Select and apply an appropriate splint 12. Stabilize and spine board for suspected spinal injury 13. Transport splinted and spine boarded individual 14. Demonstrate 1 and 2 person CPR using a bag valve mask 15. Document the tracking of medications 16. Replicate procedure for administering OTC medications 17. Replicate epinephrine injection 18. Determine indications, contraindications, and precautions for treatment protocols 19. Select, prepare and apply Modalities myofascial release traction intermittent compression massage 20. Exercise to improve: ROM Muscular endurance, speed, power Neuromuscular control and coordination 21. Instruct joint mobilizations self-mobilizations 22. Assess joint end point and select appropriate joint mobilization techniques 23. Palpate abdomen NEW PROFICIENCIES TO BE ASSESSED 1. Simulate intervention for suspected eating disorder 2. Identify proper referral sources for disordered eating 3. Develop administrative plans Risk management policies and procedures Facility hazards 4. Access and recommend nutritional guidelines for Preparticipation meal weight loss/gain fluid replacement 5. Use standardized record keeping 6. Administer functional and activity specific tests 7. Recognize signs and symptoms and predisposing conditions for the following Genitourinary tract and organs Eating disordersSTDs Gynecological Systemic 8. Simulate motivational techniques during rehab 9. Develop a resume 32 APPENDIX B CLINICAL EXPERIENCE RECORD 33 APPENDIX B ATHLETIC TRAINING EDUCATION PROGRAM CLINICAL EXPERIENCE RECORD Semester/ Year PHYSICAL ASSESSMENT UPPER EXTREMITY LAB PHYSICAL ASSESSMENT LOWER EXTREMITY LAB CLINICAL I Site Clinical Instructor Hours Completed Upper Extremity Lower Extremity High Risk Upper Extremity Lower Extremity High Risk Upper Extremity Lower Extremity High Risk General Medical General Medical CLINICAL II CLINICAL III INTERNSHIP SURGERY OBSERVATION Upper Extremity Lower Extremity High Risk Upper Extremity Lower Extremity High Risk General Medical Other General Medical General Medical ER TOUR AMBULANCE OBSERVATION PHYSICIAN EXTENDER OBSERVATION General Medical General Medical 34 APPENDIX C NATA CODE OF ETHICS 35 APPENDIX C NATA CODE OF ETHICS Principle 1: Members shall respect the rights, welfare and dignity of all individuals. 1.1 Members shall not discriminate against any legally protected class. 1.2 Members shall be committed to providing competent care consistent with both the requirements and the limitations of their profession. 1.3 Members shall preserve the confidentiality of privileged information and shall not release such information to a third party not involved in the patient's care unless the person consents to such release or release is permitted or required by law. Principle 2: Members shall comply with laws & regulations governing the practice of athletic training. 2.1 Members shall comply with applicable local, state, and federal laws and institutional guidelines. 2.2 Members shall be familiar with and adhere to all NATA guidelines & ethical standards. 2.3 Members are encouraged to report illegal or unethical practice pertaining to athletic training to the appropriate person or authority. 2.4 Members shall avoid substance abuse &, when necessary, seek rehabilitation for chemical dependency. Principle 3: Members shall accept responsibility for the exercise of sound judgment. 3.1 Members shall not misrepresent in any manner, either directly or indirectly, their skills, training, professional credentials, identity or services. 3.2 Members shall provide only those services for which they are qualified via education and/or experience and by pertinent legal regulatory process. 3.3 Members shall provide services, make referrals, and seek compensation only for those services that are necessary. Principle 4: Members shall maintain and promote high standards in the provision of services. 4.1 Members shall recognize the need for continuing education and participate in various types of educational activities that enhance their skills and knowledge. 4.2 Members who have the responsibility for employing and evaluating the performance of other staff members shall fulfill such responsibility in a fair, considerate, and equitable manner, on the basis of clearly enunciated criteria. 4.3 Members who have the responsibility for evaluating the performance of employees, supervisees, or students, are encouraged to share evaluations with them and allow them the opportunity to respond to those evaluations. 4.4 Members shall educate those whom they supervise in the practice of athletic training with regard to the Code of Ethics and encourage their adherence to it. 4.5 Whenever possible, members are encouraged to participate and support others in the conduct and communication of research and educational activities that may contribute knowledge for improved patient care, patient or student education, and the growth of athletic training as a profession. 4.6 When members are researchers or educators, they are responsible for maintaining and promoting ethical conduct in research and educational activities. 36 Principle 5: Members shall not engage in any form of conduct that constitutes a conflict of interest or that adversely reflects on the profession. 5.1 The private conduct of the member is a personal matter to the same degree as is any other person's except when such conduct compromises the fulfillment of professional responsibilities. 5.2 Members of the National Athletic Trainers' Association shall not use the Association's name or logo or their affiliation with the Association in the endorsement of products or services. 5.3 Members shall not place financial gain above the welfare of the patient being treated and shall not participate in any arrangement that exploits the patient. 5.4 Members may seek remuneration for their services that is commensurate with their services and in compliance with applicable law. 37 APPENDIX D INCIDENT REPORT FORMS 38 APPENDIX D INCIDENT REPORT Date: _____________________ Facility: _________________________________________ Clinical Instructor _____________________________ Phone Number ______________________ Student: _____________________________________ Date of Incident ____________________ Clinical Instructor's Account of incident: Immediate action taken by Clinical Instructor: Clinical Instructor Signature _______________________________________ Copy of report given to student: Date: _________________ Time: ______________ I acknowledge receiving a copy of this incident report. Athletic Training Student Signature _____________________________ Date _______________ 39 APPENDIX D INCIDENT REPORT FOLLOW-UP PD/Student Meeting Date _______________ # of Incidents Reports this semester __________ Meeting Notes: Action Taken: Program Director Signature _________________________________ Date ______________ Student Signature _________________________________________ Follow-up Notes: 40