Rugged Individualism and the Chronic Patient
advertisement
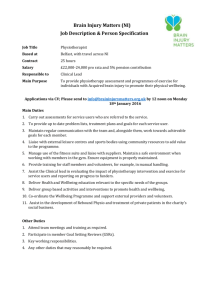
Rugged Individualism and the Chronic Patient By Aaron D. Witsoe & Andrew F. Miller Ph.D. As a general rule, the American public praises a self-made man or woman, and may cite a phrase or two such as, their “up-by-the-bootstraps” style, “sheer determination” or more obscurely their “rugged individualism.” They march to their own drum, and don’t let other distract them. They don’t let social norms get in their way, and their ferocious appetite to make a difference fuels their day to day activity. These descriptors are certainly admirable and many times are quite appropriate. What this paper intends to address is how this type of social propagation (innocent and empowering) impacts those that are less able to just “will their way” to success. I am speaking of the most chronically ill among us; relatives, friends, neighbors and fellow Americans who suffer in their quality of life because of debilitating long-term chronic illness or multiple chronic issues. Pain, discomfort and physical limitations are only a piece of their story, as they more often than not suffer with excruciating social and emotional pain and that can be worse. Rugged Individualism defined First, let’s clarify the term “rugged individualism” as it will be used here. It is not to be confused with Herbert Hoover’s use of the term “rugged individualism” after World War I, which referred to the opinion that government need not interfere into economic issues of citizens, so as to demotivate the ingenuity of the American spirit and its ability to survive in the midst of great strain (rugged individualism). The truth is, during those tough times, there was a lot of social support and common suffering that helped to glue them all together toward a common purpose in each community. They helped a neighbor rebuild a home after the storm. They shared milk with young moms and their children. They helped to parent the children together. They simply helped each other when needed. So even with the rugged individualism came a unifying spirit of social connection that no doubt allowed them to cope with desperate times. Times were different then to be certain. One thing that isn’t different is our need to connect with other people in meaningful ways, not superficial, “country club” ways. When this once powerful trait assisted Americans out of the Depression, it was anchored in the mindset and social makeup of our country for good, which to be clear, was not a bad thing. However, where it has potentially damaged us now is that we have unknowingly forsaken a key part in human flourishing, that of the need for belongingness, connection, interaction, or relationship. Impact on the Chronically Ill There is a negative side to rugged individualism for our chronically ill friends, neighbors and co-workers. It is that there is a pervasive feeling, either consciously or subconsciously, that when I have a problem, I just need to “bare down” and “get this thing under control.” The result for the chronically ill patient trying to cope with life-changing conditions is that they become isolated rather quickly. It doesn’t take a rocket scientist to know what happens when folks get isolated and on top of it have physical limitations, pain, and a disruption of their life purpose. All of their natural abilities to cope with life are scattered, regardless of their past experiences of success and social competence. (cite study?) The statistics are staggering for how many of these suffering family members struggle with the basic soft skills of life after experiencing the onset or continuation of life-altering chronic issues. Usually, isolation, loss of self, depression and self-contempt accompany such situations. So in these cases, rugged individualism does not serve the chronically ill person or their family. Because in fact, they DO need other people to walk alongside, they don’t need a individualistic mindset even if that’s what they are used to. They need others to help them, to inspire, to challenge, to encourage and to share emotions with. But they also need others who can truly understand and empathize with their condition, a fellow traveler or like-minded sufferer. For those who choose to stay on the path of isolationism and not wanting to “burden their loved ones”, there is a dismal outcome both medically and personally. All humans need to know they are contributing to life and those around them, and when that is taken away they suffer tremendously, whether they know why or not. So when a chronic patient is no longer able to contribute to others and feels that it’s only a ONE WAY street in their direction, it feels unnatural and uncomfortable. Left untreated, it morphs into self-contempt and demotivation on all levels. While they need the support, they also need to know they are contributing something into the lives of those around them. This is energizing when it happens, and draining when it doesn’t. All of these wellbeing deficiencies can be exist in any of us at any time if allowed. The chronic patient has a plethora of challenges thrown on them at one time, thoroughly scrambling their wellbeing compass. You can’t fight your way out alone when that happens, and yet we try. We all have known that individual who refuses assistance of any kind and demands to do things on their own. This is a form of rugged individualism. While this can be a great motivator for a driven individual, many times it comes from unresolved irritations within them about their condition and its consequences and a lack of capacity for social contribution. They feel trapped, just like anyone could in their shoes. No matter how grim the outlook, their wellbeing is the answer to improving all of the other areas. Wellbeing works together with medical treatments and medication, improving their effectiveness and reducing overutilization and frustration. What’s being done Many in this population turn to their physician, albeit subconsciously, for this much needed support, understanding and hope. Generally speaking, the doctor has limited training and time to address the wellbeing or emotional needs outside of medical diagnosis, treatment and prescriptions. In fact, if it gets too bad, the doctor may refer folks to a psychiatrist or psychologist, but their job kind of stops there. Thus, the current medical system in the U.S. is not setup to effectively address such a person, at least not with dignity. Yet, this population of chronic sufferers makes up 50% of the country’s total healthcare costs. This is not a judgment statement on the Physician, but a realistic appraisal of how the current medical system actually is structured to handle these challenges. By and large, from the patient’s perspective, education or wellness programs have been the answer to helping them to manage their life better, outside of the medical treatments, physical therapy and medications. There are some new concepts with regard to personal coaches and transition coaches that can also have an impact. With regard to wellness, the truth is that if someone could get these chronic patients to make better choices with their diet and exercise or smoking, it is proven to reduce costs and improve the patient’s quality of life. So why don’t these patients just do that and change their future? What is not being formally addressed is the capacity, or lack of capacity, of these chronic patients to actually follow through and take action on these habit changes. In fact, many of them are not capable for a variety of reasons, but certainly not because they are incapable human beings. Medications play a role, along with social isolation, physical and mental energy, lack of motivation and loss of self. They have lost their sense of “being”, like a sock in the washer, tumbling about trying to find which way is up. Many of these things may not have existed in the individual before the onset of a chronic issue. Almost any human being that endures a life-altering chronic condition will have reactions such as these, and it multiplies when there are more than 3 conditions simultaneously. So, in other words, no matter how good the wellness program or educational conduit, there will likely be little or no change in the actual results of these patients. This is because the filter through which they receive information is not able to appropriate the data into a decision, due to the complex nature of their multiple comorbidities. This is why the wellness movement over the past decade has had little impact on the overall population and the status of the average American’s wellbeing and health. We continue to grow in obesity, drug intake, mental services etc. in this top 5%. Not because the information of wellness is wrong, but because information and knowledge is not enough. Addressing the filter (within our mind/body) through wellbeing enhancement changes the outcomes of engagement and in decision-making leading to long-term, sustainable results. This top 5% group is a huge expense ($1.25 Trillion annually in the U.S.) and is therefore getting a lot of attention by healthcare organizations and new ideas. One of those ideas has been gamification online or via mobile, rewarding behavior and making someone forget they are “changing behavior” cause they are having fun. This will no doubt have some effect on the remaining 95%, however, there is still an unmet need of belongingness and relationship desperately needed by this 5% population of chronic sufferers. The human psyche is not made to operate alone, physically and relationally. We need to face-to-face interaction of others, a fact largely researched by social scientists. So now what? Just short of completely restructuring the medical system to address this in the physician’s office, which is not likely to happen soon, we need to find a way to connect these fellow suffering Americans with a means of social interaction, like-minded support, real tools and a proper wellbeing perspective on their condition. This can be done within the current structure by incorporating services of wellbeing within the disease management and care management departments. By connecting these patients and facilitating interaction between them, including their ability to be empowered with their health, we actually improve their outcomes. The Physician is the expert in medical training, but the individual needs to be an expert on themselves. It will take collaboration of well-empowered patients and their Doctors to optimize their medical treatment and personal quality of life, which are both drivers of lower costs and better health. The “rugged individualism” mindset will drive them back into their holes of isolation, depression, demotivation and loss of self. It’s important to note that the pride of the human spirit will always mask this need for help in our culture, and that makes it easy to play into a “victim” mentality, allowing my condition to run my life instead me running my life within the confines of my condition. Being aware of this potential is helpful for those who are facing new conditions for the first time. Helping them accept their condition, and seeing it not as a loss of who they are, is crucial. There are many stories of those who have used their rugged individualism to start the process of coping, but almost always find the strength of others to be the pivotal point of them thriving in the midst of their condition or set of conditions. We are moved by these stories because we are inspired by the force within us that gets stimulated when we connect with others, wrestle with a challenge and then ultimately triumph. That ability to thrive and stimulate our natural vigor is within all of us. Some of us just need a reminder it’s there and someone to remind us as we are rediscovering it. Wellbeing is Natural (WIN) addresses many more topics like this in its research and real-world solutions for the chronically ill. Located in Scottsdale, AZ, Wellbeing is Natural believes that wellbeing is essential to health, and that the industry studies validate it. Its programs are delivered through health organizations and large employers. They are experiential and scientifically-based wellbeing meetings, including education, peer interaction, mindfulness practices, pain reduction techniques, and more. Clinically-tested WIN programs have been researched and developed by Andrew F. Miller, PH.D.