Audio-Digest® GASTROENTEROLOGY - Audio
advertisement

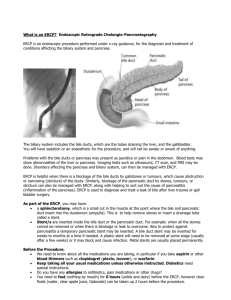
Audio-Digest GASTROENTEROLOGY ® Volume 28, Issue 16 August 21, 2014 SURGICAL CONSIDERATIONS FOR PATIENTS WITH LIVER DISEASE Highlights from the 8th Annual Advanced Liver Disease and Liver Transplantation Update, sponsored by the University of Michigan Transplant Center Pancreaticobiliary Endoscopy in Patients with Liver Disease B. Joseph Elmunzer, MD, Assistant Professor, Department of Internal Medicine, University of Michigan Medical School, Ann Arbor Endoscopic Retrograde Cholangiopancreatography (ERCP) Preprocedural considerations: sedation — ERCPs now generally performed with support of anesthesiologist; those still using conscious sedation or endoscopist-assisted propofol should be aware that metabolism of fentanyl and propofol not affected by liver disease; midazolam (Versed) preferred benzodiazepine in liver disease, except in patients on triple therapy (metabolism of drug slowed); antibiotics — because contrast catheter usually contaminated, administration recommended for all patients in whom contrast delivered and any segment of bile duct not subsequently drained (due to presence of strictures in medium-sized bile ducts secondary to, eg, primary sclerosing cholangitis [PSC], IgG4 cholangiopathy, presence of hilar cholangiocarcinoma in which one or both sides of liver opacified); starting antibiotics empirically in all patients with liver transplantation (LT) before ERCP remains controversial (supported by large study showing that LT independent predictor for systemic infection after ERCP); ascites — not relevant if ERCP performed in left lateral decubitus or supine position; prone position difficult in patient with massive ascites and uncomfortable in ERCP with conscious sedation; preprocedural paracentesis reasonable for patient with large-volume ascites Coagulopathy: presence and how to address preprocedurally most important considerations in patients with liver disease; American Society for Gastrointestinal Endoscopy (ASGE) separates endoscopies into low- and high-risk procedures; ERCP with low bleeding risk — diagnostic only (cholangiography); performed for stent placement or with extraction of stone through preexisting sphincterotomy; no specific adjustment or correction of coagulopathies recommended; ERCP with high bleeding risk — procedures with biliary sphincterotomy or dilation of intraductal stricture; recommendation states that platelets should be >50,000/μL; International Normalized Ratio (INR) not reliable predictor of bleeding in patients with advanced liver disease; speaker attempts to decrease INR to ≤1.5 before ERCP with high bleeding risk, but would not delay urgent procedure to do so; no data support use of novel prothrombotic agents (eg, recombinant factor VIIa) before ERCP; in patient with choledocholithiasis and coagulopathy, consider balloon dilation instead of biliary Educational Objectives The goals of this program are to improve the management of liver disease and the outcomes of liver transplantation. After hearing and assimilating this program, the clinician will be better able to: 1. Recognize the indications for administration of antibiotics before endoscopic retrograde cholangiopancreatography (ERCP). 2. Manage coagulopathy in patients who require ERCP. 3. Recommend appropriate testing for the diagnosis of primary sclerosing cholangitis. 4. Use morphometric measures of frailty to predict outcomes of liver transplantation. sphincterotomy to extract stone; balloon dilation has lower risk for bleeding, but has higher risk for post-ERCP pancreatitis Choledocholithiasis and Biliary Pancreatitis Spontaneous passage of stone: occurs in >80% of cases ASGE guidelines: noncirrhotic patients — perform preoperative risk stratification based on clinical, laboratory, and radiographic parameters to determine likelihood of ongoing choledocholithiasis; ERCP not indicated in patients at intermediate risk for ongoing choledocholithiasis, but should be performed for extraction of stone in high-risk patients; for intermediate-risk patient (eg, with improving pain and decreasing liver function tests [LFTs]), perform endoscopic ultrasonography (EUS) or magnetic resonance cholangiopancreatography (MRCP) to definitively exclude bile duct stone (ie, clear duct), and follow up with cholecystectomy to prevent recurrence of gallstone pancreatitis or choledocholithiasis and cholangitis; EUS and MRCP more accurate than cholangiography for bile duct stones, with none of risks associated with ERCP; cirrhotic patients — not candidates for cholecystectomy due to risk for decompensation or portal hypertension; clearing duct does not prevent recurrence in future; ERCP, extraction of stone, and performance of biliary sphincterotomy recommended to prevent recurrence of choledocholithiasis and biliary pancreatitis Sphincterotomy: prevents recurrence by expanding biliary orifice (so stones can easily pass through); also separates biliary orifice from pancreatic orifice, and bile duct from pancreatic duct, thus eliminating common channel (ie, mechanism of gallstone pancreatitis is obstruction of common channel by stone in bile duct); retrospective cohort study — looked at patients admitted to hospital for gallstone pancreatitis; found that in patients discharged without definitive treatment (ie, no cholecystectomy or endoscopic sphincterotomy), risk for recurrence ≈13%; with cholecystectomy, risk <2%; with endoscopic sphincterotomy, risk 5%; outcomes influenced by adequacy or completeness of sphincterotomy; other data — suggest that risk for recurrent gallstone pancreatitis after endoscopic sphincterotomy 0% to 5% (closer to 1%-2% with complete sphincterotomy); viable option in patients with problems related to stones in bile duct who cannot undergo cholecystectomy (usually those with advanced liver disease) Recurrent symptomatic gallstones and acute cholecystitis: common in patients with gallstones who cannot undergo cholecystectomy (mechanism is obstruction of cystic duct by stone); if obstruction transient and stone spontaneously dislodges, symptoms improve (biliary-type colic); if stone 5. Empower patients awaiting liver transplantation to improve their health and chances for good outcomes. Faculty Disclosure In adherence to ACCME Standards for Commercial Support, Audio-Digest requires all faculty and members of the planning committee to disclose relevant financial relationships within the past 12 months that might create any personal conflicts of interest. Any identified conflicts were resolved to ensure that this educational activity promotes quality in health care and not a proprietary business or commercial interest. For this program, members of the faculty and planning committee reported nothing to disclose. In his lecture, Dr. Elmunzer presents information that is related to the off-label or investigational use of a therapy, product, or device. AUDIO-DIGEST GASTROENTEROLOGY 28:16 impacted, pressure within gallbladder increases and gallbladder wall becomes inflamed (acute cholecystitis) Placement of thin-caliber gallbladder stent: endoscopic approach for patients unable to undergo cholecystectomy due to Child-Pugh class C cirrhosis; stent runs through cystic duct, with one pigtail in gallbladder and another in duodenum; occludes after 2 wk, but prevents stones from completely obstructing duct by occupying space within cystic duct; technical success rate high; highly clinically effective; originally developed as bridge to LT in patients with cirrhosis; unlike bile duct stents, routine replacement unnecessary; if difficulty encountered in inserting wire selectively into gallbladder, introduce scope directly into bile duct (cholangioscopy) and directly visualize bifurcation of bile duct, then explore bile duct endoscopically to find opening of cystic duct; under direct visualization, wire advanced selectively into cystic take-off; rendezvous procedure — recommended for selective cannulation of cystic duct (with help of interventional radiologist) when advancement of wire into gallbladder fails Primary Sclerosing Cholangitis Diagnosis: meta-analysis looked at diagnostic accuracy of MRCP; using ERCP as gold standard, found sensitivity of MRCP ≈86% and specificity 94% (ie, in patient with high pretest probability of having PSC, positive MRCP highly suggestive of diagnosis; in patient with low pretest probability, negative MRCP excludes diagnosis); MRCP found to be diagnostic even in patients with medium probability; based on data, American Association for the Study of Liver Diseases (AASLD) recommended MRCP as first step in diagnosis of PSC; AASLD algorithm — MRCP next step after laboratory evaluation and clinical assessment; ERCP reserved only for situations in which MRCP not helpful; indications for ERCP — diagnosis in question after MRCP; diagnostic certainty has implications in treating other disorders; patient requires therapeutic intervention (in context of new hyperbilirubinemia or new cholestatic LFTs); patient has symptoms suggestive of biliary obstruction; diagnostic sampling of dominant strictures needed Endotherapy: sphincterotomy — main intervention; previously avoided in PSC because of concerns that procedure provides conduit for intestinal bacteria to reach biliary system and cause cholangitis; presently, risk for cholangitis believed to be low; biliary sphincter may be involved in sclerotic process and contribute to symptoms and abnormal LFTs (sphincterotomy beneficial); balloon dilation of dominant strictures — alternative intervention; strictures due to PSC respond to balloon dilation significantly better than do other types of strictures; stents — small ducts common in PSC (require small stents); due to significant amount of sludge produced, stent occlusion and cholangitis common; therefore, stents avoided in PSC, except for refractory strictures (risk for malignancy high); benefits of endotherapy — improves symptoms; based on observational data, appears to improve survival, compared with expectations; benefits must be weighed against risk for complications (rate ≤20%; majority infectious) Other Applications of Endoscopy in Liver Disease Biliary complications: most common type of complication in LT recipients; cause ≤10% to die or require retransplantation; bile leak — occurs in ≤20 of cases; strictures — anastomotic (account for 80% that occur after LT); nonanastomotic (more difficult to treat endoscopically); others — eg, stones or blood clots in duct, sphincter of Oddi dysfunction Diagnostic ERCP: almost never done in patients with low probability of requiring endoscopic intervention because of accuracy and lack of risk associated with EUS and MRCP; in speaker’s institution, threshold for diagnostic ERCP much lower in patients who have had LT Study: compared clinical yield and complications of diagnostic vs therapeutic ERCP; therapeutic ERCP defined as clear evidence on noninvasive testing of indication that would unquestionably justify ERCP in clinical practice (all others considered diagnostic ERCP); outcome measure high-yield cholangiography (defined as ERCP that provided clinically important intervention, found on follow-up to modify disease course); findings — in therapeutic ERCP group, >90% of procedures high-yield cholangiography; >66% of cases in diagnostic ERCP group also high-yield cholangiography; overall complications infrequent; conclusions — diagnostic ERCP reasonable clinical approach in LT recipients with suspected biliary complications, based on high likelihood of high-yield study and low rate of complications; decision to proceed with ERCP in LT recipients should not be taken lightly because of small but real risk for life-threatening complications; in LT recipients, proceeding to ERCP reasonable even if probability of intervention moderate or low; MRCP — appropriate in lower-urgency, lower-probability situations Post-ERCP pancreatitis: infrequently seen in patients with liver disease and those with LT; prevented with prophylactic placement of pancreatic stent or prophylactic rectal indomethacin; speaker’s study of high-risk patients undergoing ERCP found that indomethacin appeared to reduce risk for overall pancreatitis by 50% and moderate to severe pancreatitis by 50%; adverse events same in each group Recognition and Treatment of Frailty Among Candidates for Liver Transplantation Christopher J. Sonnenday, MD, MHS, Associate Professor of Surgery, Surgical Director of Liver Transplantation, University of Michigan Health System, Ann Arbor Liver transplantation: solid organ transplantation faces persistent disparity between supply and demand; average age of patients on waiting lists, and proportion with nonalcoholic fatty liver disease and metabolic syndrome, increasing (patient population “sicker and older”); current method of allocation for LT based on Model for End-stage Liver Disease (MELD) score; among factors in MELD score, creatinine level weighted most strongly; posttransplantation 1-yr survival rate stagnant (85%-90%); need-based system of allocation for LT does not consider difference between predictors of mortality while waiting for LT and those that predict outcome after LT (MELD score poor predictor of posttransplantation survival); speaker advocates allocation based on benefit of receiving LT (ie, potential increase in life expectancy), which would require metrics for prediction (other than age) Frailty: progressive loss of muscle mass (sarcopenia), associated with decreased strength, metabolic rate, activity or walking speed, and energy expenditure, which can result in chronic malnutrition and further muscle loss; Fried metrics — 5 measurable elements, consisting of 3 objective elements (unintentional weight loss, grip strength, and walking speed) and 2 subjective elements (self-reported exhaustion and physical activity); 0 or 1 pt assigned for each element; Cardiovascular Health Study (Fried) — found that high (>3 pt) frailty score associated with increased risk for hospital admissions and falls, and decreased independent living and survival over relatively long periods; also found that frailty score remains fairly consistent over time Study of frailty in chronic liver disease: found that frailty relatively uncommon in patients seen in hepatology clinics, including those with well-compensated cirrhosis; however, differences in frailty measureable among patients being considered for LT (frailty scores found to follow normal distribution in this population [appropriate as diagnostic test or tool for risk stratification]); highly frail patients not necessarily older or have more severe liver disease; highly frail patients have higher rates of depression and reported decreased quality of life; MELD score and frailty weakly correlated; frailty distinct from other factors used to risk-stratify patients for AUDIO-DIGEST GASTROENTEROLOGY 28:16 LT; high MELD score plus high frailty score predicts poor survival (may identify patients for whom LT futile) Frailty and outcomes of LT: highly frail patients had longer hospital stays, higher rates of biliary complications and renal failure, higher rate of discharge to skilled nursing facilities, and higher readmission rates after LT; 1-yr mortality rates similar in patients with low vs high frailty scores; higher rates of reoperation seen in highly frail patients Morphometric measures of frailty: computed tomography can be used to measure physical characteristics of patients and to create volume measures of particular structures (eg, psoas muscle); 1-yr survival after LT linearly related to psoas area; distribution of subcutaneous vs visceral fat (described in other studies as marker of health) and vascular calcification additional morphometric measures; speaker measured these characteristics in control group to calculate morphometric age; in LT recipients, morphometric age did not show direct relationship with chronologic age; survival of those chronologically oldest in age, not significantly different from those younger in age; morphometrically older age found to be predictive of poor outcomes; when outcomes followed in patients in middle of age group (ie, 50 yr); survival found to be significantly reduced in those whose morphometric age increased, while those whose morphometric age decreased had excellent 1-yr survival; conclusion — frailty may predict wait list and LT outcomes better than does severity of liver disease “Prehabilitation” for LT: includes nutritional assessment, exercise instruction, incentive spirometry, tobacco cessation resources, and stress relief and relaxation techniques; aimed at potentially preventing or improving frailty and other factors that drive adverse outcomes after LT; takes advantage of waiting time for LT; empowers patients to take control of own health Acknowledgements Drs. Elmunzer and Sonnenday were recorded at the 8th Annual Advanced Liver Disease and Liver Transplantation Update, held May 3, 2013, in Novi, MI, and sponsored by the University of Michigan Transplant Center. For future CME activities from this sponsor, please visit www.med.umich.edu/intmed/cme/calendar.htm. The Audio-Digest Foundation thanks the speakers and the sponsor for their cooperation in the production of this program. Suggested Reading Cameron ID et al: A multifactorial interdisciplinary intervention reduces frailty in older people: randomized trial. BMC Med, 2013 Mar 11;11:65; De Lisi S et al: Endoscopic ultrasonography versus endoscopic retrograde cholangiopancreatography in acute biliary pancreatitis: a systematic review. Eur J Gastroenterol Hepatol, 2011 May;23(5):367-74; Draganov PV et al: Large size balloon dilation of the ampulla after biliary sphincterotomy can facilitate endoscopic extraction of difficult bile duct stones. J Clin Gastroenterol, 2009 Sep;43(8):782-6; Horiuchi A et al: Biliary stenting in the management of large or multiple common bile duct stones. Gastrointest Endosc, 2010 Jun;71(7):1200-1203.e2; Iorgulescu A et al: Post-ERCP acute pancreatitis and its risk factors. J Med Life, 2013 Mar 15;6(1):109-13; Iqbal J et al: Frailty assessment in elderly people. Lancet, 2013 Jun 8;381(9882):1985-6; Kawaguchi Y et al: Randomized controlled trial of pancreatic stenting Accreditation: The Audio-Digest Foundation is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians. Designation: The Audio-Digest Foundation designates this enduring material for a maximum of 2 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity. The American Academy of Physician Assistants (AAPA) accepts certificates of participation for educational activities designated for A AMA PRA Category 1 Credit™ from organizations accredited by ACCME or a recognized state medical society. Physician assistants may receive a maximum of 2 AAPA Category 1 CME credits for each Audio-Digest activity completed successfully. Audio-Digest Foundation is accredited as a provider of continuing nursing education by the American Nurses Credentialing Center’s (ANCC’s) Commission on Accreditation. Audio-Digest designates each activity for 2.0 CE contact hours. Audio-Digest Foundation is approved as a provider of nurse practitioner continuing education by the American Academy of Nurse Practitioners to prevent pancreatitis after endoscopic retrograde cholangiopancreatography. World J Gastroenterol, 2012 Apr 14;18(14):163541; Khandelwal D et al: Frailty is associated with longer hospital stay and increased mortality in hospitalized older patients. J Nutr Health Aging, 2012 Aug;16(8):732-5; Lynn AP et al: Endoscopic retrograde cholangiopancreatography in the treatment of intraoperatively demonstrated choledocholithiasis. Ann R Coll Surg Engl, 2014 Jan;96(1):45-8; Peterlejtner T et al: Endoscopic treatment of the choledocholithiasis — effectiveness, safety and limitations of the method. Pol Przegl Chir, 2012 Jul;84(7):333-40; Swahn F et al: Rendezvous cannulation technique reduces post-ERCP pancreatitis: a prospective nationwide study of 12,718 ERCP procedures. Am J Gastroenterol, 2013 Apr;108(4):552-9; Theou O et al: Operationalization of frailty using eight commonly used scales and comparison of their ability to predict all-cause mortality. J Am Geriatr Soc, 2013 Sep;61(9):1537-51. (AANP Approved Provider number 030904). Audio-Digest designates each activity for 2.0 CE contact hours, including 0.5 pharmacology CE contact hours. The California State Board of Registered Nursing (CA BRN) accepts courses provided for AMA PRA Category 1 Credit™ as meeting the continuing education requirements for license renewal. Expiration: This CME activity qualifies for AMA PRA Category 1 Credit™ for 3 years from the date of publication. Cultural and linguistic resources: In compliance with California Assembly Bill 1195, Audio-Digest Foundation offers selected cultural and linguistic resources on its website. Please visit this site: www.audiodigest .org/CLCresources. Estimated time to complete the educational process: Review Educational Objectives on page 1 Take pretest Listen to audio program Review written summary and suggested readings Take posttest 5 minutes 10 minutes 60 minutes 35 minutes 10 minutes AUDIO-DIGEST GASTROENTEROLOGY 28:16 SURGICAL CONSIDERATIONS FOR PATIENTS WITH LIVER DISEASE To test online, go to www.audiodigest.org and sign in to online services. To submit a test form by mail or fax, complete Pretest section before listening and Posttest section after listening. 1. Antibiotics are required before endoscopic retrograde cholangiopancreatography (ERCP) in patients with: (A) Primary sclerosing cholangitis (PSC) (B) IgG4 cholangiopathy (C) Hilar cholangiocarcinoma when one or both sides of liver opacified (D) All the above** 2. ERCP is associated with high risk for bleeding when it is performed with which of the following? 1. 2. 3. 4. Stent placement Biliary sphincterotomy Extraction of stone through preexisting sphincterotomy Dilation of intraductal stricture (A) 1,3 (B) 2,4** (C) 1,2,3 (D) 2,3,4 3. International Normalized Ratio (INR) is a reliable predictor of bleeding in patients with advanced liver disease. (A) True (B) False** 4. According to an algorithm for diagnosing PSC from the American Association for the Study of Liver Diseases, which of the following is the next step after laboratory evaluation and clinical assessment? (A) Endoscopic ultrasonography (B) ERCP (C) Magnetic resonance cholangiopancreatography** (D) Computed tomography 5. Bile leaks occur in _______ of patients who receive liver transplantation (LT). _______ strictures are more difficult to treat endoscopically. (A) ≤20; anastomotic (C) ≤5; anastomotic (B) ≤20; nonanastomotic ** (D) ≤5; nonanastomotic 6. Which of the following factors in the Model for End-stage Liver Disease (MELD) score is most strongly weighted? (A) INR (B) Bilirubin (C) Creatinine** (D) Albumin 7. The MELD score is an excellent predictor of posttransplantation survival. (A) True (B) False** 8. All the following statements about frailty among patients with liver disease are true, except: (A) Highly frail patients are usually older and have more severe disease** (B) Highly frail patients have higher rates of depression and report decreased quality of life (C) There is a weak relationship between frailty and MELD score (D) High MELD score plus high frailty score predicts poor survival after LT 9. In LT recipients, morphometric age _______ directly related to chronologic age; survival was found to be _______ by a decrease in morphometric age over time. (A) Is; unaffected (C) Is; improved (B) Is not; unaffected (D) Is not; improved ** 10. Choose the incorrect statement about “prehabilitation” for LT candidates. (A) Aimed at preventing or improving frailty and other factors that drive adverse outcomes after LT (B) Takes advantage of patient’s waiting time for LT (C) Empowers patients to take control of own health (D) Refusal to participate used as grounds for denial of LT ** Answers to Audio-Digest Gastroenterology Volume 28, Issue 15: 1-B, 2-C, 3-D, 4-D, 5-A, 6-A, 7-C, 8-A, 9-D, 10-B ⒸⓅ 2014 Audio-Digest Foundation • ISSN 0892-9386 • www.audiodigest.org Toll-Free Service Within the U.S. and Canada: 1-800-423-2308 • Service Outside the U.S. and Canada: 1-818-240-7500 Remarks represent viewpoints of the speakers, not necessarily those of the Audio-Digest Foundation.