Case study 42 Managing COPD exacerbations
advertisement
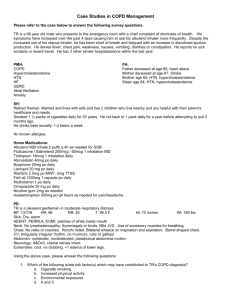
Results Case study 42: Managing COPD exacerbations June 2006 NPS is an independent, non-profit organisation for Quality Use of Medicines funded by the Australian Government Department of Health and Ageing. ABN 61 082 034 393 | Level 7/418A Elizabeth Street Surry Hills 2010 | PO Box 1147 Strawberry Hills 2012 Phone: 02 8217 8700 | Fax: 02 9211 7578 | email: info@nps.org.au | web: www.nps.org.au NPSCS0348 Inside Case study 42: Managing COPD exacerbations Scenario and questions page 3 Summary of results page 5 Results in detail page 6 Commentaries Dr Julia Walters page 14 Associate Professor Christine McDonald page 16 Appendix page 18 References page 19 The information contained in this material is derived from a critical analysis of a wide range of authoritative evidence. Any treatment decision based on this information should be made in the context of the clinical circumstances of each patient. 2 Case study 42 Managing COPD exacerbations Scenario Cedric, a 50-year-old man, was diagnosed with COPD 5 years ago. He presents with worsening dyspnoea, cough and increasing purulent sputum production over the past 3 days. On examination, BP is 130/84 mmHg, pulse 102, respiratory rate 18 and temperature 37.8 ºC. Auscultation of the chest reveals widespread expiratory wheeze and inspiratory coarse crackles in the left lung base. He is dyspnoeic but able to speak in whole sentences. No cyanosis is present. Last spirometry results (8 months ago, after his last COPD exacerbation) were: post-bronchodilator FEV1 55% predicted and FEV1/FVC ratio 65%. Cedric previously smoked 25 cigarettes per day (for 30 years) but cut down to 10 cigarettes per day after his first COPD exacerbation 2 years ago. He has attempted to quit smoking on several occasions without any success. Cedric’s regular medications for COPD are tiotropium (Spiriva) 18 micrograms once daily and salbutamol (Airomir, Asmol, Ventolin) metered-dose inhaler 200 micrograms every 4–6 hours when required. He is also taking indapamide (Dapa-Tabs, Natrilix) 2.5 mg and atorvastatin (Lipitor) 10 mg (both in the morning) for hypertension and hypercholesterolaemia, respectively. He has no other medical conditions, and has no known allergies. 1. What drug therapy would you use for the exacerbation? tiotropium Cease Continue without change Change to: o Dose o o Route o o Frequency o __________________________________________________________________________ salbutamol Cease Continue without change Change to: o Dose o o Route o o Frequency o ________________________________________________________________________ any other medications for this exacerbation: (please specify) ooooooDrugoooooo o Dose o o Route o o Frequency o o Duration o i. _________________________________________________________________________________ ii. _________________________________________________________________________________ iii. _________________________________________________________________________________ iv. _________________________________________________________________________________ Please give reasons why you did OR did not prescribe an antibiotic: ___________________________________________________________________________________ ___________________________________________________________________________________ 3 2. What would you prescribe for stable COPD management after this exacerbation? ooooooDrugoooooo o Dose o o Route o o Frequency o o Duration o i. __________________________________________________________________________________ ii. __________________________________________________________________________________ iii. _________________________________________________________________________________ iv. _________________________________________________________________________________ 3. What else (if anything) would you include in the management plan? During this exacerbation: ______________________________________________________________ In stable disease: _____________________________________________________________________ 4. What strategies would you implement to help him quit smoking? i. __________________________________________________________________________________ ii. __________________________________________________________________________________ iii. _________________________________________________________________________________ 4 Summary of results At the time of publication, 1219 responses had been received from doctors and other health professionals. Responses from 200* general practitioners have been compiled for feedback. Case synopsis A patient with COPD presents with worsening dyspnoea, cough and increasing purulent sputum production over the past 3 days. His current medications for COPD are tiotropium and salbutamol. (See page 3 for more details.) Drug therapy Acute exacerbation • 98.5% of participants would continue tiotropium. • 98.5% would continue salbutamol but 71.5% would change the method of delivery from metereddose inhaler (MDI) to MDI with spacer or nebuliser, and/or increase the dosage. • 80% would prescribe an oral steroid, most commonly prednisolone or prednisone 50 mg daily for 1–2 weeks. • 98% would prescribe one or more antibiotics, mostly amoxycillin (69.9%) or doxycyline (14.8%), and usually for 1–2 weeks. Stable disease (n = 121) • 98.3% and 70.2% would continue prescribing tiotropium and salbutamol, respectively. • 46.3% would add a long-acting beta2 agonist, either as a single product (15.7%) or in combination with an inhaled corticosteroid (30.6%). When prescribed as a single-ingredient product, about half would review the medication after 4–8 weeks, but when prescribed as a combination product, most would continue it indefinitely. • 50.4% added an inhaled corticosteroid, either as a single product (19.8%) or in combination with a long-acting beta2 agonist (30.6%). When prescribed as a single-ingredient product, most would review the medication after 4–8 weeks, but when prescribed as a combination product, most would continue it indefinitely. Other aspects in management of COPD Acute exacerbation • Other management included advice to stop smoking (49.7%), physiotherapy (18.8%), return for follow-up (14.4%) and considering other drug therapy (14.3%). Stable disease • Other management included advice and assistance with smoking cessation (61.1%), reassessing lung function (16.7%), reviewing and optimising therapy (14.4%), respiratory rehabilitation (13.3%) and ensuring currency of vaccinations (12.8%). Strategies for smoking cessation • Non-pharmacological strategies include brief counselling and/or encouragement (56.8%); referral to Quitline (44.7%); and support, follow-up and/or review (30.7%). • Pharmacological strategies included consideration of nicotine replacement therapy (52.3%) and/or bupropion (34.1%), or a general discussion about available therapies (24.1%). * Unless otherwise specified, all percentages cited in this report are based on n = 200. 5 Results in detail Drug therapy for COPD exacerbation Bronchodilator • 98.5% of participants would continue tiotropium. • 2% would also prescribe ipratropium — in one case, instead of tiotropium. • 98.5% would continue salbutamol but 71.5% would change the method of delivery (originally MDI) and/or increase the dosage (originally 200 micrograms every 4–6 hours when required): — 34% recommended using the MDI via a spacer, 9% with a nebuliser, and 3.5% with either — 28.5% increased the dose (up to 400 micrograms without a spacer, 1200 micrograms with a spacer, or 5 mg through a nebuliser) and 69.5% increased the frequency (up to every 1–2 hours) • 2% would also prescribe salmeterol (in addition to salbutamol). Oral steroid • 80% would prescribe an oral steroid (prednisolone or prednisone in all cases except one). • The most commonly prescribed dose was 50 mg daily (range 10–75 mg) mainly for 1–2 weeks (range 3 days – unspecified); 16.5% advocated a dosage reduction schedule. Inhaled corticosteroid • 4.5% would prescribe an inhaled corticosteroid (1.5% in conjunction with an oral steroid). • 6.5% would prescribe combined inhaled corticosteroid plus a long-acting beta2 agonist (3.5% in conjunction with an oral steroid). Antibiotic • 98% would prescribe one or more antibiotics, mainly for about 1–2 weeks (Table 1). • Most respondents based their decision to prescribe an antibiotic on the presence of one or more of the following signs and symptoms: fever (62.5%), increased sputum purulence (59.5%), local lung signs (39%), increased dyspnoea (20%), increased sputum volume (13%), increased cough (7%), tachycardia (6.5%), increased respiratory rate (1.0%), and tachypnoea (1.0%). • As recommended in the COPD-X guidelines,1 26% of respondents listed increased sputum purulence plus increased sputum volume and/or increased dyspnoea as the reason for prescribing an antibiotic. • Other reasons for prescribing an antibiotic included a presentation consistent with acute infective exacerbation of COPD, suspected pneumonia, and to prevent hospitalisation. Other medications • Other medications prescribed during the exacerbation included senega and ammonia mixture APF (1%) and theophylline (0.5%). 6 Table 1. Antibiotic therapy during exacerbation Amoxycillin 500 mg every 8 hours 1000 mg every 12 hours Other (e.g. 250 mg every 8 hours, 500 mg every 6 hours) Doxycycline 100 mg once daily (in some cases 200 mg on the first day) 100 mg twice daily 50 mg once daily Amoxycillin / clavulanic acid 875/125 mg twice daily Other (500/125 mg twice daily or not specified) Amoxycillin and roxithromycin Roxithromycin (150 mg twice daily or 300 mg once daily) Cephalexin (250 mg every 6 hours or 500 mg every 8 hours) Procaine penicillin and amoxycillin Procaine penicillin, amoxycillin and roxithromycin % of respondents (n = 196) 69.9 55.1 10.2 4.6 14.8 13.3 1.0 0.5 8.7 6.1 2.6 2.6 2.0 1.0 0.5 0.5 Practice points • During acute exacerbations of COPD, increase the use of short-acting bronchodilators. • An MDI with a spacer is as effective as a nebuliser if an adequate dose is taken, and is cheaper and more portable.1, 2 Nebulisers should be reserved for patients who are unable to use MDIs (with or without spacer).2 The dose via a spacer that is considered equivalent to a 5 mg salbutamol nebule varies from 8–15 puffs of a 100 microgram salbutamol MDI.1,3 • Consider oral prednisolone 30–50 mg daily for 7–14 days (short courses less than 14 days do not usually require tapering).1,2,4 • Consider antibiotic therapy if increased sputum purulence is present with increased sputum volume and/or dyspnoea.1 The goal of therapy is to reduce volume and purulence of sputum; elimination of colonising organisms is not required.2 The presence of fever is not necessarily indicative of a bacterial infection.2 • Amoxycillin (500 mg every 8 hours for 5 days) or doxycycline (100 mg twice daily for 5 days) is recommended as first-line therapy;2 other antibiotics have not been shown to be superior and are not recommended unless patients do not respond, or resistant organisms are suspected.1,2 • Amoxycillin 1000 mg twice daily is currently not recommended by Therapeutic Guidelines for acute exacerbations of COPD.2 — In a study of 395 patients with acute exacerbation of chronic bronchitis, amoxycillin 1000 mg twice daily offered no additional benefits (in efficacy or safety) compared with amoxycillin 500 mg every 8 hours.5 When compared with the current guidelines for antibiotic therapy in COPD exacerbations, the study also used a longer duration of therapy and placed less emphasis on increased sputum purulence as one of the criteria for antibiotic therapy. • If pneumonia is suspected, investigate and treat as for community-acquired pneumonia: — assessment should include history and examination, chest X-ray, measurement of arterial blood oxygen saturation, investigations for the causal pathogen, and Pneumonia Severity Index class.2 7 Drug therapy for stable COPD Table 2 summarises the medication regimens that respondents would use for stable COPD management. Table 2. Drug therapy for stable COPD management % of respondents (n = 121*) Tiotropium and salbutamol (existing treatment) 28.1 Tiotropium, salbutamol, long-acting beta2 agonist and inhaled corticosteroid 22.3 Tiotropium, salbutamol and inhaled corticosteroid 12.4 Tiotropium, long-acting beta2 agonist and inhaled corticosteroid 11.6 Tiotropium only 7.4 Tiotropium, salbutamol and long-acting beta2 agonist 5.8 Tiotropium and long-acting beta2 agonist 5.8 Tiotropium and inhaled corticosteroid 3.3 Miscellaneous 3.3 * Only responses that were clear about whether or not tiotropium and salbutamol were to be continued have been included in the analysis. Bronchodilator (n = 121) • 98.3% and 70.2% of respondents stated that they would continue tiotropium and salbutamol, respectively. • 32.2% and 14.1% would add salmeterol and eformoterol, respectively. Long-acting beta2 agonists were prescribed either on their own (15.7%) or in a combination product (30.6%). When prescribed as a single-ingredient product, about half would review the medication after 4–8 weeks, but when prescribed as a combination product, most would continue it indefinitely. • Other bronchodilators that were prescribed were ipratropium (1.7%) and terbutaline (0.8%). Inhaled corticosteroid (n = 121) • 2.5%, 11.6% and 35.5% prescribed beclomethasone, budesonide and fluticasone, respectively. Inhaled corticosteroids were prescribed either on their own (19.8%) or in a combination product (30.6%). When prescribed as a single-ingredient product, most would review the medication after 4–8 weeks, but when prescribed as a combination product, most would continue it indefinitely. 8 Practice points • To date, the use of long-acting beta2 agonists in conjunction with tiotropium has not been investigated in clinical trials.2 However, these drugs work by different mechanisms, and several guidelines advocate combined bronchodilator therapy for patients who remain symptomatic on monotherapy.1,4,6 — Long-acting beta2 agonists should be stopped and reassessed if there are no changes in symptoms, ability to perform daily activities or exercise capacity after 4 weeks.2,6 • Inhaled corticosteroid should be considered in patients who have documented evidence of responsiveness to inhaled corticosteroids, or who have moderate or severe COPD (FEV1 ≤ 50% predicted) and have 2 or more exacerbations requiring treatment with antibiotics or oral corticosteroids in a 12-month period.1,2,6 — Recommended trial periods for inhaled corticosteroids vary from 6 weeks up to 6 months (depending on the guideline).1,2,7 However, a longer trial may be necessary to assess an impact on exacerbation rates. • There are conflicting findings regarding the efficacy of combined inhaled corticosteroid plus longacting beta2 agonist in a single inhaler, compared with inhaled corticosteroid or long-acting beta2 agonist alone in COPD.8 — The option of using either long-acting beta2 agonist or inhaled corticosteroid alone should be considered first before considering adding both medications to the existing regimen. — While combination products may be more convenient for the patient, when indicated, an initial trial of inhaled corticosteroid and long-acting beta2 agonist in separate inhalers may allow better assessment of the benefits offered by each medication. 9 Other aspects of COPD management During COPD exacerbation • In addition to the drug therapy already listed on page 6, 181 respondents (90.5%) would include in their management plan for COPD exacerbation the measures listed in Table 3. Table 3. Other measures to manage COPD exacerbation % of respondents* (n = 181) Advise to stop smoking 49.7 Recommend physiotherapy/ chest physiotherapy 18.8 Follow-up 14.4 In 24 hours 8.8 In 48 hours 1.7 Not specified 3.9 14.3 Consider other drug therapy Consider oral steroid (if condition worsens) 6.6 Consider other medications (e.g. paracetamol, oral theophylline, mucolytics, long-acting beta2 agonist) 7.7 Consider hospital admission if deteriorating/ no improvement 9.9 Review inhalation device 7.7 Order chest X-ray 6.1 Check inhaler technique 4.4 Consider use of spacer and/or nebuliser 3.3 Assess lung function (using spirometry) 3.3 Miscellaneous (e.g. consider oxygen therapy, action plan, regular peak flow measurements) 20.4 * Respondents may have more than one response During stable COPD • In addition to the drug therapy already listed on page 8, 180 respondents (90%) would include in their management plan for stable COPD the measures listed in Table 4. 10 Table 4. Other measures in stable COPD management % of respondents* (n = 180) Advise/ assist with smoking cessation 61.1 Reassess lung function (via spirometry) 16.7 Review/ optimise drug therapy 14.4 Recommend respiratory rehabilitation 13.3 Ensure currency of influenza and/or pneumococcal vaccination 12.8 Recommend exercise 8.9 Check inhaler technique 7.2 Prepare an action plan 6.7 Assess compliance 3.3 Miscellaneous (e.g. advise the patient to use a peak flow meter, conduct regular reviews, consider referral to a respiratory physician) 16.7 * Respondents may have more than one response Practice points • Pulmonary rehabilitation is considered one of the most effective interventions in COPD and has been shown to improve symptoms and functioning of patients with COPD.1 It should be offered to patients with moderate to severe COPD who are sufficiently motivated and do not have severe co-morbidities which preclude active participation in the program.2 Comprehensive programs encompassing exercise training, patient education and psychosocial support have been shown to have the greatest benefit.1 • Annual influenza vaccination is recommended to reduce the incidence of acute exacerbations of COPD.1,6 • Pneumococcal vaccination is also recommended.1,2 The current schedule for pneumococcal vaccination is as follows:9 — non-Indigenous adults ≥ 65 years, or Aboriginal and Torres Strait Islander adults ≥ 50 years: one dose followed by a single revaccination 5 years later — non-Indigenous adults < 65 years with risk factors (includes pulmonary disease): one dose followed by a single revaccination at 65 years of age or 10 years after the first dose, whichever is later — Aboriginal and Torres Strait Islander adults 15–49 years of age with risk factors (includes pulmonary disease): revaccination 5 years after the first dose, then again at 50 years of age or 10 years after the first revaccination, whichever comes later. • Demonstration and repetition are essential for achieving optimal patient inhaler technique.2 Inhaler technique should be checked regularly to ensure that patients are using their inhalers correctly1,2 and compliance should be assessed. • Patients should be encouraged to take appropriate responsibility in managing their own condition.1 — A COPD action plan may be helpful and is recommended.1,2 It may include medications for stable and acute management, and instructions on how to identify and respond to an acute exacerbation. You can download a template from the Australian Lung Foundation at www.lungnet.com.au/copd/copd_action_plan.html. — Patients at risk of COPD exacerbations should keep a course of antibiotic and corticosteroid tablets at home for use as part of self-management.2 11 Strategies to assist with smoking cessation Table 5. % of respondents* (n = 199) Strategies Non-pharmacological strategies Brief counselling and/or encouragement Refer to Quitline or other resources by the national tobacco campaign Support, follow-up and/or review (at consultations or by telephone) Discuss benefits of smoking cessation and/or risks of continuing to smoke Assess readiness to change Provide education or written material Behavioural therapy Intensive counseling Use 5As (Ask, Advise, Assess, Assist, Arrange) strategy Discuss previous attempts (e.g. what was tried, what did not work) Refer to a smoking-cessation specialist Miscellaneous (e.g. hypnotherapy, exercise program, local smoking-cessation program, referral to a psychologist, setting a quit date) 56.8 44.7 30.7 12.1 5.5 5.5 4.5 4.0 4.0 2.5 2.5 19.1 Pharmacological therapies Discuss and advise about available drug therapy options Nicotine replacement therapy (NRT) Bupropion Bupropion (and intensive counselling)† Bupropion if NRT unsuccessful 24.1 52.3 27.6 6.5 * Respondents may have more than one response † Some respondents listed both NRT and bupropion Practice points • Smoking cessation is the single most important intervention to prevent or slow the progression of COPD.1,4,10 • Brief counselling (3–5 minutes) by a health professional has been shown to be effective4,11 and every smoker should be offered at least this intervention at every visit.1,4 When aware of patient’s previous attempts, it may be helpful to first discuss what worked or did not work in previous attempts. • Bupropion (in conjunction with counselling and support) or nicotine replacement therapy (NRT) doubles the rate of smoking cessation compared with placebo.11,12 There are insufficient data to recommend bupropion in preference to NRT, and vice versa.1,13 • The effectiveness of bupropion has only been studied in conjunction with intensive counselling and support program. Examples of such programs from randomised controlled trials with bupropion include a combination of:14,15 — brief intervention by a trained health professional — weekly assessment (15 minutes individual counseling session looking at motivation, identification of triggers, coping responses, weight management and use of medications) — follow-up assessments and relapse prevention strategies — supported telephone call (e.g. 8 telephone calls of approximately 10 minutes duration for 5 months). 12 • The different forms of NRT have similar effectiveness,11,12 and choice should be based on patient preference, need and tolerance.1 • Other interventions that have been shown to work include:11 — intensive (> 10 minutes) counselling by a health professional — telephone counselling services — group behavioural therapy — follow-up visits to a GP — repeated telephone support by nurses after initial intervention. 13 Dr Julia Walters Research Fellow, Discipline of Medicine University of Tasmania Hobart, Tasmania Commentary 1 Key points exacerbations. The presence of cyanosis, peripheral oedema, acute confusion and severe tachypnoea (in addition to impaired physical functioning and inability to cope at home) probably indicate the need for hospital admission.6 • The only factor known to be effective in preventing progression of COPD is smoking cessation. Intensive assistance, using quit methods with the highest success rates, should be given when COPD is diagnosed in a smoker. • Two or more exacerbations of COPD in one year are associated with more rapid lung function decline. Management of acute exacerbation Cedric’s symptoms of breathlessness were addressed effectively by most respondents, who indicated use of bronchodilators, continuing his inhaled tiotropium (98.5%) and salbutamol (98.5%). However, only 28.5% increased the dose of short-acting beta2 agonist although 69.5% increased the frequency. These agents should be used at a dose high enough to relieve breathlessness; 8 puffs 2–3-hourly may be required. More effective delivery can be ensured from an MDI by using a spacer. They have been shown to be as effective as nebulisers and are more convenient and readily available. Acute exacerbation of COPD Diagnosis This man (at age 50 relatively young compared with most general practice COPD patients) is known by his GP to have COPD. This is in itself relatively unusual, as most people (60–80%) in community surveys who are found to have COPD do not have a previous diagnosis of COPD.16-18 However, Cedric had spirometry recently (8 months ago) and this demonstrated obstruction, with an FEV1/FVC ratio of 65%. With an FEV1 of 55% of the value predicted for his age, Cedric would be classified with moderate COPD by the COPD-X guidelines1, i.e. his FEV1 lies in the range 40–59%. A recently published Cochrane systematic review21 concluded that antibiotic therapy, regardless of antibiotic choice, significantly reduced mortality (relative risk [RR] 0.23, 95% confidence interval [CI] 0.10 to 0.52; with number needed to treat [NNT] of 8, 95% CI 6 to 17) and treatment failure (RR 0.47, 95% CI 0.36 to 0.62; with NNT of 3, 95% CI 3 to 5) in exacerbations in patients who are moderately or severely ill. An appropriate antibiotic was indicated by 85% of respondents. Only 2% would prescribe roxithromycin, and 3.1% chose to give this in addition to amoxycillin — an unnecessary combination in COPD exacerbation without pneumonia that increases the possibility of side effects such as diarrhoea. For 59.5% of respondents the decision to treat with an antibiotic was based on increased sputum purulence. This agrees with the evidence-based recommendations. Fever was cited by 62.5% of respondents although this is an uncommon feature in exacerbations6 and, if found, further investigations would be merited. The presence of focal crackles might indicate you are dealing with pneumonia or lung cancer, and a chest X-ray is indicated. The clinical symptoms Cedric displays are typical of an exacerbation of COPD, defined as a sustained worsening of symptoms from the usual stable state, being acute in onset with worsening dyspnoea, cough, increased sputum production and change in sputum colour.6 Treating in the community The need for immediate treatment was recognised by at least 98% of respondents. This is an important point, as lung function may not recover fully after an exacerbation, and rapid institution of therapy is required. A study of community-managed exacerbations found that in 25% of patients recovery to baseline was not complete after five weeks.19 There is also a significantly increased risk of mortality associated with exacerbations in severe COPD.20 This case study assumes that the GP will manage the exacerbation at home and this is accepted as appropriate for all but the most severe 14 instituted, and it could help to reinforce his efforts to quit smoking. Guidelines recommend considering using oral steroids for managing an exacerbation in the community unless there are significant contraindications. A Cochrane systematic review22 found that there were significantly fewer treatment failures in patients given corticosteroid treatment (odds ratio [OR] 0.48, 95% CI 0.34 to 0.68; with NNT of 9 patients, 95% CI 6 to 14). Most respondents chose to use a conventional-length course (7–14 days) of oral prednisolone or prednisone. Only 16.5% tapered the dose; for a course less than 14 days this is not required. Medication Cedric has now had two exacerbations within one year and is at higher risk of more rapid decline in lung function. He should be given a trial of therapy with inhaled corticosteroids. His response can be assessed by symptoms and FEV1, although for assessment on exacerbation rate the length of treatment needs to be prolonged. Inhaled corticosteroids were given by 50.4% of respondents, with most reviewing efficacy after 4–8 weeks. Combination products with long-acting beta2 agonists were used by 30.6%. Use of these products in stable COPD has preceded full consideration of their efficacy. A Cochrane systematic review8 concluded that, although they led to clinically meaningful differences in quality of life, symptoms and rate of exacerbations compared with placebo, there were conflicting results when the different combination therapies were compared with either inhaled corticosteroids alone or longacting beta2 agonists alone. More data are necessary to draw firmer conclusions about the effects of combination therapy in a single inhaler, and their use is not currently recommended by guidelines. Smoking cessation Advice to stop smoking was the most frequent additional management activity undertaken during the exacerbation (49.7% of respondents). This is important because Cedric still smokes even 5 years after having the diagnosis of COPD, but it was an opportunity missed by more than half the respondents. Even brief advice to stop smoking is valuable and effective23 and is emphasised in all guidelines. Only 61.1% included smoking cessation in measures to manage Cedric’s COPD when he was stable. This should be the highest priority for treatment, as stopping smoking is the most effective intervention to slow progression. Cedric has made previous efforts — so far unsuccessful — in achieving sustained abstinence and is likely to need pharmacological therapy in addition to the counselling and encouragement offered by 56.8% of respondents, as this increases his chances of success. Both bupropion and nicotinereplacement therapy double the rates of cessation compared with placebo; 51.3% proposed using nicotine-replacement therapy and 24.6% bupropion to assist Cedric. Preventing deterioration Ensuring that influenza and pneumococcal vaccination were up to date was noted by 12.8% of respondents. Measures to develop a support network and self-management plan were addressed by some respondents: recommending respiratory rehabilitation (13.3%), recommending exercise (8.9%) and preparing an action plan (6.7%). As well as enhancing physical fitness and quality of life, respiratory rehabilitation aims to foster selfmanagement and emotional coping skills. Completing respiratory rehabilitation and/or having an action plan leads to better recognition of deterioration and more appropriate treatment of exacerbations24,25 but many patients with COPD who would benefit do not have the opportunity, through lack of referral or availability.26 Access will hopefully be improved with the launch of a toolkit this year by the Australian Lung Foundation and Australian Physiotherapy Association to assist health professionals in developing programs more widely throughout Australia.27 Management of stable COPD When reviewing Cedric at follow-up, the principles of COPD-X (optimising function, preventing deterioration, developing selfmanagement strategies) should be followed.1 Spirometry In assessing the longer-term need for therapy after Cedric is stable, only 16.7% would use spirometry to reassess lung function. Spirometry would give the GP an objective measure to assess Cedric’s severity and his response to additional treatment, which most respondents 15 Commentary 2 Associate Professor Christine McDonald Deputy Director, Department of Respiratory and Sleep Medicine Director, Institute for Breathing and Sleep Medicine Austin Hospital Melbourne, Victoria Key points Management of the acute exacerbation • Spirometry is the gold standard for diagnosing and monitoring COPD. Up to 50% of patients with moderate to severe COPD suffer recurrent exacerbations. Early diagnosis and prompt treatment of such exacerbations may prevent functional deterioration and also reduce hospital admissions. Cedric is clearly unwell but should respond to standard therapy. • Smoking cessation and oxygen therapy in patients with COPD who are hypoxaemic are the only treatments known to impact survival in COPD. • Recurrent exacerbations of COPD are associated with a more rapid decline in both lung function and quality of life and may be managed by a range of long-term treatments, including long-acting bronchodilators, corticosteroids and combinations of both. An acute exacerbation requires stepped-up therapy with more frequent and higher-dose bronchodilators, systemic corticosteroids and possibly antibiotics.1 Consistent with this, 71.5% of respondents stated they would change the method of delivery of salbutamol and/or increase the dosage. Metered-dose inhaler plus spacer is as effective as nebuliser as long as the dosage is equivalent, and this may require up to 8–10 or more puffs of 100-microgram salbutamol or equivalent short-acting bronchodilator. Management tools for COPD COPD is defined as ‘a disease state characterised by airflow limitation that is not fully reversible’.4 Spirometry is the gold standard for diagnosing COPD and it is pleasing to note that Cedric has undergone spirometric testing, which has demonstrated that he has moderate COPD (by COPD-X criteria1). Repeat spirometry may be appropriate to monitor progressive decline in lung function, which is faster in patients with COPD who continue to smoke. Eighty per cent of respondents would prescribe oral corticosteroids, most commonly prednisolone 50 mg once daily for 1–2 weeks. This should not require tapering and is associated with more rapid resolution of the exacerbation and a reduced likelihood of relapse.1 It is unclear whether knowledge about the presence of COPD impacts on patients’ success with quitting smoking. One study of patients offered smoking-cessation advice after screening spirometry found that those identified as having moderate to severe COPD were more likely to have successfully quit at 12 months after the intervention than those with normal lung function or only mild airflow obstruction.28 It is important that Cedric stops smoking during the acute attack; indeed, the occurrence of this acute attack is a perfect opportunity to intensify discussion about smoking cessation. About half of the respondents identified advice and other assistance in stopping smoking as being of importance during an acute exacerbation. There are several sets of mostly complementary guidelines to assist in managing a patient with COPD, and these have been drawn on in the practice points and this commentary.1,2,4,6 The Australian COPD-X Guidelines are updated regularly and are available online through the Australian Lung Foundation website at www.lungnet.com.au. Although many acute exacerbations are triggered by viral infections or have no clear infective trigger, bacterial infection may have a primary or secondary role in about 50% of exacerbations. Many patients with COPD are colonised with organisms such as Haemophilus influenzae, Streptococcus pneumoniae or Moraxella catarrhalis. 16 In patients who are at least moderately ill, with clinical signs of infection such as increased volume and purulence of sputum, a Cochrane review confirmed that antibiotics reduce mortality risk and risk of treatment failure.21 Australian Therapeutic Guidelines2 recommend oral amoxycillin or doxycycline for treatment of such an acute exacerbation, unless there is known colonisation with a resistant organism, or the presence of pneumonia. should be used to optimise quit rates for patients with COPD.6 In patients with moderate to severe COPD and recurrent exacerbations, inhaled corticosteroids have been demonstrated both to reduce exacerbation rate and improve quality of life. Long-acting bronchodilator therapy with either inhaled anticholinergics or long-acting beta2 agonists may also have a role in improving quality of life in COPD. The finding of crackles at the left lung base does raise the question of possible pneumonia, as recognised by some respondents. This could be confirmed by chest radiograph, if clinically indicated. Confirmation of pneumonia would prompt treatment for community-acquired pneumonia with standard combination antibiotic therapy. The place of combination therapy with inhaled corticosteroid and long-acting beta2 agonist either used separately or in one inhaler remains unclear, and a recent Cochrane systematic review8 concluded that more data are necessary before firm recommendations can be made. Useful further data should soon be available through publication of the results of the TORCH study.30 This large, randomised controlled study examined combination therapy with fluticasone and salmeterol versus placebo, versus each component alone, with the primary endpoint of mortality and secondary endpoints including exacerbation rate and quality of life. Management of stable COPD Both during and after the acute attack, attention to smoking-cessation strategies is paramount. Smoking cessation has been shown to reduce the accelerated decline in lung function seen in COPD.1 The COPD-X Checklist (available from www.lungnet.com.au) contains the well-known modified Fletcher and Peto graph of decline in FEV1 over time and the positive impact of smoking cessation on this decline. Discussing the graph with patients may be a useful adjunct in addressing this issue. The rate of referral for pulmonary rehabilitation seems rather low at 13.3% of respondents. This could be because of Cedric’s relatively young age and the potential impact a 6-week program may have on his working life. However, it is important to recognise that pulmonary rehabilitation is one of the most effective interventions available in managing COPD, improving both exercise capacity and quality of life as well as impacting on the anxiety and depression commonly associated with the condition.1 If not available locally, the recently released Pulmonary Rehabilitation Toolkit (www.lungnet.com.au) provides practical information about how to set up such a program. The type of smoking-cessation program should be tailored to the patient and may include assessing the degree of nicotine addiction using the Fagerstrom questionnaire (available in Smoking Cessation Guidelines for Australian General Practice29). Unless contraindicated, nicotine replacement therapy and/or bupropion in addition to ongoing support and counselling 17 Appendix Inhaled medications used in COPD Strength Generic name Device Brand names (in micrograms, unless otherwise indicated) Bronchodilators Short-acting beta2 agonists Salbutamol Autohaler Airomir Autohaler 100 MDI Airomir, Asmol CFC-free, Epaq, Ventolin CFC-free 100 Nebuliser Asmol Uni-dose, Butamol, Ventolin Nebules 2.5mg/2.5mL, 5mg/2.5mL Rotahaler Ventolin Rotacaps 200 Nebuliser Bricanyl Respules 5mg/2mL Turbuhaler Bricanyl Turbuhaler 500 Aeroliser Foradile 12 Turbuhaler Oxis Turbuhaler 6, 12 Accuhaler Serevent Accuhaler 50 MDI Serevent 25 MDI Atrovent CFC-Free 21 Nebuliser Aeron, Apoven, Atrovent preparations, Ipratrin, Ipravent 250/mL, 500/mL Handihaler Spiriva 18 MDI Combivent 100/20 Autohaler Qvar Autohaler 50, 100 MDI Qvar 50, 100 Nebuliser Pulmicort Respules 500/2mL,1000/2mL Turbuhaler Pulmicort Turbuhaler 100, 200, 400 Ciclesonide MDI Alvesco 80, 160 Fluticasone Accuhaler Flixotide Accuhaler 100, 250, 500 MDI Flixotide Terbutaline Long-acting beta2 agonists* Eformoterol Salmeterol Anticholinergic bronchodilators Ipratropium Tiotropium Combination bronchodilator † Salbutamol/ipratropium ‡ Corticosteroids Beclomethasone Budesonide 50, 125, 250 ‡ Combination corticosteroid / long-acting beta2 agonists Budesonide/eformoterol Fluticasone/salmeterol Turbuhaler Symbicort Turbuhaler 100/6, 200/6, 400/12 Accuhaler Seretide Accuhaler 100/50, 250/50, 500/50 MDI Seretide 50/25, 125/25, 250/25 * Long-acting beta2 agonists are approved by the Therapeutic Goods Administration for COPD (except for Oxis Turbuhaler) but are not subsidised on the PBS for COPD † Combination bronchodilator is only subsidised for COPD under the Repatriation PBS Inhaled corticosteroids and combination corticosteroid / long-acting beta2 agonists are not approved by the Therapeutic Goods Administration for COPD (except for Seretide) and are not subsidised on the PBS for COPD MDI = metered-dose inhaler ‡ 18 References 1. Australian Lung Foundation and Thoracic Society of Australia and New Zealand. The COPD-X Plan: Australian and New Zealand guidelines for the management of chronic obstructive pulmonary disease. Australian Lung Foundation, 2006. http://www.copdx.org.au/guidelines/documents/COPDX_March31_2006.pdf (accessed 25 May, 2006). 2. Therapeutic Guidelines. Therapeutic Guidelines Respiratory (electronic). Melbourne: Therapeutic Guidelines Limited; 2006. 3. National Asthma Council. Asthma Management Handbook. 5th edn. South Melbourne: National Asthma Council Australia, 2002. 4. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. 2005. http://www.goldcopd.org/Guidelineitem.asp?l1=2&l2=1&intId=989 (accessed 6 December, 2005). 5. Georgopoulos A, Borek M, Ridl M, et al. Randomized, double-blind, double-dummy study comparing the efficacy and safety of amoxycillin 1 g bd with amoxycillin 500 mg tds in the treatment of acute exacerbations of chronic bronchitis. J Antimicrob Chemother 2001;47:67–76. 6. National Institute for Clinical Excellence. Chronic obstructive pulmonary disease: management of chronic obstructive pulmonary disease in adults in primary and secondary care. NICE, 2004. http://www.nice.org.uk/pdf/CG012_niceguideline.pdf (accessed 23 January, 2006). 7. Rossi S, ed. Australian Medicines Handbook. Adelaide: Australian Medicines Handbook Pty Ltd, 2006. 8. Nannini L, Cates C, Lasserson T, et al. Combined corticosteroid and long-acting beta-agonist in one inhaler for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2004;3:Art.No.CD003794:1–78. 9. Australian Technical Advisory Group on Immunisation. Australian Immunisation Handbook. 8th edn. Canberra: Australian Government Department of Health and Ageing, 2003. 10. Australian Institute of Health and Welfare. Chronic respiratory diseases in Australia: their prevalence, consequences and prevention. AIHW, 2005. http://www.aihw.gov.au/publications/phe/crdapcp/crdapcp.pdf (accessed 6 December, 2005). 11. Miller M, Wood L. Smoking cessation interventions: review of evidence and implications for best practice in health care settings. Australian Government Department of Health and Ageing, 2002. http://www.health.gov.au/internet/wcms/publishing.nsf/content/health-pubhlth-publicat-documentsmoking_ces-cnt.htm/$FILE/smoking_ces.pdf (accessed 8 December, 2005). 12. Woolacott NF, Jones L, Forbes CA, et al. The clinical effectiveness and cost-effectiveness of bupropion and nicotine replacement therapy for smoking cessation: a systematic review and economic evaluation. Health Technology Assessment (Winchester, England) 2002;6:1–245. 13. Hughes JR, Stead LF, Lancaster T. Antidepressants for smoking cessation. Cochrane Database Syst Rev 2004;4:Art.No.CD000031.pub2. 14. Jorenby DE, Leischow SJ, Nides MA, et al. A controlled trial of sustained-release bupropion, a nicotine patch, or both for smoking cessation. New Eng J Med 1999;340:685–91. 15. Tashkin D, Kanner R, Bailey W, et al. Smoking cessation in patients with chronic obstructive pulmonary disease: a double-blind, placebo-controlled, randomised trial. Lancet 2001;357:1571–5. 19 16. Mannino DM, Gagnon RC, Petty TL, et al. Obstructive lung disease and low lung function in adults in the United States: data from the National Health and Nutrition Examination Survey, 1988–1994. Arch Intern Med 2000;160:1683–9. 17. Pena VS, Miravitlles M, Gabriel R, et al. Geographic variations in prevalence and underdiagnosis of COPD: results of the IBERPOC multicentre epidemiological study. Chest 2000;118:981–9. 18. Matheson MC, Abeysena C, Raven JM, et al. How have we been managing chronic obstructive pulmonary disease in Australia? Int Med J 2006;36:92–9. 19. Seemungal TAR, Donaldson GC, Bhowmik A, et al. Time course and recovery of exacerbations in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2000;161:1608–13. 20. Roberts CM, Lowe D, Bucknall CE, et al. Clinical audit indicators of outcome following admission to hospital with acute exacerbation of chronic obstructive pulmonary disease. Thorax 2002;57:137–41. 21. Ram FSF, Rodriguez-Roisin R, Granados-Navarrete A, et al. Antibiotics for exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2006;(2):Art.No.CD004403. 22. Wood-Baker RR, Gibson PG, Hannay M, et al. Systemic corticosteroids for acute exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2005;(1):Art.No.CD001288: 1–36. 23. Lancaster T, Stead F. Physician advice for smoking cessation. Cochrane Database Syst Revi 2004;(4): Art.No.CD000165. 24. Monninkhof EM, van der Valk PD, van der Palen J, et al. Self-management education for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2003;(4):Art.No.CD002990. 25. Turnock AC, Walters EH, Walters JAE, et al. Action plans for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2005;(4):Art.No.CD005074. 26. Barr RG, Celli BR, Martinez FJ, et al. Physician and patient perceptions in COPD: the COPD Resource Network Needs Assessment Survey. Am J Med 2005;118:1415. 27. Australian Lung Foundation and Australian Physiotherapy Association. The Pulmonary Rehabilitation Toolkit. 2006. http://www.pulmonaryrehab.com.au/PDFs/ToolkitChecklist.pdf (accessed 14 May, 2006). 28. Gorecka D, Bednarek M, Nowinski A, et al. Diagnosis of airflow limitation combined with smoking cessation advice increases stop-smoking rate. Chest 2003;123:1916–23. 29. Guideline Development Group. Smoking Cessation Guidelines for Australian General Practice. Australian Government Department of Health and Ageing, 2004. http://www.health.gov.au/internet/wcms/Publishing.nsf/Content/health-pubhlth-publicat-documentsmoking_cessation-cnt.htm/$FILE/smoking_cessation.pdf (accessed 12 June, 2006). 30. Vestbo J, TORCH Study Group. The TORCH (towards a revolution in COPD health) survival study protocol. Eur Respir J 2004;24:206–10. 20