Patient Case Questions: Exacerbation of COPD – Dr
advertisement
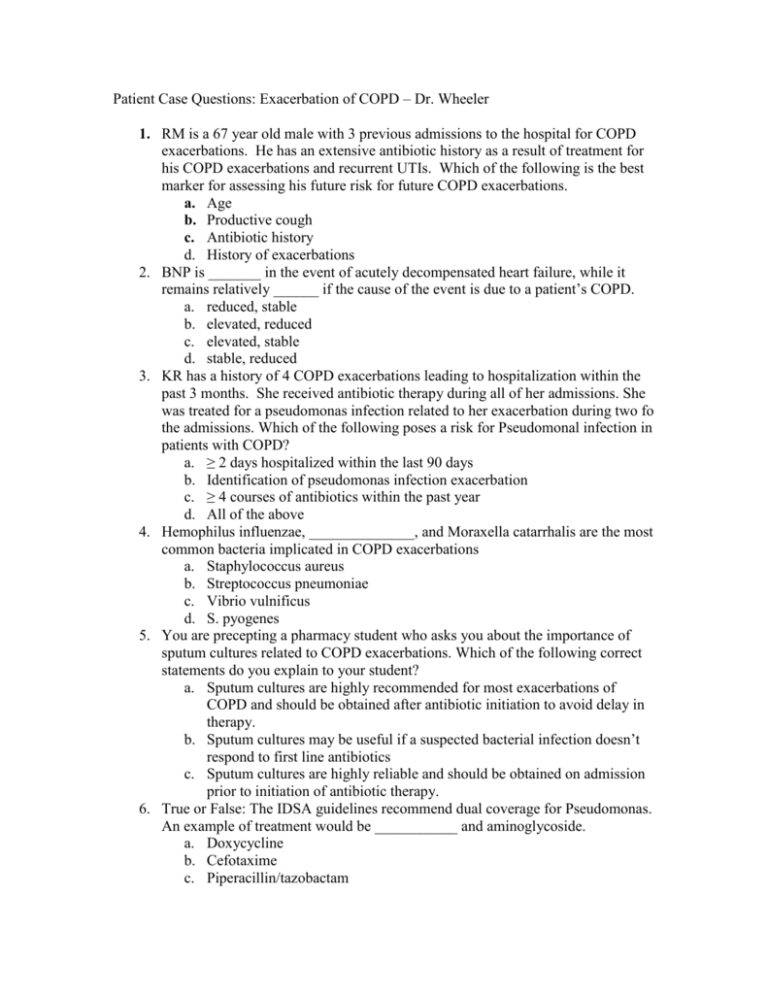
Patient Case Questions: Exacerbation of COPD – Dr. Wheeler 1. RM is a 67 year old male with 3 previous admissions to the hospital for COPD exacerbations. He has an extensive antibiotic history as a result of treatment for his COPD exacerbations and recurrent UTIs. Which of the following is the best marker for assessing his future risk for future COPD exacerbations. a. Age b. Productive cough c. Antibiotic history d. History of exacerbations 2. BNP is _______ in the event of acutely decompensated heart failure, while it remains relatively ______ if the cause of the event is due to a patient’s COPD. a. reduced, stable b. elevated, reduced c. elevated, stable d. stable, reduced 3. KR has a history of 4 COPD exacerbations leading to hospitalization within the past 3 months. She received antibiotic therapy during all of her admissions. She was treated for a pseudomonas infection related to her exacerbation during two fo the admissions. Which of the following poses a risk for Pseudomonal infection in patients with COPD? a. ≥ 2 days hospitalized within the last 90 days b. Identification of pseudomonas infection exacerbation c. ≥ 4 courses of antibiotics within the past year d. All of the above 4. Hemophilus influenzae, ______________, and Moraxella catarrhalis are the most common bacteria implicated in COPD exacerbations a. Staphylococcus aureus b. Streptococcus pneumoniae c. Vibrio vulnificus d. S. pyogenes 5. You are precepting a pharmacy student who asks you about the importance of sputum cultures related to COPD exacerbations. Which of the following correct statements do you explain to your student? a. Sputum cultures are highly recommended for most exacerbations of COPD and should be obtained after antibiotic initiation to avoid delay in therapy. b. Sputum cultures may be useful if a suspected bacterial infection doesn’t respond to first line antibiotics c. Sputum cultures are highly reliable and should be obtained on admission prior to initiation of antibiotic therapy. 6. True or False: The IDSA guidelines recommend dual coverage for Pseudomonas. An example of treatment would be ___________ and aminoglycoside. a. Doxycycline b. Cefotaxime c. Piperacillin/tazobactam d. Azithromycin 7. MH is a 56 year old male presenting to clinic with a COPD exacerbation. He has experienced one exacerbation within the last year, 4 months ago, requiring hospitalization and treatment with antibiotics. His medical history includes: hypertension, diabetes, heart failure, asthma, an extensive smoking history but has quit smoking 3 years ago. Which of the following is an indicator of a poor outcome related to a COPD exacerbation that is demonstrated in MH’s story? a. Age b. Comorbidities c. Antibiotics within the last 90 days d. ≥ 3 exacerbations within the past year 8. You are staffing in the local hospital when you receive an order for a mucolytic via nebulizer for a patient being admitted for a COPD exacerbation. You call the prescriber to discuss the order. Based on current evidence which of the following is the best recommendation? a. Discontinuation of the mucolytic due to little supporting evidence of benefit with increased risk of bronchospasm when delivered via nebulizer. b. Initiation of the mucolytic ASAP to facilitate the clearance of mucus from the patient’s lungs during the exacerbation. Nebulization will deliver the drug to the desired site quickly. 9. Steroids are recommended in the GOLD guidelines for treatment of exacerbations of COPD. According to the guidelines which of the following represents the most appropriate dose of steroids for this purpose? a. Hydrocortisone 100mg q6h b. Prednisolone 30mg daily c. Methylprednisolone 125mg q8h 10. MP has been admitted to the hospital for a COPD exacerbation. Which of the following medications do you expect to see ordered by the prescriber As a primary therapy for the treatment of the exacerbation? a. Advair 250/50 1 puff BID b. Albuterol MDI with spacer 1 puff q1h c. Albuterol 2.5/3mL q1h or continuous and Ipratropium 0.5mg/3mK q4h via nebulizer