Autoclave Qc Policy - Northwestern University
advertisement

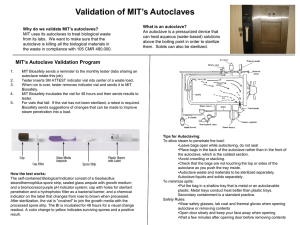
Northwestern University Autoclave Quality Control Policy Office of Research Safety Office of the Vice President for Research Oct 2010, Aug 2005, Aug 2004, May 2002 1 Table of Contents 1.0 INTRODUCTION 3 2.0 THE ART OF STERILIZATION 3 3.0 VALIDATION OF STERILIZATION 5 4.0 AUTOCLAVE TRAINING AND OPERATION 7 5.0 USING AUTOCLAVES SAFELY 7 6.0 AUTOCLAVE OPERATING PROCEDURES 8 7.0 STANDARD OPERATING PROCEDURES 9 8.0 CAUSES OF AUTOCLAVE FAILURE 11 9.0 AUTOCLAVE TESTING 11 10.0 MAINTENANCE PROCEDURES 12 11.0 BENCHTOP AUTOCLAVES 13 12.0 SUMMARY 14 13.0 PURCHASING GUIDELINES 15 APPENDIX A: DAILY AUTOCLAVE LOG 19 APPENDIX B: SIDE DIAGRAM OF AN AUTOCLAVE 20 2 1.0 INTRODUCTION The following information is intended for use as a general guide concerning the operation and maintenance of autoclaves. Consult the owner’s manual or manufacturer for specific information regarding the autoclave used in your facility. Autoclaves are used to destroy microorganisms by subjecting them to steam at elevated temperatures and pressure. These machines are generally used to sterilize materials and pieces of equipment prior to use in laboratories or other facilities. Also, autoclaves are used to make equipment safe for use and reuse and to eliminate risks associated with materials prior to being placed into the waste streams. It is important to consider the performance of steam sterilizers and autoclaves used for these purposes with regard to the potential hazard posed by the microorganism in use. For some microorganisms, additional measures are needed to prevent their release from the autoclave before or after sterilization and to treat exhaust gases and/or condensates, which can be released during or after the process. Considerations should be given to workers, the environment and the public in general. 2.0 THE ART OF STERILIZATION Sterilization is defined as the complete destruction of all forms of microbial life, including bacterial spores through physical or chemical methods. The main physical method is autoclaving; other methods include boiling and dry heat. Chemical sterilization methods involve the use of gases such as ethylene oxide and formaldehyde and liquids like glutaraldehyde or sodium hypochlorite (bleach). Of all these sterilizing methods, autoclaving is the fastest and most reliable. Steam sterilization is a time-tested, dependable and economical process of killing microorganisms through the application of moist heat (saturated steam) under pressure. Steam sterilization generally denotes heating in an autoclave employing saturated steam under a pressure of approximately 15psi to achieve a chamber temperature of at least 121 degrees C (250 degrees F). Heat damages the cell’s essential structures, including the cytoplasmic membrane rendering the cell no longer viable. The rate by which bacterial cells are thermally inactivated depends on the temperature and the time of heat exposure to which they are exposed. In practical terms this means that it would take a longer amount of time at lower temperatures to sterilize a population than at a higher temperature. Additionally, the higher the concentration of organisms that need to be killed, the longer it will take to kill all of the cells in that population at the same temperature. The most critical factor in insuring the reliability of this sterilization method, other than proper temperature and time, is the prevention of entrapment of air that is not replaced by steam. Some autoclaves utilize a steam activated exhaust valve that remains open during the replacement of air by live steam until the steam triggers the valve to close. 3 Physical controls such as pressure gauges and thermometers are widely used but are considered secondary methods of insuring sterilization. The use of appropriate biological indicators at locations throughout the autoclave is considered the best indicator of sterilization. The biological indicator most widely used for wet heat sterilization is a Bacillus stearothermophilus spore suspension or strip. 2.1 Operation Cycles The autoclave uses different patterns of high heat, vacuum, and pressure to sterilize its load. The type of materials you sterilize will determine the type of sterilization cycle you use. The general types of cycles are "liquids" for any type of water-based solutions, "dry goods with vacuum," and "dry goods without vacuum." Autoclaves often have an additional "drying" cycle in which hot air is drawn through the chamber to dry materials before removal. Controls for different brands of autoclaves will vary, so you should follow manufacturers' instructions about loading, load sizes, cycle types and settings carefully. The "liquid” cycle is longer than the other two but uses lower temperatures to minimize evaporation of the liquids being sterilized. The seals on containers of liquids should be loose so that vapor can expand during heating and will not cause an explosion. Never autoclave any flammable or volatile liquids because they could explode. The "dry goods with vacuum" cycle moves steam and heat into the deepest parts of large bags or bundles of materials and produces the best conditions for killing persistent organisms. During this cycle, the chamber alternates between cycles of vacuum and high pressure. Then the chamber is pressurized with steam for a long period, followed by a short vacuum cycle. It is important that steam and pressure be able to reach the entire load, so make sure that autoclave bag closures are not tightly closed once they are in the autoclave. The "dry goods without vacuum" cycle simply pressurizes the chamber with steam for the duration of the cycle, and then returns to normal. This process is used primarily for items that have been cleaned but need to be sterilized. Materials should be packed so that the heat and pressure can readily reach the whole load. 2.2 Methods of Decontamination The two most common categories of physical and chemical decontamination currently used are heat and liquid. 2.2.1 Physical Decontamination Steam heat is the most dependable method of sterilization. Autoclaving (saturated steam under pressure of approximately 15psi to achieve chamber temperature of at least 121 degrees Celsius for a prescribed time) is the most convenient method of rapidly achieving destruction of all infectious agents. In addition to appropriate time and temperature, prevention of the entrapment of air 4 is critical to achieving sterility. Material to be sterilized must come in contact with steam and heat. Chemical indicators, e.g., autoclave tape, must be used with each load placed in the autoclave. The use of autoclave tape alone is not an adequate monitor of efficacy. Autoclave sterility monitoring should be conducted on a regular basis using appropriate biological indicators (Bacillus stearothermophilus spore strips) placed throughout the autoclave. The spores are more resistant to heat, thus providing an adequate safety margin when validating decontamination procedures. The Joint Commission on Accreditation of Healthcare Organizations recommends keeping autoclave spore testing data for 12 months. Dry heat is less efficient than wet heat and requires longer time and/or higher temperature to achieve sterilization, e.g., 12 minutes will kill most spores with steam heat at 121 degrees Celsius while six hours are needed to kill spores with dry heat at the same temperature. Dry heat is suitable for the destruction of viable organisms on impermeable non-organic surfaces such as glass, but it is not reliable in the presence of layers of organic and inorganic materials acting as insulation. Sterilization of glassware by dry heat can usually be accomplished at 160-170 degrees Celsius for periods of 2-4 hours. Dry heat sterilizers should be monitored on a regular basis using appropriate indicators. Most laboratories have gravity displacement autoclaves, which operate at 121o C (15lbs/in2 of pressure). Because of high levels of organic matter normally associated with infectious waste, these types of autoclaves should be operated for a minimum of 60 minutes. Some laboratories may have vacuum-type autoclaves, which operate at 132o C (27lbs/in2 of pressure). It is recommended that these autoclaves be operated for a minimum of 10 minutes. The shorter time period for this type of autoclave is due to the higher temperatures and pressures attainable with the vacuum cycle and the more effective penetration of steam. 2.2.2 Liquid Disinfection The most practical use for liquid disinfectants is surface decontamination and decontamination of liquid wastes prior to final disposal in the sanitary sewer. If liquid disinfectants are used, they must be effective against the organism(s) present. No liquid disinfectant is equally useful or effective under all conditions and for all viable agents. 3.0 VALIDATION OF STERILIZATION The success of sterilization is dependent upon the performance reliability of the autoclave, its users and those factors that determine how valid the results will be. This should include validation of decontamination effectiveness. Validation of effectiveness includes monitoring temperature, pressure and cycle duration time for each cycle and providing periodic decontamination challenges (quality assurance), i.e. use of biological indicators. A logbook should be maintained to record autoclave use and be available for inspection. 5 3.1 Temperature: This denotes the heat produced inside an autoclave using saturated steam under a pressure of approximately 15psi to achieve a chamber temperature of a least 121°C (250°F) for a minimum of 30 minutes. 3.2 Time: Adequate autoclaving time is a minimum of 30 minutes, measured after the temperature of the material being sterilized reaches 121 degrees C and 15psi pressure. The tighter the autoclave is packed, the longer it will take to reach 121 degrees in the center of the load. 3.3 Contact: Steam must contact all areas of the load. Autoclave bags should be left partially open during decontamination to allow steam to penetrate into the bag. Air pockets or inadequate steam supply will cause sterilization failure. Additional water should be added to the bag's interior to facilitate heat transfer to the items being decontaminated. Do not add water if there is a chance that biohazardous materials may splash out of the bag. 3.4 Containers: Properly select and use leak-proof containers for items to be autoclaved. Make sure plastic bags and pans are autoclavable, to avoid having to clean up melted plastic. Plastic bags should specify on the label that they can be autoclaved. 3.4.1 Primary Containers: Autoclave bags come in a wide variety of sizes and colors. They are usually placed in a secondary container during decontamination cycles to catch liquids that may drain out of the bag. 3.4.2 Secondary Containers: Plastic or stainless steel containers are commonly used to contain material during autoclaving. Polypropylene plastic pans with 6-12 inch sides are favored over polyethylene and polystyrene because it can withstand autoclaving without melting. Stainless steel containers are durable and good conductors of heat. 3.5 Indicators: This term refers to the tools used to validate the decontamination process. The most common type of indicator that is used in laboratories is autoclave tape. Tape indicators can only verify that the autoclave has reached normal operating temperatures for decontamination, and have no time factor. Most chemical indicators change color after being exposed to 121 degree C, but cannot measure the length of time spent at 121 degrees C. Biology indicators (such as Bacillus stearothermophilus spore strips) and certain chemical indicators (such as Sterigage) verify that the autoclave reached adequate temperature for a long enough time to kill microorganisms. Once a month, the use of either a biological indicator (e.g., Bacillus stearothermophillus spore strips) or a chemical indicator (e.g., Sterigage) that measures both time and temperature should be buried in the center of the load to validate adequate steam penetration. Record the results in a logbook. 6 3.6 Moisture: Steam saturation is essential for maximum heat transfer. Air pockets or inadequate steam supply will cause sterilization failure. Water can be added to the containers to add moisture prior to autoclaving. 4.0 AUTOCLAVE TRAINING AND OPERATION Principal investigators or supervisors must train and qualify their staff for operation of steam autoclaves for decontamination of materials. Qualified autoclave users should understand the time, temperature, pressure relationships required for proper materials decontamination. Additional training on handling materials to be decontaminated should also be provided. Supervisors should maintain a permanent record of training provided to their staff. Personnel should wear proper personal protective equipment, i.e., heat-resistant gloves, shoes, eye protection and a lab coat, particularly when unloading the autoclave. Regularly inspect your autoclave components for proper operation. If a problem is found, promptly notify your area supervisor, who will contact the appropriate, contracted service provider for repair (e.g, Stericycle). DO NOT OPERATE AN AUTOCLAVE UNTIL IT HAS BEEN PROPERLY REPAIRED. Decontamination conditions vary with type of load, therefore processing times will vary according to the conditions. Consult your owner’s manual or manufacturer for operating instructions. At the end of a decontamination cycle make sure that the pressure in the autoclave chamber is near zero before opening the door. Slowly crack open the autoclave door and allow the steam to gradually escape from within the autoclave. CAUTION: Opening the autoclave door too quickly may result in glassware breakage and/or steam burns on your skin. Allow materials inside the autoclave to cool for 10 minutes before removing them from the autoclave. 5.0 USING AUTOCLAVES SAFELY Autoclaves have become such a commonplace item in many laboratories that people often forget that there are hazards associated with them. Most notable is that they can generate extreme heat and high pressure, potentially resulting in serious burns and health hazards if not operated properly. The conditions created inside steam autoclaves are so extreme that they can easily malfunction if they are not carefully maintained. Autoclave doors and their gaskets must be firmly locked into place before operating the autoclave to prevent a sudden release of highpressure steam. Most, but not all, autoclaves have safety interlocks that prevent the autoclave from running if the door isn't closed properly. Know if yours has an interlock--you'll need to use extra caution if it doesn't. Some older autoclaves have little or no heat shielding around the outside. Attach signs warning of "Hot Surfaces, Keep Away" or similar wording on or next to the autoclave to remind people of the hazard. Do not stack or store combustible materials next to an autoclave (cardboard, plastic, volatile or flammable liquids). Use heat-resistant gloves when removing materials after sterilization and avoid touching the inner chamber surfaces. 7 Burns to the face, third-degree burns, or burns over large areas of the body should be treated as emergencies. Call 911 to get help. You can treat minor burns yourself using standard first aid. Regardless of the degree of severity, report the burn to your supervisor or Principal Investigator as an occupational injury. 5.1 Safety Precautions For safety, please observe the following precautions before operating autoclave equipment. Some materials to be sterilized will be adversely affected by the changes in temperature and pressure, which occur in the sterilization process. To prevent possible injury to personnel and to avoid damage to equipment, products and the environment, the operator must be guided by these rules for safety: DO NOT: • Attempt to sterilize highly volatile and corrosive chemical substances. Autoclave items containing solvents, volatile or corrosive chemicals (phenol, trichloroacetic acid, ether, chloroform, bleach, etc.) or any radioactive materials. Call ORS (Chicago #3-8300, Evanston #-1-5581) if you have questions regarding waste disposal. • Sterilize any substances known to have unstable chemical compositions, which may cause explosive reactions and combustion. • Attempt to sterilize any soiled or badly contaminated material that has not undergone preliminary asepsis. • Attempt to sterilize any glass receptacles, labware, or other material, which has not been designated by its manufacturer as being heat- and moisture-resistant. • Sterilize liquids in containers that are not heat-resistant. Use only Type I borosilicate (Pyrex) glassware. If closures are used on bottles, etc., they must be of the positive self-venting type. • Do not use screw caps or stoppers; use only the “Liquid” cycle for processing liquids. • Sterilize any substances capable of producing noxious and/or toxic fumes, unless the sterilizer (autoclave) is equipped with appropriate filtering and venting features. • Load and unload the chamber in any manner that may loosen closures, topple receptacles or cause any fragile item to crack and break apart. Hot glassware may shatter if jolted. • Ever place sealed containers in an autoclave. Large bottles with narrow necks can simulate sealed containers if filled with too much liquid. • Remove “liquid” loads that are still venting, or that show signs of agitation such as foaming or bubbling. It is advisable to wait at least ten (10) minutes before opening the door to remove the load. 6.0 AUTOCLAVE OPERATING PROCEDURES A written sterilization procedure shall be in place for each workplace. This shall include the following: 8 6.1 Parameters • Appropriate parameters for sterilization shall be determined from the testing with spore vials. • The time it takes to sterilize a load will change depending upon the load density and the sterilization cycle one chooses. Therefore, tests should be performed which imitate these various situations. 6.2 Protocol • Identification of standard treatment containers and proper load placement shall be made. 6.3 Cleaning • The autoclave and work areas shall be cleaned after every use and the work area shall be disinfected, as needed. 7.0 STANDARD OPERATING PROCEDURES 7.1 Dress Code • Leather shoes, which cover the whole foot or rubber boots, are the only types of footwear allowed. Cloth shoes should not be worn, as they do not provide enough protection against hot water spills. • Buttoned lab coats are mandatory at all times • Rubber aprons should be used when removing hot liquids or decontaminated waste bags. • Heavy-duty autoclaving gloves such as Kelklave or Clavies gloves (both available through VWR) are to be worn while removing items from the autoclaves. • Rubber (neoprene) gloves are to be worn while handling dirty glassware in order to prevent cuts, contamination, or acid burns. Figure 1. Examples of protective equipment for personnel 9 7.2 Pre-Loading of Autoclave • Place glassware in a metal pan large enough to contain the summation liquids that are inside the glassware. • Bottle caps should be slightly open to allow steam to escape. Sealing the bottle can cause a dangerous steam build-up. • Arrange loading in autoclave so that the maximum amount of surface can be exposed to the jets for better sterilization. • Use only Type I borosilicate glassware (i.e. Pyrex) in the autoclave. Ordinary glass might shatter from the temperature change caused in running the autoclave. • Apply autoclave tape to each container that will be placed inside autoclave. 7.3 Loading of Autoclave • Follow instructions specific to make and model of autoclave for loading. • Close the door to the chamber, again, follow instructions specific to the make and model of the autoclave. Failure to do so can be disastrous. 7.4 Running of Autoclave • See time setting instructions specific to make and model of autoclave. • Do not alter settings while the autoclave is running in order to prevent incomplete (and therefore false) sterilization. • Do not open the door at any time while the autoclave is running or within ten minutes of the end of the drying cycle. 7.5 Unloading of Autoclave • When the cycle is complete, wait until the chamber pressure gauge reads zero before attempting to open the autoclave. A waiting period of several minutes before removing the bag from the autoclave will allow the chamber and any residual liquids to cool, significantly reducing your chances of getting burned. Also be aware of molten agar that may have collected in the secondary container during the cycle. • Do not stand directly in front of door or touch the door when first opening it! Only touch handle when opening the door. Use the door as a shield when you open the chamber. Otherwise, steam will fly out and scald any flesh in the line of fire. • After ten minutes after the end of the cycle, open the door slightly in order to bleed the high-pressure steam from the chamber. • If sterilizing liquids, let the glassware sit for an additional fifteen minutes. • After steam had been bled from the chamber, open the door (Do not stand directly in the line of fire) and let glassware cool to the touch. Do not remove or jar hot glassware. Hot glassware can easily shatter. Be extremely careful of spillage from liquid still in the glassware. • Remove cool glassware. • Use special caution when autoclaving containers that may have become pressurized. Never autoclave a sealed container of liquids as this may result in an explosion of super-heated liquid during the cycle or when the container is opened. 10 Do not autoclave containers or other receptacles containing bleach. The combination of bleach and residual cotton and oil (improperly cleaned autoclaves) may result in an explosive combustion within the autoclave. 8.0 CAUSES OF AUTOCLAVE FAILURE The reasons behind autoclave failure usually fall into two categories – failure of the operator or mechanical failure. 8.1. The Operator. The operator should be a conscientious, dependable and skilled person. Proper training for the operator will help to minimize autoclave failure due to operator error. Some techniques the operator should be familiar with include: • Use of personal protective equipment (PPE) (see figure 1) • Minimization of aerosol formation • Prevention of waste spillage during autoclave loading and unloading • Prevention of burns from handling hot contents • Management/procedure for managing spills 8.2 Mechanical Failure. Mechanical failures need to be attended to by a trained technician. Contact the service company responsible for the maintenance of your autoclave or your department’s safety representative for more information. Do not override the autoclave’s built-in safety control features under any circumstances. If you suspect that there is a problem with the autoclave's performance notify the principal investigator or repair representative for assistance. 9.0 AUTOCLAVE TESTING Autoclaves shall be tested before being placed into service and then periodically for effectiveness. 9.1 New Autoclaves Prior to placing an autoclave into service, a test load approximating the weight and density of the type of waste generated shall be autoclaved with test spore vials. The spore vials should be placed at the bottom, top, front, rear, and center of the autoclave chamber. This can be achieved by either: • placing vials at those positions within one large test load, OR • making several smaller test packs with 1 vial at the center of each and placing the packs at those locations within the chamber. 9.2 Autoclaves Already In Use The appropriate parameters for sterilization including temperature, pressure, and treatment time shall be determined in this way. For periodic testing place a spore vial in the very center of a test load prior to autoclaving. 9.2.1 Periodic Testing 11 • • Every 40 hours of use (Required for autoclaves that are used to inactivate human or non-human primate blood, tissues, clinical samples, or human pathogens.) Every 6 months (Required for autoclaves that are used to inactivate other material.) 9.2.2 Method • A commercially available test indicator kit that uses bacterial spores (Bacillus stearothermophilus) is the approved method of testing autoclave efficiency. Most spore vial test kits require 56° to 60° C incubation of the autoclaved test vial along with a non-autoclaved control vial. Incubation causes surviving spores to grow. 9.2.3 Storage of Vials • Please read the product information sheet for appropriate storage information, but, in general, spore vials should not be frozen. Each batch of vials has an expiration date. Vials should not be used after their expiration date. 9.3 Routine Maintenance It is a good practice to use a biological indicator (e.g., SGM Biotech’s EZTest® SelfContained Biological Indicator or 3M™ Attest™ Rapid Readout Biological Indicators) monthly to confirm that the autoclave is working properly. If biological indicator fails, you must examine the autoclave to identify and correct the problem and also re-autoclave the load to ensure sterility. The best way to ensure your autoclave is working properly is to have regular maintenance performed semi-annually. In addition, users should perform the daily and weekly maintenance procedures described in the owner's manual. Also, make sure the drain strainer is clean before each run, if applicable. 9.4 Record keeping The following records regarding autoclave use must be kept: • On-site maintenance records • Autoclave use log. Each load of material inactivated shall be logged as follows: • Date, time, and operator's name • Type and approximate amount of waste • Confirmation of sterilization • Record the temperature, pressure, and length of time the load is sterilized. Please note that temperature-sensitive autoclave tape is not sufficient to indicate that the load reached sterilization conditions because the tape will change color at lower temperatures, OR • Save the autoclave printout, if the autoclave has a working printer. 10.0 MAINTENANCE PROCEDURES 12 10.1 Daily Maintenance • Inspect the chamber and loading equipment as necessary followed by a thorough rinse with plain water. Dry with lint free cloths. Never use wire brushes, steel wool, or other abrasive cleaning products on door or chamber surfaces. • Inspect chamber for broken glassware, stoppers, etc. and remove all soil and debris before operating the autoclave. The chamber drain strainer should be lifted out and cleaned and flushed if spilling has occurred during a sterilizing cycle. 10.2 Weekly Maintenance • Flush chamber drain to remove accumulated deposits. Begin by removing and cleaning chamber drain strainer. • Clean exterior surfaces of sterilizer with any good detergent solution and polish dry with a clean soft cloth. 10.3 Quarterly Maintenance • See maintenance and repair manual if needed. 11.0 BENCHTOP AUTOCLAVES The quality of the steam produced in a benchtop steam sterilizer can have a major influence on the efficacy of the sterilization process, the quality of the sterile product and the longevity and serviceability of the sterilizer. The water used in these autoclaves should be one of the following types: • Distilled Water • De-ionized water • Water processed by reverse osmosis. Metals, organic compounds, microorganisms, pyrogens (substances that cause fever) and particulate material are known to have adverse effects on patients and therefore must be controlled. Pyrogens are of particular concern because unlike other contaminants, there are no controls on the level of pyrogens in the public water supply. They are extremely heat stable and are only destroyed when exposed to steam at 250oC for 30 minutes. Some reactive contaminants such as chlorides or phosphates within the steam may cause corrosion to the sterilizer and instruments. For these reasons tap water should not be used. 11.1 Internally Generated Clean Steam In Bench Top Autoclaves 13 Demonstrating compliance to clean steam poses severe difficulties in benchtop autoclaves, as the amount of steam generated in each cycle is so small that the volume of condensate is insufficient for the required laboratory tests. The problem is compounded, as steam-sampling points are not provided. Assurance of clean steam conditions in the chamber must rely on good operating practice rather than testing of samples. 11.2 Operating Practices • • • • • • • Fill with the manufacturers recommended water At the end of each working day the reservoir should be drained down and left to dry. If the autoclave is in constant use and the water is being constantly replenished then the reservoir should be drained down weekly. It is vital to ensure that all instruments are scrupulously clean and dry before being placed in the chamber. If the autoclave is not going be used for long periods of time drain the reservoir and rinse all internal surfaces with distilled water, a mild diluted disinfectant may be flushed through the reservoir and then rinse again with distilled water. If the autoclave has not been used for several weeks then repeat the flushing and rinsing process. Water should not be allowed to remain standing in the reservoir for long periods of time. If water has become contaminated, drain the reservoir and repeat the flushing and rinsing process. 12.0 SUMMARY When the autoclave cycle is complete, you cannot see if the microorganisms have been destroyed and there is no practical test that you can apply. Autoclave tape that changes color only enables you to distinguish between loads that have been in the autoclave and those that have not. Some sterilization indicators can tell you that critical parameters of time and temperature may have been met, but they do not prove sterility. You can infer that a load is sterile because it has been properly processed in an autoclave that is working properly. This means that the instruments have been properly cleaned, correctly loaded into the autoclave chamber, that the correct cycle has been selected and that the autoclave has been pre-tested to ensure that it is performing correctly. It is vital that users are properly trained in safe operation of the equipment, correct preparation of the load, identification of the load type and appropriate cycle, routine testing and record keeping. Validation involves testing the autoclave to ensure that it is working correctly when delivered and periodically thereafter. It also means checking that it is effective for the type of load that you intend to sterilize. 14 The vacuum autoclaves on the market have surprisingly different levels of performance and price. Some may not be capable of sterilizing all of the types of loads you wish to process. The minimum level of performance required is the ability to process porous loads. 13.0 PURCHASING GUIDELINES 13.1 Chamber Construction 13.1.1 Nickel-clad chambers are required: Chlorides are often used in laboratory medias and solutions. Chlorides are known to cause corrosion and pitting of stainless steel that will eventually lead to possible stress cracking of the chamber. Chamber failure may result, posing a potential safety problem. 13.1.2 The chamber weldments, doors and jackets shall be designed to meet the requirements and shall be stamped by ASME. This will ensure that the requirements of the ASME Boiler and Pressure Vessel Code, Section IX are met. 13.1.3 A welded endring of Monel (nickel-copper alloy) or material of similar strength and corrosion resistance shall make up the doorframe. This will ensure that there will be adequate protection against corrosion that can weaken the design integrity, resulting in a door failure and associated safety hazards. 13.2 Controls 13.2.1 A microcomputer control system is preferred. Electromechanical controls are not recommended because they cannot maintain the required documentation and control needed for GLP (Good Laboratory Practice). 13.2.2 The control should be mounted so as not to expose the sensitive components to steam and heat. Controls mounted over the door are not acceptable. This precaution will extend the usable life of the controls and minimize malfunctions. The controls must document all cycle information, including key transition points in the cycle, alarms and deviations that may jeopardize the sterilization process, resulting in inadequate decontamination. 13.2.3 All information and alarms should be in COMPLETE MESSAGES. Coded information that requires a separate manual or chart to decipher what is on the screen or printout is discouraged. An operator must respond to an emergency as quickly as possible. 13.2.4 Controls must document the following minimum cycle alarms: • Vessel Flood Alarm This alarm informs the operator that steam supply failure causes a vessel flood condition. A flooded chamber filled with hot water could 15 result in a serious burn to the operator if he should open the door unaware of the problem. • Steam Table Deviation Alarm This alarm informs the operator that the chamber pressure does not meet the saturated steam table values within 5psi. This is important to guarantee quality control and assure the operator of a proper steam sterilization process. • Chamber Drain Probe Alarm This alarm informs the operator that the chamber drain probe has failed. This will ensure that the operation is aware of this problem and that corrective maintenance can be arranged. • Under Temperature Alarm This alarm informs the operator that the temperature has dropped below a set temperature required for adequate sterilization. • Over Temperature Alarm This alarm informs the operator that the temperature has gone above a set point. This is important with heat labile media’s that can be destroyed if sterilized at too high a temperature. 13.2.5 The sterilizer must provide a manual control that can run a complete cycle, from start to finish manually, in the event of a power failure. Failure to complete a cycle may result in injury to the operator if partially sterilized material must be removed forcibly from the chamber to reset the sterilizer. At a minimum, the operator will be inconvenienced having to restart the sterilization cycle. 13.2.6 The manual control must be located in an easily accessible and safe location for usage, not behind the unit or in an area that is hard to get at. This feature is critical in emergency situations because it allows the complete operation of a cycle with no electrical power. It should also allow manual exhausting of the sterilizer chamber during a malfunction that would otherwise trap a load in the chamber. 13.2.7 The sterilizer should also provide a tamper-proof control with an access code that will prevent programming changes of the cycle parameters (time, temperature) with one or all of the programmed cycles. This feature is important to insure proper sterilization of biohazard contamination and documentation that is required for the load. No "short cuts" can be taken to reduce time, creating an improperly sterilized load. 13.2.8 The tamper-proof control feature must only lock out changes to the cycle parameters, and not the operation of the sterilizer. The tamper- 16 proof control feature must not interfere with the function of the sterilizer. Furthermore, a key lock is not satisfactory due to the fact that misplacement or loss of the key may also shut down the unit. 13.3 Door(s) 13.3.1 The autoclave door should be designed with several independent mechanical and control features that provide for safety. • A control lockout switch in the door that prevents starting a cycle if the door is not closed and locked. • Mechanical steam pressure lock - chamber pressure should "activate" a mechanism engaging the lock mechanism. This will prevent an operator from opening a door if pressure exists in the chamber. • Visual chamber gauge that easily identifies pressure in the chamber must be accessible to the operator. This gauge is a back up to the control read out and will operate with no electrical power to the unit. 13.3.2 Even with a total control failure, all mechanical safety features must be left intact. 13.4 Mounting 13.4.1 The sterilizer should be supported on a steel stand, appropriately coated for corrosion protection. 13.5 Administrative Considerations Questions to ask your autoclave vendor: 13.5.1 What is the cost of maintenance per year of operation? Be sure to compare the costs of replacement parts and the years of warranty because the purchase price will not factor in future repair costs. 13.5.2 What is the warranty of the autoclave? Some autoclave companies charge a lower purchase price but offer a shorter warranty. If a warranty is important to you, ensure that you compare warranties and maintenance service contracts before purchasing. Any savings on the purchase price may disappear after compare the cost of maintenance. 13.5.3 What is the cost of installation? Be sure that if you order a sterilizer that you will not have to spend an exuberant amount to install it. Plumbing and room exhaust renovations may be prohibitively expensive. 17 13.5.4 Does the company have a service representative in the area? Some autoclaves are foreign made and therefore, service representatives are often not available. Be sure that you can get information and a service representative when you need one. 13.6 Facility Considerations 13.6.1 Lab design is very important. The room must have adequate plumbing and electricity. Each autoclave must be installed with a canopy exhaust or other suitable means to dissipate the heat and odors, which may be generated during the sterilization process. 13.6.2 Tabletop Autoclaves. Tabletop autoclaves should not be approved for purchase by the principal investigator or department unless it can be determined that adequate ventilation is present to accommodate the resulting odor. 18 APPENDIX A: DAILY AUTOCLAVE LOG Instructions: (please print) Fill out the boxes below each time you use the autoclave. • • • • • • • • Principal Investigator Location – indicate what lab the biohazard waste was generated Time at 1210C – minimum autoclave time at 12 Chamber temperature – maximum temperature reached Type of waste – check box to indicate the type of waste or material is being autoclaved. Black bag – place check in the box if the material has been placed in a sealed black, opaque plastic bag that is ready for disposal. Operator – indicate person who autoclaved waste Comments – list comments Date PI Lab Rm. Time Max temp Pressure Cycle Used Operator Comments 19 APPENDIX B: SIDE DIAGRAM OF AN AUTOCLAVE 20