undescended testis in awareness - University of Benin University of
advertisement

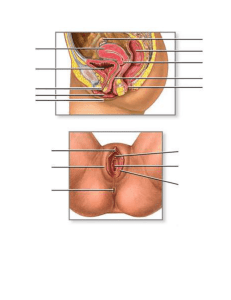
UNDESCENDED TESTIS IN AWARENESS-POOR SUB-REGION BY DR OSARUNWENSE DAVID OSIFO. Consultant Paediatric Surgeon, Paediatric Surgery Unit, UBTH, Benin City. Seminar presented on 4th October, 2012 in Institute of Child Health, University of Benin, Benin City, Edo state, Nigeria. INTRODUCTION During the Institute of Child Health monthly seminar for the month of September 2012 Dr David Osifo a consultant paediatric surgeon of the department of Paediatric surgery, University of Benin Teaching Hospital, Benin City discussed the problem of undescended testis. He noted that complications often result due to late presentation among Nigeria patients. This late presentation he believed was due to lack of awareness. He started the presentation by showing pictures of normal scrotum (figure i) and then pictures of abnormal scrotal sacs. He defined cryptorchid scrotum as meaning hidden testes. This he said may include retractile testes 60.0% of cases, undescended testes 35.0%, ectopic testes 3.0% and ascending in <2.0% cases. The retractile testes is common in adolescents and is usually due to testosterone perhaps due to cold, fear, pain, etc; and sometimes regarded as 'welcome back testes'. Ectopic testes can be found in different parts of the body -inguinal region, abdomen, peritoneum, etc. EMBRYOGENESIS By 8th week of intra-uterine life, the testis is already formed. However due to changes in temperature, the testes migrate from the flanks where it is formed to the scrotum. Fully formed testes function at temperature 3 - 4°C less than the normal body temperature. Continuous exposure to core body temperature has deleterious effect on the testis. The scrotum forms as the shutter window. The descent of the testes occurs in two distinct ways: (a). Intra-abdominal (mechanical) phase- 8 - 1 5 week of gestation (b). Inguinoscrotal phase28 - 35 weeks (hormonal phase). Hormones which include the androgen-calcitonin gene related peptide, and androgen play key roles in that the testes tend to migrate towards areas where there is high concentration of this hormone. Factors which affect intra- abdominal pressures such as in anterior abdominal wall defects as seen in omphalocele, gastroschisis, prune belly syndrome, extrophy of the bladder, etc affect the descent of the testes resulting in undescended testes. The time table for testicular descent according to Dr Osifo is 8th week-formation 12th week: Iliac fossa 15th week: close to the deep inguinal ring 28th week: burrows through the deep inguinal ring 32 week: emerges from the superficial inguinal ring 35 -40th week: descends into the scrotum. 1 There is post natal testicular descent. 4.0% of all males at birth will have undescended testes. This reduces by 1.0% at 1st birthday. In a study published by Dr Osifo and his colleagues in 20091 it was observed that 178/6180(34.9%) infants had fully descended by 7th month of post natal life. About 20.8% of those with undescended testes developed complications between the agel2 and 24 months. The conclusion from this study was to follow-up all undescended testes for 7 months and thereafter all undescended testes should be brought to the scrotum by surgery to avoid irreversible damage to the testes. COMPLICATION OF UNDESCENDED TESTES Dr Osifo noted that almost all complications of undescended testes are preventable. Complications usually result from the effect of the higher intra-abdominal temperatures on the testes which require lower temperatures to function effectively. The effect of undescended testes on the Endocrine function of the testes is usually irreversible. Other complications are reduced germ cell development located in the seminiferous tubules, infertility due to azospermia; malignancy (commonly a seminoma). Inguinal hernia (hernias associated with undescended testes), torsion of a crytorchid testes, trauma, recurrent epididymorchitis, micro-trauma which may damage the testes before the age of 4 years, psychological complications resulting from impotence may also occur. MANAGEMENT Dr Osifo stated that early presentation is very important. Late presentation when complications have occurred can be deleterious to health. Management entails adequate history. Every male is entitled to have two testes in the scrotum. Refer to the specialist if there is only one or no testes in the scrotal sac. Ask for groin swelling, acute pain in the groin and through physical examination should be done. Treatment should be instituted between ages 6 months to 2 years. Surgery is the main stay treatment and involves bringing the undescended testes into the scrotum and fixing it there. 2