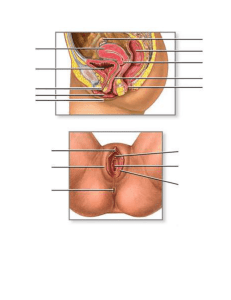
CHAPTER 3: FEMALE SEXUAL
ANATOMY AND PHYSIOLOGY
Gynecological Health Concerns
• Hysterectomy (removal of the uterus) or
oophorectomy (removal of the ovaries)
– Used in cases of cancer of the cervix, uterus or ovaries
– Hysterectomy is most frequently performed U.S.
operation (33% of women undergo by age 65)
– Also used to treat fibroids (non-cancerous growths),
endometriosis, pelvic pain, and irregular bleeding
– Hysterectomy may decrease sexual response in many
women; oophorectomy induces the same hormonal
changes associated with menopause unless
replacement hormones are taken
– More common in poor and less educated women
THE BREASTS
Breasts
• Breasts are a secondary
sex characteristic:
something other than
genitals that distinguishes
men and women
• Mammary glands produce
milk after pregnancy
• Areola is darker area
• Nipple is in center of
areola & has openings for
milk
Cross-Section of Breast
Breast Health Problems
• Breast Lumps: can be detected by self exam
– Cysts (fluid-filled sacs)
– Fibroadenomas (solid, round, benign tumors)
– Malignant tumor
• Breast cancer
–
–
–
–
Treatments: surgery, chemotherapy, radiation
Risk factors: age, hormones, smoking, family history
Reconstructive breast surgery
Early detection & treatment boosts survival
CHAPTER 4
MALE SEXUAL ANATOMY AND
PHYSIOLOGY
Male genitalia are as diverse as female
genitalia
The Penis
• Consists of nerves, blood
vessels, fibrous tissue &
spongy tissue; no bones!
• Interior portion of the
penis is the root
• Head of the penis is called
the glans; this is
surrounded by a ridge
called the corona
• Remainder of penis is the
shaft
The Penis
• Like the vagina, the penis
has 3 layers of tissue: 2
cavernous bodies, and 1
spongy body
• These fill with blood during
sexual excitation, creating
an erection
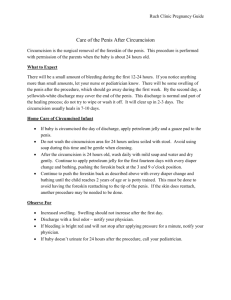
The foreskin & circumcision
• The glans of the penis is
covered by a loose layer of
skin called the foreskin
• Some cultures practice
removal of the foreskin,
usually in infant boys
Circumcision for health?
• 1971: American Academy of
Pediatrics states that there is
no medical benefit to
circumcision
• 1989: AAP states that there
are “potential benefits”
• 1999: AAP states that there
are “insufficient data” to
recommend circumcision
• 2012: AAP states that the
health benefits of
circumcision outweigh the
risks
Circumcision: pros and cons
Cons:
• Complications can arise (rare)
• Foreskin removal may cause trauma from pain
• Reduced sexual enjoyment (?-controversial)
• Cannot be easily reversed
Pros:
• Circumcision reduces rates of sexually transmitted
diseases, including HIV
• Also reduces risk of urinary tract and bladder infections,
and of cancer
For many parents, medical concerns are secondary to
religious/cultural or appearance concerns
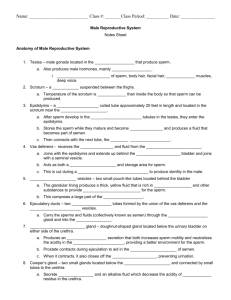
The scrotum
• Scrotum: pouch with two
chambers for each of two
testicles or testes
• Has two layers:
– skin layer: skin is darker
than on rest of body and
becomes covered with hair
at puberty; analogous to
labia majora in women
– tunica dartos: muscle layer
• Pulls sac closer to body
in cold temperatures
The scrotum and testes
• Testes are the equivalent
of the ovaries in females
• Make sperm and also
testosterone and other
hormones
• Spermatic cord holds
each testis
• Also contains the vas
deferens, which delivers
sperm from the testes to
the penis (a vasectomy is
surgical closing off of the
vas deferens)
The testes
• Male gonads (testes) are
outside the body unlike
female gonads (ovaries)
• This is true for most but
not all mammals
• Sperm survive yet at a
temp slightly cooler than
body temperature
Castration
• Castration: surgical removal of the testes;
drastically decreases testosterone and
male sexual behavior; destroys fertility
• Eunuchs: men or boys who have
undergone castration
• Castration has been used as punishment;
many cultures have castrated slaves or
servants
• Castration before puberty was used until
the 19th century in Europe to preserve the
singing voices of boys; some boys’ voices
still underwent changes
The testes: function
• Seminiferous tubules:
site of sperm
production
• Sperm travel from there
to the epididymis,
where they are stored
• Interstitial cells
between seminiferous
tubules make most of
the body’s testosterone
Testicular problems: Cryptorchidism
• In male fetuses, testes develop inside the
abdominal cavity and usually descend into the
scrotum by birth
• Cryptorchidism: failure of the testes to
descend; affects 3–5% of male infants
• Can result in infertility and increased risk of
cancer, but can be treated very effectively
with hormones and/or surgery
Testicular problems: testicular cancer
• Most common cancer in males
age 20–35
• Accounts for 1–2% of all
cancers in males
• Risk factors include smoking,
family history, white race, and
cryptorchidism
• Usually shows up as a mass in
one testicle, can be detected
by male genital self-exam
(described in book)
• Early detection results in
greater than 90% survival
The prostate
• The prostate makes
seminal fluid, the fluid in
which sperm leave the
body
• Seminal fluid + sperm =
semen
• 50% of men over age 60
and 90% of men over age
90 experience benign
prostatic hyperplasia or an
enlarged prostate
• This can cause urinary
issues!
Prostate cancer
• Second most common cancer in American
males (after skin cancer)
• Risk factors are: old age, family history, highfat diet, African-American race
• 218,000 U.S. men are diagnosed each year
and 28,000 U.S. men die from it each year
• Can be detected with a blood test (somewhat
controversial) or with a physical examination
(digital rectal examination)
“Male and female reproductive anatomy
shows more similarities than differences”
How strongly do you agree or disagree with this
statement? Support your answer with specific
evidence.
1
2
3
4
5
strongly
disagree
somewhat
disagree
neutral
somewhat
agree
strongly agree