DISSECTION 18 The Thoracic Wall and Pleura
advertisement
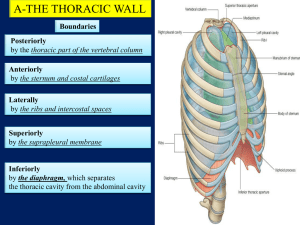
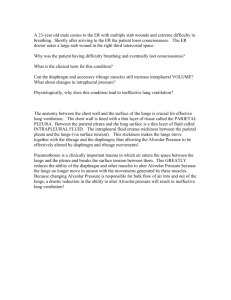
DISSECTION 18 The Thoracic Wall and Pleura References: M1 72-97, 106-111; N 178-188, 192-194, 226-227; N 185-194, 196-198, 230-231; R 195-201, 254-255 AT THE END OF THIS LABORATORY PERIOD YOU WILL BE RESPONSIBLE FOR THE IDENTIFICATION AND DEMONSTRATION OF THE STRUCTURES LISTED BELOW: 1. Bones and bony features: sternum [manubrium (clavicular notch, suprasternal (jugular) notch), body of the sternum (costal notches), xiphoid process] manubriosternal synchondrosis, sternoclavicular joint, sternal angle; ribs (head, neck, tubercle, costal angle, costal groove), costal cartilages, thoracic vertebrae (facets on bodies for head of rib, facets on transverse process for tubercle of rib). 2. Muscles and fascia: external intercostal, external intercostal membrane, internal intercostal, innermost intercostal, transversus thoracis. 3. Nerves: intercostal. 4. Vessels: posterior intercostal, anterior intercostal, internal thoracic artery and vein. 5. Serous membranes: parietal pleura, (costal, cervical, mediastinal, diaphragmatic), costomediastinal reflection, costodiaphragmatic reflection, visceral pleura. 6. Subdivisions of the pleural cavity: costomediastinal recess, costodiaphragmatic recess. YOU SHOULD ALSO BE ABLE TO DO THE FOLLOWING THINGS: 1. State the characteristics of thoracic vertebrae and the changes one encounters in moving from upper to lower thoracic regions. 2. Identify the basic features of a rib and special characteristics of the first rib and lower five "false ribs". 3. Describe the basic movement of the ribs in respiration and name the major muscles involved in inspiration and expiration. 4. State the relationship of the intercostal vessels and nerves to the intercostal muscles. 5. Define the following terms: pleura, pleural cavity, pleural recess, pleural reflection, mediastinum and visceral, parietal, costal, cervical, mediastinal and diaphragmatic pleura. 6. Draw and label on a diagram of the thoracic wall the approximate position of the pericardial sac and the lines of reflection of the parietal pleura. 7. Label on a diagram a typical intercostal nerve or artery and its branches; be aware of the general distribution of the branches. 8. List the types of fibers found in an intercostal nerve and its muscular and cutaneous branches. Locate the cell bodies of origin of each type of fiber. The Thoracic Wall Before beginning the dissection identify on the skeleton the bones and bony features listed above. Then on the cadaver palpate the STERNOCLAVICULAR JOINTS, the SUPRASTERNAL NOTCH, the MANUBRIUM, BODY OF THE STERNUM and the STERNAL ANGLE between them. Note that the first rib articulates Dissection 18, Thoracic Wall and Pleura with the manubrium near the sternoclavicular joint, the second rib articulates with the sternum at the sternal angle and the remaining five true ribs articulate with the body of the sternum. Besides the seven true ribs there are five "false" ribs, three of which articulate anteriorly by means of a common cartilage attached at the xiphisternal junction and two of which, the "floating" ribs, have no anterior attachment (G1.9A; N178; N185; A149). Carefully dissect the structures in an intercostal space (the area between two ribs). Note that the EXTERNAL INTERCOSTAL MUSCLE does not reach to the sternum but is replaced by an EXTERNAL INTERCOSTAL MEMBRANE. Deep to this muscle is the INTERNAL INTERCOSTAL MUSCLE whose fibers run almost at right angles to those of the external intercostal. The intercostal vessels and nerves run in the cranial part of the intercostal spaces just below the ribs deep to the internal intercostal muscle. The POSTERIOR INTERCOSTAL VEIN lies in the COSTAL GROOVE, just internal to the inferior border of the rib, and the POSTERIOR INTERCOSTAL ARTERY and the INTERCOSTAL NERVE are just below the vein in that order (N184; N191). Near the midaxillary line the INNERMOST INTERCOSTAL MUSCLE layer can be seen. The intercostal vessels and nerves lie between the innermost intercostal and internal intercostal muscles and these are the best guides for distinguishing between these two muscle layers. Posteriorly the internal intercostal muscle does not reach the vertebral column but is replaced by the internal intercostal membrane (G1.15, 18; N187; N192). This will be seen when the posterior wall of the thorax is dissected. Remove the external intercostal membrane and the deeper internal intercostal muscle for an inch or so lateral to the sternum in each of the intercostal spaces. Leave the underlying pleura intact (G1.19, 20, 26; A182). This will reveal the vertically running INTERNAL THORACIC ARTERY and VEIN (A146; N184; N191). The ANTERIOR INTERCOSTAL ARTERIES arise from the artery and the vein receives as tributaries the ANTERIOR INTERCOSTAL VEINS. The anterior intercostal Page 2 vessels are continuous with the posterior intercostal vessels, which have their origin from the thoracic aorta or terminate in the azygos or hemiazygos veins (G1.15, 75, 76; A233, 234, 235; N183, 184, 187; N189, 191, 192). The first intercostal space is an exception to this general vascular pattern in that it is usually supplied by a costal branch from the costocervical trunk of the subclavian artery (A233). In preparation for removal of the anterior thoracic wall be sure to leave the previously dissected intercostal muscles intact, but remove the remaining intercostal musculature from the upper seven interspaces on both sides as far laterally as the midaxillary line, carefully avoiding damage to the parietal pleura. Using your fingertips, depress the pleura from the thoracic wall, to which it is usually bound by a small amount of connective tissue, the endothoracic fascia. When the parietal pleura has been freed, the sternum and ribs may be divided. Rib and Sternal Incisions To remove the anterior thoracic wall, reflect the serratus anterior to the midaxillary line and divide the manubrium transversely above the sternal angle, but keep the sternoclavicular joint intact. Cut the second through the fifth ribs in the midaxillary line and sever the sternum once more, below its junction with the fifth pair of COSTAL CARTILAGES. Dissection 18, Thoracic Wall and Pleura After removing the sternum and ribs demonstrate the INTERNAL THORACIC ARTERIES (G1.19, 20; N184; N191; A162); these are branches of the subclavian arteries. Look for their ANTERIOR INTERCOSTAL BRANCHES. How many are present in each interspace? What are the terminal branches of the internal thoracic arteries? Note any retrosternal lymph nodes and vessels. The TRANSVERSUS THORACIS MUSCLE, the sternal representation of the innermost intercostal, should also be identified. Retain the detached sternum and ribs for further study. As the dissection proceeds, occasionally replace the excised portion of the thoracic cage to review the thoracic visceral topography. Give particular attention to the relation of the pleura, heart, and great vessels to the anterior thoracic wall. The Pleura Each lung is enveloped by a serous membrane, the VISCERAL PLEURA (G1.24C, 26; N194; N198; A168-171), which is continuous with the PARIETAL PLEURA lining the thoracic wall (G1.24C; N194; N198; A163). These two membranes are continuous with each other at the hila of the lungs. The VISCERAL PLEURA intimately invests the lung and is not separable from it. The parietal pleura is adherent to the internal surface of the thoracic wall by the endothoracic fascia. Between the parietal pleura and the visceral pleura is a potential space containing only a thin film of serous fluid. This potential space is called the PLEURAL CAVITY (N192, 193; N196-197). The parietal pleura, visceral pleura and pleural cavity of the right side make up the right pleural sac, which is not continuous with that of the left side. The parietal pleura is subdivided for convenience of description and named according to its location. Distinguish the COSTAL (lining the ribs), CERVICAL (extending above the first rib into the root of the neck), MEDIASTINAL, and DIAPHRAGMATIC components of the parietal pleura. These subdivisions of the parietal pleura are, of course, continuous with one another where they "reflect" from contact with one surface to another. Observe on the specimen the COSTODIAPHRAGMATIC (N192; N196) and Page 3 REFLECTIONS of the parietal pleura (G1.68; A163). What is the rib level of the costodiaphragmatic reflection in the midaxillary line? (G1.26; A166, 167). COSTOMEDIASTINAL In quiet respiration the lungs are not expanded fully, and the parietal pleura is not everywhere in contact with the visceral pleura covering the lungs. Below the lower border of the lung (eighth rib) the costal and diaphragmatic portions of the parietal pleura are in apposition. Similarly, anteriorly, the costal and mediastinal parietal pleurae are in apposition along the line of reflection. These areas within the parietal pleura which are not in direct contact with visceral pleura of the lung are called "recesses" or "sinuses." Thus there are COSTODIAPHRAGMATIC RECESSES and COSTOMEDIASTINAL RECESSES in each pleural cavity. Some of these recesses allow a needle to be placed in the pleural space with little danger of damage to the lung. What is this procedure called? For what purpose is this done? After inspecting and palpating the extensions of the parietal pleura, make an incision in the parietal pleura over each lung as indicated in the previous diagram. Place your hand in the PLEURAL CAVITY, and explore the limits of the cavity, noting the costodiaphragmatic and costomediastinal recesses in particular. Dissection 18, Thoracic Wall and Pleura Put your fingertips in each costomediastinal recess. Is the space continuous across the midline? Can you pass your hand from one pleural cavity into the one on the opposite side dorsal to the pericardial sac? Does your cadaver Page 4 have any strands of connective tissue attaching the adjacent visceral and parietal pleurae over the convexity of the lung? What are such connections called? What is the origin of these connections? ______________________________________________________________________________________________ STUDY QUESTIONS 1. Localize the position of the pericardial sac with respect to the anterior thoracic wall. 1. See M1 171-173 or G1.42. a. The apex is in the 5th. interspace just medial to the midclavicular line. b. The right border extends from the 3rd costal cartilage to the 6th costal cartilage a fingerbreadth from the right margin of the sternum. c. The inferior border lies along a line from the inferior end of the right border through the xiphisternal joint to the apex. d. The left border lies along a line from the apex to the second interspace a fingerbreadth to the left of the sternum. e. The superior border lies along a line from the left second interspace to the right third costal cartilage. 2. What are the divisions of the thoracic cavity? 2. The thoracic cavity is divided into the right and left pleural cavities and the mediastinum. 3. What are the normal contents of the pleural cavities? 3. Only a capillary layer of serous fluid. 4. Name and define the subdivisions of the pleura. 4. The visceral pleura is the serous membrane that covers the lung everywhere except at the root of the lung. The parietal pleura lines the thoracic wall. It has four components which are 1) the costal pleura which lines the inner surface of the ribs and costal cartilages and the intercostal muscles; 2) the mediastinal pleura which covers the mediastinum; 3) the diaphragmatic pleura, which covers the superior surface of the diaphragm lateral to the mediastinum; and the cervical pleura, which extends into the root of the neck. Dissection 18, Thoracic Wall and Pleura Page 5 5. What are the lines of pleural reflection? 5. The lines of pleural reflection mark where the costal pleura becomes continuous with mediastinal pleura and with the diaphragmatic pleura. 6. Where does the sternal (anterior costomediastinal) reflection of the pleura deviate from the midline? 6. Above the sternal angle on both sides; behind the xiphoid process on the right side and at the 4th costal cartilage on the left side. 7. Where does the costodiaphragmatic reflection cross the a) midclavicular line? b) midaxillary line? c) body of the vertebra? 7. 8. Where do the reflections of the parietal pleura pass beyond the limits of the thoracic skeleton? 8. At the right xiphisternal angle, at both right and left costovertebral angles (below 12th ribs), and above the anterior portions of both first ribs. 9. What is the pulmonary ligament? 9. The pulmonary ligament is a double layered reflection of mediastinal pleura that becomes continuous with visceral pleura below the root of the lung. a. b. c. 8th rib 10th rib below the 12th rib 10. Discuss the innervation of the pleura. Is the pleura sensitive to pain? Is there pain referral from the pleura to other parts of the body? 10. The costal pleura and peripheral part of the diaphragmatic pleura are innervated by intercostal nerves and are quite sensitive to pain. The mediastinal pleura and central part of the diaphragmatic pleura are innervated by the phrenic nerve, and pain from these regions tends to be referred to the lower neck and shoulder. Why? The visceral pleura is insensitive to pain. 11. Add lines of pleural reflection to a diagram of the thoracic skeleton. 11. Dissection 18, Thoracic Wall and Pleura 12. From what artery is the internal thoracic a branch? What are the branches of the internal thoracic? Underline the terminal branches. To what vessel does the internal thoracic vein drain? 13. Define: Pleural cavity Page 6 12. The subclavian Pericardiacophrenic, thymic, sternal, mediastinal, anterior intercostal, perforating, musculophrenic, and superior epigastric. The brachiocephalic vein. 13. Potential space between parietal and visceral pleurae. Costomediastinal recess Pleural "space" along the anterior pleural reflection where the parietal pleura is not in contact with the lung (visceral pleura). Costodiaphragmatic recess Pleural space between the eighth and tenth ribs in the midaxillary line into which the lung does not extend in quite respiration; lined peripherally by costal (parietal) pleura and centrally by diaphragmatic (parietal) pleura; a common site for thoracentesis. 14. The sternal angle is a surface landmark of considerable importance. What structures lie deep to it? 14. The sternal angle marks the junction of the second ribs with the sternum and also is at the level of the disk between T4 and T5. The bifurcation of the trachea and the beginning and end of the aortic arch lie at this level. A horizontal plane through the sternal angle is the boundary between the superior mediastinum and the inferior mediastinum. 15. What structure is in direct relationship to the left sides of the bodies of the middle four thoracic vertebrae? 16. What is the nature of the union between rib and costal cartilage? Between costal cartilage and sternum? 17. Define the term "thoracic inlet". Give its boundaries. 18. Define the term "thoracic outlet". Give its boundaries. Dissection 18, Thoracic Wall and Pleura Page 7 19. What is a dermatome? 19. A dermatome is the region of skin supplied by the afferent fibers of a single spinal nerve. 20. Which spinal nerve supplies the dermatome including: a. the nipple? b. the infrasternal angle? c. the umbilicus? 20. 21. Describe the movements of the ribs in inspiration and expiration. 21. a. b. c. T4 T7 T10 M1 Fig. 1.10,p82 LJ:bh revised 06/18/09