- American College of Obstetricians and Gynecologists
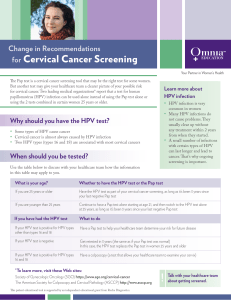
advertisement

AMERICAN COLLEGE OF OBSTETRICIANS AND GYNECOLOGISTS ARMED FORCES DISTRICT 2013 Project J-FIT Proposal 1) TOOLKIT NAME: An Initiative to Educate Primary Care Providers: PAP Smear Guidelines and Contraception Options at Your Finger Tips 2) PROJECT MANAGER CONTACT INFORMATION: Name: April McGill Address: 4789 Sunmore Pkwy, Twentynine Palms, CA 92277 Phone number: (706) 825-6963 Email address: april.mcgill@med.navy.mil 3) TEAM MEMBERS NAMES AND EMAIL ADDRESSES Kaycee Fiaseu Kaycee.Fiaseu@med.navy.mil Joshua Combs Joshua.Combs.5@us.af.mil Erin Keyser Erin.A.Keyser.mil@mail.mil The Armed Forces District Junior Fellow Officers 4) OBJECTIVES: To educate primary care providers on important topics in the women’s health care field including the 2013 ASCCP Pap Smear Guidelines, the appropriate use of HPV Genotype testing, and basic information about contraceptive options along with their indications/contraindications. With the PAP smear initiative, we hope to ensure that the correct frequency and type of tests are performed for all women and that the appropriate follow-ups are offered to maximize the use of pap smears as screening tests for cervical cancer. With the contraceptive initiative, we hope to improve the unintended pregnancy rate in the military population, which currently remains high despite universal access to healthcare and free contraception. Both of these initiatives will also provide leadership and teaching opportunities for Junior Fellows. 5) KEY WORDS FOR SEARCHES: ASCCP Consensus Guidelines, Pap Smear, HPV, Primary Care Physicians, Contraception, Unintended Pregnancy, Women’s Health Education, Cervical Cancer Screening 6) TARGET AUDIENCE: Military primary care providers (including OB/GYN physicians, Family Medicine physicians, Internal Medicine physicians, Nurse Practitioners, Physician’s Assistants, Nurse Midwives, General Medical Officers, Flight Surgeons, and Independent Duty Corpsmen) 7) DATES OF PROJECT / TIMELINE: The resource cards were developed over 2012 and 2013 after the new ASCCP guidelines and algorithms were published. The PAP smear cards were published on the ACOG Junior Fellow AFD website in the summer of 2013 and the badge cards were printed for distribution at the AFD Annual Clinical Meeting in October. The study associated with the Contraception Card was submitted for IRB approval in August 2013 at William Beaumont Army Medical Center, and is currently being submitted to IRBs at other commands to increase the data included in the study. Junior Fellow volunteer teachers were identified at the AFD District Meeting in October, and the educational materials were distributed to them at that time including electronic versions of both resource cards and badge cards for the PAP smear resource. The volunteers will plan lectures and distribution of educational material throughout the upcoming year at their own commands and near-by facilities. 8) VENUE: Annual Armed Forces District meeting, Individual commands 9) Contact Person email address at venue: N/A 10) NUMBER OF PARTICIPANTS: 1000 PAP badge cards were produced and distributed to attendees of the 2013 Armed Forces District Meeting to be distributed to medical facilities nationwide in the Navy, Army and Air Force. 205 charts total were included in the initial Contraceptive Card Study (pre- and postdistribution) 11) LIST OF ALL SUPPLIES NEEDED: PAP Smear Badge Cards (ordered online) Contraceptive Information Cards (produced at individual facilities) Brief Powerpoint Presentation 12) PROJECT PREP TIME: After development of the resources (which are now available for anyone to use), this project only requires printing of the resources and distribution to providers with the optional 15-minute PowerPoint presentation. NUMBER OF VOLUNTEERS NEEDED: Variable on your targeted distribution. Could be as little as 1 person 2 DELEGATION OF PROJECT RESPONSIBILITIES: Each volunteer is responsible for producing the resource cards and distributing to primary care providers at an identified facility 13) ADVERTISEMENT: Recruitment of volunteers to distribute materials was done by word of mouth within the AFD Junior Fellow Leadership. Also, the resource cards were placed at each of the seats at the AFD Annual Clinical Meeting with several announcements made that additional cards were available for attendees to take back to their home facilities. 14) BUDGET: - cost of 1000 PAP badge cards to be printed online (double-sided in color with lanyard hole punch) and delivery costs – $355 on http://4colorprint.com Powerpoint – Free Contraceptive Cards were printed for free at local medical facilities 15) FUNDING: Funding ($1000) was provided by the ACOG Armed Forces District Advisory Council 16) SUMMARY: PAP Smear Initiative The PAP Smear resource badge card was developed over several months based on the article by Saslow et al in 2012 detailing the new screening guidelines, the 2013 ASCCP Cytology Algorithms, and the ACOG Practice Bulletin #131 published in NOV 2012. The card was reviewed by several Gynecologic Oncologists for accuracy. The PDF files were then uploaded to http://4colorprint.com for printing (12mil plastic cards were chosen because they are both tear and water proof). A copy of the PDF files are included below and are available for download on the AFD Junior Fellow website. Several Junior Fellows were also able to print some cards at their home command free of charge. The cards were then brought to the Armed Forces District Annual Clinical Meeting. A set of the cards was placed at each seat for attendees of the meeting. Several announcements were made for people to take cards back with them to their home hospitals. The extra cards were available at the registration desk. The junior fellow officers were instructed to take cards back with them for distribution at their home hospitals and were given access to a power point presentation to give a brief lecture to the primary care providers that they would be distributing to. A copy of the power point presentation is also included below as well as available on the AFD Junior Fellow website. Contraception Initiative The Contraceptive resource badge was developed from the CDC U.S. Medical Eligibility Criteria for Contraceptive Use and various textbooks. The card was reviewed by several 3 OB/GYN providers for accuracy. A copy of the PDF is included below and will be available shortly on the AFD Junior Fellow Website. An IRB-approved study was conducted at William Beaumont Army Medical Center using this contraception card. This study was designed to try to assess if women are being asked and offered contraception regularly at well women/routine visits. It is ACOG’s standard of care and belief that every woman should be on contraception if not actively trying to conceive. So, at each visit, every woman should be asked about contraception and offered birth control if interested, hence our slogan, “Every Woman, every time!” This study contained three parts. The first was a chart review of randomly selected charts to see if women are being asked about birth control, and, if not using anything, are being offered contraception during their primary care visits. Six data points were extracted from the charts: 1. Age range (18-­‐25, 26-­‐35, >35) 2. Asked about contraception? Y/N 3. Using contraception? Y/N 4. Trying to conceive? Y/N 5. If not using and not trying to conceive, was she offered contraception? Y/N 6. If yes, was she offered: pills, patch/ring, depo, implant, IUD, permanent? Y/N. And was GYN consult placed? Y/N In the second portion of the study, primary care providers were asked to complete a pre-­‐test on their knowledge about current contraceptives and their uses. Following this test, each provider was given the contraception card that we created. A month later, the providers were given the same test as a post-­‐test (included below). The third part of the study was a chart review of another set of randomly selected charts (for visits that took place one month following the distribution of the “contraception cards”) to see if there has been improvement in their contraceptive counseling. The study has not yet reached statistical significance, but overall the resource card was well received by the primary care providers. The study is currently being expanded for replication at other facilities to determine if it did indeed help improve counseling and provider knowledge. The resource card will be available for distribution from the Junior Fellow Website. 4 17) Photography/Pictures Motivating Junior Fellows to take resources back to their home facilities at the Armed Forces District Meeting 5 PAP Smear Card Abbreviations When to Perform Cervical Cytology Based on ASCCP 2012 Guidelines Population Recommended Screening <21 None 21-29 PAP every 3 yrs (no HPV) 30-65 PAP & HPV every 5 yrs (or PAP every 3 yrs) >65 None (following adequate negative prior screening*) After Hysterectomy NILM ASCUS None (without cervix and without Hx of CIN2 or greater) LSIL Low-grade squamous intraepithelial lesion HSIL High-grade squamous intraepithelial lesion ASC-H Atypical squamous cells, cannot rule out high-grade lesion HPV Human papillomavirus Hx of CIN2 or greater Routine screening for 20 years (even after hysterectomy) EC/TZ Endocervical/Transformation zone HIV+ Twice in the first year after diagnosis, then annually CIN Cervical intraepithelial neoplasia AGC Atypical glandular cells ECC Endocervical curettage DES Diethylstilbestrol EmBx Endometrial biopsy Colpo Colposcopy Immunosuppressed Annually Annually DES in utero HPV vaccination Follow age-specific guidelines (same as unvaccinated) *3 consecutive negative cytology results (or 2 consecutive negative co-tests) within 10 yrs prior to cessation of screening, with the most recent within 5 yrs Based on ASCCP 2013 Algorithms Cytology Results Unsatisfactory Age Recommendations Repeat PAP 2-4 months OR Any if ≥ 30 and HPV+, may colpo If HPV-, routine screening If HPV+, PAP & HPV in 1 yr. ≥30 OR HPV genotype for 16/18 If HPV unk, HPV testing OR PAP in 3 yrs. HPV genotype for 16/18 OR repeat PAP & HPV in 1 yr. If repeat PAP ≥ASC or HPV+, colpo NILM & HPV+ ≥30 ASCUS, HPV unk HPV testing OR repeat PAP in 1 yr. If repeat PAP is NILM, Any routine screening, otherwise colpo Recommendations ≥25 PAP & HPV in 3 yrs. PAP & HPV in 1 yr. (preferred) If NILM, HPV-, repeat PAP & HPV in 3 yrs, otherwise colpo OR immediate colpo LSIL, HPV- Any ASC-H or HSIL Colpo OR If HSIL & ≥25 & not Any pregnant, may do immediate LEEP AGC or Atypical Endocervical Cells Atypical Endometrial Cells 21-24 Routine screening ASCUS, HPV- Age PAP in 1 yr. - If NILM, ASC, or LSIL, repeat PAP again in 1 yr. 21-24 If 2nd repeat PAP is ≥ASC, then colpo. Return to routine screening after NILM x 2 ASCUS,HPV+ or LSIL Colpo ≥25 If pregnant, colpo now (preferred) or at least 6 wks postpartum 21-29 Routine screening NILM, EC/TZ insufficient Cytology Results Referral Guidelines for Abnormal PAP Negative for intraepithelial lesion and malignancy Atypical squamous cells of undetermined significance Colpo, ECC, and EmBx if ≥ 35 Any or chronic anovulation or unexplained vaginal bleeding Any ECC and EmBx. Colpo if both negative Saslow D, et al. ACS, ASCCP, and ASCP screening guidelines for the prevention and early detection of cervical cancer. ©2012 ASCCP Cytology Algorithms ©2013 ACOG Practice Bulletin #131 NOV 2012 6 Pap Smear Power Point Abbreviations NEW Pap Smear Guidelines ASCCP 2012 GUIDELINES AND ASCCP 2013 ALGORITHMS ERIN A. KEYSER, MD, FACOG MAJ, MC, USA DEPT OF WOMEN’S HEALTH WILLIAM BEAUMONT ARMY MEDICAL CENTER ! NILM: Negative for intraepithelial lesion and malignancy ! ASCUS: Atypical squamous cells of undetermined significance ! LSIL: Low-grade squamous intraepithelial lesion ! HSIL: High-grade squamous intraepithelial lesion ! ASC-H: Atypical squamous cells, cannot rule our high-grade lesion ! AGC: Atypical glandular cells ! Used to be AGUS Cervical Cancer ! In US, about 12,000 cases of cervical cancer/year -> 4,000 deaths/year ! ! ! 50% never screened 10%, not screened in last 5 years Mean age: 48 years ! Worldwide: major health problem ! ! 530,000 cases per year worldwide -> 230,000 deaths/year Mortality: 52% ! On average, severe dysplasia takes 3-7 years to progress to invasive cervical cancer ! Cervical cancer screening effective! ! Key to getting cancer: persistent HPV (at 1 and 2 years) ! Increased likelihood of persistent infection: " Smoking, compromised immune system, and HIV Cervical Cancer and HPV ! Oncogenic HPV causes cervical cancer ! Among 40 types of HPV, 15 are oncogenic ! HPV 16 highest carcinogenic potential ! 55-60% of all cases of cervical cancer worldwide ! HPV infection ! 75-80% of sexually active adults will acquire HPV " Most common in teenagers and women in early 20’s 85-90% will clear infection in an average of 8 months (8-24 months) ! CIN 1 usually reflects acute HPV and most will regress ! 7 1% 12/1/13% When to screen 2012 Recommended Screening ! As of 2012 ! ! ! ! ! Pap smear screening should begin at age 21, regardless of age of sexual initiation. Based on low incidence of cancer (0.1% of cases of cervical cancer) Lack of data that screening is effective in this age group Overtreatment " Increasing rates of PTB " Anxiety Only exception: HIV infected patient ! Type of pap smear screening ! Liquid based allows you to concurrently test HPV and other tests " Same sensitivity/specificity as conventional cervical cytology screening HPV Testing risk” HPV genotypes Additional HPV DNA Genotype that can test specifically for 16 or 18 ! Two indications for HPV testing ! ! ! ! ! ! 30-65: PAP and HPV every 5 years (or PAP every 3 years) ! > 65: None (following adequate negative prior screening*) ! After Hysterectomy: None (without cervix and without Hx of CIN 2 or greater) * 3 consecutive negative cytology results or 2 consecutive negative co-tests within 10 years prior to cessation of screening, with the most recent within 5 years. ! HIV patients: Twice in the first year of diagnosis, then annually ! Immunosuppressed: Annually ! DES in utero: Annually Reflex Testing – following ASCUS PAP " ALTS Trial, 2002 Co-Testing in women 30-65 yrs of age ! s/p HPV vaccination: No change, follow age based screening recommendations ! Co-Testing q 5 years ! ! 21-29: PAP every 3 years (NO HPV) Special circumstances ! HPV screening: 15-18 potentially cancer causing “high ! ! < 21: None 3 RCTs: More effective at detecting high grade dysplasia and adenocarcinoma which is often missed by cytology alone Lower cancer rates Fewer follow up colposcopy Ordered in CHCS 1 or ahlta: " Labs -> HPV -> digene brush 8 2% What do the results mean? What to do with the results ! Risks of cervical neoplasia with abnormal cervical cytology: Incidence (percent) Cervical Cytology CIN 2+ CIN 3+ Cervical cancer Negative 0.68 0.26 0.025 ASCUS, HPV pos 18 6.8 0.41 ASCUS, HPV neg 1.1 0.43 0 LSIL 16 5.2 0.16 ASC-H 35 18 2.6 HSIL 69 47 7.3 AGC 13 8.5 2.7 Referral Guidelines for Abnormal Paps ! Unsatisfactory: Repeat PAP in 2-4 months ! OR if > 30 and HPV pos may colpo ! NILM, EC/TZ insufficient: ! 21-29: routine screening, assume negative ! > 30: Neg: Routine screening " HPV Pos: repeat PAP and HPV in 1 year " Or HPV genotype 16/18, and if pos, colpo now " HPV ?: HPV testing or repeat PAP in 3 years ! NILM and HPV Pos: > 30 ! HPV genotype for 16/18 and if pos, colpo now OR ! Repeat PAP and HPV in 1 year ! ASCUS, HPV unknown: Any age ! HPV Testing OR ! Repeat PAP in 1 year and if NILM, routine screening ! ASCUS, HPV Neg ! 21-24: Routine screening ! > 25: PAP and HPV in 3 years " HPV " If Referral Guidelines for Abnormal Paps repeat PAP abnormal or HPV pos, colpo ! ASCUS, HPV pos or LSIL ! 21-24: PAP in 1 year " If " If ! NILM, ASC or LSIL, repeat PAP in 1 year 2nd repeat PAP > ASC, then colpo > 25: Colpo 3% 9 Referral Guidelines for Abnormal Paps Treatment ! LSIL, HPV Neg: ANY age ! ! PAP and HPV in 1 year " If NILM, HPV neg, repeat PAP and HPV in 3 years " If abnormal PAP or HPV pos, colpo OR Colpo ! ASC-H or HSIL: ANY Age ! ! Colposcopy OR if > 25 and not pregnant, immediate LEEP ! AGC or atypical endocervical cells: ANY age ! ! Colposcopy and ECC +/- EMBx EMBx if > 35 " And < 35 if chronic anovulation or unexplained vaginal bleeding ! Atypical endometrial cells: ANY age ! ! ECC and EMBx Colpo also if both negative Treatment of dysplasia Adolescents ! In general: ! We treat CIN 2+ lesions " CIN 3 – need to treat " CIN 2 – interobserver variability, mix of CIN 1 and CIN 3 " Change in path to simply report Low grade or high grade ! Treatment: Excisional Procedure ! ! ! LEEP: done in clinic Cold Knife Cone (CKC): Done in OR Risks: " Pregnancy implications: 1-3% risk " Cervical Incompetence " Stenosis " Bleeding " Cure: 95% ! Ideally pap never done! ! ASCUS or LSIL ! Repeat in 1 year ! HSIL -> colposcopy ! Surveillance with pap and colpo every 6 months ! Excisional procedure only if HSIL/CIN3 persists for 1 year 4% 10 Key Points Questions ! No PAPS until age 21 ! ASCUS HPV neg = normal PAP ! AGC = bad! ! PAPS every 3 years until age 30 ! Over 30, perform concurrent HPV and PAP q 5 years 5% 11 Contraceptive Card Every Woman, Every Time Contraceptive Options Method Implant (Nexplanon™) Efficacy* The Good >99% 3 years Safe while breastfeeding Progesterone only The Bad Irregular bleeding Irregular Progestin IUD >99% Mirena™ 5 years, Skyla™ 3 years Treatment for menorrhagia bleeding (Mirena™, May cause amenorrhea Skyla™) Safe while breastfeeding Progesterone only Safe in nulliparous and adolescents Cramping and Copper IUD >99% Lasts up to 10 years Safe while breastfeeding heavier (Paragard™) Hormone free periods Safe in nulliparous and adolescents Emergency contraception – place within 5 days of unprotected sex Irregular bleeding Injection 94% Each shot lasts 12 weeks Safe while breastfeeding Decreased bone (Depo-Provera™) Progesterone only density Ring 91% Can make periods more regular Weight gain Vaginal discharge and Must remember less painful monthly One ring lasts up to 4 weeks Skin irritation 91% Can make periods more regular Patch and Must remember (Ortho Evra™) less painful weekly One patch lasts 1 week Combination Pill 91% Can make periods more regular and Must remember (Estrogen + less painful daily Progestin) *Efficacy'Percentages'by'the'CDC'based'on'typical'use'within'the' first'year'of'use' (Nuvaring™) Myth Busters' • • Contra-indications to ESTROGEN containing birth control (OCPs, Nuvaring and patch). Ok to use progesterone only forms. – Smoker > 35 years of age – History of VTE – Lupus with Antiphospholipid Antibodies – Poorly controlled HTN – HTN with vascular disease > 35 years of age – Diabetes with end organ disease – Migraines with aura at any age – HPL: TG > 250 or LDL > 160 – CAD, CHF or cerebrovascular disease – May decrease lactation if not well established Antibiotics, to include Doxycycline, does not effect the efficacy of birth control – Rifampin does decrease the steroid level in women taking combination oral contraceptives • Additional Benefits of combination oral contraceptives: Decreases blood flow and pain with menses Improves acne Decreases hirsutism Decreases the risk of ovarian cancer (beneficial in BRCA carriers) – Cycle control and uterine protection in PCOS – – – – • IUDs: – Can place at time of STI screening, and if positive, treat infection with IUD in place – Do not place if concern for active infection – Safe to place in nulliparous and adolescent patients – Is NOT associated with infertility or PID – Can safely perform colposcopy, LEEP, and endometrial biopsy with IUD in place Only condoms protect against sexually transmitted infections 12 Recruitment Flyer for the Contraception Study 28 May 2013 Dear Providers, In the past few months, the military has received poor publicity due to the military’s high rate of unintended pregnancies despite a soldier’s free access to health care. In light of these recent publications and the known 50% rate of unintended pregnancies in the United States, we, the military gynecologists, are hoping to improve this with the help of our primary care providers. We will be conducting a study to try and assess if women are being asked and offered contraception regularly at visits. It is our belief that every woman should be on contraception if not actively trying to conceive. So, at each visit, every woman should be asked about contraception and offered birth control if interested, hence our slogan, “Every Woman, every time!.” I will be performing a random chart review to see if women are being asked about birth control and if not using anything, offered. I will then be asking you, our primary care providers, to complete a pre-test on your knowledge about current contraceptives and their uses. Following this test, each provider will be given a “contraception card” with basic information about contraceptive options along with their indications/contraindications. A month later we will conduct a post-test followed by a repeat chart review to see if there has been improvement in our contraceptive counseling. Your participation will be completely voluntary and anonymous. Regardless of your choice to participate in the pre and post-test, we will share our cards and information. This is not a test of your knowledge, rather a conglomerate assessment of how well our primary care providers are trained in contraceptive counseling. I do hope you will be honest in your answers. I do believe that military women have access to great medical care. Military providers are the leaders in trauma and battle-field medicine. We want to do our part to assure that women’s health issues are being addressed as well. Please do not hesitate to contact me if you have any questions or concerns. Sincerely, Erin A. Keyser, MD, FACOG MAJ, MC, USA Staff OB/GYN Department of Women’s Health William Beaumont Army Medical Center 13 Post-Test Script for Recruitment Thank you to all of those that participated in the pre-test of my contraception study. Today I am recruiting you to participate in the post-test. I want to again reiterate that your participation will be completely voluntary and anonymous. There will be no identifiable data collected. This is not a test of your knowledge, rather a conglomerate assessment of how well our primary care providers are trained in contraceptive counseling. I do hope you will be honest in your answers. Thank you again for your help. 14 The Pre/Post Test that was Given to Providers 1. The rate of unintended pregnancies in the US is: a. 10% b. 25% c. 50% d. 75% 2. Typical use of birth control pills make the pills effective a. 80% of the time b. 90% of the time c. 95% of the time d. 99% of the time 3. True or False: IUDs are as effective as permanent sterilization at preventing pregnancy 4. True or False: Nulliparous and adolescent women can be offered IUDs 5. True or False: There is evidence to suggest that IUDs are associated with higher rates of PID and infertility. 6. True or False: Colposcopy, LEEP and endometrial biopsies cannot be performed with IUDs in place 7. True or False: Routine screening for gonorrhea and Chlamydia is required prior to placement of IUD 8. True or False: An IUD must be removed if there is a positive Gonorrhea or Chlamydia test 9. True or False: The copper IUD can be used as post-coital contraception up to 5 days after unprotected intercourse 10. True or False: Long acting reversible contraceptive methods have few contraindications and almost all women are eligible for Implants or IUDs 11. Circle the absolute contraindications to estrogen containing contraceptives: circle all that apply a. Smoking > 35 yrs of age b. Smoking > 1ppd at any age c. History of venous thromboembolism d. Lupus e. Lupus with antiphospholipid antibodies f. Well established breastfeeding mothers g. Well controlled hypertension h. Poorly controlled hypertension i. Diabetes < age 35 j. Diabetes with retinopathy or end organ disease k. Migraine headaches l. Migraine headaches with aura m. TG > 250 or LDL > 160 n. Women with CAD, CHF or Cerebrovascular disease 12. True or False: Doxycycline effects the efficacy of birth control pills 15 NEW Pap Smear Guidelines ASCCP 2012 GUIDELINES AND ASCCP 2013 ALGORITHMS ERIN A. KEYSER, MD, FACOG MAJ, MC, USA DEPT OF WOMEN’S HEALTH WILLIAM BEAUMONT ARMY MEDICAL CENTER Abbreviations NILM: Negative for intraepithelial lesion and malignancy ASCUS: Atypical squamous cells of undetermined significance LSIL: Low-grade squamous intraepithelial lesion HSIL: High-grade squamous intraepithelial lesion ASC-H: Atypical squamous cells, cannot rule our high-grade lesion AGC: Atypical glandular cells Used to be AGUS Cervical Cancer In US, about 12,000 cases of cervical cancer/year -> 4,000 deaths/year 50% never screened 10%, not screened in last 5 years Mean age: 48 years Worldwide: major health problem 530,000 cases per year worldwide -> 230,000 deaths/year Mortality: 52% On average, severe dysplasia takes 3-7 years to progress to invasive cervical cancer Cervical cancer screening effective! Key to getting cancer: persistent HPV (at 1 and 2 years) Increased likelihood of persistent infection: Smoking, compromised immune system, and HIV Cervical Cancer and HPV Oncogenic HPV causes cervical cancer Among 40 types of HPV, 15 are oncogenic HPV 16 highest carcinogenic potential 55-60% of all cases of cervical cancer worldwide HPV infection 75-80% of sexually active adults will acquire HPV Most common in teenagers and women in early 20’s 85-90% will clear infection in an average of 8 months (8-24 months) CIN 1 usually reflects acute HPV and most will regress When to screen As of 2012 Pap smear screening should begin at age 21, regardless of age of sexual initiation. Based on low incidence of cancer (0.1% of cases of cervical cancer) Lack of data that screening is effective in this age group Overtreatment Increasing rates of PTB Anxiety Only exception: HIV infected patient Type of pap smear screening Liquid based allows you to concurrently test HPV and other tests Same sensitivity/specificity as conventional cervical cytology screening 2012 Recommended Screening < 21: None 21-29: PAP every 3 years (NO HPV) 30-65: PAP and HPV every 5 years (or PAP every 3 years) > 65: None (following adequate negative prior screening*) After Hysterectomy: None (without cervix and without Hx of CIN 2 or greater) * 3 consecutive negative cytology results or 2 consecutive negative co-tests within 10 years prior to cessation of screening, with the most recent within 5 years. HPV Testing HPV screening: 15-18 potentially cancer causing “high risk” HPV genotypes Additional HPV DNA Genotype that can test specifically for 16 or 18 Two indications for HPV testing Reflex Testing – following ASCUS PAP ALTS Trial, 2002 Co-Testing in women 30-65 yrs of age Co-Testing q 5 years 3 RCTs: More effective at detecting high grade dysplasia and adenocarcinoma which is often missed by cytology alone Lower cancer rates Fewer follow up colposcopy Ordered in CHCS 1 or ahlta: Labs -> HPV -> digene brush Special circumstances HIV patients: Twice in the first year of diagnosis, then annually Immunosuppressed: Annually DES in utero: Annually s/p HPV vaccination: No change, follow age based screening recommendations What do the results mean? Risks of cervical neoplasia with abnormal cervical cytology: Incidence (percent) Cervical Cytology CIN 2+ CIN 3+ Cervical cancer Negative 0.68 0.26 0.025 ASCUS, HPV pos 18 6.8 0.41 ASCUS, HPV neg 1.1 0.43 0 LSIL 16 5.2 0.16 ASC-H 35 18 2.6 HSIL 69 47 7.3 AGC 13 8.5 2.7 What to do with the results Referral Guidelines for Abnormal Paps Unsatisfactory: Repeat PAP in 2-4 months OR if > 30 and HPV pos may colpo NILM, EC/TZ insufficient: 21-29: routine screening, assume negative > 30: HPV Neg: Routine screening HPV Pos: repeat PAP and HPV in 1 year Or HPV genotype 16/18, and if pos, colpo now HPV ?: HPV testing or repeat PAP in 3 years NILM and HPV Pos: > 30 HPV genotype for 16/18 and if pos, colpo now OR Repeat PAP and HPV in 1 year If repeat PAP abnormal or HPV pos, colpo Referral Guidelines for Abnormal Paps ASCUS, HPV unknown: Any age HPV Testing OR Repeat PAP in 1 year and if NILM, routine screening ASCUS, HPV Neg 21-24: Routine screening > 25: PAP and HPV in 3 years ASCUS, HPV pos or LSIL 21-24: PAP in 1 year If NILM, ASC or LSIL, repeat PAP in 1 year If 2nd repeat PAP > ASC, then colpo > 25: Colpo Referral Guidelines for Abnormal Paps LSIL, HPV Neg: ANY age PAP and HPV in 1 year If NILM, HPV neg, repeat PAP and HPV in 3 years If abnormal PAP or HPV pos, colpo OR Colpo ASC-H or HSIL: ANY Age Colposcopy OR if > 25 and not pregnant, immediate LEEP AGC or atypical endocervical cells: ANY age Colposcopy and ECC +/- EMBx EMBx if > 35 And < 35 if chronic anovulation or unexplained vaginal bleeding Atypical endometrial cells: ANY age ECC and EMBx Colpo also if both negative Treatment Treatment of dysplasia In general: We treat CIN 2+ lesions CIN 3 – need to treat CIN 2 – interobserver variability, mix of CIN 1 and CIN 3 Change in path to simply report Low grade or high grade Treatment: Excisional Procedure LEEP: done in clinic Cold Knife Cone (CKC): Done in OR Risks: Pregnancy implications: 1-3% risk Cervical Incompetence Stenosis Bleeding Cure: 95% Adolescents Ideally pap never done! ASCUS or LSIL Repeat in 1 year HSIL -> colposcopy Surveillance with pap and colpo every 6 months Excisional procedure only if HSIL/CIN3 persists for 1 year Key Points No PAPS until age 21 ASCUS HPV neg = normal PAP AGC = bad! PAPS every 3 years until age 30 Over 30, perform concurrent HPV and PAP q 5 years Questions