USDA Avian Influenza Virus Diagnostic Workshop
Iowa State University, Ames, Iowa
Molecular Diagnostics Laboratory
Real-time RT-PCR
Introduction
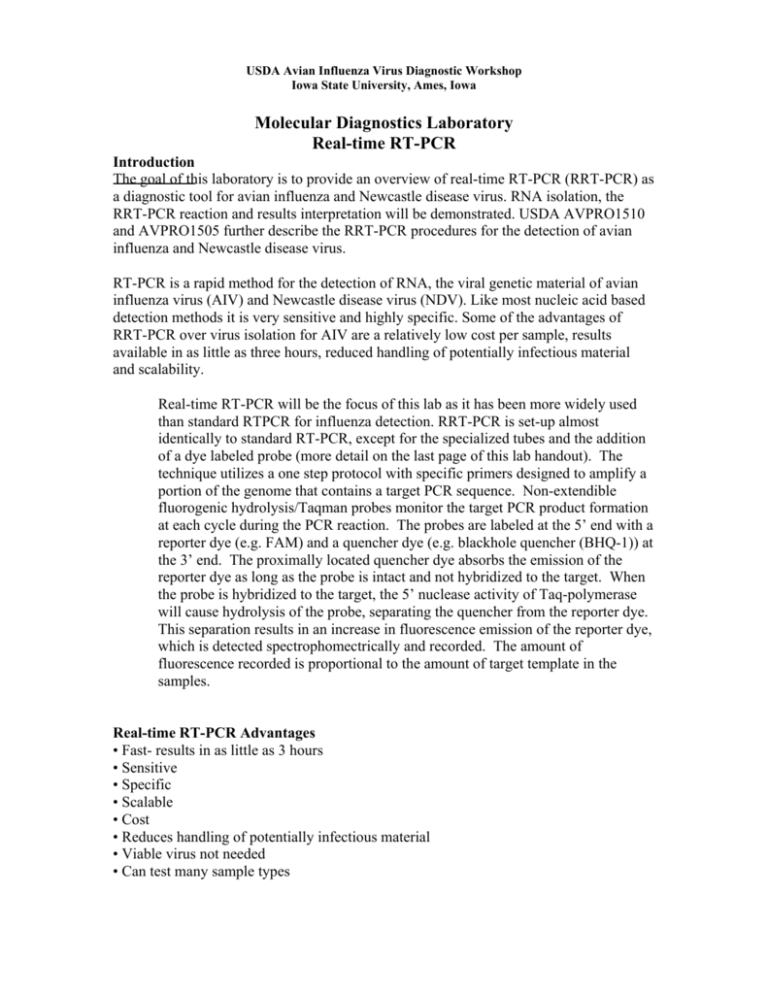
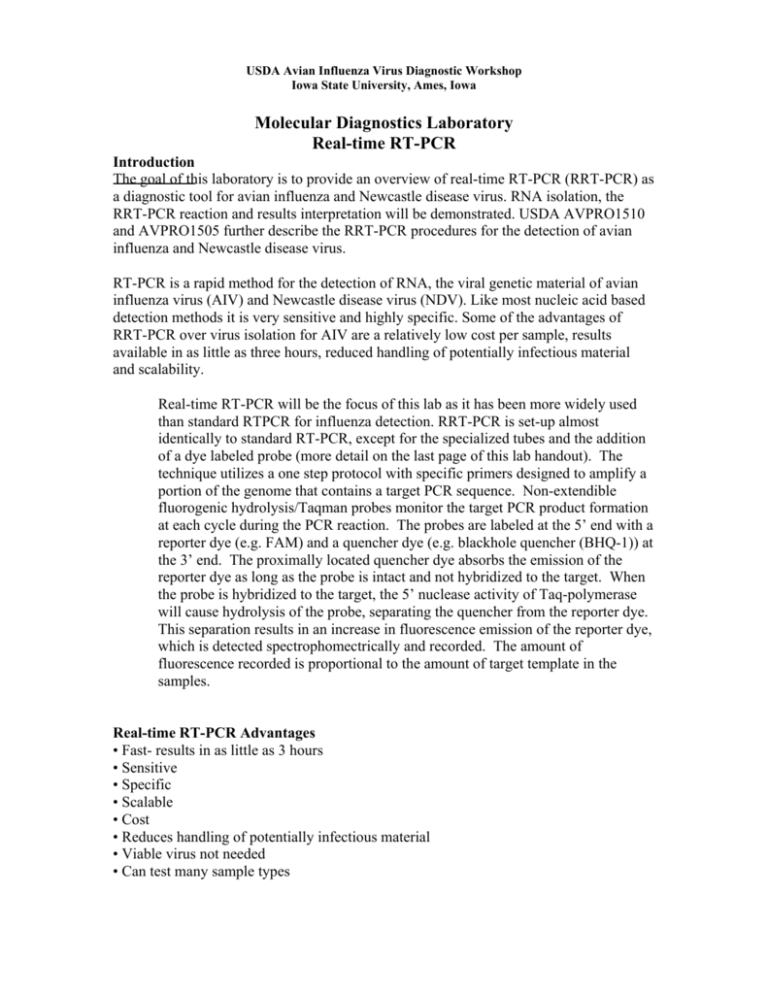
The goal of this laboratory is to provide an overview of real-time RT-PCR (RRT-PCR) as
a diagnostic tool for avian influenza and Newcastle disease virus. RNA isolation, the
RRT-PCR reaction and results interpretation will be demonstrated. USDA AVPRO1510
and AVPRO1505 further describe the RRT-PCR procedures for the detection of avian
influenza and Newcastle disease virus.
RT-PCR is a rapid method for the detection of RNA, the viral genetic material of avian
influenza virus (AIV) and Newcastle disease virus (NDV). Like most nucleic acid based
detection methods it is very sensitive and highly specific. Some of the advantages of
RRT-PCR over virus isolation for AIV are a relatively low cost per sample, results
available in as little as three hours, reduced handling of potentially infectious material
and scalability.
Real-time RT-PCR will be the focus of this lab as it has been more widely used
than standard RTPCR for influenza detection. RRT-PCR is set-up almost
identically to standard RT-PCR, except for the specialized tubes and the addition
of a dye labeled probe (more detail on the last page of this lab handout). The
technique utilizes a one step protocol with specific primers designed to amplify a
portion of the genome that contains a target PCR sequence. Non-extendible
fluorogenic hydrolysis/Taqman probes monitor the target PCR product formation
at each cycle during the PCR reaction. The probes are labeled at the 5’ end with a
reporter dye (e.g. FAM) and a quencher dye (e.g. blackhole quencher (BHQ-1)) at
the 3’ end. The proximally located quencher dye absorbs the emission of the
reporter dye as long as the probe is intact and not hybridized to the target. When
the probe is hybridized to the target, the 5’ nuclease activity of Taq-polymerase
will cause hydrolysis of the probe, separating the quencher from the reporter dye.
This separation results in an increase in fluorescence emission of the reporter dye,
which is detected spectrophomectrically and recorded. The amount of
fluorescence recorded is proportional to the amount of target template in the
samples.
Real-time RT-PCR Advantages
• Fast- results in as little as 3 hours
• Sensitive
• Specific
• Scalable
• Cost
• Reduces handling of potentially infectious material
• Viable virus not needed
• Can test many sample types
Real-time RT-PCR disadvantages
• Expensive initial investment (equipment)
• Probes must be stored and handled correctly
• False positives
Cross contamination
Cross reactions/non-specific detection
• False negatives
Inhibitory substances in the sample
Template modification/ degradation: RNA fragile
During this laboratory we will extract RNA with a silicon-nucleic acid binding column
(Qiagen RNeasy kit) and will be performing the RRT-PCR test for the avian influenza
virus Matrix gene. The procedures for the avian influenza and Newcastle disease virus
are similar, except for the primers and probes used and the temperature cycling
conditions used. Specifics of each test are provided in the detailed protocols in your note
book.
For laboratories interested in standard RT-PCR, it is recommended that the primers used
with realtime RT-PCR test not be used due to the small product size. A procedure for a
standard RT-PCR for avian influenza has been reported by Fouchier, et al. (Fouchier, R.
A., T. M. Bestebroer, S. Herfst, L. Van Der Kemp, G. F. Rimmelzwaan and A. D.
Osterhaus. Detection of influenza A viruses from different species by PCR amplification
of conserved sequences in the matrix gene. J Clin Microbiol 38:4096-101. 2000.) A copy
of which is provided in your notebook.
RNA Extraction
• Isolates RNA from other materials in the sample
• Concentrates the RNA (5-10 times)
• Removes inhibitory substances
• Removes substances that will degrade the RNA
Each student will extract RNA from 2 samples and will with the other members of their
group set-up and run RRT-PCR reactions for AIV matrix or H5.
Materials needed
• 2 test samples for each person (4-5 lab members per group)
• 1.5ml microfuge tubes
• Pipets and tips
• 2 RNeasy columns per person
• Vacuum manifold and tubing
• RNeasy Kit components
– RLT
– RPE buffer with ethanol added
– RW1 buffer
– Nuclease free water (elution buffer)
Notes:
• All Procedures should be carried out in a biological safety cabinet or other primary
containment device.
• Kit supplied buffers should be prepared as specified in the kit instructions (i.e. 10μl per
1ml of 2-mercapto-ethanol should be added to the RLT buffer immediately prior to use).
• Wear gloves at all times during this procedure.
RNA Extraction with Qiagen RNeasy Kit- QiaVac 24 Vacuum Manifold Method
Procedure:
1. Each participant will start with two 1.5 ml centrifuge tube
which will contain 500 µl of swab specimen.
2. Add to each microfuge tube from step 1
500μl RLT buffer
Steps 1 - 5
in a 1.5ml tube
3. Vortex 15 sec. and pulse centrifuge.
4. Add 500μl 70% ethanol to the lysed swab specimen.
Vortex for 15 sec. Centrifuge for 5 minutes at 5000 Xg at RT.
5. Set-up the vacuum manifold: place the appropriate
number of RNeasy columns in the luer locks of the vacuum
manifold, cover any empty positions with the luer caps
supplied with the vacuum manifold.
6. Apply vacuum and add the entire sample/RLT/ethanol
mixture to an RNeasy column for each sample. Press
down on the top of the manifold once the vacuum is on to
seal the manifold, then open the lids of all the columns and
keep them open at all times. The vacuum should not be
turned off until after the final wash.
Step 6 -8 - turn
on vacuum and
add sample to
column and
wash
Steps 9-10 put
column in tube
and centrifuge to
dry
7. Wash by applying 700μl RW1 buffer to each column.
8. Wash again by applying 500μl RPE buffer to the column
and repeat for a total of 2 washes with buffer RPE.
9. Shut off the vacuum and place each RNeasy column in
a 2ml collection tube.
10. Centrifuge the column and collection tube for 2 minutes
at ~14 KXg and discard the collection tube.
11. Place the column in an elution tube (or 1.5ml microfuge
tube)
Steps 11-13
place in elution
tube, add water
and elute RNA
by centrifugation
12. Add 50μl nuclease free water to the column and incubate at room temperature 1
minute.
13. Elute RNA by centrifuging for 1 minute at ~14KXg. Store at -70°C long term.
Real-time RT-PCR
• RT- reverse transcription
o cDNA is made from the viral RNA
Adds time to test
• PCR- polymerase chain reaction
o cDNA is amplified
o DNA is more stable and more easily amplified than RNA
• Real-time
o Increases in the amount of DNA produced are detected as they occur
Each lab-group will need:
– Smart Cycler tube cooling block
– Smart Cycler tubes
– A set of RT-PCR reagents
• Enzyme and RNase inhibitor in a bench top cooler
• 5X buffer
• dNTPS
• Positive control (AIV M or H5 transcribed RNA positive control)
• Nuclease free water
• Forward primer (Matrix or H5)
• Reverse primer (Matrix or H5)
• Probe (Matrix or H5)
– RNA samples
– Pipets and aerosol resistant pipet tips
– 1.5ml tubes
Real-time RT-PCR for type A Influenza (MA gene) Procedure:
• Wear gloves at all times during this procedure.
• This should be performed in a biological safety cabinet or similar device
The Smart Cycler has already been programmed to run the sample with the conditions
given in tables 1 and 2.
RT Step
Table 1. RT step thermocycling for Qiagen one-step RT-PCR Kit.
1 cycle
30 min.
50 C
15 min.
95 C
Table 2. Thermocycling conditions for gene specific probe and primer sets.
Probe/Primer set
Step
Time
Temp
Type A influenza
45 cycles
denaturation 1 sec.
94 C
(MA gene)
Annealing*
20 sec.
60 C
Subtype H5 (HA gene)
40 cycles
Denaturation 1 sec.
Annealing*
20 sec.
Extension
5 sec.
*Note: The fluorescence is acquired at the annealing step.
94 C
57 C
72 C
1. In a new, clean 1.5 ml tube prepare the reaction master mix (everything but the
template) as shown in table. 3. Add the enzyme and probe last.
Step 1 Notes:
• The probe is light sensitive and when working in a biological safely cabinet the light
should be turned off when the probe is added to the master mix and should remain off
until the samples are placed in the Smart Cycler instrument.
• The quantity of reagents needed for master mix is described below for 4 and 5 person
group. Be sure to prepare master mix using the protocol designed for your group size.
As a rule, make one extra reactions worth of master mix for every 10 reactions to ensure
you will have enough. For example: for 5 reactions, prepare master mix for 6, for 15
reactions prepare master mix .2for 17, for 25 reactions prepare master mix for 28, and so
on.
Table3. Real-time RT-PCR reaction mix volumes and conditions for type A
influenza (MA gene).
Master mix
for 5 person
group
97.3
70.0
17.5
14.0
7.0
7.0
11.2
Volume Per
Reaction
H2O
5X
25mM MgCl2
Enzyme Mix
Forward Primer
Reverse Primer
dNTP’s
Master mix
for 4 person
group
83.4 μl
60.0
15.0
12.0
6.0
6.0
9.6
Probe
Rnase Inhibitor
MM per rxn
Template
Total
6.0
6.0
17
8
25
7.0
7.0
17
8
25
0.5
0.5
Component
6.95μl
5
1.25
1
0.5
0.5
0.8
Final
Concentration
1X
3.75 mM
10 pmol
10 pmol
320 μM ea.
dNTP
0.15 μM
13 units
2. Mix by vortexing for 3-5 seconds and centrifuge briefly.
3. Add 17μl of the master mix to each of your Smart Cycler tubes (add the mix to the
bottom of the cup at the top of the reaction tube).
4. Add 8μl of template to the Smart Cycler tubes, close and label each tube.
Step 4 notes:
• The template for the positive controls is in vitro transcribed RNA from the target gene
• The template for the negative controls is nuclease free water.
5. Centrifuge the reaction tubes briefly in the Smart Cycler centrifuge.
6. Place the reaction tubes into the Smart Cycler and run with assay specific
program.
III. ANALYSIS OF RESULTS
On the Smart Cycler the default minimum increase in fluorescence for a sample to be
classified as positive by the software is 30 units. Because this is an arbitrary threshold,
any samples which have an increase in fluorescence between 20 and 40 should be
considered suspect and should be retested.
Any questionable samples should be re-tested. If results of the second test are
unsatisfactory additional sampling from the flock or premises should be considered if
possible.
Determining the results
• Check the controls
• Check each sample
• Record the cycle threshold (Ct) values
– If a sample has no cycle threshold values (0.00) it is negative
• Determine if there are any suspect samples
– Weak positives- Ct values >35
Suspect samples
• For AIV or NDV a farm or premise is never considered positive based on one positive
RTPCR
result
– Epidemiology- dangerous contact
– Clinical condition
– Other positive diagnostic test
• Directigen (AIV)
• Virus isolation
• A second RT-PCR test for a different target
– AIV subtype specific
– NDV- vNDV or vaccine virus specific
• Are other samples from the same farm positive?
• Are there enough samples from the farm?
• Were the controls valid?
Real-time PCR Basics
The general principle of real-time PCR is the same as standard PCR; however the
reaction product can be monitored in real-time with a fluorogenic probe. There are
several types of detection systems for real-time PCR: hydrolysis probes, hybridization
probes, molecular beacons and double stranded DNA binding dyes, among others. This
assay utilizes hydrolysis probes.
In the hydrolysis probe system, a DNA probe which binds the PCR product is added to
the PCR reaction. The DNA probe has a fluorogenic reporter dye on one end and a
quencher dye on the other end (figure 1). As the target PCR product increases the probe
binds the amplicons and reporter dye is cleaved from the 5’ end of the probe by taq
polymerase (due to 5’ exonuclease activity). As the reporter is cleaved from more and
more probe molecules the fluorescence signal from the reaction increases. The
fluorescence signal is monitored every cycle, revealing increases in the PCR product as it
occurs.
Additional information about Real-time PCR, primers and probes can be found at
www.operon.com and www.idtdna.com.
Figure 1. Hydrolysis probe mechanism. a. The probe ( ) binds the PCR product ( )
during amplification. b. The polymerase ( ) runs into the probe during synthesis of the
PCR product. c. Taq polymerase cleaves the reporter dye from the probe, increasing the
detectable
JOURNAL OF CLINICAL MICROBIOLOGY, Nov. 2000, p. 4096–4101
0095-1137/00/$04.00⫹0
Copyright © 2000, American Society for Microbiology. All Rights Reserved.
Vol. 38, No. 11
Detection of Influenza A Viruses from Different Species by PCR
Amplification of Conserved Sequences in the Matrix Gene
RON A. M. FOUCHIER,* THEO M. BESTEBROER, SANDER HERFST, LIANE VAN DER KEMP,
GUUS F. RIMMELZWAAN, AND ALBERT D. M. E. OSTERHAUS
National Influenza Center and Department of Virology, Erasmus University, Rotterdam, The Netherlands
Received 11 May 2000/Returned for modification 27 July 2000/Accepted 5 September 2000
The recently raised awareness of the threat of a new influenza pandemic has stimulated interest in the
detection of influenza A viruses in human as well as animal secretions. Virus isolation alone is unsatisfactory
for this purpose because of its inherent limited sensitivity and the lack of host cells that are universally
permissive to all influenza A viruses. Previously described PCR methods are more sensitive but are targeted
predominantly at virus strains currently circulating in humans, since the sequences of the primer sets display
considerable numbers of mismatches to the sequences of animal influenza A viruses. Therefore, a new set of
primers, based on highly conserved regions of the matrix gene, was designed for single-tube reverse transcription-PCR for the detection of influenza A viruses from multiple species. This PCR proved to be fully reactive
with a panel of 25 genetically diverse virus isolates that were obtained from birds, humans, pigs, horses, and
seals and that included all known subtypes of influenza A virus. It was not reactive with the 11 other RNA
viruses tested. Comparative tests with throat swab samples from humans and fecal and cloacal swab samples
from birds confirmed that the new PCR is faster and up to 100-fold more sensitive than classical virus isolation
procedures.
of phenotypically and genotypically diverse influenza A viruses.
To this end, we have designed a primer set for PCR-based
detection of influenza A viruses that was validated with clinical
specimens and a panel of influenza A virus strains representing
all known HA and NA subtypes obtained from a variety of host
species and from different geographical locations. The efficacy
of this PCR-based screening of samples from avian and human
origin was compared with classical isolation of influenza A
virus in embryonated chicken eggs or mammalian cell culture.
We conclude that this PCR, based on the detection of gene
segment 7 of influenza A virus, is fast, sensitive, and specific
and is suitable for all genetic variants of influenza A virus
known to date.
Migratory birds and waterfowl are thought to serve as the
reservoir for influenza A viruses in nature (24). To date, influenza A viruses representing 15 hemagglutinin (HA) and nine
neuraminidase (NA) subtypes have been detected in wild birds
and poultry throughout the world (19, 24). Since the general
human population is serologically naive with respect to most
avian HA and NA antigens, influenza A viruses of avian origin
pose a threat that is at the basis of new pandemics in humans
(4, 24). For some time it was thought that avian influenza
viruses could be transmitted to humans only through coinfection and genetic reassortment of avian and swine or human
influenza viruses in pigs (4, 13, 22, 24, 25). However, the recent
zoonotic events in Hong Kong and mainland China caused by
H5N1 and H9N2 influenza viruses suggest that avian influenza
viruses can be transmitted directly to humans as well (5, 8–10,
15). The link between human influenza and the avian influenza
virus reservoir has boosted the public health-related and scientific interest in the prevalence, variability, and zoonotic potential of avian influenza viruses.
Although the routine procedures for the detection of human
influenza A viruses described to date, including in vitro virus
isolation, immunofluorescence (IF), and PCR-based assays,
are powerful tools, they may be less effective for the detection
of influenza viruses of avian and porcine origin. The phenotypic and genetic heterogeneities of the latter viruses may
result in a false-negative diagnosis of influenza A virus infection by in vitro cell culture or current protocols for PCR analysis. Importantly, sporadic zoonotic events of influenza A virus
infection may remain undetected as a result of such falsenegative diagnoses.
The aim of this study was to set up a rapid and sensitive PCR
method for the screening of clinical specimens for the presence
MATERIALS AND METHODS
Design of oligonucleotides. PCR primers were designed on the basis of sequence information obtained from the Influenza Sequence Database at Los
Alamos National Laboratories, Los Alamos, N.M. (http://www.flu.lanl.gov). To
identify conserved sequences in the influenza virus gene segments, entropy plots
were created with the Bioedit software package (available through http:
//www.mbio.ncsu.edu/RNaseP/info/programs/BIOEDIT/bioedit.html). Because
the HA and NA genes are genetically diverse and sequence information on the
PA, PB1, and PB2 polymerase genes is limited (less than 100 sequence entries
are available from the database, including partial sequences) only (partial) sequences representing gene segments 5, 7, and 8 encoding nucleoprotein, matrix,
and nonstructural proteins, respectively, were analyzed. The degree of heterogeneity was expressed as entropy as defined by Shannon: H (1) ⫽ ⫺⌺f(b, 1) ln
[f(b, 1)], where H (1) is the uncertainty at position 1, b represents a residue out
of the allowed choices for the sequence in question (A, C, G, T, ⫺), and f(b, 1)
is the frequency at which residue b is found at position 1 (16, 21). Oligonucleotides M52C (5⬘-CTT CTA ACC GAG GTC GAA ACG-3⬘) and M253R
(5⬘-AGG GCA TTT TGG ACA AAG/T CGT CTA-3⬘) were designed for PCR
amplification of influenza A virus matrix gene sequences, and the biotinylated
oligonucleotide Bio-M93C (5⬘-CCG TCA GGC CCC CTC AAA GCC GA-3⬘)
was synthesized for hybridization purposes (Eurogentec, Seraing, Belgium).
Specimens. Cloacal swab specimens were collected from ducks (widgeon
[Mareca penelope], gadwall [Mareca strepera], and mallard [Anas plathyrhynchos])
at a marshaling lake in Lekkerkerk, The Netherlands, and droppings as well as
cloacal swab specimens were collected from geese (greylag goose [Anser anser],
white-fronted goose [Anser albifrons albifrons], barnacle goose [Branta leucopsis],
and brent goose [Branta bernicla]) in Groningen and Eemdijk, The Netherlands,
between 1997 and 1999. Cloacal swab specimens and droppings were collected
from shorebirds at Öland, Sweden, in the spring of 1999. Cotton swabs were used
* Corresponding author. Mailing address: Department of Virology,
Erasmus University Rotterdam, P.O. Box 1738, 3000 DR Rotterdam,
The Netherlands. Phone: 31 10 4088066. Fax: 31 10 4089485. E-mail:
fouchier@viro.fgg.eur.nl.
4096
VOL. 38, 2000
PCR-BASED DETECTION OF INFLUENZA A VIRUSES
for sampling and were subsequently stored in transport medium (23). Throat
swab specimens collected from humans were also stored in transport medium.
The samples were stored at 4°C for a few days, at ⫺20°C for less than a week, or
at ⫺70°C for extended periods of time. Transport medium consisted of Hanks
balanced salt solution supplemented with 10% glycerol, 200 U of penicillin per
ml, 200 g of streptomycin per ml, 100 U of polymyxin B sulfate per ml, 250 g
of gentamicin per ml, and 50 U of nystatin per ml (all from ICN, Zoetermeer,
The Netherlands).
RNA isolation. RNA was isolated with a high pure RNA isolation kit (Roche
Molecular Biochemicals) according to the instructions from the manufacturer,
with minor modifications. A 0.2-ml sample was homogenized by vortexing and
was subsequently lysed with 0.4 ml of lysis-binding buffer to which poly(A)
(Roche Molecular Biochemicals) was added as a carrier to 1 g/ml. After binding
to the column, DNase I digestion, and washing, the RNA was eluted in 50 l of
nuclease-free double-distilled water preheated to 80°C.
PCR. The reverse transcription (RT) and PCRs were optimized with respect to
enzymes, primer sets, and concentrations of reagents as well as cycling parameters. Samples were amplified in a one-step RT-PCR in a final volume of 25 l
containing 50 mM Tris 䡠 HCl (pH 8.5), 50 mM NaCl, 7 mM MgCl2, 2 mM
dithiothreitol, 1 mM each deoxynucleoside triphosphate at a concentration of 1
mM, each oligonucleotide at a concentration of 0.4 M, 2.5 U of recombinant
RNAsin, 10 U of avian myeloblastosis virus reverse transcriptase, 2.5 U of
Ampli-Taq DNA polymerase (all enzymes were from Promega Benelux B.V.,
Leiden, The Netherlands), and 5 l of RNA. Thermocycling was performed in an
MJ PTC-200 apparatus with the following cycling conditions: 30 min at 42°C and
4 min at 95°C once and then 1 min at 95°C, 1 min at 45°C, 3 min at 72°C 40 times.
Each reaction was analyzed by agarose gel electrophoresis and ethidium bromide
staining (10 l/sample), followed by Southern blot hybridization (2) or dot blot
hybridization (5 l/sample).
Dot blot hybridization. Five microliters of each of the PCR products was
incubated for 5 min at room temperature with 45 l of 10 mM Tris 䡠 HCl (pH
8.0), 1 mM EDTA, and 50 l of 1 M NaOH for denaturation. The samples were
transferred to prewetted Hybond N⫹ membranes (Amersham Pharmacia Biotech Benelux, Roosendaal, The Netherlands) with a dot blot apparatus while
applying vacuum. The samples were then treated for 3 min with 0.1 ml of 1 M
Tris 䡠 HCl (pH 8.0), after which vacuum was again applied for 10 s and the
membrane was removed from the apparatus. The blots were washed three times
for 10 min each time with 0.3 M NaCl–30 mM sodium citrate (pH 7), dried, and
stored at 4°C. The blots were prehybridized for 5 min at 55°C in 2⫻ SSPE (0.3
M NaCl, 20 mM NaH2PO4, 2 mM EDTA [pH 7.4]) and 0.1% sodium dodecyl
sulfate (SDS), after which biotinylated oligonucleotide probe Bio-M93C was
added to 2 pmol/ml and hybridization was continued for 45 min at 55°C. The
blots were washed twice for 10 min each time at 55°C with hybridization buffer
and transferred to 2⫻ SSPE with 0.5% SDS, after which streptavidin-peroxidase
(Roche Molecular Biochemicals) was added to 0.125 U/ml and the mixture was
incubated for 45 min at 42°C. The blots were washed for 10 min at 42°C in 2⫻
SSPE–0.5% SDS, 10 min at 42°C in 2⫻ SSPE–0.1% SDS, and 10 min at room
temperature in 2⫻ SSPE, after which the samples were visualized with enhanced
chemiluminescence detection reagents and by exposure to hyperfilm (Amersham
Pharmacia Biotech Benelux) for 5 to 60 s.
Virus isolation and propagation. The influenza A viruses listed in Table 1 have
been described earlier and were kindly provided by R. G. Webster (14, 19). All
of these viruses had been isolated and propagated in the allantoic cavities of
11-day-old embryonated chicken eggs (12). Influenza virus A/Netherlands/18/94
has been described previously (18). Influenza A virus strains not listed in Table
1 were isolated and propagated in Madin-Darby canine kidney (MDCK) cells or
tertiary monkey kidney (tMK) cells derived from cynomolgus macaques (Macaca
fascicularis) (7, 17). Virus stocks were titrated by end point dilution in MDCK or
tMK cells, and the 50% tissue culture infective doses (TCID50s) were calculated
as described previously (17). The HA titers in the virus stocks were determined
with turkey erythrocytes by standard procedures (17). Virus isolates were characterized by hemagglutination inhibition assays with subtype-specific hyperimmune rabbit antisera raised against HA and NA preparations of the virus isolates
listed in Table 1 (20).
Human respiratory syncytial virus (HRSV) was grown in HEp-2 cells, mumps
and measles viruses were grown in Vero cells, human parainfluenza virus (PIV)
types 1 through 4 (PIV-1 through PIV-4) and influenza B virus were grown in
tMK cells, and Sendai virus, simian parainfluenza virus type 5 (SV5), and Newcastle disease virus (NDV) were grown in embryonated chicken eggs. The virus
titers of these stocks typically ranged from 104 to 106 TCID50s/ml.
RESULTS
Design of oligonucleotides for PCR detection of influenza A
viruses. Avian and mammalian influenza A virus nucleotide
sequences available from the influenza sequence database
(http://www.flu.lanl.gov) were compared to the sequences of
previously described primer sets Mx1 and Mx2 (3), Fam1 and
Fam2 (1), and NS486C and NS637R (6, 7) to analyze their
potential for the detection of genetically diverse influenza A
4097
TABLE 1. Virus isolates used for the validation of PCR-based
detection of influenza A virus
Influenza A virus strain
A/Puerto Rico/8/34
A/Fort Monmouth/1/47
A/Swine/Shope/56
A/Duck/Alberta/35/76
A/Singapore/1/57
A/Hong Kong/1/68
A/Equine/Miami/1/63
A/Duck/Ukraine/1/63
A/Duck/Czechoslovakia/1/56
A/Tern/South Africa/61
A/Duck/Hong Kong/205/77
A/Turkey/Massachusetts/65
A/Shearwater/Australia/1/72
A/Equine/Prague/1/56
A/Seal/Massachusetts/1/80
A/Turkey/Ontario/6118/68
A/Turkey/Wisconsin/1/66
A/Chicken/Germany/49
A/Duck/England/1/56
A/Duck/Memphis/546/76
A/Duck/Alberta/60/76
A/Gull/Maryland/704/77
A/Mallard/Gurjev/263/82
A/Duck/Australia/341/83
A/Shearwater/West Australia/2576/79
a
HA
NA
HA Lane no.
subtype subtype titer (Fig. 2)
1
1
1
1
2
3
4
5
6
5
5
6
6
7
7
8
9
10
11
11
12
13
14
15
15
1
384
1
384
1
512
1
768
2
256
2
512
8
256
8
512
6
256
3
256
3
128
a
—
512
5
192
7
1024
7
128
4
128
2
384
7
384
6
256
9
768
5
128
6
256
—
768
8
256
9
512
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
—, NA subtype unknown.
viruses. The variability between the influenza A virus nucleotide sequences and each position in the potential PCR primers
was calculated by using the entropy algorithm available from
the Bioedit software package (16, 21). Although each of the
primer sequences was based on a relatively conserved domain
of gene segments 7 and 8 of influenza A virus, considerable
heterogeneity was observed for each of the oligonucleotide sets
(Fig. 1). The 3⬘ ends of oligonucleotides are of the greatest
importance for the successful amplification by PCR. Of all
three published primer sets (Fig. 1A to F), at least one of the
oligonucleotides displayed considerable numbers of mismatches with the sequences in the database. Since such mismatches may lead to false-negative PCR results, we designed
new primer sets based on segment 7 of influenza A virus, which
is relatively conserved compared to the other segments. Within
the M1 coding sequence of gene segment 7, several regions
(positions 32 to 93, 149 to 204, and 218 to 276) were identified
that are relatively conserved among influenza A virus strains
obtained from a variety of host species and from different
geographical regions. Oligonucleotides M52C (nucleotide positions 32 to 52), M93C (positions 71 to 93), and M253R
(positions 253 to 276) (Fig. 1) were designed on the basis of
these conserved regions of the influenza A virus genome. Although other conserved regions were identified in the NS2
coding sequence of gene segment 8 and the M1 coding sequence of segment 7, we found primers based on these sequences to be less suitable for PCR amplification of selected
influenza A virus strains (data not shown).
Sensitivity and specificity of influenza A virus PCR. RNA
was isolated from 0.2 ml of allantoic fluid containing the influenza A viruses shown in Table 1, and the equivalent of 4 l
of allantoic fluid was used for amplification by PCR with
primer set M52C-M253R. For each of the virus strains tested,
a band of 244 bp was amplified and was easily visualized on a
1% agarose gel stained with ethidium bromide (Fig. 2). Hy-
4098
FOUCHIER ET AL.
J. CLIN. MICROBIOL.
FIG. 1. Entropy plots of oligonucleotide-annealing sites in human and animal influenza A virus sequences available from the influenza virus sequence database. The
sequences recognized by oligonucleotides Mx1, Fam1, NS486C, Mx2, Fam2, NS637R, M52C, M253R, and M93C were compared to all available influenza A virus
sequences (n ⫽ 189, 189, 234, 203, 204, 249, 175, 215, and 189, respectively), and their heterogeneities are displayed in panels A through I, respectively. Oligonucleotide
positions are given in the 5⬘ to 3⬘ direction, with position 1 being the extreme 5⬘ nucleotide. Asterisks indicate primer positions with degeneracy in the designed
oligonucleotides. Oligonucleotides M52C, M253R, and M93C were designed in the present study.
bridization of dot blots with the internal biotinylated oligonucleotide probe M93C also resulted in clear signals for each of
the influenza A virus strains tested.
We next compared the sensitivity of this PCR with virus
propagation in cell cultures. A stock of influenza virus A/Netherlands/18/94 (H3N2) was generated in tMK cells. This virus
stock contained 107 TCID50s of influenza A virus per ml of
culture supernatant, as determined with tMK and MDCK cells
(17). Serial 10-fold dilutions of virus were made in transport
medium, and RNA was isolated for use in PCR analysis, agarose gel electrophoresis, or dot blot hybridization. The expected DNA fragment of 244 bp was visible on an agarose gel
stained with ethidium bromide when the RNA equivalent of
0.2 TCID50 of influenza A virus was used as input in the PCR
(Fig. 3, lane 8). By using dot blots and hybridization, 0.02
TCID50 of influenza A virus was found to be the detection limit
of the assay (Fig. 3, lane 9, and data not shown). Similar results
were obtained with a second influenza A virus isolate, and such
FIG. 2. PCR analysis of the influenza A viruses, listed in Table 1, which
originated from different hosts and geographical locations. RNA was isolated
from influenza A viruses grown in embryonated chicken eggs, followed by PCR
analysis and agarose gel electrophoresis (top panels) or dot blot analysis (bottom
panels). Lanes 1 to 25, see Table 1; lane 26, negative control.
results were found to be reproducible (data not shown). These
data indicate that our PCR procedure is up to 100-fold more
sensitive than virus propagation in MDCK and tMK cells.
To test the specificities of our PCR primers, RNA was isolated from stocks of a number of RNA viruses, followed by
PCR amplification and gel electrophoresis or dot blot hybridization. RNA was isolated from 0.2 ml of virus stocks containing either influenza B virus, HRSV, PIV-1 through PIV-4,
simian parainfluenza virus type 5 (SV5), NDV, mumps virus,
measles virus, or Sendai virus. One-tenth of the RNA, representing the equivalent of 20 l of virus stock ranging in titer
from 104 to 106 TCID50s/ml, was used for PCR. Upon agarose
gel electrophoresis, weak bands and smears of bands ranging
from 150 to 400 bp in length were observed after PCR amplification of some of the virus samples (PIV-1, -2, and -3, NDV,
mumps virus, and influenza B virus), presumably as a result of
nonspecific amplification of the high levels of viral RNA
present in these samples. However, upon hybridization of dot
blots with the biotinylated oligonucleotide M93C, all RNA
FIG. 3. Sensitivity of detection of influenza A virus RNA by PCR. RNA was
isolated from 0.2 ml of 10-fold serial dilutions of influenza virus A/Netherlands/
18/94 (107 TCID50s/ml) and was used for PCR analysis followed by agarose gel
electrophoresis and ethidium bromide staining (top panel) or dot blot analysis
(bottom panel). Lane 1, negative control; lanes 2 to 9, dilution series representing the equivalent of 2 ⫻ 105 to 0.02 TCID50s per sample. Samples containing
less than 0.02 TCID50 were negative by PCR and dot blot analysis (data not
shown).
VOL. 38, 2000
PCR-BASED DETECTION OF INFLUENZA A VIRUSES
4099
FIG. 4. Specificity of detection of influenza A virus RNA by PCR. RNA was
isolated from virus stocks and was used for PCR analysis and subsequent agarose
gel electrophoresis (top panel) or dot blot hybridization (bottom panel). Lanes:
1, HRSV; 2, PIV-1; 3, PIV-2; 4, PIV-3; 5, PIV-4; 6, Sendai virus; 7, SV5; 8, NDV;
9, mumps virus; 10, measles virus; 11, influenza B virus; 12, influenza A virus.
virus samples except for that with influenza A virus were negative (Fig. 4).
Detection of influenza A virus in human throat swab samples. Throat swab samples sent to the virus diagnostic laboratory at Erasmus University Medical Center are routinely tested
for the presence of influenza A virus by direct IF (DIF) and
inoculation in MDCK or tMK cell cultures in combination with
IF (7). For a selection of influenza A virus-positive throat swab
samples obtained in the 1994-1995 influenza season, influenza
A virus titers were determined by end point dilution and inoculation of tMK cells. A selection of influenza A virus-positive (n ⫽ 13) and influenza A virus-negative (n ⫽ 26) samples
was coded and tested blindly by PCR and dot blot hybridization. All influenza A virus-positive samples, with titers ranging
from 0 to 105.75 TCID50s per ml of throat swab sample, were
positive upon agarose gel electrophoresis and dot blot hybridization (Fig. 5). One of the influenza A virus PCR-positive
samples (lane 6) tested negative upon inoculation of mammalian cell cultures (hence, 0 TCID50). This sample had been
found to be influenza A virus positive by DIF with the cells
present in the throat swab sample (7), but no virus could be
isolated. Of 26 negative control samples (13 were influenza B
FIG. 5. PCR-based detection of influenza A virus in 39 human throat swab
samples. Throat swab samples that were tested previously for the presence of
influenza A virus by classical screening methods (7) were randomized and tested
blindly by PCR. RNA was isolated from 0.2 ml of a throat swab sample and was
used for PCR and dot blot analysis. Lanes 1, 4, 7, 8, 13, 16, 18, 23, 24, 30, 34, 35,
and 38, influenza virus-negative samples; lanes 2, 5, 9, 10, 12, 14, 15, 20, 21, 22,
25, 29, and 31, influenza B virus-positive samples; lane 40, 10 TCID50s of
influenza virus A/Netherlands/18/94 as a positive control; lanes 3, 6, 11, 17, 19,
26, 27, 28, 32, 33, 36, 37, and 39, influenza A virus-positive samples in which virus
titers determined in MDCK cells were 105.75, 0, 103.5, 102.25, 100.75, 104.25, 100.75,
103.75, 104.25, 105.25, 104.5, 105.75, and 103.5 TCID50s/ml respectively.
FIG. 6. PCR-based detection of influenza A virus in a representative set of
avian cloacal swab and dropping samples. RNA was isolated from 0.2 ml of 38
pooled samples, each consisting of five individual bird samples, and was used for
PCR and Southern blot analysis. Lanes 1, 11, 21, 31, and 41, positive controls
representing 10 TCID50s of influenza virus A/Netherlands/18/94; lanes 7, 14, 20,
27, 34, 40, and 47, negative controls; lanes 2 to 5, duck cloacal swab samples;
lanes 6, 8 to 10, 12, 13, 15 to 19, 22 to 26, and 28 to 30, goose dropping samples;
lanes 32, 33, 35 to 39, 42 to 46, and 48 to 50, goose cloacal swab samples. Each
of the pools represented in lanes 13, 15, 23, 30, 36, 39, 43, and 44 was found to
contain a single positive individual bird sample. Virus was isolated in embryonated chicken eggs from samples represented in lanes 13, 15, 23, 30, 39, and 43
but not from those represented in lanes 35, 36, and 44.
virus positive and 13 were influenza A and B virus negative in
mammalian cell cultures), 24 were negative upon PCR and dot
blot analyses. Two of the swabs were negative for influenza A
virus in mammalian cell culture and by IF but yielded very
weak signals after PCR and dot blot hybridization (lanes 9 and
30). These weak dot blot signals may be due to background
hybridization or the presence of very small amounts of influenza A virus RNA in the throat swabs.
Detection of influenza A virus in bird samples. We next
tested the suitability of the PCR for avian influenza A virus
screening of cloacal swab and dropping samples from ducks,
geese, and shorebirds collected in The Netherlands and Sweden. Because PCR screening appeared to be up to 100-fold
more sensitive than virus isolation (see above) and to reduce
cost and workload, the numbers of RNA isolations and PCR
analyses were reduced by making pools of five samples each
(40 l per sample). Between each five pooled samples, a negative control consisting of transport medium was inserted to
check for contamination during processing of the samples.
Among the 235 pools of samples representing 1,175 individual
specimens, RNA isolation, PCR, and Southern or dot blot
hybridization revealed the presence of influenza A virus in 19
of them (the results of the analysis of 38 of these pools is shown
in Fig. 6). RNA was then isolated from each of the individual
samples present in these 19 pools, revealing that all except 1
pool contained a single positive bird sample; the one exception
contained two positive samples.
Each of the 20 positive individual samples was used to in-
4100
FOUCHIER ET AL.
oculate two to four embryonated chicken eggs from which the
allantoic fluids were collected, pooled, and inoculated a second
time in duplicate in embryonated chicken eggs (blind passage).
For 15 of 20 PCR-positive samples we were able to isolate
influenza A virus in eggs. For the other five samples, which
appeared to contain less virus, as judged by the intensity of the
signals on dot blots (e.g., lanes 35, 36, and 44 in Fig. 6), no
influenza A virus could be isolated even upon blind passage in
embryonated chicken eggs.
To test the possibility that the PCR analysis would give
false-negative results compared to virus isolation in eggs, 243
individual PCR-negative cloacal swab and dropping samples
were inoculated into two to four embryonated chicken eggs
each, followed by a blind passage of the pooled allantoic fluids
in duplicate. We were unable to isolate influenza A virus from
these PCR-negative samples, indicating that no false-negative
results were obtained by PCR analysis. Inoculation of tMK and
MDCK cell cultures with 212 random PCR-negative individual
bird samples also did not reveal additional influenza A viruspositive samples. In fact, these cell lines were found to be less
susceptible to avian influenza A virus than embryonated
chicken eggs were (data not shown).
DISCUSSION
PCR-based methods for virus detection have been described
for many clinically relevant viruses. The sensitivities and specificities of PCR-based methods are most critically determined
by the choice of primer sequences. The sequences of the
primer sets described earlier for PCR-based detection of influenza A virus may be appropriate for the detection of virus
strains currently circulating in humans (1, 3, 6, 7) but display
considerable numbers of mismatches when they are compared
with the sequences of animal influenza A viruses. We have
used an extensive amount of the sequence information available for influenza A virus to design a new PCR primer set for
diagnostic purposes. Primers M52C and M253R and probe
M93C span conserved sequences in gene segment 7 of influenza A virus and have no homology to nucleotide sequences
from other species available from GenBank (http://www
.ncbi.nlm.nih.gov). Our experimental data confirmed that PCR
amplification and dot blot analyses with this set of primers does
not pick up cross-reacting host-derived sequences or other
RNA viruses and is suitable for detection of a wide variety of
influenza A virus strains. The limited variability in influenza A
virus sequences spanning the primer sequences is mostly confined to the 5⬘ ends of the oligonucleotides and therefore is
unlikely to obscure PCR amplification. Indeed, we successfully
amplified the genomes of virus isolates with mismatches in
these primer sequences that were included in the viruses shown
in Table 1 and Fig. 2.
On the basis of the results of titration experiments as well as
on analyses of clinical specimens, we conclude that the PCRbased method is more sensitive (up to 100-fold) than virus
isolation in eggs or mammalian cell cultures. This is not surprising in view of the sensitivity of PCR-based assays in general
and the low ratio of infectious units to physical particles for
RNA viruses such as influenza A virus. Perhaps as a result of
the high sensitivity, we detected influenza A virus in a human
throat swab sample from which no virus could be isolated.
Individual cells isolated from this throat swab sample were
positive upon DIF analysis, confirming influenza A virus infection.
An additional advantage of the PCR-based method is its
value in the identification of influenza A viruses from different
species. Because of differences in cellular tropism between
J. CLIN. MICROBIOL.
avian, human, and swine influenza A viruses, a single cell type
for virus isolation for diagnostic purposes is not available.
Continuous and primary cell lines obtained from a variety of
animal species and embryonated chicken eggs are routinely
used for isolation of influenza A viruses. Using the PCR-based
method, we have detected many influenza A viruses in bird
samples that could not be isolated in mammalian cell cultures
and some that could not be isolated in embryonated chicken
eggs. Presumably, this failure was due to a combination of low
virus titers in the original specimens and the limited susceptibilities of the target cells to certain influenza A virus strains. As
a national influenza center, we occasionally receive specimens
from humans from which no virus can be isolated in mammalian cell cultures but that are readily found to be influenza A
virus positive by this PCR approach (data not shown).
One disadvantage of PCR-based assays is that it is difficult to
assess if weak positive PCR results (e.g., Fig. 5, lanes 9 and 30,
and Fig. 6, lanes 35, 36, and 44) are the result of background
hybridization or low virus titers in the original samples because
of the lack of confirmation assays that are as sensitive as PCRbased methods. Therefore, it is of great importance that sufficient negative controls be included to determine a cutoff
value for background hybridization. In addition, we routinely
use 10-fold serial dilutions of a titrated influenza A virus stock
as input material in our PCR-based assays to provide a semiquantitative estimate of variability between independent assays. Both sets of controls will aid in the determination of a
cutoff value for background hybridization and weak positive
samples.
By PCR-based assays, diagnosis of influenza A virus infection can be achieved within a single working day, which is
significantly faster than the time to diagnosis of infection by
classical methods. By virus culture approaches, positive results
may be obtained in 24 h or more after inoculation, but a
definite negative diagnosis may require culture for up to 2
weeks. The availability of NA inhibitors for the treatment of
influenza virus infection may demand more rapid diagnosis of
virus infection in the future. The benefit of these new drugs
appears to depend heavily on the early start of treatment, i.e.,
within 2 days after the onset of disease (11).
Taken together, our data indicate that the newly designed
PCR offers a more sensitive and faster tool for the diagnosis of
human influenza A virus infection than virus isolation. Because
of the better matching primers, it can be expected that for the
detection of animal influenza A viruses this PCR is also more
suitable than previous PCR protocols (1, 3, 7).
ACKNOWLEDGMENTS
We thank John de Boer, Hans Zantinge, Dick Jonkers, Björn Olsen,
and their colleagues for collection of bird samples, Rob Webster for
providing influenza A virus isolates, Jan Groen and Bernadette van
den Hoogen for samples from RNA viruses, and Jan de Jong for
critically reading the manuscript. R.A.M.F. is a fellow of the Royal
Dutch Academy of Arts and Sciences.
This work was made possible in part through a grant from the Dutch
Ministry of Agriculture and from the Foundation for Respiratory Virus Infections (SRVI).
REFERENCES
1. Atmar, R. L., B. D. Baxter, E. A. Dominguez, and L. H. Taber. 1996. Comparison of reverse transcription-PCR with tissue culture and other rapid
diagnostic assays for detection of type A influenza virus. J. Clin. Microbiol.
34:2604–2606.
2. Brown, T. 2000. Analysis of DNA sequences by blotting and hybridization, p.
2.9.1–2.9.15. In F. M. Ausubel, R. Brent, R. E. Kingston, D. D. Moore, J. G.
Seidman, J. A. Smith, and K. Struhl (ed.), Current protocols in molecular
biology, suppl. 45. John Wiley & Sons, Inc., New York, N.Y.
3. Cherian, T., L. Bobo, M. C. Steinhoff, R. A. Karron, and R. H. Yolken. 1994.
VOL. 38, 2000
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
Use of PCR-enzyme immunoassay for identification of influenza A virus
matrix RNA in clinical samples negative for cultivable virus. J. Clin. Microbiol. 32:623–628.
Claas, E. C., and A. D. Osterhaus. 1998. New clues to the emergence of flu
pandemics. Nat. Med. 4:1122–1123.
Claas, E. C., A. D. Osterhaus, R. van Beek, J. C. De Jong, G. F. Rimmelzwaan, D. A. Senne, S. Krauss, K. F. Shortridge, and R. G. Webster. 1998.
Human influenza A H5N1 virus related to a highly pathogenic avian influenza virus. Lancet 351:472–477.
Claas, E. C., M. J. Sprenger, G. E. Kleter, R. van Beek, W. G. Quint, and N.
Masurel. 1992. Type-specific identification of influenza viruses A, B and C by
the polymerase chain reaction. J. Virol. Methods 39:1–13.
Claas, E. C., A. J. van Milaan, M. J. Sprenger, M. Ruiten-Stuiver, G. I.
Arron, P. H. Rothbarth, and N. Masurel. 1993. Prospective application of
reverse transcriptase polymerase chain reaction for diagnosing influenza
infections in respiratory samples from a children’s hospital. J. Clin. Microbiol. 31:2218–2221.
de Jong, J. C., E. C. Claas, A. D. Osterhaus, R. G. Webster, and W. L. Lim.
1997. A pandemic warning? Nature 389:554.
Guan, Y., K. F. Shortridge, S. Krauss, and R. G. Webster. 1999. Molecular
characterization of H9N2 influenza viruses: were they the donors of the
“internal” genes of H5N1 viruses in Hong Kong? Proc. Natl. Acad. Sci. USA
96:9363–9367.
Guo, Y. J., S. Krauss, D. A. Senne, I. P. Mo, K. S. Lo, X. P. Xiong, M.
Norwood, K. F. Shortridge, R. G. Webster, and Y. Guan. 2000. Characterisation of the pathogenicity of members of the newly established H9N2
influenza virus lineage in Asia. Virology 267:279–288.
Hayden, F. G., A. D. Osterhaus, J. J. Treanor, D. M. Fleming, F. Y. Aoki,
K. G. Nicholson, A. M. Bohnen, H. M. Hirst, O. Keene, and K. Wightman.
1997. Efficacy and safety of the neuraminidase inhibitor zanamivir in the
treatment of influenzavirus infections. GG167 Influenza Study Group.
N. Engl. J. Med. 337:874–880.
Hinshaw, V. S., R. G. Webster, and B. Turner. 1978. Novel influenza A
viruses isolated from Canadian feral ducks: including strains antigenically
related to swine influenza (Hsw1N1) viruses. J. Gen. Virol. 41:115–127.
Ito, T., J. N. Couceiro, S. Kelm, L. G. Baum, S. Krauss, M. R. Castrucci, I.
Donatelli, H. Kida, J. C. Paulson, R. G. Webster, and Y. Kawaoka. 1998.
Molecular basis for the generation in pigs of influenza A viruses with pandemic potential. J. Virol. 72:7367–7373.
PCR-BASED DETECTION OF INFLUENZA A VIRUSES
4101
14. Matrosovich, M., N. Zhou, Y. Kawaoka, and R. Webster. 1999. The surface
glycoproteins of H5 influenza viruses isolated from humans, chickens, and
wild aquatic birds have distinguishable properties. J. Virol. 73:1146–1155.
15. Peiris, M., K. Y. Yuen, C. W. Leung, K. H. Chan, P. L. Ip, R. W. Lai, W. K.
Orr, and K. F. Shortridge. 1999. Human infection with influenza H9N2.
Lancet 354:916–917.
16. Pierce, J. R. 1980. An introduction to information theory: symbols, signals
and noise, 2nd ed. Dover Publications, Inc., New York, N.Y.
17. Rimmelzwaan, G. F., M. Baars, E. C. Claas, and A. D. Osterhaus. 1998.
Comparison of RNA hybridization, hemagglutination assay, titration of infectious virus and immunofluorescence as methods for monitoring influenza
virus replication in vitro. J. Virol. Methods 74:57–66.
18. Rimmelzwaan, G. F., M. Baars, R. van Beek, G. van Amerongen, K. LovgrenBengtsson, E. C. Claas, and A. D. Osterhaus. 1997. Induction of protective
immunity against influenza virus in a macaque model: comparison of conventional and iscom vaccines. J. Gen. Virol. 78:757–765.
19. Rohm, C., N. Zhou, J. Suss, J. Mackenzie, and R. G. Webster. 1996. Characterization of a novel influenza hemagglutinin, H15: criteria for determination of influenza A subtypes. Virology 217:508–516.
20. Schild, G. C., R. W. Newman, R. G. Webster, D. Major, and V. S. Hinshaw.
1980. Antigenic analysis of influenza A virus surface antigens: considerations
for the nomenclature of influenza virus. Brief review. Arch Virol. 63:171–
184.
21. Schneider, T. D., and R. M. Stephens. 1990. Sequence logos: a new way to
display consensus sequences. Nucleic Acids Res. 18:6097–6100.
22. Scholtissek, C., H. Burger, O. Kistner, and K. F. Shortridge. 1985. The
nucleoprotein as a possible major factor in determining host specificity of
influenza H3N2 viruses. Virology 147:287–294.
23. Sharp, G. B., Y. Kawaoka, S. M. Wright, B. Turner, V. Hinshaw, and R. G.
Webster. 1993. Wild ducks are the reservoir for only a limited number of
influenza A subtypes. Epidemiol. Infect. 110:161–176.
24. Webster, R. G., W. J. Bean, O. T. Gorman, T. M. Chambers, and Y.
Kawaoka. 1992. Evolution and ecology of influenza A viruses. Microbiol.
Rev. 56:152–179.
25. Zhou, N. N., D. A. Senne, J. S. Landgraf, S. L. Swenson, G. Erickson, K.
Rossow, L. Liu, K. J. Yoon, S. Krauss, and R. G. Webster. 1999. Genetic
reassortment of avian, swine, and human influenza A viruses in American
pigs. J. Virol. 73:8851–8856.
Real-Time RT-PCR Detection
of Avian Paramyxovirus-1
and Avian Influenza Virus
Real-Time RT-PCR
Sample: i.e.
Swab material
RNA
Extraction
RRT-PCR
Results
analysis
Jan Pedersen
Avian Section Diagnostic Virology Laboratory
National Veterinary Services Laboratory
Ames, Iowa 50010
Janice.c.pedersen@aphis.usda.gov
Advantages of rRT-PCR for the
Detection of AIV and ND
Advantages of rRT-PCR for the
Detection of AIV and ND
Speed –results in as little as 3 hrs.
Scalable - large numbers of samples can be
processed
Sensitive in-vitro surveillance assay that can test
many samples
Cost (~$8 sample)
Viable virus not necessary
Reduced handling of potentially infectious material
Sensitivity similar to virus isolation
Specific
Can differentiate virulent NDV (vNDV) strains from vaccine
strains or lentogenic APMV-1 strains
Can detect H5 and H7 AIV, but can not differentiate HPAIV
from LPAIV
Reduced chance for cross-contamination vs. standard RTPCR
Disadvantages of rRT-PCR
Disadvantages of rRT-PCR
False Positives
Very sensitive: Cross-contamination
Non-specific detection
AIV and APMV-1 assays have been validated to
error on the side of false positive rather than false
negatives results
Initial equipment investment is expensive
Will detect live or inactivated virus
Not appropriate for environmental specimens
False negatives
Inhibitory substances in sample
¾ Internal controls to identify false negative
¾ Overloading silica-gel columns with organic
material
Template modification/degradation
¾ RNA fragile
Real-time RT-PCR
Isolation vs. Detection
Isolation of the
etiological agent
PCR product is detected in real-time
Sequence specific probe
¾
¾
¾
¾
Taqman/ Hydrolysis
FRET/ Hybridization
Molecular beacons
Lux Primers
Non-sequence specific DNA binding dyes
¾
SYBR green
¾
¾
Matrix
Primers/probe
Will detect all 16
H subtypes (H116) of AIV
Detects both HPAI
and LPAI
Detects Asian
H5N1
H5 Primers/probe
Detects most North
American strains of H5 AIV
Detects Asian H5N1
Detects both HPAI & LPAI
H7 Primers/probe
Detects most North
Americans strains of H7
AIV
Detects both HPAI & LPAI
APMV-1 RRT-PCR Assay
APMV-1 primer/probe
Target: Matrix gene
Conducted in chicken
embryos
Will detect most APMV-1
isolates
Virulent NDV
Avirulent vaccine strains
PPMV
Cree/CalMex-VFP-1
primer/probe
Target: fusion gene
cleavage site
Designed to detect the
CA 2002/03 strain of
vNDV
Will detect most velogens
and mesogens.
Will not detect vaccine
strains
Will detect some PPMV
Isolation of RNA from
swab or tissue
specimens
Necessary for
characterization and
pathogenicity studies
Time needed - 3 to 14
days
Virus may be infectious
or non-infectious
Time needed – 3 hrs.
Less expensive assay system
Not pathogen specific
Amplification and
identification of RNA
and not live virus
Evaluation of H5 Subtype RRT-PCR
Test for Asian H5N1
RRT-PCR for AIV
Detection of Nucleic
Acid
H5 test was originally designed primarily for North
American isolates
Could identify Asian H5N1 viruses with lower
sensitivity
Sequence analysis of Asian isolates showed good
conservation with reverse primer and probe, but 4
mismatches with forward primer
Redesigned H5 test to include forward primers
optimized for both Asian and North American viruses
NA H5F
TGACTATCCACAATACTCA
EA H5F
TGACTACCCGCAGTATTCA
Hydrolysis/Taqman probes
Reporter
Primer 1
Quencher
Taq
Primer 2
Reporter
Quencher
Taq
Hydrolysis or Taqman Probes
R
Q
Primer 1
Primer 1
Taq
R
R
Q
5’ to 3’ nuclease activity of
Taq DNA polymerase
Q
Specimens
Swabs – Can be pooled
Specimen processing and RNA extraction
¾
BSC II
Less sensitive than tracheal/oralpharyngeal
Tissue pools – small pieces of tissue in viral
transport media
Isolates RNA from other materials in the
sample
Removes inhibitory substances – may not
eliminate all
Strong detergents inactivate RNases that will
degrade RNA
Reagent preparation and RNA transfer
¾
Lung, spleen, kidney
RNA Extraction
Preferred specimen
Tissues
All Procedures should be carried out in a biological safety cabinet or
other primary containment device
Cloacal – 5/tube
¾
Tracheal or oralpharyngeal – 5/tube
¾
Specimen Processing in Lab
BSC or PCR workstation
Wear gloves at all times during this procedure
Powder-free
Extraction
Obtaining high quality RNA is the 1st and most
important step
Handling of specimen
Storage of isolated RNA
Store in RNase – free solution
24 hr. - Store at 4 C
>24 hr. - Store at -70 C
RNA Extraction- Materials
2 test samples for each person
1.5ml microfuge tubes
Extraction pipets and tips- dedicated
equipment
Vacuum manifold
and tubing
RNA Extraction- Materials
RNeasy Kit components
RLT with BME
RPE buffer with ethanol added
RW1 buffer
Nuclease free water
2ml collection tubes
2 RNeasy columns
Elution tubes
RNA Extraction- RNeasy Kit
RNA Extraction- RNeasy Kit
1. Add 500μl swab supernatant to a
1.5 ml micro centrifuge tube
2. Add 500μl RLT buffer
3. Vortex for 15 sec.
4. Pulse centrifuge
5. Add 500 μl 70% ethanol and vortex 15
sec.
6. Centrifuge lysed specimen @ 5,000 xg for 5 min.
RNA Extraction- RNeasy Kit
RNA Extraction- RNeasy Kit
9. Wash by applying 700μl RW1 buffer to
each column.
12. Centrifuge the column and collection tube for 2 minutes
at ~14 K xg and discard the collection tube.
10. Wash again by applying 500μl RPE
buffer to the column and repeat for a total
of 2 washes with buffer RPE.
11. Shut off the vacuum and place each
RNeasy column in a 2ml collection tube.
7. Set-up the vacuum manifold:
Place the appropriate number of RNeasy columns in
the luer locks of the vacuum manifold
Cover any empty positions with the luer caps
supplied with the vacuum manifold.
8. Apply vacuum and add the entire
sample/RLT/ethanol mixture to an RNeasy
column for each sample.
13. Place the column in an elution tube (or 1.5ml microfuge
tube)
14. Add 50μl nuclease free water to the column membrane
and incubate at room temperature 1 minute.
15. Elute RNA by centrifuging for 1 minute at ~14K xg.
Store at -70°C long term.
Real-time RT-PCR
RT- reverse transcription – 50 C°
cDNA is produced from RNA template
For each lab group
PCR- polymerase chain reaction
Real-time RT-PCR Materials
cDNA is amplified
DNA is more stable and more easily amplified than
RNA
Real-time
PCR amplification is monitored in real-time and the
amplicon is detected with a fluorogenic probe
Smart Cycler tube
cooling block
Smart Cycler tubes
RNA samples
Dedicated pipets and
aerosol resistant pipet
tips
1.5ml tubes
Prepare the reaction master mix in a 1.5ml tube
Real-time RT-PCR Materials
A set of RT-PCR reagents
Enzyme and RNase inhibitor in a bench top cooler
5X buffer
dNTPS
Positive control (AIV M or H5 RNA)
Nuclease free water
Forward primer (AIV M+25 or H5+1456)
Reverse primer (AIV M-124 or H5-1685)
Probe (AIV M+64 or H5+1637)
RNA Transfer
Mix reagents by vortexing for 3-5 seconds and centrifuge
briefly.
Add 17μl of the master mix to each of your Smart Cycler
tubes (add the mix to the bottom of the cup at the top of
the reaction tube).
Add 8μl of template to the Smart Cycler tubes, close and
label each tube as follows:
1.
2.
3.
4.
Positive control: in vitro transcribed RNA from the target gene
Negative control: nuclease free water.
test sample 1
test sample 2
4 people/group
5 people/group
Volume in μl
Component
H2O
5X
25mM MgCl2
Enzyme Mix
Forward Primer
83.4
60
15.0
12
6.0
Reverse Primer
dNTP’s
Probe
Rnase Inhibitor
6.0
9.6
6.0
6.0
Component
Volume in μl
H2O
97.3
5X
25mM MgCl2
Enzyme Mix
Forward Primer
Reverse Primer
70
17.5
14.0
7.0
7.0
dNTP’s
Probe
Rnase Inhibitor
11.2
7.0
7.0
Setting up rRT-PCR
Centrifuge the reaction tubes briefly in
the Smart Cycler centrifuge.
Place the reaction tubes into the Smart
Cycler and run with the “AIV Matrix” or
“H5” program.
The program has already been
programmed into the smart cycler
Primary Growth Curve
Results Interpretation
Plateau
Log-linear
Log-linear
baseline
Baseline
Evaluation of Growth Curve
Results interpretation
Threshold set too low
Log-linear
baseline
Results interpretation
Positive
Threshold set appropriately
25
Curve entering Log-linear
baseline
Negative
Results Table
Results interpretation
Check the controls
Check background fluorescence
Check each sample individually
The computer is not always correct
Look for software artifacts
Software Artifacts
Results interpretation
Record the cycle threshold (Ct) values
Software Artifacts
Suspect samples
If a sample has no cycle threshold values
(0.00) it is negative
Determine if there are any suspect
samples
For AIV or NDV a farm or premise is never
considered positive based on one positive RT-PCR
result
Epidemiology- dangerous contact
Clinical condition
Other positive diagnostic test
Weak positives- Ct values >35
Directigen (AIV)
Virus isolation
A second RT-PCR test for a different target
Internal Control for Detection
of False Positive Results
Competitive IC
Uses the same primer sites as viral target
AI matrix reagent beads - Cepheid
Non-competitive
Multiplex – completely different target and
PCR in the same tube
Spiked positive control – duplicate well
with diagnostic specimen and spiked +
AIV subtype specific
NDV- vNDV or vaccine virus specific
Are other samples from the same farm positive?
Are there enough samples from the farm?
Were the controls valid?
Background Fluorescence
Is a normal property of Real Time PCR
Fluorescence derived from unbound probe,
free dye, non-specific cleavage of probe or
sample auto-fluorescence
Represents the baseline phase
Log-linear phase represents background +
fluorescence from amplified DNA
Total FU – background FU = specific FU
Background Fluorescence Represents the Baseline of a Real
Time PCR Growth Curve
Background Subtraction
Corrects for any positive or negative drift
Calculates the average background signal and
subtracts this from each data point
Between Bkgnd Min and Max Cycle
After a cycle threshold is detected there is no
further background subtraction
All calculations are performed and applied
individually for each site
Background
Fluorescence
Off
Raw fluorescence data provides essential information about the magnitude
of the background signal and the shape of the growth curve without drift
correction.
Background Subtraction
Background Fluorescence On
Background fluorescence is derived from unbound probe
•Free dye
•Non-specific cleavage of probe
•Sample auto-fluorescence
Lab Equipment Logistics
Bio-safety cabinet space
Lab Equipment Logistics
3 Dedicated cabinets
¾
¾
¾
1. RNA extraction (full exhaust for Trizol® & Qiagen®)
2. RNA transfer to reaction tubes (BSC or PCR cabinet)
3. Clean reagents, master mix preparation (Cell culture
hood, BSC, or PCR cabinet)
Preparation of clean reagents, extraction and RNA
transfer should not be conducted in the same
laboratory space as electrophoresis of amplified RNA
Pipets
Ideally 3 sets
¾
¾
If a 2 cabinet system is used RNA transfer and
master mix preparation can be conducted in the
same hood if the hood is cleaned routinely with
10% bleach solution or Vircon-S
¾
1. RNA extraction
2. RNA transfer
3. clean reagents
2 sets – increases possibility of false +
ONLY USE AEROSOL RESISTANT TIPS
¾
¾
1. RNA extraction and transfer
2. clean reagents
Sample
APMV-1 RRT-PCR
Sample Storage
RNA extraction
Swab materials
Tissue samples
4 C for 3-4 days, more than 4 days (-70 C)
Sample RNA
Control RNA
APMV-1 Matrix
RRT-PCR
-20 C short term storage, Long term -70 C
4 C less than 24 hrs., more than 24 hrs. -70 C
Cree/CalMex
RRT-PCR
4 C up to 2 weeks, Long term -70 C (aliquot)
4 C up to 2 weeks, Long term -20 or -70 C (aliquot)
Avoid multiple freeze thaw cycles for everything
Sample
No further
testing
Positive
Probe
Negative
Positive
Negative
Report to NVSL for
Confirmation with VI and
B1 RRT-PCR (vaccine)
Report to NVSL for
Confirmation with VI and
RRT-PCR
AIV RRT-PCR
Assay Validation
RNA extraction
AIV Matrix
RRT-PCR
Negative
No further
testing
RNA extraction
Positive
H5 & H7 RRT-PCR
RRT-PCR
Negative
Report to NVSL for
Confirmation with VI
Positive
Report to NVSL for
Confirmation with VI and
RRT-PCR
Calculation of Background
Subtraction
Bkgnd Min (5) and Max (28) cycle
define the range that can be used to
calculate the average background
fluorescence
The 4 most recent cycles of data are
not included in the calculations to avoid
using specific fluorescence data
Methods and sample types compared
Primer targets
Compared primers sets
Compared with VI as “gold standard”
Calculation of Background
Subtraction Continued
At least 5 data points are used to calculate
background
Cycles 5,6,7,8,9 when the Bkgnd Min is 5
The bkgnd sub is not applied till cycle 13
1st cycle for detection of positive specimen
Cycles 10,11,12,13 are not included
4 most recent cycle
This occurs until a threshold crossing occurs
APMV-1 RRT-PCR Assay
APMV-1 primer/probe
Target: Matrix gene
Will detect most APMV-1
isolates
Virulent NDV
Avirulent vaccine strains
PPMV
Cree/CalMex-VFP-1
primer/probe
Target: fusion gene
cleavage site
Designed to detect the
CA 2002/03 strain of
vNDV
Will detect most velogens
and mesogens.
Will not detect vaccine
strains
Will detect some PPMV
1. Real-Time RT-PCR using Applied Biosystems® Sequence Detection Systems
The following procedures should be used with the Applied Biosystems Sequence
Detection instruments (ABI). The following methods were validated with the 7900HT
system, and other systems (7000, 7300, 7500) should operate similarly when the 9600
emulation mode is selected.
The ABI Sequence Detection System uses an internal passive reference molecule
(ROX™), which acts as a normalization factor for fluorescent emissions detected in the
samples. The master mix formulas have been adjusted to include a ROX™ reference dye
(Catalog # 12223-012, Invitrogen, Carlsbad, CA). THESE MASTER MIX
FORMULAS SHOULD ONLY BE USED WITH THE ABI SYSTEMS. THE ROX
DYE WILL INTERFERE WITH SMART CYCLER DATA COLLECTION.
Table 4. Real-time RT-PCR reaction mix volumes and conditions for type A influenza
(MA gene), H5 and H7 primer/probe sets using the ABI Sequence Detection System
H2O
5X buffer
25mM MgCl2
dNTP’s (10 mM each)
Forward Primer
(20 pmol/ul)
Reverse Primer
(20 pmol/ul)
Rnase Inhibitor
13.3 units/µl
Enzyme Mix
Probe (6 pmol/ul)
ROX reference dye
MM per rxn
Template
Total
Volume Per
Reaction
6.45 μl
5
1.25
0.8
0.5
1X
3.75 mM*
320 μM ea. dNTP
10 pmol/25μl
0.5
10 pmol/25μl
0.5
0.266 units/µl
1.0
0.5
0.5
17
8
25μl
Final
Concentration
Volume for
___ Reactions
0.12 μM
The ABI Sequence Detection systems use a 96-well plate format. Before setting up
reactions, the PCR plate should be placed into a Splash-free Support Base (P/N 4312063,
ABI, Foster City, CA). The base is used to protect the bottom of the plate from picking
up particles that may interfere with the optical system. Any residual dust, disinfectant
materials, etc. on the bottom of the plate may alter the background fluorescence in that
well position.
The arrangement of the reactions on the plate must match the configuration of
information on the corresponding plate document.
Add 17 µl of master mix to the PCR plate in the Support Base. Touch the tip to the side
of the well to draw all of the liquid out of the pipet tip. Add 8 µl of the test sample RNA
to the appropriate well using a pipettor designated for RNA transfer. After all of the
sample RNA have been added, add 8 µl of positive control to the designated positive
control well (using a pipettor designated for transcribed RNA), and 8 µl of RNase free
water to the designated negative control well. After all of the RNA have been added to
the PCR plate, place an optical adhesive cover (ABI catalog #4311971) over the top of
the plate. Be sure to press the adhesive cover firmly against the top of the plate using the
MicroAmp Adhesive Seal Applicator (as supplied with Optical Adhesive Cover Starter
Kit) so that each well is sealed air-tight. If the adhesive cover is not sealed against the
plate, there may be evaporation from the wells and results may be jeopardized.
Visually verify that each reaction is positioned at the bottom of its well. If the sample is
lying against the side wall of the well, or if there is an air bubble at the bottom of the
well, the plate may be centrifuged briefly to position all contents at the bottom.
Apply the compression pad that is specific to your particular instrument to the sealed
optical plate, and place into the ABI machine.
Thermal cycling Conditions for AIV wet reagent PCR for Cepheid Smart Cycler
and Applied Biosystems Inc. (ABI) instrumentation
Probe/Primer set
AIV matrix
(Smart Cycler)
45 cycles
Step
denaturation
Time
1 sec.
Temp
94° C
Annealing*
20 sec.
60° C
AIV matrix (ABI)
45 cycles
denaturation
Annealing*
15 sec.
1 min.
94° C
60° C
H7 (Smart Cycler)
40 cylces
denaturation
Annealing*
1 sec.
20 sec.
94°C
58°C
H7 (ABI)
40 cycles
denaturation
Annealing*
15 sec.
1 min.
94°C
58°C
H5 (Smart Cycler)
40 cycles
denaturation
Annealing*
extension
1 sec.
20 sec.
5 sec.
94°C
57°C
72°C
H5 (ABI)
41 cycles
extension
denaturation
Annealing*
5 sec.
1 sec.
20 sec.
72°C
94°C
57°C
The order of programming is different for ABI and Smart Cycler when using
a 3 step PCR procedure. For the ABI, it is necessary to program the 5 sec.
extension step first, 1 sec. denaturation step second, and the 20 sec. annealing
step third. The fluorescence is acquired during the annealing stage which is
the third step. ABI instrumentation can not collect fluorescence during the
second step of a 3 step PCR.
* The fluorescence is acquired at the annealing step.
2. Setting up Applied Biosystems Sequence Detection System reactions
Setting up the reactions
Create a new document. Select Assay: Absolute Quantification (Standard Curve);
Container: 96 Wells Clear Plate from the drop down menus. Select the appropriate
protocol under the Template drop down. The matrix protocols are used for screening
specimens. The AIV H5 and AIV H7 primers/probes are used to detect these specific
subtypes of AIV. The thermal cycling parameters for each protocol are described in
appendix D.
Click on Add Detector to create a marker for the absolute quantification probe being
used. Click New to create a new detector and assign a name, identify the correct reporter
dye and quencher dye, and assign a color for the detector. Click OK. Highlight the
Detector and click Copy to Plate Document. Click Done.
Using the Ctrl and Shift keys, select individual wells or groups of wells on the plate grid
that contain reaction mix. In the well inspector, click the Use check box of the marker
you want to add to the selected wells. NOTE: The detectors associated with the marker
are automatically applied to the selected wells when the marker is placed in Use.
Click on each well position and apply the sample ID to the appropriate well (this may
also be done after the instrument completes the run).
Note the Passive Reference box defaults to ROX. This refers to the passive reference dye
that is added to the master mix.
Select the Instrument tab of the plate document. If necessary, check the 9600
Emulation box. (When the 9600 Emulation box is checked, the SDS Software reduces
the ramp rate of the 7900HT instrument to match that of the ABI PRISM® 7700
Sequence Detection System instrument.) Change the sample volume to 25 µl. Check to
ensure the thermal profile is set to the appropriate thermal cycling parameters for the
selected assay.
Select File/Save As and enter a unique run name.
Connect to the instrument. Open the tray and place the PCR plate in the instrument.
Check to be sure that position A1 on the instrument matches position A1 on the PCR
plate. Close the instrument tray. Start the run.
3. Interpretation of Results from ABI Sequence Detection Systems
After the run has completed successfully, select Analysis>Analysis Settings from the
menu. Select Manual Ct and Automatic Baseline. Then select Analysis>Analyze. The
results are displayed in the Results tab. Use the Automatic Baseline option to
automatically calculate the placement of the threshold. Visually inspect the placement of
the threshold value. The threshold should lie in approximately the center of the linear
phase of amplification (refer to Figure 1). The amplification plot of each specimen
should also be analyzed individually. Aberrant curves should be viewed in the
Multicomponent Pane. The multicomponent illustrates absolute change in emission
intensity and the SDS software displays cycle-by-cycle changes in normalized reporter
signal (Rn). There are up to five curves in the Multicomponent Pane: the reporter
component (FAM), the quencher component (TAMRA), the reference component
(ROX), the background component, and the mean squared error (mse). The quencher
component may not be present if a Black Hole Quencher (BHQ) is used. Check to be
sure that the quencher or reference components do not increase as the FAM component
increases. If these dyes increase in fluorescence as the FAM increases, these Ct values
should be disregarded and the reaction should be repeated.
Procedure for the Roche LightCycler® 1.2 Real-Time Reverse Transcriptase PCR
Instrument for the Detection of Avian Influenza and Avian Paramyxovirus-1 with
Official USDA rRT-PCR Protocol
The following procedure should be used with the Roche LightCycler® 2.0 real-time
instrumentation for the detection of avian influenza and avian paramyxovirus-1. The
procedure describes the modifications that are required for the implementation of NVSL
AVPRO1510 and AVPRO1505. Equivalency validation studies were conducted by
NVSL to support the necessary changes in the standard protocols for the use of the
LightCycler® 2.0 real-time instrumentation.
Equipment and Reagents
Non-acetylated Bovine Serum Albumin (BSA). It is essential the BSA be non-acetylated as
acetylated BSA is inhibitory to PCR.
Recommended sources and preparation of 5 mg/ml concentration for a final
concentration of 250 µg/ml in 20 μl reaction.
New England Biolabs (Ipswich, MA) Catalog # B9001S - 10 mg/ml. Dilute 1 in 2 for 5
mg/ml concentration in RNase free water
Ambion (Austin, TX) Catalog # 2616 or 2618 – 50 mg/ml. Dilute 1 in 10 in RNase free
water for 5 mg/ml concentration.
LightCycler® 20 μl Capillaries (Roche Catalog Number: 11 909 339 001)
LightCycler® Centrifuge Adaptors (in a block) (Roche Catalog Number: 11 909 312 001)
Table 1. Real-time RT-PCR reaction mix volumes using Qiagen One-Step RT-PCR Kit:
Component
Water
5x reaction buffer*
25 mM MgCl2
Enzyme mix*
Forward primer
Reverse primer
dNTPs*
Probe
RNase Inhibitor
BSA (5.0 mg/ml)
MM per reaction
RNA Template
Total volume
Volume Per
Reaction (μl)
2.4
4
1
0.8
0.5
0.5
0.8
0.5
0.5
1
12
8
20
Final
Concentration
1x
3.75 mM
10 pmol
10 pmol
400 mM each
0.3 μM
0.33 units/µl
250 μg/ml
* Qiagen (catalog # 210210) buffer already contains 2.5 mM MgCl2 at 1X concentration
RT Step Thermocycling conditions for Qiagen® one-step RT-PCR kit.
RT Step
1 cycle
30 min
15 min
50°C
95°C
Thermocycling conditions for gene specific probe and primer sets:
Probe/Primer set
AIV Matrix
Cycles
45 cycles
Step
Denaturation
Annealing*
Time
10 sec
20 sec
Temp
94°C
60°C
H5
40 cycles
Denaturation
Annealing*
Extension
10 sec
20 sec
5 sec
94°C
57°C
72°C
NDV
40 cycles
Denaturation
Annealing*
Extension
10 sec
30 sec
10 sec
94°C
56°C
72°C
*Fluorescence is collected during the annealing stage.
Programming the LightCycler® Instrument
LightCycler® 4.0 Software:
1. Start the LightCycler® 4.0 Software by double-clicking on the LightCycler® 4.0
Software icon on the desktop.
2. In the Login dialog box, type your user name and password.
3. To connect to the database on the local computer, select My Computer in the Log
on to box.
4. Click Login.
5. To program a new protocol, access New Experiment in one of the following ways.
If the Front Screen is displayed, click on New Experiment to start a run. Otherwise,
click the New button, or select New from the File menu and then New Experiment
from the New window, or click on the Run button.
6. In the Setup section of the Programs tab, specify general instrument settings:
a. Default Channel: select the 530 Channel.
b. Seek Temperature: 30°C.
c. Max. Seek Pos.: enter the number of sample positions the instrument
should look for.
d. Instrument Type: choose the 6 Ch. Instrument type for your LightCycler®
2.0 Instrument (this is default). For LightCycler® 1.2 Instrument, select the
3 Ch. Instrument type.
e. Capillary Size: for the 6 Ch. Instrument type, select the capillary size (20
or 100 μl).
5. In the Programs section of the Programs tab, click (+) to add a new program.
6. Edit the default values for the program parameters, clicking the tab button on your
keyboard to move from one column to the next.
Parameter
Program Name
Cycle
Analysis Mode
Description/Instructions
The name for the program. Click in the
Program Name box, then enter a new name.
The number of times the program should be
repeated. Enter a value or select it by
clicking on the up and down arrows.
The type of analysis expected for this
program (if any). Select an analysis mode
from the pull-down list.
Valid Values
Any alphanumeric string
1-99 cycles
None: no analysis
Melting Curves: a melting
curve analysis is expected.
Quantification: a quantification
analysis is expected.
Color Compensation: a color
compensation analysis is
expected.
7. In the Temperature Targets section, edit the default values for the temperature
parameters.
Parameter
Description/Instructions
Valid Values
Value of
Value for
AI Matrix
AI Matrix
RT
PCR assay
The
target
temperature.
Enter
a
37°C-98°C
50
step
1
94°C
Target
Hold
Slope
Sec. Target
Step Size
Step Delay
Acquisition
Mode
temperature.
The length of time to hold the target
temperature in
hours:minutes:seconds. Enter a hold
time.
The speed with which the
temperature must be reached,
specified in degrees per second.
Enter a slope.
A second target temperature to be
reached by the last cycle of the
program. Useful for Touchdown
PCR. Enter a temperature.
The number of degrees to change the
temperature with each cycle to reach
the secondary target. Enter a step
size.
The cycle number at which the
temperature step up or step down
begins. Enter a cycle number.
The frequency with which
fluorescence data is acquired. Select
an acquisition mode from the pulldown list.
94 step 2
30:00 step 1
15:00 step 2
1.0
0.05°C - 20°C per
second.
20.0
20.0
37°C-98°C
0.00
0.0
0°C - 20°C
0.00
0.0
0-99 cycles
0.00
0.0
None: no fluorescence
data is acquired.
Single: acquires
fluorescence data once at
the end of this
temperature segment in
each cycle.
Continuous: acquires
fluorescence data
continuously.
Step: acquires
fluorescence data at each
temperature transition.
None
Single
00:00:00-12:00:00
8. Click (+) to add another temperature target to the current program, then enter
parameter values. Repeat to define as many temperature targets, as you need for
the current program.
9. Repeat steps 7 – 10 to create additional programs and their temperature targets.
Programs or temperature targets can be reordered by selecting the item you want
to move, then clicking the up or down arrow. To delete an item, select the item,
then click (-).
10. Look at the Overview section to see a graphical representation of all the programs
you have defined.
11. Click Save in the global toolbar to save the protocol. Navigate to a location to
save the protocol, enter a protocol name, then click OK.
LightCycler® 3.5.3 Software:
1. Start the LightCycler® 3.5.3 Software by double-clicking on the LightCycler® 3
Front Screen icon on the desktop. Alternatively, in the Windows Start Menu bar,
click on the LightCycler® Front Screen under the LightCycler® 3 folder.
2. In the LightCycler® Front Screen, click the Run button to enter the Programming
Screen. If you have not switched on the LightCycler® instrument, the software
will prompt you to do so.
3. A dialog box will appear which offers the execution of an optional 1-2 minutes
self test. The performance of one self test a day is recommended.
4. In the programming screen, click on the New Experiment button to create a new
Experimental Protocol. To open and modify an existing file, select the Open
Experiment File button.
5. Use the buttons in the Cycle Program Field to define the Cycle Programs for your
Experimental Protocol:
Button
Function
Add
Creates a new Cycle Program.
Remove
Removes a selected program.
Import
Imports a cycle program from other experiment protocols.
Move Up
Changes the order in which cycle programs will be executed.
6. To alter the name of a Cycle Program, double click on the name in the Cycle
Program field. A window will pop up which allows change of the name.
7. Upon addition of a Cycle Program, the Cycle Program Data field in the middle of
the screen is activated.
8. Use the Temperature Targets Segment to define the temperature profiles for each
individual program: Click on the green Ins button to enter a new temperature
segment. Click on the red Del button to delete a temperature target.
9. Enter the appropriate target temperatures and times:
Field
Purpose
Target Temperature (°C) Defines the temperature of the segment in °C.
Defines the holding time of a temperature segment.
Incubation Time
(h:min:secs)
Temperature Transition Defines rates at which the instrument changes temperature between
temperature targets. The slowest rate is 0.1°C/sec and the fastest rate is
Rate (°C/sec)
Secondary Target
Temperature (°C)
Step Size (°C)
Step Delay (cycles)
20°C/sec.
Defines a second target temperature within a segment beginning at a
defined cycle number. This is for Touchdown PCR.
Defines the degree of change per cycle used to step up/step down from the
Target Temperature to the Secondary Target Temperature.
Defines the cycle number at which the step up/step down from the Target
Temperature to the Secondary Target Temperature begins.
10. Specify the fluorescence acquisition mode:
Type
Description
No fluorescence measurement.
None
Fluorescence is measured once per sample at the end of the temperature
Single
Cont. (Continuous)
Step (Stepwise)
segment selected.
Fluorescence of all samples is measured continuously from the first sample to
the last one.
Fluorescence of all samples is measured after each temperature transition.
11. Select the correct Analysis Mode for the Cycle Program:
a. Default setting is None (no data analysis is intended for this cycle
program)
b. Choose Quantification for later quantification analysis of the data.
c. Choose Melting Curve Analysis for later analysis of melting curve data.
12. Type in the number of cycles to be run with the selected Temperature Targets.
The resulting Cycle Program profile can be monitored in the Cycle Simulation
field.
13. Add all Cycle Programs needed for the Experimental Protocol. The resulting
Experimental Protocol profile can be monitored in the Experiment Simulation
field.
14. Select the Fluorescence Display Mode according to the detection system you have
chosen.
15. Click the Save Experiment File button to save a newly defined or modified
Experimental Protocol. The file is automatically saved as *.exp in the User
directory.
Setting Up Roche LightCycler® Reactions
1. In a 1.5 ml tube, prepare reagent mastermix according to table 1(everything
except RNA template) as described above. To prepare the mastermix for more
than one reaction, multiply the amount in the “Volume per reaction” column by z,
where z = the number of reactions to be run plus 1-2 additional reactions
(compensates for pipetting errors). To eliminate laboratory contamination it is
necessary to prepare the reagent mix in a dedicated clean reagent hood with
pipettes and filtered pipette tips that are dedicated to the preparation of clean
reagents.
2. Place the number of LightCycler® capillaries required in the pre-cooled
LightCycler® Centrifuge Adaptor Block.
3. Pipette 12 microliters of mastermix into each capillary.
4. Pipette 8 microliters of RNA (controls or unknown samples) into each capillary.
The transfer of RNA should be conducted in a PCR workstation or biosafety
cabinet that is not used for the extraction of RNA from diagnostic specimens or
the preparation or clean reagents.
5. Cap each capillary with the supplied caps using the LightCycler® Capping Tool.
When capping make sure to press straight down on capillary, not from an angle.
Lift capped capillary out of adaptor and release cap from Capping Tool.
6. If you have a LightCycler® Carousel Centrifuge, place capillaries into the
LightCycler® Carousel and centrifuge according to the manufacturer’s
instructions, prior to placing the LightCycler® Carousel in the LightCycler®
instrument. If you do not have a LightCycler® Carousel Centrifuge, centrifuge
LightCycler® capillary adaptors with capped capillaries in a microcentrifuge. Only
a short pulse is required. Then place centrifuged capillaries in the LightCycler®
Carousel, prior to placing the loaded carousel in the LightCycler® instrument.
7. Set up the cycling parameters as described above and start the RT-PCR by
clicking on the “Start Run” button.
Interpretation of Results from Roche LightCycler® Detection Systems using the
Automated Method
LightCycler® 4.0 Software:
The automated absolute quantification method uses a different algorithm method of
calculating the crossing point (CP) than the Fit Points method. Equivalency testing has
not been conducted on the Fits Points method. The Fits Points method should not be
used to interpret and analyze results for NVSL AVPRO1510 and AVPRO1505.
1. Click Analysis on the main toolbar.
2. Select Absolute Quantification, then click OK
3. In the Sample Editor, enter specimen identification information on the Capillary
View tab, and select the channel (FAM) to be used in the experiment.
4. On the Abs Quant tab of the Sample Editor, enter sample information as follows:
Column Name
Valid Values
Description
Target Name
Any name
Name of the target for this
channel
Type
Unknown Standard
Type of sample in this
capillary
Concentration
Any concentration value
Concentration of a standard
sample
5. Click Abs Quant in the module bar to open the analysis module.
6. From the Channel menu select the channel (FAM) for the targets you want to
analyze.
7. To see the crossing points and concentrations, drag or click on the slide bar.
LightCycler® 3.5.3 Software:
1. In the LightCycler® Front Screen, click on the Analysis button.
2. Select your experiment and click the Open button. Alternatively double-click your
experiment.
3. Select the appropriate part of the run to be analyzed in the Select a Program drop
down menu: Select Cycles.
4. Adjust the y-axis for the Fluorescence graph: Choose F1 axis setting for TaqMan
Probes.
5. Select the type of analysis you want to perform:
a. Click on Quantification to proceed to the Quantification Screen.
6. Highlight the samples to be analyzed.
7. Select Second Derivative Maximum in the Analysis field (top left corner).
8. Click Proportional in the Baseline Adjustment box (to the right of the Analysis
box).
9. Then select Step 2: Analysis to see the standard curve.
10. Crossing points and concentrations will be displayed next to the sample names.
11. If sample names and concentrations of standards need to be edited after the run:
a. From the LightCycler® Front Screen, click on Options and select LC Data
File Editor.
b. Click the Open button and find and select your experiment. Click the
Open button, or double-click the experiment to open it.
c. Click on the Change Samples button to enter the Sample Editor.
d. Edit the names and/or concentrations and click on the Done button.
e. Click the Save button to save the changes.
f. Click the Exit button to exit the data editor.
Tips for preventing breakage of capillaries:
1. Handle the capillaries with care; prevent breakages by not “bending” capillaries.
2. When capping make sure to press straight down on capillary, not from an angle.
Lift capped capillary out of adaptor and release cap from Capping Tool.
3. Before loading capillaries in the LightCycler® Carousel, clean out the carousel
with the dental floss cleaner.
4. If a capillary breaks in the carousel, make sure that there is no glass shards left in
the hole by cleaning with the dental floss cleaner.
5. Replace the rubber ring in the carousel before the rubber starts to break down and
become hard.
Blank Page
Prepare the reaction master mix in a 1.5ml tube
4 people/group
Component
H2 O
5X
25mM MgCl2
Enzyme Mix
Forward Primer
Reverse Primer
dNTP’s
Probe
Rnase Inhibitor
Volume in μl
83.4
60
15.0
12
6.0
6.0
9.6
6.0
6.0
5 people/group
Component
Volume in μl
H2O
97.3
5X
70
25mM MgCl2
17.5
Enzyme Mix
14.0
Forward Primer
7.0
Reverse Primer
7.0
dNTP’s
11.2
Probe
7.0
Rnase Inhibitor
7.0
Blank Page