TIMI-617; No of Pages 5
Opinion
Staphylococcus aureus as an
intracellular pathogen: the role of small
colony variants
Parham Sendi1,2 and Richard A. Proctor3
1
Unit of Infectious Diseases, Basel University Medical Clinic, 4410 Liestal, Switzerland
Center for Infectious Medicine, Department of Medicine, Karolinska Institutet, 141 86 Stockholm, Sweden
3
Departments of Medical Microbiology/Immunology and Medicine, University of Wisconsin School of Medicine and Public Health,
Madison, WI 53706, USA
2
Increasing evidence indicates that Staphylococcus aureus might be a facultative intracellular pathogen. In
particular, certain subpopulations, called small colony
variants (SCVs), seem to be well adapted to the intracellular milieu. When compared to ‘normal’ staphylococcal strains, SCVs show increased uptake by host cells,
resistance to intracellular defenses and reduced stimulation of host defenses. We propose that the ability to
form two subpopulations with different phenotypes
might allow S. aureus the option for both extra- cellular
and intra-cellular survival in the host.
Small colony variants of Staphylococcus aureus: a link
to recurrent infections?
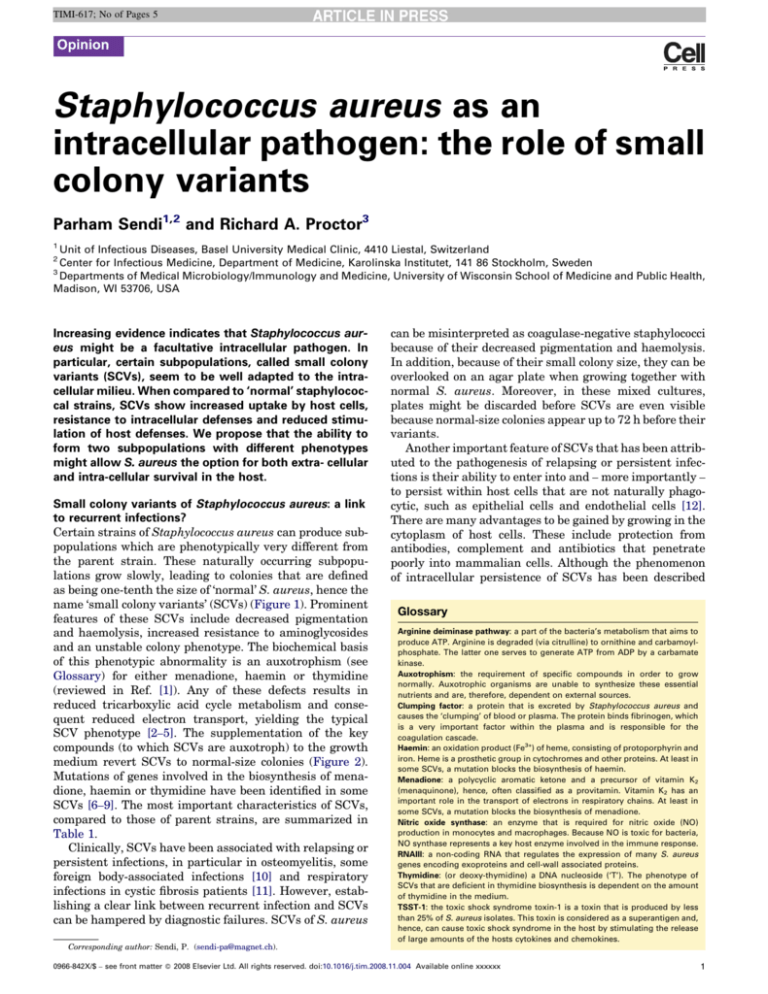
Certain strains of Staphylococcus aureus can produce subpopulations which are phenotypically very different from
the parent strain. These naturally occurring subpopulations grow slowly, leading to colonies that are defined
as being one-tenth the size of ‘normal’ S. aureus, hence the
name ‘small colony variants’ (SCVs) (Figure 1). Prominent
features of these SCVs include decreased pigmentation
and haemolysis, increased resistance to aminoglycosides
and an unstable colony phenotype. The biochemical basis
of this phenotypic abnormality is an auxotrophism (see
Glossary) for either menadione, haemin or thymidine
(reviewed in Ref. [1]). Any of these defects results in
reduced tricarboxylic acid cycle metabolism and consequent reduced electron transport, yielding the typical
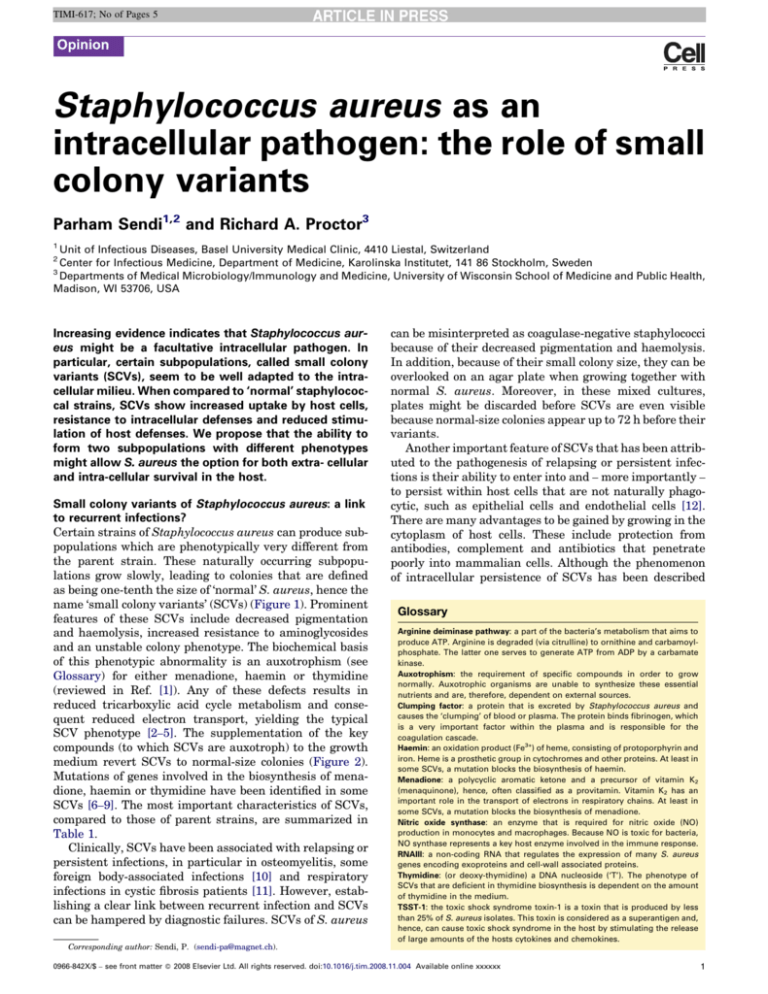
SCV phenotype [2–5]. The supplementation of the key
compounds (to which SCVs are auxotroph) to the growth
medium revert SCVs to normal-size colonies (Figure 2).
Mutations of genes involved in the biosynthesis of menadione, haemin or thymidine have been identified in some
SCVs [6–9]. The most important characteristics of SCVs,
compared to those of parent strains, are summarized in
Table 1.
Clinically, SCVs have been associated with relapsing or
persistent infections, in particular in osteomyelitis, some
foreign body-associated infections [10] and respiratory
infections in cystic fibrosis patients [11]. However, establishing a clear link between recurrent infection and SCVs
can be hampered by diagnostic failures. SCVs of S. aureus
can be misinterpreted as coagulase-negative staphylococci
because of their decreased pigmentation and haemolysis.
In addition, because of their small colony size, they can be
overlooked on an agar plate when growing together with
normal S. aureus. Moreover, in these mixed cultures,
plates might be discarded before SCVs are even visible
because normal-size colonies appear up to 72 h before their
variants.
Another important feature of SCVs that has been attributed to the pathogenesis of relapsing or persistent infections is their ability to enter into and – more importantly –
to persist within host cells that are not naturally phagocytic, such as epithelial cells and endothelial cells [12].
There are many advantages to be gained by growing in the
cytoplasm of host cells. These include protection from
antibodies, complement and antibiotics that penetrate
poorly into mammalian cells. Although the phenomenon
of intracellular persistence of SCVs has been described
Glossary
Arginine deiminase pathway: a part of the bacteria’s metabolism that aims to
produce ATP. Arginine is degraded (via citrulline) to ornithine and carbamoylphosphate. The latter one serves to generate ATP from ADP by a carbamate
kinase.
Auxotrophism: the requirement of specific compounds in order to grow
normally. Auxotrophic organisms are unable to synthesize these essential
nutrients and are, therefore, dependent on external sources.
Clumping factor: a protein that is excreted by Staphylococcus aureus and
causes the ‘clumping’ of blood or plasma. The protein binds fibrinogen, which
is a very important factor within the plasma and is responsible for the
coagulation cascade.
Haemin: an oxidation product (Fe3+) of heme, consisting of protoporphyrin and
iron. Heme is a prosthetic group in cytochromes and other proteins. At least in
some SCVs, a mutation blocks the biosynthesis of haemin.
Menadione: a polycyclic aromatic ketone and a precursor of vitamin K2
(menaquinone), hence, often classified as a provitamin. Vitamin K2 has an
important role in the transport of electrons in respiratory chains. At least in
some SCVs, a mutation blocks the biosynthesis of menadione.
Nitric oxide synthase: an enzyme that is required for nitric oxide (NO)
production in monocytes and macrophages. Because NO is toxic for bacteria,
NO synthase represents a key host enzyme involved in the immune response.
RNAIII: a non-coding RNA that regulates the expression of many S. aureus
genes encoding exoproteins and cell-wall associated proteins.
Thymidine: (or deoxy-thymidine) a DNA nucleoside (‘T’). The phenotype of
SCVs that are deficient in thymidine biosynthesis is dependent on the amount
of thymidine in the medium.
TSST-1: the toxic shock syndrome toxin-1 is a toxin that is produced by less
than 25% of S. aureus isolates. This toxin is considered as a superantigen and,
hence, can cause toxic shock syndrome in the host by stimulating the release
of large amounts of the hosts cytokines and chemokines.
Corresponding author: Sendi, P. (sendi-pa@magnet.ch).
0966-842X/$ – see front matter ß 2008 Elsevier Ltd. All rights reserved. doi:10.1016/j.tim.2008.11.004 Available online xxxxxx
1
TIMI-617; No of Pages 5
Opinion
Trends in Microbiology Vol.xxx No.x
Figure 1. Pictures of S. aureus of same clonal origin on sheep blood agar plates
after 48h incubation. Scale bar = 1 cm. (a) Normal-sized colonies, of 2–3 mm in size,
show a typical golden pigmentation. (b) Small colony variants.
many years ago [13], there is accumulating evidence that
normal colony-size S. aureus is also a facultative intracellular microorganism. Garzoni et al. [14] have reviewed
important findings that highlight the potential of S. aureus
to enter host cells that are not naturally phagocytic, such
as epithelial cells. They also draw attention to the fact that
no coherent model of pathogen–host interaction presently
encompasses all aspects of S. aureus intracellular survival
and virulence properties because there are clearly differences among strains. Here, we would like to emphasize the
growing evidence indicating that SCVs are particularly
well endowed with the bacterial strategies required for
intracellular survival.
Intracellular S. aureus: normal colony-size or SCVs?
Recent studies using cell cultures [15] and clinical samples
[16] strongly suggest that S. aureus is able to persist
Figure 2. Haemin-auxotrophic small colony variants of S. aureus. Cells grow only
in the proximity of a disc containing haemin. The diameter of the disc is 10 mm.
intracellularly. Therefore, questions are raised whether
all intracellular staphylococci are in fact SCVs, or whether
SCVs are an artefact because of the difficulties in culturing
intracellular pathogens. No study has fully addressed this
question with clinical isolates, most likely because of technical limitations and the ability of SCVs to revert rapidly in
the extracellular milieu. However, certain indicators allow
us to postulate that there are true differences between
SCVs and normal colony-size S. aureus.
Two recent studies revealed the presence of normal
colony-size S. aureus in epithelial cells [15,16]. Although
SCVs were actively searched, no altered colonies could be
found. These results indicate that these normal colony-size
Table 1. Characteristics of SCVs of S. aureus, as compared to parent strains
Refs
Phenotypic characteristics
Colony size
Pigmentation
Haemolytic activity
Coagulase production
Resistance towards aminoglycosides
Auxotrophism
Growth
Cell wall
Electrical potential across membrane
Metabolism
Tricarboxylic acid cycle
Acetate catabolism
Arginine deiminase pathway
Virulence determinants
Toxin production
Clumping factor
Fibronection binding proteins
Polysaccharide intercellular adhesion
RNAIII
sigB
agr
hla
2
10 times smaller than normal colonies
Weak
Weak
Weak
Increased
Present
Slow
Thick
Low
[13,49,50]
[13,49,50]
[13,49,50]
[13,49,50]
[13,49,50]
[13,49,50]
[13,49,50]
[22]
[23,24]
Reduced
Reduced
Increased
[2]
[2]
[3]
Weak or absent
Increased levels
Increased levels
Increased
Very low levels
Upregulated
Downregulated
Downregulated
[1,51]
[27]
[27]
[45]
[1,36,37]
[20]
[20]
[20]
TIMI-617; No of Pages 5
Opinion
S. aureus did not require a phenotypic change for at least
short term survival in cells. In contrast, several analyses of
clinical isolates clearly showed the classical phenotypic
characteristics of SCVs, including auxotrophism [17–19].
Moreover, although normal colony-size S. aureus can enter
host cells, their ability to persist has not been clearly
established. Compared to SCVs, normal S. aureus seem
to reside intracellularly for a shorter period of time, at least
in cell cultures [18]. Finally, a recent work was able to
confirm the hypothesized genetic basis of SCV phenotypes
in clinical isolates, by revealing mutations in menB, the
gene encoding naphtoate synthase for menadione biosynthesis [6].
Based on our own observations (Proctor) and those of
others (O. Vesga et al., personal communication), it is
possible that a selection process occurs when non-phagocytic cells are infected with S. aureus. It can be speculated
that a pressure to survive intracellularly selects for these
mutations, and hence for the occurrence of SCVs because
normal colony-size S. aureus rapidly kills the host cell.
However, potential details of such a mechanism are largely
unknown.
SCVs defense strategies to facilitate colonization
In SCVs, a gene coding for an alternate sigma factor, sigB,
is upregulated [20]. This gene is recognized as an important regulator of bacterial stress responses and is involved
in bacterial strategies to overcome a variety of environmental stress factors, such as pH, temperature and osmolarity [21].
Additionally, SCVs have a thick cell wall [22] and their
electrical potential across the cytoplasmic membrane
drops immediately when nutrients are expired (e.g. glucose) or do not allow further growth (e.g. lactate, acetate)
[23,24]. A reduced membrane potential is known to confer a
certain degree of resistance to cationic antimicrobial peptides [25], which are effector components of the host’s
innate defense system. The peptides are produced by
neutrophils and macrophages, but also by epithelial cells
[26].
Increased uptake and adherence of SCVs?
Bacterial adherence to the host cell is a prerequisite for
invasion. The interaction between S. aureus and host cells
is believed to occur through a bridging mechanism, in
which bacterial adhesion proteins, host proteins (e.g. fibronectin) and cell integrins participate. Integrins mediate
communication and adhesion between mammalian cells
and the extracellular matrix. S. aureus expresses an array
of adhesins, including the ‘microbial surface components
recognizing adhesive matrix molecules’ (MSCRAMMs)
that are anchored to the bacterial surface. S. aureus utilizes MSCRAMMs to adhere directly to host cells or via
bridging ligands with fibronectin-binding proteins. SCVs
show increased expression of the fibrinogen-binding
clumping factor and fibronectin-binding proteins [27]
because of positive regulation by sigB and the loss of
negative RNAIII regulation [20]. These variants are, therefore, well adapted for efficient attachment to host cells.
Once attached to the host cell surface, bacteria induce
changes in the host cell cytoskeleton that result in their
Trends in Microbiology
Vol.xxx No.x
engulfment. By inducing such rearrangements in normally
non-phagocytic cells, the bacteria are, in effect, forcing
phagocytosis by eliciting formation of pseudopod-like
structures that mediate their uptake. Ingestion of S. aureus by epithelial cells is initiated by either direct or indirect
engagement of host integrin receptors. Through integrinmediated signal transduction, a protein kinase for serine
and threonine can interact with cytoplasmic domains of
integrins [28]. This so-called integrin-linked kinase (ILK)
has an important role in regulating actin cytoskeleton
reorganization [29]. S. aureus, among other pathogens,
requires ILK in the host cell to promote invasion in epithelia [30]. Although ILK mechanisms have not yet been
elucidated in SCVs, the observed increased uptake of SCVs
compared to normal-phenotype S. aureus into non-professional phagocytes could well be because of the increased
expression of MSCRAMMs and their interaction with host
cell integrins [27] and, consequently, rapid activation of
ILK.
After engulfment, bacteria require several characteristics to survive intracellularly. These include (i) not killing
the host cell, either by lysis or by inducing apoptosis; (ii)
resisting the intracellular host defenses; (iii) not activating
the host immune system and, (iv) the ability to proliferate
in the cytoplasm.
SCVs cause less damage to host cells
In contrast to normal colony-size S. aureus, SCVs have a
decreased production of a-toxin and, consequently, do not
lyse their host cells [1]. In addition, SCVs produce lower
amounts of toxic shock syndrome toxin 1 (TSST-1), which
would result in a lower activation of host immune cellmediated cytotoxicity [31].
Several studies have suggested that normal colony-size
intracellular S. aureus mediates apoptosis in epithelial
cells [32], endothelial cells [33] and keratinocytes [34],
with the well-known virulence regulatory gene, agr, having
an important role. Strains of S. aureus carrying mutations
in agr are internalized but do not induce apoptosis in
endothelial cells [35]. Remarkably, transcriptional studies
of clinical SCV isolates using DNA microarrays show no
activation of agr and low levels of a-toxin gene (hla)
expression [20]. Furthermore, SCVs show extremely low
levels of RNAIII, the intracellular effector of the quorumsensing system in S. aureus known to control the expression of a large number of virulence genes [1,36,37].
There are, however, some unanswered questions about
toxin production by SCVs. For example, the toxin release of
SCVs containing the TSST-1 gene or that of other superantigens has as yet not been addressed. Also, it has been
reported that some normal colony-size strains have an
inactive agr gene and low toxin production [35,38]; however, these strains were not assessed for their ability to
persist intracellularly. Furthermore, in various animal
models, a comparison of the virulence of SCVs and normal
S. aureus has shown variable results; although most studies show a reduced virulence of SCVs, few of them demonstrate normal or heightened pathogenicity (reviewed in
Ref. [1]). Yet, in a recent study using a Caenorhabditis
elegans infection model, both clinical SCVs in addition to
hemB- and menD-deficient mutants showed greatly
3
TIMI-617; No of Pages 5
Opinion
reduced virulence when compared to the parental strain of
normal colony size [39]. Of note, the large majority of these
animal studies determined virulence by measuring lethal
doses and fatality rates. Hence, infections by SCVs might
be less severe, although more recurrent or persistent, than
those caused by normal S. aureus.
In summary, SCVs seem to have decreased levels of
functional RNAIII and agr expression, and show very little
toxin production, which can facilitate intracellular survival
by avoiding damage to the host cells. This line of reasoning
is compatible with clinical observations wherein loss of agr
function is associated with persistent infections in the
lungs of cystic fibrosis patients [40], chronic catheter infections [41,42] and long term soft tissue infections [43,44].
Resistance to intracellular host defenses
As mentioned earlier, a reduced membrane potential can
protect SCVs from cationic proteins. Also, because the
activity of the tricarboxylic acid cycle is reduced and catabolism of acetate is thus prevented [2], the carboxylate is
shunted into the production of polysaccharide intercellular
adhesin (PIA), levels of which are elevated in SCVs [45].
PIA is known to contribute to S. aureus resistance against
non-oxidative killing mechanisms of neutrophils [46] and
thus could enable SCVs to resist host cytoplasmic defenses.
Many years ago, Balwit et al. [47] observed that SCVs
are able to escape from phagosomes. In a recent live-cell
imaging study of phagosome maturation, Schröder et al.
[12] provide evidence that certain SCVs can withstand the
bactericidal activity of lysosomes in endothelial cells,
whereas this activity is more effective against normalphenotype staphylococci. Of note, the use of such live-cell
imaging studies represents an interesting approach to
trace the intracellular life of SCVs.
Decreased activation of the host immune system
Bacterial attachment alone is not sufficient to start the
signaling process and the inflammatory response. A more
intimate connection, such as disruption of normal actin
polymerization, is required to set off the cytokine and
chemokine alarm system. Infection of endothelial cells
with S. aureus leads to induction of cytokines, although
different clinical isolates vary greatly in their ability to
elicit a proinflammatory response [48], which might reflect
their virulence properties. Given that certain genes
involved in important virulence properties of S. aureus
(e.g. agr, hla) are inactivated or downregulated in SCVs
and that infected epithelial cells remain viable and show
no signs of disruption [18], it is plausible that SCVs activate the host immune system only weakly or not at all. This
poor stimulation of the immune system is supported by
clinical findings in which SCV infections persist asymptomatically for many years [13,17].
Proliferation in the cytoplasm of non-professional
phagocytes
An assay using human keratinocytes and staphylococci from
a patient with Darier’s disease revealed that >100-fold more
SCVs persisted intracellularly relative to the normal phenotype [18]. Additionally, in a model of endovascular infection used to determine intracellular persistence, >2004
Trends in Microbiology Vol.xxx No.x
Box 1. Questions for future research
Are SCVs part of the normal life cycle of staphylococci?
What are the (genetic) mechanisms for reversion to the normal
phenotype, in particular in vivo?
What determines the differences in duration of intracellular
residence among various staphylococcal strains?
Can intracellular staphylococci migrate directly from one cell to
another adjacent cell?
Does cell division occur with S. aureus being released or
maintained in one or both daughter cells?
Is there a specific and individual-related host factor within nonprofessional phagocytes that enables staphylococci to persist
intracellularly?
fold more SCV (hemB) mutants persisted within cultured
endothelial cells relative to the parent strain [47]. Similar
results were obtained when endothelial cells were infected
with SCVs from cystic fibrosis patients [11]. These data
indicate that SCVs can proliferate within non-professional
phagocytes. The arginine deiminase pathway is markedly
increased in SCVs [3], providing one example of how these
variants use compounds from and within the host cell. The
use of certain amino acids by the intracellular bacteria can
result in a reduced function of key host enzymes involved in
the immune response, such as nitric oxide synthase [3].
Concluding remarks and future directions
Currently, there still is not definitive proof that S. aureus is
a (facultative) intracellular pathogen because there are
still important questions that need to be addressed (Box
1). Yet, the evidence is accumulating that at least certain
strains of S. aureus can persist intracellularly. It is clear
that these staphlyococci must adapt their lifestyle to the
intracellular milieu. SCVs exhibit many properties that
facilitate their attachment to, uptake into and residence
and proliferation within host cells. Moreover, the observations that SCVs can be recovered many symptom-free
weeks – or even years – after an episode of staphylococcal
disease [10,13,17], support the view of S. aureus as a
facultative intracellular pathogen. Furthermore, we
suggest that the S. aureus ability to form either ‘normal’
cells or SCVs could be a key strategy for survival in the
host, either outside or inside its cells.
References
1 Proctor, R.A. et al. (2006) Small colony variants: a pathogenic form of
bacteria that facilitates persistent and recurrent infections. Nat. Rev.
Microbiol. 4, 295–305
2 Chatterjee, I. et al. (2007) Enhanced post-stationary-phase survival of a
clinical thymidine-dependent small-colony variant of Staphylococcus
aureus results from lack of a functional tricarboxylic acid cycle. J.
Bacteriol. 189, 2936–2940
3 Kohler, C. et al. (2003) Physiological characterization of a hemedeficient mutant of Staphylococcus aureus by a proteomic approach.
J. Bacteriol. 185, 6928–6937
4 Seggewiss, J. et al. (2006) Reporter metabolite analysis of
transcriptional profiles of a Staphylococcus aureus strain with
normal phenotype and its isogenic hemB mutant displaying the
small-colony-variant phenotype. J. Bacteriol. 188, 7765–7777
5 von Eiff, C. et al. (2006) Phenotype microarray profiling of
Staphylococcus aureus menD and hemB mutants with the smallcolony-variant phenotype. J. Bacteriol. 188, 687–693
6 Lannergard, J. et al. (2008) Identification of the genetic basis for
clinical menadione-auxotrophic small-colony variant isolates of
TIMI-617; No of Pages 5
Opinion
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
Staphylococcus aureus. Antimicrob. Agents Chemother. 52, 4017–
4022
Chatterjee, I. et al. (2008) In vivo mutations of thymidylate synthase
(encoded by thyA) are responsible for thymidine dependency in clinical
small-colony variants of Staphylococcus aureus. J. Bacteriol. 190, 834–
842
Besier, S. et al. (2007) Molecular analysis of the thymidine-auxotrophic
small colony variant phenotype of Staphylococcus aureus. Int. J. Med.
Microbiol. 297, 217–225
Schaaff, F. et al. (2003) Mutations are involved in emergence of
aminoglycoside-induced small colony variants of Staphylococcus
aureus. Int. J. Med. Microbiol. 293, 427–435
Sendi, P. et al. (2006) Staphylococcus aureus small colony variants in
prosthetic joint infection. Clin. Infect. Dis. 43, 961–967
Kahl, B. et al. (1998) Persistent infection with small colony variant
strains of Staphylococcus aureus in patients with cystic fibrosis. J.
Infect. Dis. 177, 1023–1029
Schroder, A. et al. (2006) Live cell imaging of phagosome maturation in
Staphylococcus aureus infected human endothelial cells: small colony
variants are able to survive in lysosomes. Med. Microbiol. Immunol.
195, 185–194
Proctor, R.A. et al. (1995) Persistent and relapsing infections associated
with small-colony variants of Staphylococcus aureus. Clin. Infect. Dis.
20, 95–102
Garzoni, C. and Kelley, W.L. (2009) Staphylococcus aureus: new
evidence for intracellular persistence Trends Microbiol. 17.
Garzoni, C. et al. (2007) A global view of Staphylococcus aureus whole
genome expression upon internalization in human epithelial cells.
BMC Genomics 8, 171
Clement, S. et al. (2005) Evidence of an intracellular reservoir in the
nasal mucosa of patients with recurrent Staphylococcus aureus
rhinosinusitis. J. Infect. Dis. 192, 1023–1028
Kipp, F. et al. (2003) Detection of Staphylococcus aureus by 16S rRNA
directed in situ hybridisation in a patient with a brain abscess caused
by small colony variants. J. Neurol. Neurosurg. Psychiatry 74, 1000–
1002
von Eiff, C. et al. (2001) Intracellular persistence of Staphylococcus
aureus small-colony variants within keratinocytes: a cause for
antibiotic treatment failure in a patient with darier’s disease. Clin.
Infect. Dis. 32, 1643–1647
von Eiff, C. et al. (1997) Recovery of small colony variants of
Staphylococcus aureus following gentamicin bead placement for
osteomyelitis. Clin. Infect. Dis. 25, 1250–1251
Moisan, H. et al. (2006) Transcription of virulence factors in
Staphylococcus aureus small-colony variants isolated from cystic
fibrosis patients is influenced by SigB. J. Bacteriol. 188, 64–76
Horsburgh, M.J. et al. (2002) sigmaB modulates virulence determinant
expression and stress resistance: characterization of a functional rsbU
strain derived from Staphylococcus aureus 8325-4. J. Bacteriol. 184,
5457–5467
Bulger, R.J. and Bulger, R.E. (1967) Ultrastructure of small colony
variants of a methicillin-resistant Staphylococcus aureus. J. Bacteriol.
94, 1244–1246
Baumert, N. et al. (2002) Physiology and antibiotic susceptibility of
Staphylococcus aureus small colony variants. Microb. Drug Resist. 8,
253–260
Koo, S.P. et al. (1996) Staphylocidal action of thrombin-induced platelet
microbicidal protein is not solely dependent on transmembrane
potential. Infect. Immun. 64, 1070–1074
Peschel, A. (2002) How do bacteria resist human antimicrobial
peptides? Trends Microbiol. 10, 179–186
Lehrer, R.I. and Ganz, T. (1999) Antimicrobial peptides in mammalian
and insect host defence. Curr. Opin. Immunol. 11, 23–27
Vaudaux, P. et al. (2002) Increased expression of clumping factor and
fibronectin-binding proteins by hemB mutants of Staphylococcus
aureus expressing small colony variant phenotypes. Infect. Immun.
70, 5428–5437
Hannigan, G.E. et al. (1996) Regulation of cell adhesion and anchoragedependent growth by a new beta 1-integrin-linked protein kinase.
Nature 379, 91–96
Trends in Microbiology
Vol.xxx No.x
29 Persad, S. and Dedhar, S. (2003) The role of integrin-linked kinase
(ILK) in cancer progression. Cancer Metastasis Rev. 22, 375–384
30 Wang, B. et al. (2006) Integrin-linked kinase is an essential link
between integrins and uptake of bacterial pathogens by epithelial
cells. Cell. Microbiol. 8, 257–266
31 Peterson, M.L. and Schlievert, P.M. (2006) Glycerol monolaurate
inhibits the effects of Gram-positive select agents on eukaryotic
cells. Biochemistry 45, 2387–2397
32 Bayles, K.W. et al. (1998) Intracellular Staphylococcus aureus escapes
the endosome and induces apoptosis in epithelial cells. Infect. Immun.
66, 336–342
33 Menzies, B.E. and Kourteva, I. (1998) Internalization of
Staphylococcus aureus by endothelial cells induces apoptosis. Infect.
Immun. 66, 5994–5998
34 Nuzzo, I. et al. (2000) Apoptosis of human keratinocytes after bacterial
invasion. FEMS Immunol. Med. Microbiol. 27, 235–240
35 Haslinger-Loffler, B. et al. (2005) Multiple virulence factors are
required for Staphylococcus aureus-induced apoptosis in endothelial
cells. Cell. Microbiol. 7, 1087–1097
36 Clements, M.O. et al. (1999) CtaA of Staphylococcus aureus is required
for starvation survival, recovery, and Cytochrome biosynthesis. J.
Bacteriol. 181, 501–507
37 Boisset, S. et al. (2007) Staphylococcus aureus RNAIII coordinately
represses the synthesis of virulence factors and the transcription
regulator Rot by an antisense mechanism. Genes Dev. 21, 1353–1366
38 Krut, O. et al. (2003) Strain-specific association of cytotoxic activity and
virulence of clinical Staphylococcus aureus isolates. Infect. Immun. 71,
2716–2723
39 Sifri, C.D. et al. (2006) Virulence of Staphylococcus aureus small colony
variants in the Caenorhabditis elegans infection model. Infect. Immun.
74, 1091–1096
40 Kahl, B.C. et al. (2005) Thymidine-dependent Staphylococcus aureus
small-colony variants are associated with extensive alterations in
regulator and virulence gene expression profiles. Infect. Immun. 73,
4119–4126
41 Rothfork, J.M. et al. (2003) Fibrinogen depletion attenuates
Staphyloccocus aureus infection by preventing density-dependent
virulence gene up-regulation. J. Immunol. 171, 5389–5395
42 Yarwood, J.M. and Schlievert, P.M. (2003) Quorum sensing in
Staphylococcus infections. J. Clin. Invest. 112, 1620–1625
43 Schwan, W.R. et al. (2003) Loss of hemolysin expression in
Staphylococcus aureus agr mutants correlates with selective
survival during mixed infections in murine abscesses and wounds.
FEMS Immunol. Med. Microbiol. 38, 23–28
44 Beenken, K.E. et al. (2004) Global gene expression in Staphylococcus
aureus biofilms. J. Bacteriol. 186, 4665–4684
45 Al Laham, N. et al. (2007) Augmented expression of polysaccharide
intercellular adhesin in a defined Staphylococcus epidermidis mutant
with the small-colony-variant phenotype. J. Bacteriol. 189, 4494–4501
46 Ulrich, M. et al. (2007) The staphylococcal respiratory response
regulator SrrAB induces ica gene transcription and polysaccharide
intercellular adhesin expression, protecting Staphylococcus aureus
from neutrophil killing under anaerobic growth conditions. Mol.
Microbiol. 65, 1276–1287
47 Balwit, J.M. et al. (1994) Gentamicin-resistant menadione and hemin
auxotrophic Staphylococcus aureus persist within cultured endothelial
cells. J. Infect. Dis. 170, 1033–1037
48 Strindhall, J. et al. (2005) Clinical isolates of Staphylococcus aureus
vary in ability to stimulate cytokine expression in human endothelial
cells. Scand. J. Immunol. 61, 57–62
49 Jensen, J. (1957) Biosynthesis of hematin compounds in a hemin
requiring strain of Micrococcus pyogenes var. aureus. I. The
significance of coenzyme A for the terminal synthesis of catalase. J.
Bacteriol. 73, 324–333
50 Proctor, R.A. et al. (1994) Variant subpopulations of Staphylococcus
aureus as cause of persistent and recurrent infections. Infect. Agents
Dis. 3, 302–312
51 Ross, R.A. and Onderdonk, A.B. (2000) Production of toxic shock
syndrome toxin 1 by Staphylococcus aureus requires both oxygen
and carbon dioxide. Infect. Immun. 68, 5205–5209
5