Landscape analysis of maternal and perinatal infections
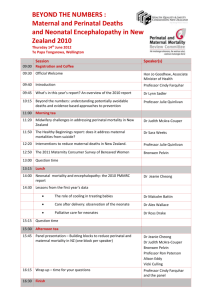
advertisement

Landscape Analysis of Maternal and Perinatal Infections The following Executive Summary is excerpted from a report prepared by PATH, June 2012. Executive Summary Introduction Maternal, perinatal, and newborn infections are important yet under-researched and poorly controlled contributors to developing-country mortality. The lifetime risk of maternal death for a woman in a developing country may be more than 300 times greater than for a woman living in an industrialized country. Africa and Asia account for the vast majority of maternal deaths globally, with sub-Saharan Africa contributing 56 percent and South Asia 29 percent of the global total burden. In absolute numbers, approximately, 287,000 women die each year from complications during pregnancy and childbirth.1 Additionally, up to 20 million women survive their pregnancy but suffer injury, infection, disease, and disability outcomes that are largely preventable.2 Although maternal morbidity is generally poorly understood and little-researched, Fortney and Smith (1996) estimated that the ratio of women with morbidities to maternal mortality was 186:1 in Bangladesh and 251:1 in India.3 Similar to maternal deaths, 98 percent of neonatal deaths occur in low- and middle-income countries (LMICs); however, the figures are even more striking. Within the first 28 days of life, an estimated 3.3 million babies die annually.4 Other estimates indicate that the total number of perinatal deaths, which groups stillbirths with early neonatal deaths, is as high as 5.9 million deaths annually.5 The major causes of maternal mortality and morbidity are fairly well understood, with the largest proportion of deaths accounted for by five obstetric causes, including hemorrhage, hypertensive disorders often linked to eclampsia, septic abortion, obstructed labor, and puerperal sepsis. Maternal infections (which include puerperal sepsis as well as infections incidental to and/or aggravated by pregnancy and puerperium) are one of the most understudied yet important contributors to morbidity and mortality of both the mother and neonate during the pregnancy, intrapartum, and early postpartum periods in developing countries. Infections are implicated in 15 percent or more of maternal deaths, and 36 percent or more of neonatal deaths.6 Estimates of perinatal and newborn deaths attributed to infection are underreported, as deaths associated with infection among premature and/or low-birthweight babies are often recorded as deaths due to prematurity. Intrauterine infection is strongly associated with preterm birth7 and is recognized as being one of the most important and potentially preventable causes of early preterm birth. Infections are thought to be responsible for up to 50 percent of extreme preterm births of less than 28 weeks of gestation, while preterm birth associated with infection is rare beyond 34 weeks of gestation. Low birth weight, closely associated with intrauterine infection, is the underlying factor in 60 to 80 percent of neonatal deaths.8 Furthermore, maternal infection has been identified as an underlying risk factor of intrapartum hypoxia and related sequelae.9 PATH: Landscape Analysis of Maternal and Perinatal Infections i A broad array of pathogens contributes to maternal infections that have heterogeneous modes of transmission, treatment requirements, and sequelae for mother and baby. The major categories of pathogens that impact mother and baby are sexually transmitted infections (STIs), vaginally acquired nonsexually transmitted infections, urinary tract infections (UTIs), and environmentally acquired Gramnegative bacteria acquired during labor and delivery. Risk and outcomes associated with these groups of pathogens are often modulated by co-infection with other diseases such as HIV, tuberculosis, malaria, and viral hepatitis in these women. Although in many cases the reporting systems are weak and subject to inaccuracies in areas with high perinatal and neonatal mortality, it is clear that infections, including sepsis, pneumonia, tetanus, and diarrhea, account for the largest proportion of neonatal deaths globally. In high-income countries, early onset neonatal infection (during the first week of life) is often attributed to maternal infections of the genital or urinary tract, while those that occur after the first week of life are often attributed to environmentally acquired infections either from the home or nosocomially.10 Furthermore, vaginally acquired nonsexually transmitted infections, such as bacterial vaginosis, are implicated in the pathogenesis of premature birth. In LMICs a review of the available evidence presents a different clinical picture for early-onset infections during the first week of life—an overwhelming majority of Gram-negative organisms and a high frequency of Staphylococcus aureus.11,12 This pattern of pathogens suggests that early infections in the first week of life in LMICs may be acquired predominantly from the hospital or community environment due to poor hygienic practices during delivery and postnatal care, rather than from maternal exposure as conventionally understood in high-income countries. Beyond the first week, the most common isolates from community-acquired infections are E. coli; group B Streptococcus; and S. aureus, as well as Streptococcus pneumoniae, S. pyogenes, and Salmonella species.12 Although data from LMICs are limited in both quality and quantity, the available information speaks to the need for state-of-the-art microbiologic or molecular diagnostics to reliably define the etiology of serious infections and to devise community-based tools that lead to better control of these infections in high-mortality low- and middle-income settings. In the developed world, diagnostic tools are laboratorybased, allow for rapid return of results in some cases, and can have impact on control of pathogens associated with poor maternal and neonatal health outcomes. Unfortunately, the currently available diagnostic tools and the systems that deliver them are not configured to provide actionable information for effective care of mothers and babies in low-resource settings. Additionally, physical proximity to health services; the lack of qualified staff; cultural beliefs among families, especially in low-income areas; and financial barriers to accessing health care may inhibit efficient uptake of services which could prevent maternal and neonatal death. The Integrated Management of Pregnancy and Childbirth (IMPAC) calls for an integrated policy, technical, and managerial approach to maternal and neonatal survival and health improvement.13 Central to the IMPAC strategy is the rational provision of effective disease prevention and health outcome, detection and management, and treatment tools during a continuum of care that begins prior to conception and continues through childbirth for mother and baby. This strategy requires a movement toward earlier, more frequent, and more impactful interactions between trained clinicians and mothers, and subsequently their babies, and investment in the health system, healthcare workers, and in encouraging pregnant women to access services. However, severe human resource constraints in many LMICs, especially in rural areas and among impoverished or ethnic or religious minority populations, prevent poorer mothers and newborns from accessing care by trained clinicians, contributing to remarkable inequities in health outcomes within individual countries. Improved diagnostics that target biomarkers for pathogens and/or the specific and relevant host immune responses in developing countries may improve the ability of health workers to manage infections at or near the point of care with resultant improvement in equity. It is unclear at present what combination of new diagnostic and therapeutic tools, human resources, timing, and setting of patient and health worker interaction will provide the most impact in terms of mortality and morbidity reduction. The identification and management of maternal infections has important implications for pregnancy outcomes for both mothers and neonates. In addition to the puerperal sepsis and serious infections, with resultant maternal death and morbidity, maternal infections during pregnancy are implicated in the pathway to preterm births, stillbirths, and early infection of preterm and term neonates. Maternal mortality from infection remains high in developing countries due to inadequate quality case management and infection control. In both developing and developed countries, there is limited understanding of the role of early infection during pregnancy in eventual pregnancy outcomes for mothers and babies. Diagnostics that detect infection early through direct pathogen detection, specific host response, or markers of immune system regulation; guide treatment; and expand care opportunities are lacking in most clinical settings in developing countries. This landscape exercise sought to achieve the following three primary objectives: 1. To consolidate and evaluate global evidence on the burden of pathogens associated with serious maternal and perinatal infections and identify promising diagnostic tests and platforms for detection of these infections. 2. To analyze country-level factors that support or inhibit the uptake of maternal and neonatal infection diagnostic control measures. 3. To integrate results from global evidence and country-level research and identify opportunities, barriers, and gaps in knowledge around promising diagnostics that support control of maternal and perinatal infections. To this end, we evaluated and reconciled three bodies of evidence: (1) epidemiological evidence on priority pathogens and their association with other important infectious causes of morbidity and mortality (e.g., HIV, TB, malaria, hepatitis); (2) academic, commercial, and clinical evidence on potentially impactful diagnostic, management, and treatment modalities; and (3) country-based contextual evidence on the needs, feasibility, and acceptability of existing and novel maternal, perinatal, and neonatal infection management approaches. Project activities began in 2010 and spanned a two-year period. They included a desk-based literature review around the pathogen and diagnostic landscape and primary research in two high-burden countries (Bangladesh and Uganda), one low-HIV-prevalence setting, and one high-HIV-prevalence setting. PATH: Landscape Analysis of Maternal and Perinatal Infections iii Collaborating partners included the Seattle-based Global Alliance for the Prevention of Prematurity and Stillbirth (GAPPS), International Center for Diarrhoeal Disease Research, Bangladesh (ICDDR,B), and the Makarere University School of Public Health, Uganda. This report includes the results of three separate studies designed to address the specific objectives listed above. Chapter 1 provides an overview of the etiology and incidence of maternal infections to identify opportunities and challenges for screening, treatment, and prevention. Chapter 2 presents findings from a literature review of current and potential diagnostic technologies for the syndromes and pathogens delineated in Chapter 1. Chapter 3 details the results of primary research undertaken in Bangladesh and Uganda around community and provider receptivity and perceived barriers to potential diagnostic testing during the continuum of care. Additionally, at the request of the Bill & Melinda Gates Foundation, some exploratory work was undertaken around the commercial feasibility and health impact of “bundling” diagnostics. Chapter 4 presents findings of a landscape study of manufacturers producing rapid diagnostic tests for use during antenatal and peripartum care. Chapter 5 provides the results of a preliminary modeling exercise to assess the scope and potential of improved antenatal diagnostic testing for HIV and malaria in two sub-Saharan African settings. Summary of Findings and Conclusions Landscape Review of Serious and Life-Threatening Maternal Infections Serious infections during pregnancy are an important preventable cause of maternal and neonatal mortality and morbidity. Our literature review revealed significant gaps in the understanding of the microbiology of life-threatening maternal infections in low-resource settings, and the need for rapid recognition and treatment call for clinical, syndromic management of infections. Five life-threatening clinical syndromes account for the majority of maternal deaths and adverse maternal and neonatal outcomes. These include chorioamnionitis and postpartum endometritus (together referred to as puerperal sepsis), pyelonephritis, septic abortion, and rapidly progressive soft tissue infections. These syndromes occur at distinct time points during pregnancy, offering specific opportunities for “bundled interventions” for screening, prevention, and treatment. To facilitate these needs we recommend: Improved diagnostics that target biomarkers for pathogens and/or specific and relevant host immune response to improve the ability of health workers to recognize and to manage infections at or near the point of care. Point-of-care screening for selected pathogens across the continuum of pregnancy care. Development and validation of context-specific diagnostic and treatment algorithms suitable for both community and facility health care workers. Ongoing microbiologic surveillance surveys to identify shifts in microbial flora or emergence of microbial resistance. Nonobstetric infections, including malaria, HIV, tuberculosis, and curable STIs are also recognized as significant contributors to maternal morbidity and mortality. Literature Review of Diagnostics Technologies for Common Pathogens Associated With Maternal Infection During Pregnancy Our landscape review of the different diagnostic technologies, their performance, and the types of specimens required to identify the common pathogens associated with maternal infections during pregnancy focused on the diagnostic methods used to detect the primary pathogens associated with UTIs, septic abortion, chorioamnionitis, endometritis, soft tissue infection, and the risk of vertical transmission of group B Streptococcus. While rapid diagnostic tests are available for the diagnosis of maternal infections and syndromes, they generally require confirmatory testing. The available literature is heavily weighted in favor of primary pathogens of concern to developed world health care, where infrastructure, trained staff, and good logistics permit technology of much greater complexity or procedures that would be high-risk in low-resource settings (e.g., amniocentesis). Fully integrated technologies are emerging for nucleic-acid based diagnosis, but these are currently prohibitively expensive and infrastructure-dependent, missing the majority of the intended population in this project. As with many other diseases, biomarkers have potential, but the identification of optimal ones to strongly indicate infection is difficult for a variety of reasons. Some potential technologies were identified as having potential, but these are still in development and none are expected to be on or close to market in the next three years. Given the fact that diagnostics, including rapid diagnostic tests, for STIs were covered by other work in our project, they were not a focus of this review. Landscape Assessment of Community and Providers Findings from our landscape assessment of providers and communities indicate that women seek antenatal care (ANC) with a formal provider at least once in their pregnancy. Return visits are rare unless dictated by an emergency. Where there is a strong perception of risks and benefits of diagnostic testing, as in the case of HIV in Uganda, it often becomes a major driver for formal ANC. Traditional birth attendants continue to be the provider of choice for labor and delivery care. The postpartum period constitutes an important cultural milestone and is generally viewed as being outside the continuum of care, with little perceived need for biomedical care. Husbands and mothers-in-law significantly shape women’s behaviors around care seeking. Cost as well as physical and cultural access to facilities act as significant barriers to care seeking. Diagnostic testing during ANC was generally viewed positively; however, women and their families would prefer that any proposed diagnostic tests be administered by skilled and trained providers. Communities expressed reservations in providing biological specimens during labor and the immediate postpartum period. Families expressed almost universal preference for immediate turnaround of results, though some concerns were expressed about “quality” with too rapid a return of results. Regarding care provision, providers currently rely on physical examination and signs and symptoms for diagnoses. While providers are familiar with the concept of diagnostic testing, there is limited use of diagnostics in maternal health care, with HIV testing in Uganda being a notable exception. Providers had strong recognition of logistic limitations, and while they saw a definite advantage of diagnostic testing in terms of patient management, they also expressed reservations about the additional workload this would necessitate. PATH: Landscape Analysis of Maternal and Perinatal Infections v Findings suggest diagnostic testing may provide an opportunity to optimize ANC by utilizing bundled or multiplexed tests that can be administered together to optimize what may often be a single antenatal contact. This would have the added advantage of providing better perceptions of the quality of care received and potentially additional uptake of follow-on ANC. Landscape Analysis of Maternal and Perinatal Infection Diagnostic Manufacturers At the request of the Foundation, PATH also conducted a landscape study of potential manufacturing partners to identify and engage diagnostics companies capable of producing improved infectious disease rapid diagnostic tests for use during antenatal care in low-resource settings. Secondary research and contact with more than 50 potential partner companies indicate that the most impactful way forward is in developing serology test bundles for HIV, malaria, syphilis, and/or hepatitis B. Not only is there a wide array of capable companies and technologies in this space, but there appear to be clear paths forward to introduce impactful products in the near term. The landscape is less promising for UTIs, where few products are available in the short term to meet all needs of women in low-resource settings. A small but well defined group of tests exists for anemia, with known issues related to performance and logistics. Several available tests are available for premature rupture of membranes diagnosis, but it is unclear how to gauge their value against the high costs involved. More work around analyzing current needs is required to gauge the impact of a new product. It seems clear that a single manufacturer or product will not necessarily best serve every low-resource market or region. A strategy that incorporates multiple products suited to specific markets, aggressively implementing short-term solutions while developing longer-term solutions, would be appropriate. Finally, there is a clear need for an overall commercial plan to define the markets in the context of the product concepts. As a next step, knowledge gaps around the specific clinical needs in the regions of interest, specific product criteria, and market information need to be filled in order to construct a clear and attractive business case that would be the foundation for negotiations with manufacturing partners. Modeling the Potential Impact of Improved Diagnostic Testing During Pregnancy Preliminary modeling was undertaken in two geographical settings—Mali in West Africa, in which malaria prevalence is high but HIV prevalence is low, and Malawi in Southern Africa, where both malaria and HIV prevalence are high. For HIV, results demonstrate that there remain large numbers of women attending ANC who are HIV-positive but have not received an HIV test, and hence there is scope to improve universal HIV testing with improved diagnostics. The potential impact of improved diagnosis on maternal life-years saved and in preventing onward transmission to infants is greatest in rural areas due to the large number of women residing in such areas. For malaria, the current rates of uptake of malaria testing depend on access to ANC, which we found varied in the two countries. In Malawi, where attendance at ANC is high, there was substantial opportunity to increase diagnostic testing and treatment or prophylaxis. In Mali, while the medical benefits of improving diagnosis and treatment remain high, access to ANC first needs to be improved, particularly in rural areas, where the malaria burden is the highest but attendance at ANC remains low. In countries with high HIV prevalence, the risk of malaria co-infection during pregnancy can be substantial. In Malawi, we found women who did not receive the recommended malaria intervention during their previous pregnancy to be more likely to be HIV-positive, with a large proportion of these women being unaware of their HIV status. Thus, improved combined diagnosis of HIV and malaria in this setting has significant potential to improve health outcomes. 1 UNFPA, UNICEF, WHO, World Bank (2012) Trends in Maternal Mortality: 1990 to 2010. Available at: http://www.unfpa.org/webdav/site/global/shared/documents/publications/2012/Trends_in_maternal_mortality_A41.pdf. Last accessed June 11, 2012. 2 UK All Party Parliamentary Group on Population, Development and Reproductive Health. Better Off Dead? A report on maternal morbidity from the UK All Party Parliamentary Group on Population, Development and Reproductive Health. 2009. Available at: http://www.appgpopdevrh.org.uk/Publications/Maternal%20Morbidity%20Hearings/Maternal%20Morbidity%20Report%20%20FINAL%2009.pdf. 3 Fortney JA, Smith JB. The base of the iceberg: prevalence and perceptions of maternal morbidity in four developing countries. The Maternal Morbidity Network. Research Triangle Park, North Carolina: Family Health International (FHI), Maternal and Neonatal Health Center; 1996. 4 Oestergaard MZ, Inoue M, Yoshida S, Mahanani WR, Gore FM, et al. Neonatal Mortality Levels for 193 Countries in 2009 with Trends since 1990: A Systematic Analysis of Progress, Projections, and Priorities. PLoS Medicine. 2011;8(8): e1001080. doi:10.1371/journal.pmed.1001080. 5 Zupan J, Aahman E. Neonatal and perinatal mortality: country, regional and global estimates 2004 developed by WHO. Geneva: World Health Organization; 2007. 6 UNICEF. The State of the World’s Children 2009: Maternal and Newborn Health. Chapter 1, Maternal and Newborn Health: Where We Stand. New York: UNICEF; 2008. 7 Goldenberg RL, Hauth JC, Andrews WW. Intrauterine infection and preterm delivery. New England Journal of Medicine. 2000;342(20):1550–1557. 8 Bang A, Reddy MH, Deshmukh MD. Child mortality in Maharashtra. Economic Political Weekly. 2002;37:4947– 4965. 9 Lee AC, Mullany LC, Tielsch JM, et al. Risk factors for birth asphyxia mortality in a community-based setting in southern Nepal: a prospective cohort study. Pediatrics. 2008;121(5):1381–1390. 10 Klein JO. Bacterial sepsis and meningitis. In: Remington JS, Klein JO, eds. Infectious Diseases of the Fetus, Newborn, and Infants. 5th ed. Philadelphia, PA: WB Saunders; 2001:943–984. 11 Zaidi AK, Thaver D, Syed AA, Khan TS. Pathogens associated with sepsis in newborns and young infants in developing countries. The Pediatric Infectious Disease Journal. 2009;28(1)S10–15. 12 Zaidi AK, Huskins WC, Thaver D, et al. Hospital-acquired neonatal infections in developing countries. The Lancet. 2005;365:1175–1188. 13 World Health Organization. Department of Making Pregnancy Safer. WHO Recommended Interventions for Improving Maternal and Newborn Health. Second Edition. Geneva: WHO; 2009. PATH: Landscape Analysis of Maternal and Perinatal Infections vii