Transaction Processing
advertisement
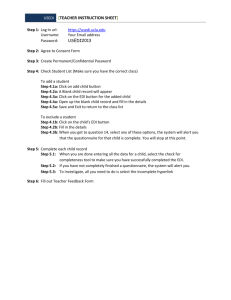
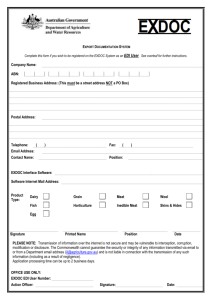
Chapter IV Transaction Processing The Enterprise EDI Gateway/Clearinghouse is critical to the process of exchanging electronic transactions with Trading Partners. Its programs expedite the movement of transactions to their destination by performing the following functions: HIPAA Syntax Edits Control Segment (File) Balancing Return of 997 Functional Acknowledgments Routing of Transactions Although the Enterprise EDI Gateway/Clearinghouse is used for all HIPAA transactions, this chapter focuses on how it relates to the 837 Health Care Claim transactions. Adjudication through the Enterprise EDI Gateway/Clearinghouse is a process by which a claim passes through Level 1 and Level 2 edits to determine proper payment liability. The diagram in this chapter illustrates the process. ©Anthem Page 1 of 3 Release 05 (January 2009) EDI User Guide IV-Transaction Processing Edit Process Process – 837 Health Care Claim Enterprise EDI Gateway/ Clearinghouse Pre-LEVEL 1 2 5 TA1 Report 837 Health Care Claim Edited LEVEL 1 3 997 Functional Acknowledgment 6 LEVEL 2 4 1 835 Electronic Remittance 864 Text Message Transaction (Level 2 Status Report) 837 Health Care Claim g Tradin r Partne Anthem Trading Partne Adjudication of a claim includes the following steps: Submit your 837 Health Care Claims file to the Enterprise EDI Gateway/Clearinghouse. The Enterprise EDI Gateway/Clearinghouse returns a TA1 Report only if an error occurs with enveloping and duplicate GS control numbers. The Enterprise EDI Gateway/Clearinghouse returns a 997 Functional Acknowledgment to your mailbox. Any Level 1 errors that occur will be indicated on this report. NOTE: Contact your EDI Representative if you do not receive this acknowledgment after you submit your claims file. The Enterprise EDI Gateway/Clearinghouse returns an 864 Text Message Transaction (Level 2 Status Report) to your mailbox. This report will show any Level 2 errors that occurs. ©Anthem The Enterprise EDI Gateway/Clearinghouse submits the edited 837 Health Care Claims file, formatted to HIPAA standards, to Anthem. (Refer to Chapter VI, Submitting and Receiving Transactions, for more information on submitting and receiving.) After Anthem receives the 837 Health Care Claims file and is processed, an 835 electronic remittance is returned to your mailbox via the Enterprise EDI Gateway/Clearinghouse. (Additional set up is required to receive an 835 electronic remittance.) If there are errors, you need to make the necessary corrections and resubmit your 837 Health Care Claim file to the Enterprise EDI Gateway/Clearinghouse for claims processing. Page 2 of 3 Release 05 (January 2009) EDI User Guide IV-Transaction Processing Edit Levels The Strategic National Implementation Process (SNIP) White Paper on Front End Edits recommends two levels of reporting: 1) Level 1: Transaction Format (X12) Syntax Checking 2) Level 2: HIPAA Implementation Guide Compliance Checking NOTE: “There are no reporting mechanisms required by the Transactions and Code Sets Final Rule. It is imperative that an accurate audit trail be maintained to provide relevant feedback between Trading Partners. Today, the reporting of front-end edits between Trading Partners is inconsistent and incomplete. To solidify the audit process and add value to the transaction processing cycle, it is critical to include complete, accurate and consistent reporting mechanisms between trading partners.” —Front End Edits White Paper, Strategic National Implementation Process (SNIP) Level 1 Edits Level 1 edits look for correct syntax according to the X12 Control and Transaction standards (see below). Errors that occur are reported in the 997 Functional Acknowledgment. 1) Interchange identification (ISA/IEA) Correct length of ISA (106 bytes, fixed length) Legal separators and terminators Valid Receiver and Sender IDs 2) Functional Group Identification (GS/GE) Data content (Control numbers, GE count, group ID, version) Valid application IDs 3) Transaction Set Syntax (ST/SE) Valid data types Valid data separators and terminators Valid transaction and segment IDs Overall data content and SE totals Level 2 Edits Level 2 edits check for compliance with the HIPAA Implementation Guide (see below). Errors that occur are reported on the 864 Text Message Transaction (Level 2 Status Report). ©Anthem 1) Variables based on the Implementation Guide 2) Code Sets 3) Looping Structures 4) Situational Edits (inter-segment dependencies) 5) Implementation Guide Balancing Rules 6) Other Implementation Guide specific edits and requirements 7) Member ID lookup 8) Provider ID lookup 9) Business Rules edits 10) Trading Partner specific edits Page 3 of 3 Release 05 (January 2009)