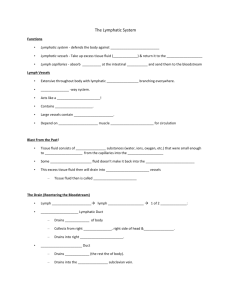
The Lymphatic System
advertisement

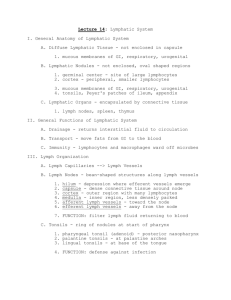
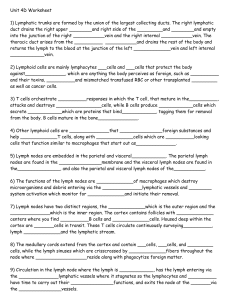
The Lymphatic System Inflammation: is the response triggered whenever body tissues are injured. It occurs following physical trauma, infection, or irritation, and effectively delivers white blood cells to the area. The purpose of inflammation is to: 1) Prevent the spread of damaging agents to nearby tissues 2) Dispose of pathogens and cell debris 3) Prepare for regeneration The four signs of acute inflammation are 1) Redness 2) Heat 3) Swelling 4) Pain Inflammation Continued • Chemical messengers such as Histamine, Bradykinin and prostaglandins released by damaged tissue and WBCs cause vasodilation and increased capillary permeability • This increases the delivery of phagocytes to the injured area, that ultimately leads to tissue clean-up and healing • Increased vasodilation causes Heat and Redness at the site of inflammation, while increased capillary permeability causes Pain and Swelling Inflammation Continued Tissue Injury Release of Histamine, Bradykinin and PGs Vasodilation Capillary Permeability Heat and Redness Capillaries leak fluid and protein (exudate) Increased metabolic rate, oxygen and nutrient delivery Pain and Swelling Release of Leukocytosis inducing factor Chemotaxis Increased WBCs in blood PMNs and monocytes migrate to injured area Blood clot ‘walls-off’ injured area Healing Phagocytosis by PMNs and macrophages The Complement System Antibody bound to an antigen Bacterial surface Classical Pathway Alternative Pathway Complement Proteins Stimulate Inflammation Enhance Phagocytosis (Opsonins) Bacterial Lysis • The complement proteins are blood plasma proteins that help us defend against bacterial infections • The complement proteins are activated by an antibody-antigen complex (Classical pathway) or by the surface of a bacterial membrane (Alternative pathway) • Once activated, complement proteins stimulate inflammation, enhance phagocytosis, and lysis bacteria Immunity Antigen: Substances that can mobilize our immune systems, leading to an immune response. Most often antigens are large molecules (natural or artificial) that are not normally present in our bodies. They are the ultimate target of the immune system. Antibody: Also called immunoglobulins (Ig), antibodies are soluble proteins secreted by activated B cells or plasma cells in response to exposure to an antigen. Antibodies are capable of binding with high specificity to that antigen. The 3 Principles of Immunity: 1) It is antigen-specific 2) It is systemic 3) It has ‘memory’ Our immune systems are divided into 2 different branches: 1) Humoral (antibody-mediated) immunity involving B cell lymphocytes 2) Cellular immunity involving T cell lymphocytes Differentiation of Lymphocytes • Lymphocytes begin their lives as stem cells in the red bone marrow. • They enter the blood before they are fully mature. • B cells (plasma cells) mature in the blood and form the Humoral or antibodyproducing arm of our immune system. Most mature B cells reside in the lymph organs. • T cells complete their maturation in the thymus gland. Following maturation they reside in lymph organs and some in the blood. T cells comprise our Cellular mediated immune system. • Natural killer cells are similar to T cells, but do not require the thymus for maturation. (2) Humoral Immunity • When a B cell is exposed to an antigen, the B cell proliferates (clones) and becomes a Plasma Cell or a Memory Cell • Plasma Cells are antibody ‘factories’ that release antibodies in the blood • On the subsequent exposure, the Memory Cells rapidly produces many more antibodies • The Secondary response is greater than the Primary Response Antibodies • Once released into the blood, antibodies can bind to the antigen and/or the invading organism • This leads to phagocytosis, inflammation or cell lysis of the invading organism (2) • Antibodies achieve these effects by: 1) Neutralization 2) Enhancing inflammation 3) Activating the complement system or Natural Killer (NK) cells Cellular Immunity (2) • In cellular immunity, an antigen is engulfed by a macrophage, which then presents the antigen to a Helper T cell. The Helper T can then ‘activate’ a Cytotoxic (Killer) T cells and B cells. Cytotoxic T cells then seek viral infected cells. T cells also form ‘memory cells’. • Cellular immunity is particularly important in defending against a viral infection and cancerous cells . Cellular Immunity Continued (7) • Cytotoxic T-cells are activated by interleukin 2 (IL-2). • Activated T-cells search the body for an infected cell that is presenting an antigen that matches their receptor. • Once the T-cell receptor binds to the viral antigen, the infected cell initiates ‘programmed cell dealth’, also called apoptosis. This is achieved by the insertion proteins called perforins into the viral infected cell’s membrane, creating a pore so that the cytotoxic T-cell can insert enzymes into the infected cell or by the binding of a cell surface protein called Fas. (7) Lymph Vessels • Lymph vessels begin as openended capillaries that are interspersed between the blood capillaries • The lymph vessels drain the excess ISF and return this fluid to the systemic circulation, thus helping to maintain the blood volume • Proteins, bacteria, viruses, and cell debris are carried in the lymph, especially in areas of inflammation • Before returning to the blood stream, the lymph is passed through Lymph Nodes, to be cleansed by white blood cells (1) Lymph Nodes • Before entering the blood stream, lymph is passed through Lymph Nodes to be cleansed. • Lymph Nodes contain Macrophages and Lymphocytes which remove bacteria, viruses, cell debris, and even cancerous cells • During infection Lymph Nodes can become swollen as they ‘trap’ incoming lymph while pathogens are destroyed • The Nodes are localized in three regions of our body: Cervical, Axillary, and Inguinal (2) Other Lymph Organs Tonsils: The tonsils are similar to lymph nodes, as they contain white blood cells. The tonsils act to cleanse bacteria, viruses and debris that enter our oral cavity. There are 3 pairs of tonsils and they are named according to there location: Palatine, Lingual, and Pharyngeal (adenoids) Spleen: In addition to destroying old RBCs, the spleen acts to filter bacteria, viruses and other debris by containing macrophages and lymphocytes Thymus: The thymus gland function to release Thymosin, a hormone that aids in T cell differentiation MALT: mucosa-associated lymphatic tissue serve a similar function as Nodes (eg. Tonsils, Peyer’s patches, the appendix and bronchi nodules) (2) The Tonsils Pharyngeal (Adenoid) Palatine Lingual (1)