Digestive tract Accessory organs
advertisement

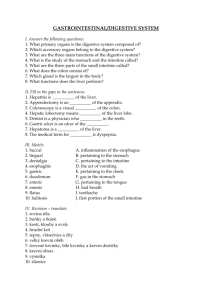
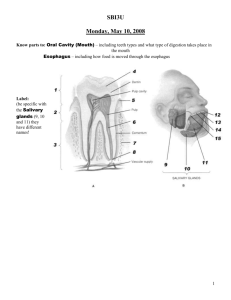
Digestive System • The digestive system can be divided into two major parts: Digestive System The process of chemically and physically breaking down foods into simpler forms that can be absorbed is called digestion. Digestive tract The digestive tract is the tube that extends from the mouth to the anus, and it consists of the – (1) mouth, – (2) pharynx, – (3) esophagus, – (4) stomach, – (5) small intestine, and – (6) large intestine. – (1) the alimentary canal (gastrointestinal, or digestive tract) and – (2) the accessory organs. The digestive tract is the tube that extends from the mouth to the anus, and it consists of the (1) mouth, (2) pharynx, (3) esophagus, (4) stomach, (5) small intestine, and (6) large intestine. The accessory organs include the (1) teeth, (2) tongue, (3) salivary glands, (4) liver, (5) gallbladder, and (6) pancreas. Accessory organs The accessory organs include the – (1) teeth, – (2) tongue, – (3) salivary glands, – (4) liver, – (5) gallbladder, and – (6) pancreas. Digestive System Overview • The oral cavity (mouth) contains the tongue and the teeth. • Salivary glands produce saliva, a mixture of mucus and enzyme (amylase), and empty into the oral cavity. • Located behind the mouth is the throat (pharynx). The pharynx is divided into three parts, and the two digestive components are the (1) oral pharynx and the (2) laryngopharynx, which function in swallowing and the passage of food. Figure 26.1 Illustration showing the design and structures of the digestive system. 1 Digestive System Overview Digestive System Overview • Swallowing forces food into the esophagus, the tube that descends from the pharynx to the stomach. • The small intestine is a long twisted tube that extends from the stomach to the large intestine. • The large intestine is divided into the (1) cecum, (2) appendix, (3) colon, (4) rectum, and (5) anal canal. – The duodenum receives a liquid mixture of food from the stomach called chyme and secretions from the liver and the pancreas. – The liver produces bile which contains bile salts for the emulsification of fats. – The pancreas produces pancreatic juice which contains two major components, (1) enzymes for digestion and (2) bicarbonate ions for adjusting the acidic chyme toward neutral. – The ileocecal valve regulates the emptying of the small intestine. Digestive System Overview – The sigmoid colon joins the rectum, which terminates at the anal canal. The short anal canal terminates at the opening to the outside called the anus. • The wall of the alimentary canal is organized from the esophagus to the anal canal into four distinctive layers. Located from the inside to the outside, the layers of the wall are called the – – – – (1) mucosa, (2) submucosa, (3) muscularis externa, and (4) serosa. MUCOSA • The mucosa of the digestive tract is its innermost layer, a mucous membrane that opens to the body’s exterior. – The mucosa consists of an epithelial lining, under which is attached a layer of loose connective tissue called the lamina propria. Under the lamina propria is a layer of smooth muscle called the muscularis mucosae. • Regions of the alimentary canal show variations in the structure of the mucosa that relate to its functions, which include protection, secretion, and absorption. Figure 26.2 Illustration showing the organization of the layers of the digestive tract. Figure 26.3 Photograph of a crosssection of the small intestine showing the organization of the layers of the digestive tract. MUCOSA • Stratified Squamous Epithelium – The mucosal epithelium of the mouth, esophagus, and the anal canal is stratified squamous epithelium which functions in protection. Figure 26.4 Illustration of stratified squamous epithelium of the esophagus. Figure 26.5 Low power photograph of stratified squamous epithelium of the esophagus. Stratified squamous epithelium functions as a protective epithelium. MUCOSA • Simple Columnar Epithelium The mucosal epithelium of the stomach, small intestine, large intestine, and rectum is simple columnar epithelium. – Often the exposed (apical) plasma membranes of the columnar cells are modified into projections called microvilli. Microvilli function to increase the surface area of the exposed (apical) plasma membranes. – The apical plasma membranes of the columnar cells contain digestive enzymes and function in the absorption of the end products of digestion. Associated with the epithelium are numerous goblet cells. – A goblet cell functions as a mucous gland. 2 •Simple Columnar Epithelium Modifications of the Mucosa Figure 26.6 Illustration of simple columnar epithelium of the small intestine. Figure 26.7 High power photograph of simple columnar epithelium of the small intestine. In addition to forming a protective membrane, the epithelium’s cells have microvilli that contain digestive enzymes and function in absorption. In addition to having a layer of epithelium, the mucosae of the stomach, small intestine, and large intestine are modified for digestive functions. Mucosa of the Stomach • A modification of the stomach’s mucosa is the presence of gastric glands. Figure 26.8 The mucosa of the stomach is modified to contain gastric glands, which produce gastric juice and hormones. Mucosa of the Small Intestine • Two modifications of the small intestine’s mucosa are the presence of villi and intestinal glands (crypts). Figure 26.9 The mucosa of the small intestine is modified to form villi and contains intestinal glands. Villi increase the mucosal surface area and gastric glands produce intestinal juice. Mucosa of the Large Intestine A modification of the large intestine’s mucosa is the presence of intestinal glands which function in absorption and secretion of mucus. SUBMUCOSA • The submucosa consists of loose connective tissue. It contains abundant blood vessels, lymphatics, and nerves. Only slight variations are seen in the various regions of the alimentary canal. Figure 26.10 The mucosa of the large intestine is modified to contain intestinal glands which function in absorption and secretion of mucus. 3 MUSCULARIS EXTERNA • MUSCULARIS EXTERNA The muscularis externa is the muscular layer located to the outside of the submucosa. It functions in the mixing and propulsion movements of the contents of the alimentary canal. – The mouth, pharynx, and upper esophagus have various percentages of skeletal muscle tissue for voluntary movements such as chewing and swallowing. – From the lower esophagus to the anus, the muscularis externa consists of smooth muscle, under control of the autonomic nervous system. – Except for the stomach, the muscularis is arranged in two layers, an inner circular layer and an outer longitudinal layer. The stomach has an additional layer, located inside of the circular layer, called the oblique layer. Figure 26.11 The muscularis externa is the muscular layer located to the outside of the submucosa. Except for the stomach, the muscularis externa consists of two muscular layers that function in the mixing and propulsion movements of the contents of the alimentary canal. MUSCULARIS EXTERNA MUSCULARIS EXTERNA • Peristalsis – Peristalsis is the wavelike muscular contractions that produce forward movement of the organ’s internal contents. Peristalsis of the digestive tract is produced by the sequential contraction of the smooth muscles of the muscularis externa. Contraction of the circular layer constricts the lumen (cavity) and contraction of the longitudinal layer dilates the lumen (cavity). • Segmentation – Segmentation is the process where non-sequential segments of the digestive tract contract resulting in the mixing of the internal contents. The contraction of each segment pushes a portion of the contents forward and a portion backward. Thus, the contents are mixed, rather than pushed in a forward direction. Figure 26.12 Peristalsis is the wavelike muscular contractions that produce forward movement of the organ’s internal contents. Segmentation is the nonsequential contraction of segments of the tract that results in the forward and backward movements (mixing) of the contents. MUSCULARIS EXTERNA Serosa • Except for the esophagus, the outermost layer of the alimentary canal is called the serosa (visceral peritoneum). – The serosa consists of loose connective tissue and an epithelium that produces a lubricating serous fluid. – The esophagus is lined by a layer of connective tissue called the adventitia. The adventitia connects the esophagus to surrounding tissues in the thoracic cavity. Figure 26.13 An X-ray of the upper digestive tract shows peristaltic waves of the stomach. Peristaltic waves of the stomach move the contents of the stomach (chyme) into the duodenum. 4 Serosa The Peritoneum and its Cavity The peritoneum is the serous membrane that lines the abdominal cavity and continues inward to cover its viscera, the internal organs. Figure 26.14 The serosa is the outer layer of the digestive tract (except for the esophagus). The serosa, also called the visceral peritoneum, functions in the maintenance of the serous fluid in the abdominopelvic cavity. The Peritoneum and its Cavity • The peritoneum consists of a layer of simple squamous epithelium (mesothelium) and forms two layers. • The outer layer lines the abdominal wall and is called the parietal peritoneum. • The inner layer covers the organs of the abdominal cavity and is called the visceral peritoneum. • The space between the two layers, the peritoneal cavity, contains a film of serous fluid. Mesenteries • When organs extend into the peritoneal cavity, the peritoneum is formed into the mesenteries, two layers of peritoneum that house blood vessels and nerves. – Some organs of the abdomen, such as the kidneys, pancreas, ascending colon, and duodenum, are located to the outside of the peritoneum (between the peritoneum and the abdominal wall) and are called retroperitoneal organs. • Mesenteries include the mesenteries of the small intestine (mesenteries of jejunum and ileum) and the transverse colon (mesocolon), which connect their respective viscera to the posterior abdominal wall. Omentum • The omentum is a double layer sheet or fold of the peritoneum and connects the stomach to other abdominal organs. • The omentum is organized into the greater omentum and the lesser omentum. – The lesser omentum mostly connects the stomach to the liver. – The greater omentum mostly connects the stomach to the transverse colon. – From the stomach the greater omentum extends downward over the abdominal viscera and then loops back upon itself to attach to the transverse colon. – The transverse colon is attached by the mesentery, the mesocolon, to the posterior abdominal wall. – A large peritoneal ligament, the falciform ligament attaches the liver to the anterior abdominal wall. Figure 26.15 Sagittal section of the abdomen showing the peritoneum, its cavity, and relationship to the abdominal viscera. 5 ORGANS OF THE DIGESTIVE SYSTEM MOUTH The mouth (oral cavity, or buccal cavity) is the area posterior the lips, anterior to the pharynx, medial to the cheeks, inferior to the palate, and superior to the tongue. MOUTH – The anterior region of the mouth is the vestibule. The vestibule is the area between by the lips and cheeks, and the gums and teeth. – The cavity of the mouth, the oral cavity proper, is located within the boundary of the teeth and gums, the palate, the tongue, and the posterior pharynx. – The pharynx (commonly called the throat) is the portion of the digestive tract that extends from the mouth and the superior nasal cavity to the larynx (commonly called the voice box). The pharynx is divided into the nasopharynx, oropharynx, and laryngopharynx. – The roof of the mouth, the palate, consists of the hard palate and the soft palate. Hanging from the posterior boundary of the soft palate is the uvula. During swallowing, the soft palate and uvula close the entrance to the nasal pharynx to prevent the entrance of food. Figure 26.16 Illustration of major structures of the head and neck. Tongue • Internally, the tongue consists of bundles of skeletal muscle fibers (intrinsic muscles) arranged in various directions which are mostly used to change the shape of the tongue. Extrinsic muscles move the tongue for the Tongue Internally, the tongue consists of bundles of skeletal muscle fibers (intrinsic muscles) arranged in various directions with its surface structured as a modified mucous membrane – (1) manipulation of food during chewing, drinking, and swallowing and – (2) movements for the production of sound. • The surface of the tongue is a mucous membrane containing abundant sensory receptors and is lined with protective stratified squamous epithelium. • The superior (top) surface of the tongue contains three types of small protuberances called papillae: – (1) filiform, the (2) circumvallate, and (3) fungiform papillae. • The inferior surface of the tongue is attached to the floor of the oral cavity by the midline lingual frenulum. 6 Figure 26.17 The illustration of the tongue shows the general distribution of its surface projections, the papillae. The two low power photographs show the structure of the papillae. Figure 26.20 High power photograph of a taste bud from a circumvallate papilla. Taste buds contain receptor cells that communicate with the surface by way of “taste hairs” (microvilli) that pass through a pore. Salivary Glands The major salivary glands are the paired Salivary Glands The salivary glands empty saliva into the oral cavity. – (1) parotid - located superficially, slightly inferior, and anterior to the ears – (2) sublingual - located beneath the tongue. – (3) submandibular glands - located medial to the mandible at each mandibular angle The glands may be classified according to the type of secretion they produce or their structural organization. PHARYNX The pharynx is the tube that extends inferiorly from behind the nose to the base of the larynx (voice box). Figure 26.21 High power photograph of the submandibular salivary gland. The submandibular salivary gland contains both mucous and serous cells. 7 PHARYNX • The pharynx is divided into three divisions: – (1) the nasopharynx - does not function as part of the digestive system. – (2) the oropharynx - extends from the level of the soft palate to the level of the hyoid bone – (3) the laryngopharynx - extends from the level of the hyoid bone downward to the cricoid cartilage of the larynx and to the origin of the esophagus Esophagus Esophagus The esophagus is located between the laryngopharynx and the cardiac region of the stomach Esophagus • The esophagus passes through an opening in the diaphragm, the esophageal hiatus, into the abdomen where it joins the cardiac orifice of the stomach. • A sphincter, the cardiac (or gastroesophageal) sphincter surrounds the cardiac orifice and functions to prevent reflux of the stomach’s contents back into the esophagus. • The lumen (inner cavity) of the esophagus is closed by the folding of the mucosa and submucosa, except when in contact with passing food. Figure 26.22 X-ray showing radiopaque substance passing through the esophagus into the stomach. The position of the cardiac sphincter is shown by the constriction where the esophagus meets the stomach. Esophagus STOMACH Figure 26.24 A low power photograph of Figure 26.23 A scanning power photograph the esophagus showing the details of its four layers. of the esophagus in cross-section. Located between the esophagus and the first portion of the small intestine, the duodenum 8 STOMACH STOMACH • The functions of the stomach include – (1) food storage, the – (2) mechanical and enzymatic digestion of foods, and – (3) the production of intrinsic factor for the intestinal absorption of vitamin B12. • The stomach is divided into four regions, the – – – – – (1) cardia, (2) fundus, (3) body, and (4) pylorus. The lateral curved surface of the stomach is called the greater curvature, and the medial curved surface is the lesser curvature Figure 26.25 Illustration showing the general structure of the stomach. STOMACH Stomach Mucosa • Figure 26.27 X-ray of upper digestive tract showing the stomach and the small intestine. Figure 26.28 Scanning power photograph of the wall of the stomach. Stomach Mucosa Figure 26.26 Illustration showing the internal detail of the stomach and the relationship of the stomach to the liver and small intestine. The mucosa of the stomach is modified to allow for expansion (rugae) and to produce gastric juice (gastric glands). Figure 26.29 Illustration of the mucosa of the stomach. The mucosa of the stomach is modified to contain gastric glands, which produce gastric juice, intrinsic factor, and hormones. Figure 26.30 Low power photograph of the mucosa of the stomach. The gastric glands contain parietal, chief, and enteroendocrine cells. Stomach Mucosa • Rugae – The rugae are folds in the mucosa and submucosa that allow for expansion when the stomach fills. • Simple columnar epithelium – The surface epithelium of the mucosa consists of simple columnar epithelium. • Gastric pits – The gastric pits are the openings to the gastric glands. They are lined with the mucous neck cells of the gastric glands. • Mucous neck cells – The cuboidal to columnar mucous neck cells are the cells of the gastric glands that line the gastric pits. • Gastric glands – The gastric glands are glands in the mucosa that mostly produce (1) gastric juice, (2) intrinsic factor, and (3) hormones (by the enteroendocrine cells). The two types of cells that contribute to gastric juice are the (1) parietal cells and the (2) chief (zymogenic) cells. Figure 26.31 High power view of the parietal and chief cells of the gastric glands. Parietal cells produce hydrochloric acid and intrinsic factor. The chief cells produce the inactive enzyme called pepsinogen. 9 Parietal cells • The parietal cells are mostly located in the proximal portions of the gastric glands. Parietal cells function in the production of hydrochloric acid and intrinsic factor. • Hydrogen ions (H+) produced within the parietal cells (CO2 + H2O -> H2CO3 -> H+ + HCO3) are pumped out of the cells into the lumen of the gland. In the lumen, the hydrogen ions combine with chloride ions (from the parietal cells) to form hydrochloric acid (HCl). Hydrochloric acid functions to – (1) activate the enzyme pepsinogen, which is produced by the chief cells, and – (2) denatures proteins of ingested foods and many microorganisms (bacteria and fungi). • Intrinsic factor is a substance produced by the parietal cells that is essential for the intestinal absorption of vitamin B12. Vitamin B12 is essential for the production of normal red blood cells (lack of B12 results in pernicious anemia). Chief (zymogenic) cells • The chief (zymogenic) cells produce an inactive enzyme called pepsinogen. – Hydrochloric acid activates pepsinogen into pepsin, an enzyme that digests proteins to smaller fragments called peptides. – Pepsin begins protein digestion by breaking certain peptide bonds. Further protein digestion occurs in the small intestine. – The chief (zymogenic) cells are mostly located in the distal portions of the gastric glands. Enteroendocrine cells Control of Gastric Activity • Enteroendocrine cells are mostly located in the distal portions of the gastric glands located in the stomach’s pylorus. • The activity of the gastric mucosa is under neural and hormonal control and can be divided into three phases, the – Enteroendocrine cells of the stomach produce hormones mostly involved in regulation of the activity of the stomach’s gastric glands and muscularis. – The release of the hormone gastrin is triggered by the arrival of partially digested proteins into the pylorus. Gastrin enters circulation and targets the gastric glands, which increases – (1) the production of gastric juice and – (2) gastric mixing. Cephalic phase • The cephalic (head) phase begins with the thought, sight, and smell of food. • These stimuli by way of the hypothalamus increase parasympathetic neural output to the stomach by way of the vagus nerves. • The cephalic phase functions to begin the stimulation of the gastric glands to increase gastric juice and hormone production. The neural stimulation of the muscularis externa increases gastric churning. – (1) cephalic phase, – (2) gastric phase, and – (3) intestinal phase. Gastric Phase • The gastric (stomach) phase begins when food enters the stomach. Three primary stimuli for increased gastric secretion are – (1) distension (stretch) of the stomach, – (2) an increase of the stomach’s pH (contents become more basic), and – (3) the presence of proteins. • The primary hormone released by the gastric mucosa is gastrin, which targets the gastric glands resulting in increased release of gastric juice. • As the stomach’s pH decreases to at about a pH of 3, the gastric glands begin to decrease secretion. • Gastrin also – (1) targets the small intestine and increases its motility, – (2) targets the valve between the small and large intestine, the ileocecal valve, resulting in its relaxation, and – (3) targets the large intestine and increases motility. 10 Intestinal phase • The intestinal phase is regulated by chyme entering the duodenum. • As chyme enters the duodenum, it – stretches the duodenum producing a neural response, and – its chemical contents (the presence of lipid, protein, carbohydrate, and pH) trigger a hormonal response. Intestinal phase Distension of the duodenum • The duodenum’s primary neural response to being distended (stretched) results in the inhibition of gastric secretions, mixing, and propulsion. Intestinal phase Response to lipid and protein • The duodenum’s response to the presence of lipid and protein is the secretion of the hormone cholecystokinin (CCK). • Cholecystokinin targets – (1) the gastric glands and inhibits their secretion of gastric juice. Cholecystokinin also targets the – (2) pancreas to produce enzyme rich pancreatic juice, targets – (3) gallbladder stimulating its contraction and release of bile, and targets the – (4) hepatopancreatic sphincter causing its relaxation for the entrance of pancreatic juice and bile into the duodenum. Intestinal phase Response to protein • The duodenum’s response to the presence of proteins is the release of the hormone intestinal gastrin from its mucosa. • Intestinal gastrin targets the gastric glands to increase gastric juice production and gastric mixing. • Pancreatic juice facilitates the digestion of the arriving lipid, protein, and carbohydrate, and buffers the acidic chyme. Bile functions to change lipid into small globules (emulsification) to facilitate their digestion. Intestinal phase Response to decreased pH • The duodenum’s response to the arrival of chyme with a pH of below 4.5 is the secretion of the hormone secretin. • Secretion – (1) targets the stomach and inhibits the gastric glands, gastric mixing, and propulsion, – (2) targets the pancreas and increases the release of bicarbonate ions into the pancreatic juice, and – (3) targets the liver and increases the secretion of bile. • Bicarbonate ions bind hydrogen ions and increase the pH (to more alkaline) of the duodenum’s contents. Submucosa, Muscularis, Serosa • Submucosa – The submucosa is located beneath the mucosa. It consists of loose connective tissue and is highly vascular. • Muscularis Externa – The muscularis externa contains three layers of smooth muscle: (1) an inner oblique layer, (2) a middle circular layer, and (3) an outer longitudinal layer. The muscular contractions aid the churning of food and the emptying of the contents into the small intestine. • Serosa – The serosa is the outer layer and is covered with simple squamous epithelium. The serosa is also called the visceral peritoneum. 11 SMALL INTESTINE SMALL INTESTINE The small intestine is divided into three regions, the (1) duodenum, the (2) jejunum, and the (3) ileum. SMALL INTESTINE • The duodenum begins at the pyloric sphincter and curves to the left around the head of the pancreas. • The duodenum receives chyme from the stomach, bile from the liver and gallbladder, and pancreatic juice from the pancreas. – The common bile duct, which delivers bile from the liver and gallbladder, merges with the pancreatic duct in the wall of the duodenum forming the hepatopancreatic ampulla (pancreaticohepatic ampulla, or duodenal ampulla). – The duodenal ampulla enters the duodenum at a small projection called the duodenal papilla. A sphincter, the hepatopancreatic sphincter (pancreaticohepatic sphincter, or sphincter of Oddi) controls the entrance of bile and pancreatic juice into the duodenum. SMALL INTESTINE • The hepatopancreatic sphincter is mostly controlled by the hormone cholecystokinin (CCK) released from the duodenum in response to the arrival of lipid and/or carbohydrate rich chyme. • The jejunum functions as the primary site for intestinal digestion and absorption. • In the ileum, digestion and the absorption of the end products are finalized. – The ileocecal valve regulates the movement of materials from the ileum to the cecum, the first region of the large intestine. – The relaxation of the ileocecal valve is mostly controlled by the hormone gastrin, which is secreted by the stomach’s mucosa. Gastrin results in • increased gastric gland secretion and gastric motility, and • relaxes the ileocecal valve allowing the small intestine to begin emptying its materials into the large intestine. Figure 26.32 Illustration showing the relationships of the duodenum, liver, and pancreas. SMALL INTESTINE SMALL INTESTINE - MUCOSA • The mucosa of the small intestine is modified for – (1) increasing surface area for absorption and the – (2) secretion of intestinal juice. • Modifications for increasing surface area include – (1) villi - small fingerlike vascular projections formed by the mucosa – (2) microvilli - microvilli are minute “hairlike” projections of the surface (apical) plasma membranes of the columnar cells. Figure 26.33 Scanning power photograph of a cross-section of the small intestine (jejunum). The wall of the small intestine consists of four layers. Figure 26.34 Low power photograph of the wall of the small intestine (jejunum). The photograph shows details of the intestine’s four layers. 12 SMALL INTESTINE - MUCOSA Figure 26.35 Illustration showing the modification of the mucosa of the small intestine into villi and intestinal glands. Figure 26.36 Low power photograph showing the mucosa of the small intestine. Villi increase the surface area and intestinal glands produce intestinal juice. SMALL INTESTINE - MUCOSA SMALL INTESTINE - MUCOSA Figure 26.38 Except for fats, the end-products of digestion enter the blood capillaries immediate beneath the epithelium. The capillaries enter the hepatic portal circulation and are transported to the liver. Fats enter the lacteal and are transported into systemic circulation. SMALL INTESTINE MUSCULARIS EXTERNA • The muscularis externa contains two distinctive layers of smooth muscle. – The outer layer of smooth muscle is called the longitudinal layer as the cells are located parallel to the long axis of the organ. Contraction of the longitudinal layer shortens the organ and causes a dilation of its internal cavity. – The inner layer of smooth muscle is called the circular layer as the cells are located around the circumference of the organ. Contraction of the circular layer lengthens the organ and causes a constriction of its internal cavity. • Contraction of the smooth muscle produces segmentation and peristalsis. Figure 26.39 High power photograph of intestinal glands. Intestinal glands produce intestinal juice, a watery mixture of mucus. – Segmentation is the process of dividing and mixing the intestinal contents. – Peristalsis is the wavelike muscular contractions that produce forward movement of the intestinal contents. SMALL INTESTINE MUSCULARIS EXTERNA REGIONS OF THE SMALL INTESTINE Figure 26.40 Scanning and high power photographs of the muscularis externa of the small intestine. The muscularis externa consists of an inner circular and an outer longitudinal layer. Intestinal movements include peristalsis and segmentation. Duodenum - Duodenal (Brunner’s) Glands and Ileum - Peyer’s Patches 13 Duodenum - Duodenal (Brunner’s) Glands Figure 26.41 • The duodenum, is specialized for the mixing of chyme, bile, and pancreatic juice. • The acidic chyme entering the duodenum is prevented from damaging the mucosa by the thick alkaline mucous coating produced by the duodenal (Brunner’s) glands. Duodenal glands are located in the submucosa and empty onto the surface of the duodenum through ducts. Peyer’s Patches • Peyer’s patches are lymphatic nodules located in the submucosa of the ileum. When found in groups, or aggregated, they are called Peyer’s patches. • Peyer’s patches are sites of lymphatic tissue which defend against bacteria and antigenic substances in the intestinal contents. Peyer’s patches become more numerous at the distal portion of the ileum. Figure 26.41 PANCREAS PANCREAS The pancreas is located beneath the stomach in a transverse position along the fold of the duodenum. The pancreas functions as both an endocrine gland and as an exocrine gland. PANCREAS • The most abundant cells of the pancreas (about 99%) are exocrine in function and are organized into groups called acini. Each pancreatic acinus is formed by a group of exocrine cells that surrounds a central lumen (cavity). • The acini produce pancreatic juice which enters into small ducts. The small ducts merge into the pancreatic duct which leaves the pancreas, unites with the common bile duct, and enters the duodenum at a common region called the hepatopancreatic ampulla. • The least abundant cells of the pancreas (about 1%) are endocrine in function and are organized into the islets of Langerhans. • The islets of Langerhans are highly vascular, and their secretions (hormones) enter the blood. Two of the hormones released from the islets are – insulin and – glucagon, – Both function in the regulation of blood glucose levels. Pancreatic Juice • The release of pancreatic juice (and bile) from the hepatopancreatic ampulla is controlled by the hepatopancreatic sphincter. • The hormone cholecystokinin produced at the duodenum targets the hepatopancreatic sphincter and results in its relaxation. • Pancreatic juice neutralizes the acidic chyme from the stomach, and it contains digestive enzymes for the digestion of carbohydrate, protein, and lipid. 14 Secretin Pancreatic Juice • The secretion of pancreatic juice is under hormonal and neural control. – Neurally, the pancreas is controlled by the parasympathetic division of the autonomic nervous system by way of the vagus nerves. – The dominate control mechanism for secretion of pancreatic juice is by the hormones secretin and cholecystokinin, which are released by the enteroendocrine cells of the duodenum. Secretin • The hormone secretin is released when the enteroendocrine cells of the duodenum are stimulated by the arrival of acidic chyme. • Secretin targets the pancreas and stimulates the release of bicarbonate rich pancreatic juice. Bicarbonate functions as a hydrogen ion acceptor and neutralizes the acidity. Cholecystokinin (CCK) • The hormone cholecystokinin (CCK) is released when the enteroendocrine cells of the duodenum are stimulated by the arrival of chyme rich in fats and proteins. • Cholecystokinin targets the pancreas and stimulates the release of enzyme rich pancreatic juice. Enzymes function in the intestinal digestion of incoming fats, proteins, and carbohydrates. Figure 26.43 Illustration showing the function of the hormone secretin. Cholecystokinin (CCK) PANCREAS Figure 26.45 Scanning power photograph of the pancreas. The pancreas is organized into exocrine (acini) and endocrine (islets) cells. Figure 26.46 High power photograph of the pancreas showing an islet and groups of acini. Pancreatic acini function in the secretion of pancreatic juice. Figure 26.43 Illustration showing the function of the hormone cholecystokinin (CCK). 15 Liver LIVER The liver is located in the upper right part of the abdominal cavity immediately below the diaphragm. Liver • Two major vessels enter the liver, the hepatic artery and the hepatic portal vein. – The hepatic artery delivers oxygen rich blood to the liver. – The hepatic portal vein delivers oxygen-poor blood rich in nutrients from the digestive tract to the liver. • The liver functions to process the nutrient rich blood from hepatic portal circulation before it enters systemic circulation. Liver – Bile Secretion • The liver consists of four divisions, or lobes, the (1) right lobe, (2) left lobe, (3) quadrate lobe, and (4) the caudate lobe. • The falciform ligament, a large ligament that attaches the liver to the diaphragm and the anterior abdominal wall, separates the right and left lobes. The larger of these two lobes is the right lobe and at its medial inferior surface is the much smaller quadrate lobe. The small caudate lobe is found at the liver’s superior posterior surface between the right and left lobes. • The remnant of the fetal umbilical vein, the ligamentum teres (or round ligament) is located at the anterior free margin of the falciform ligament. • The gallbladder is located in a shallow depression on the inferior surface of the right lobe. Liver • The liver also functions to produce bile. Increased secretion of bile results from stimulation of the liver by – (1) increased blood levels of bile salts and the hormone – (2) secretin. • Bile salts are the components of bile that function in the emulsification of fats. • When acidic, protein and fat rich chyme enters the duodenum the enteroendocrine cells release the hormones secretin and cholecystokinin (CCK). – Cholecystokinin targets the gallbladder resulting in contraction, and targets the hepatopancreatic sphincter resulting in relaxation. – Bile then enters into the small intestine where its bile salts function in the emulsification of fats. The bile salts are reabsorbed from the small intestine into the blood. Liver – Lobules • The functional units of the liver are called lobules. A lobule consists of hepatic cells (hepatocytes) that form rows (cords or plates) in a radial pattern around a central vein. • Between the cords are modified capillaries (sinusoids) that receive blood from both the hepatic artery (highly oxygenated) and the hepatic portal vein (contains products of digestion). • The sinusoids are lined with macrophages (Kupffer cells) that destroy worn-out blood cells and bacteria. The blood leaves the sinusoids and enters the central vein. Figure 26.46 Illustration showing the control of the secretion of bile. 16 Liver – Lobules Liver – Lobules • The central veins of the lobules ultimately merge and route blood into systemic circulation through the hepatic veins. • Bile ducts collect bile from small channels, the bile canaliculi, located at the basal surface of the hepatocytes. The bile ducts lead to the right and left hepatic ducts, which exit the liver. Figure 26.48 Illustration showing the structure of the functional units of the liver, the lobules. Liver – Lobules Figure 26.49 Scanning power photograph of the liver’s lobules with Masson’s stain. Masson’s stain differentiates the connective tissue that surrounds the lobules. Figure 26.50 High power photograph of a lobule. The lobules are the functional units of the liver. Liver - Glucose Figure 26.51 Low and high power photographs of the liver showing hepatocytes with glycogen. Storage of glycogen is promoted by the hormone insulin, which is secreted by the pancreatic islets when blood levels of glucose increase. Figure 26.52 Low and high power photographs of hepatocytes with their glycogen removed. The tissue is treated with amylase which digests the glycogen into glucose. Liver - Glucose • The liver has several metabolic functions that relate to the processing of blood received from the digestive system. One function is the processing of glucose. • The liver functions as the primary glucose storage organ for the maintenance of blood glucose levels. The liver is targeted by the blood sugar regulating hormones insulin and glucagon, which are secreted by the pancreas. Liver - Kupffer Cells • The liver functions as a site for macrophages which remove substances such as bacteria and worn out red blood cells from the blood. The macrophages of the liver are called Kupffer cells and are fixed macrophages because they remain in the sinusoids of the liver Figure 26.53 Kupffer cells are the fixed macrophages of the liver. Located within the sinusoids, the Kupffer cells function to remove foreign materials found within the blood. 17 LARGE INTESTINE LARGE INTESTINE • The large intestine extends from the end of the ileum to the anus and is mostly positioned around the small intestine. • The gross anatomy of the large intestine differs from the small intestine in three major differences, – (1) in its diameter, the – (2) presence of haustra, and – (3) epiploic appendages. The large intestine functions mainly as the (1) final absorption site for water and remaining electrolytes, (2) compacts remaining fecal material, and is a (3) storage site for waste materials prior to defecation. LARGE INTESTINE • As its name indicates, the diameter of the large intestine is greater than that of the small intestine. – The longitudinal muscle of the large intestine is not organized into an encircling layer as found in the small intestine. Instead, the longitudinal muscle is organized into three ribbon-like bands, the teniae coli. Muscle tone of the teniae coli shortens the large intestine forming pouch-like regions called haustra. • Projecting from the surface of the large intestine are numerous fat-filled sacs, the epiploic appendages. The epiploic appendages are formed from the serosa (visceral peritoneum). LARGE INTESTINE LARGE INTESTINE • The large intestine is divided into five regions, the – (1) cecum, – (2) appendix, – (3) colon, – (4) rectum, and – (5) anal canal. LARGE INTESTINE • Cecum – The large intestine begins with a pouch-like portion, the cecum. The distal region of the small intestine, the ileum, joins the cecum at the ileocecal valve. The ileocecal valve is relaxed by the hormone gastrin, produced during the gastric phase of the stomach’s response to arriving food. Attached to the inferior aspect of the cecum is the appendix. • Appendix – The walls of the appendix house lymphatic tissue. • Colon – – – – – The colon is divided into four major divisions, the (1) ascending colon, the (2) transverse colon, the (3) descending colon, and the (4) sigmoid colon. • The short anal canal terminates at the opening to the outside called the anus. Figure 26.54 The large intestine functions mainly as the final absorption site for water and remaining electrolytes, compacts remaining fecal material, and is a storage site for waste materials prior to defecation. The large intestine is divided into five regions, the (1) cecum, (2) appendix, (3) colon, (4) rectum, and (5) anal canal. 18 LARGE INTESTINE LARGE INTESTINE - Mucosa Figure 26.56 The mucosa of the large intestine is modified for absorption (simple columnar epithelium) and the secretion of mucus (intestinal glands). Figure 26.55 Scanning power photograph of the large intestine showing its four layers. Figure 26.57 The mucosa of the large intestine contains numerous goblet cells, which function in the secretion of lubricating mucus. LARGE INTESTINE - Muscularis Externa The muscularis externa consists of (1) an inner circular muscle layer, and (2) the teniae coli. • The teniae coli are the three ribbon-like bands of longitudinally arranged smooth muscle of the large intestine. Muscle tone of the teniae coli puckers the large intestine into pouch-like areas called haustra. • The muscularis externa functions in the mixing and the movement of the intestinal contents. Mixing by segmentation occurs as some haustra undergo contractions and move the contents into adjacent haustra. Mass movements occur as peristaltic waves travel long distances to move the intestinal contents forward and into the rectum. 19